Abstract
Sperm granuloma is a common finding following vasectomy, with majority of the lesions located at the site of the vasectomy defect. Sperm granulomas are typically small and asymptomatic. We describe a case in which the nodule presented similarly to a supernumerary testis by radiographic features.
Keywords: Sperm granuloma, Vasectomy, Supernumerary testis, Polyorchidism
Introduction
Various lesions can occur following vasectomy that represent the body's response to increasing fluid and pressure in the proximal ejaculatory system. The dissection of sperm into the vasal wall and extravasation into the interstitium can cause vasitis nodosa and sperm granuloma, respectively. While vasitis nodosa represent a benign proliferation of vasal epithelium cells, sperm granuloma is a granulomatous lesion that constitutes a foreign-body giant cell reaction to the extravasated sperm and commonly occurs in up to 42% of patients following vasectomy.1 While the majority of sperm granulomas are asymptomatic and less than 1 cm in size, they can occasionally present with pain and swelling of the upper pole of the epididymis, spermatic cord, and testis. Ultrasound typically shows a well-defined, hypoechoic extratesticular lesion located within the epididymis or at the cut ends of the vas deferens.2
Case presentation
A 38-year-old man presented with 6 weeks of right-sided testicular pain and an enlarging intra-scrotal mass. He described the pain as a pressure, occasionally sharp, localized to the scrotal contents. The pain was worse with sitting and at the end of the day. The pain did not improve with naproxen. He reported an enlarging mass above the testicle that he noticed over the past several months. The mass was increasing in size according to the patient. Review of systems was negative for any lower urinary tract symptoms (LUTS), hematuria, and erectile dysfunction. The patient underwent a vasectomy 13 months previously performed by an outside provider, with no complication or discomfort until this recent episode. The mass was also not palpable prior to the vasectomy. Otherwise, medical history is only significant for esophageal reflux, essential hypertension, and hyperlipidemia. Of note, he did have an inguinal surgery as a child–the details of this were not known. There is no family history of genitourinary malignancy.
On physical examination, he was noted to have a small firm round structure lateral to the right spermatic cord. The structure was felt to be adjacent to but separate from the vas deferens and superior to the right testis on physical examination. The mass was non-tender. On ultrasound, a 1.6 × 1.5 × 1.3 cm oval shaped mass was identified in the right scrotum, superior to the right testicle, corresponding to the palpable mass. This lesion showed homogeneous low-level echogenicity similar to both testicles and contained a cluster of echogenic, shadowing calcifications centrally. No vascular flow was identified within the lesion on color Doppler imaging (Fig. 1). Tumor markers, including alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (hCG), and lactate dehydrogenase (LDH), were all negative.
Fig. 1.
Sagittal greyscale ultrasound image shows a well-circumscribed, oval-shaped mass (white star) superior to the right testicle (labeled). The mass is isoechoic to the right testicle with similar echotexture. An echogenic, shadowing calcification (white dashed arrow) is noted within the supratesticular mass.
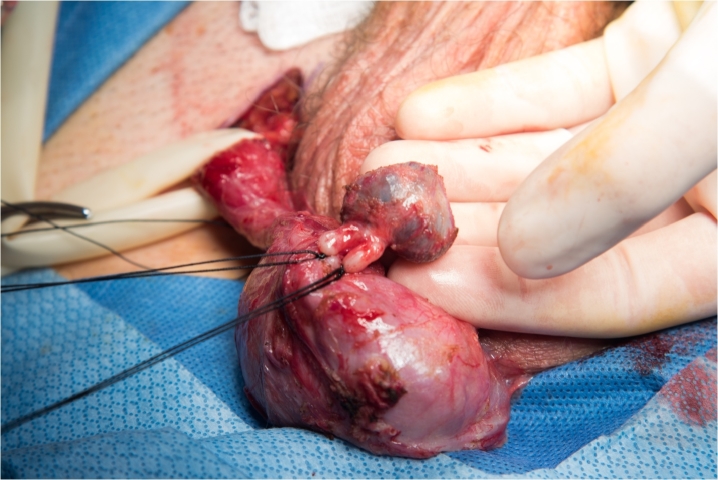
Given the firm nature of the structure, the timing of appearance after vasectomy (13 months later and enlarging per patient), and coarse calcifications, decision was made to proceed with inguinal exploration and excision with frozen section rather than a pre-surgical biopsy. Intra-operatively, the convoluted vas deferens was entering the structure. Gross examination revealed a 2.0 × 1.0 × 0.5 cm circular soft mass with a blue tinge and when opened by the pathologist, was noted to be filled with old blood (Fig. 2). The mass was excised–frozen section confirmed no evidence of malignancy. Histopathological examination of the right paratesticular mass revealed suture granuloma, sperm granuloma, vasitis nodosa, and fibrosis near the prior vasectomy site.
Fig. 2.
Gross specimen of the excised right paratesticular mass.
Discussion
While sperm granulomas have been occasionally reported to produce tumor-like lesions, with firm nodule and cysts formation, we observed a sperm granuloma that mimicked as a supernumerary testis due to its appearance on ultrasound and time-course of its presence post-vasectomy. The only feature that was not consistent with a supernumerary testis was the lack of vascular flow on Doppler ultrasound. In situations where ultrasonography is indeterminate, magnetic resonance imaging (MRI) can confirm the nature of a supernumerary testis, as they have the same signal intensity to the normal testis. However, in this case, surgical excision was pursued due to the patient's pain rather than advanced imaging or biopsy. Additionally, the lesion was enlarging in size with significant coarse calcifications which prompted us to rule out testicular malignancy, as one report has estimated an increased risk (6.4%) of malignancy in the setting of polyorchidism.3
The acoustic shadowing from the macrocalcification further obscured a definitive diagnosis, as this radiographic feature can be seen with regressed, or “burned-out”, testicular tumors.4 Some germ cell tumors have been reported to spontaneously regress as they outgrow their blood supply, resulting in a necrotic area that precipitates calcium deposition. While calcification can be observed in a granulomatous process, this is a relatively uncommon finding, reported to occur in less than 10% of sperm granulomas in one study.5
Of note, the gross examination of the excised mass was also unusual. To our knowledge there is no report of sperm granuloma containing blood. Because the histology revealed an expected inflammatory change near the site of vasectomy, no further testing, such as immunohistochemical staining, was performed to rule out other blood-filled masses.
Conclusion
We present a sperm granuloma that mimicked a supernumerary testis with possible malignancy. The natural history underlying this case was rather unconventional and did not convey a benign change that typically follows vasectomy. Because of the echogenicity of the nodule and the finding of an “intratesticular” calcification, differential diagnosis of a testicular neoplasm in a supernumerary testis was kept in mind.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Consent
Informed consent was obtained from the patient for publication of the case report.
Declaration of competing interest
The authors do not have conflicts of interest to disclose.
Acknowledgements
None.
Contributor Information
Johnny S. Su, Email: suj@ccf.org.
Nicholas J. Farber, Email: farbern@ccf.org.
Myra K. Feldman, Email: feldmam2@ccf.org.
Sarah C. Vij, Email: vijs@ccf.org.
References
- 1.Cheng L. fourth ed. Elsevier; St. louis, MO: 2019. Urologic Surgical Pathology.https://www.clinicalkey.com/#!/browse/book/3-s2.0-C20160034927 [Google Scholar]
- 2.Oh C., Nisenbaum H.L., Langer J., Rowling S., Arsdalen K.N.V. Sonographic demonstration, including color Doppler imaging, of recurrent sperm granuloma. J Ultrasound Med. 2000;19(5):333–335. [PubMed] [Google Scholar]
- 3.Bergholz R., Wenke K. Polyorchidism: a meta-analysis. J Urol. 2009;182(5):2422–2427. doi: 10.1016/j.juro.2009.07.063. [DOI] [PubMed] [Google Scholar]
- 4.Coursey Moreno C., Small W.C., Camacho J.C. Testicular tumors: what radiologists need to know—differential diagnosis, staging, and management. RadioGraphics. 2015;35(2):400–415. doi: 10.1148/rg.352140097. [DOI] [PubMed] [Google Scholar]
- 5.Schmidt S.S., Morris R.R. Spermatic granuloma: the complication of vasectomy. Fertil Steril. 1973;24(12):941–947. [PubMed] [Google Scholar]