Abstract
Background:
Acne vulgaris (AV) is one of the most common skin diseases with major psychological impacts. Hence, selecting the best treatment modality is so important; there are different ways to treat AV such as topical and systemic agents, laser, and also photodynamic therapy. In this study, we tried to assess the difference between the efficacy of combination therapy with intense pulsed light (IPL) and benzoyl peroxide (BPO) in comparison with IPL and adapalene (AD) in the treatment of the mild to moderate AV.
Materials and Methods:
Thirty Iranian females in reproductive age with mild to moderate acne were enrolled in this study. The left and right side of the patients were randomized to receive either AD 0.1% or BPO 5% every other day plus three sessions of monthly apart IPL in the treatment of AV. Different parameters of AV such as acne severity index (ASI), total acne lesions counting (TLC), and Acne Global Severity Scale (AGSS) were measured before, during, and after the treatments.
Results:
There was a significant difference regarding AGSS, TLC, and ASI before and after treatment with AD plus IPL (P < 0.001). Furthermore, there was a significant difference regarding AGSS, TLC, and ASI before and after treatment with BP plus IPL (P < 0.001). However, no significant difference regarding AGSS, TLC, and ASI were observed between the 2 groups after treatment (P > 0.05). No significant side effects were observed in both groups.
Conclusion:
Our study shows that there was not any significant difference between combining IPL with either AD or BPO so we can use either one of these combinations to achieve similar efficacy.
Keywords: Acne vulgaris, adapalene, intense pulsed light
INTRODUCTION
Acne vulgaris (AV) is the most common inflammatory skin disease treated by dermatologists. Moreover, it is the most frequent disease worldwide, especially in adolescents.[1,2] It is characterized by inflammatory lesions such as papules, pustules, nodules or cysts and also noninflammatory lesions such as codomones.[3] AV is a multifactorial disease, and the exact mechanism or pathogenesis is unknown.[4,5] AV affects people in a different range specially between of ages and it is more severe in males. While it is not a life-threating disorder with no reported mortality due to AV, it has major emotional and psychological impacts such as depression, decreased self-confidence, and anxiety.[2,6]
There are different ways to treat AV such as topical and systemic agents, laser, and also photodynamic therapies. The choice of therapy depends on different factors such as the age of patients, site, and severity of acne.[7,8] Topical therapies including antibiotics, benzoyl peroxide (BPO), retinoids, and sulfone agents are the first-line treatment in mild to moderate acne.[9,10,11] The most common approach for treating AV is oral antibiotics plus topical retinoid or BPO. BPO is a non antibiotic, anti bacterial agent and lipophilic nature that reduce the sebaceous gland activity. Studies showed that BPO can reduce inflammatory and noninflammatory lesions, but it is more effective in noninflammatory lesions.[12,13]
Adapalene (AD) is a synthetic, third-generation topical retinoid that is derived from naphthoic acid. It has a critical role in the treatment of acne because of its anti-inflammatory effects in addition to its comedolytic activity.[14,15]
Intense pulsed light (IPL) therapy is a treatment modality that uses ultraviolet and visible light. It has photodynamic effects, and it is used alone or in combination with other treatments for AV.[16,17] The exact mechanism of action of IPL therapy in treatment of AV is unknown, but it may reduce Propionibacteriumacne acne proliferation and sebum production.[18]
As the combination therapy with different modalities could increase the response rate in a shorter interval, we decided to investigate the efficacy of combining AD and BPO to IPL to achieve better results.
MATERIALS AND METHODS
This randomized clinical trial study was performed in dermatology outpatient clinics of Isfahan University of medical sciences, Isfahan, Iran between May 2017 and May 2018. The study was approved by the Ethics Committee of Isfahan University of Medical Sciences and performed according to the Declaration of Helsinki (IRCT20181229042165N1). Informed consent was obtained from all participants before entering the study.
Thirty females in reproductive ages with mild and moderate AV disorder which was diagnosed by the dermatologist who was the author of the proposal were enrolled in the study. We considered persons with the following conditions as mild and moderate acne patients:
(1) clear skin with rare noninflammatory lesions and rare noninflamed papules, (2) some noninflammatory lesions with few inflammatory lesions, and (3) non inflammatory lesions predominate, with multiple inflammatory lesions evident, several to many and papules/pustules, and there may or may not be one small nodulocystic lesion.[19]
Inclusion criteria were preference of laser therapy, no previous history of photosensitivity, no history for systemic retinoids and steroids therapy in the last 6 months, systemic lupus erythematosus or porphyria,[19] no history of systemic or topical medications for acne for the previous 3 weeks, and the absence of severe acne scars. The exclusion criteria were pregnancy or breastfeeding, being photosensitized during study, and withdrawal of the therapy. The excluded patients were replaced with new cases. We treated our patients with AD 0.1% gel (Najo Company, Iran) and BPO 5% gel (Acne fight kit) in either side of the face for 1 h at night, 3 times a week for 2 weeks. If there was no allergic reaction, the patients gradually increased the time at first we used topical treatment on both side of face, we increased the dose of treatment gradually. Patients were recommended to use a SPF 50 antisolar cream (patient used the antisolar cream about 5 g before of any exposure to sunlight and refresh it every 2 hours).
The parameters such as acne severity index (ASI), total acne lesions counting (TLC),[20] and Acne Global Severity Scale (AGSS)[21] were measured before and after treatment for each side of the face of participants.
We used simple randomization to detect which side of the face should be treated with each treatment technique; also for decreasing of side effects, patients were asked to stop the topical treatment. Participants used topical treatment, 3 times a week overnight for 3 months. At the end of the 1st, 2nd, and 3rd-month topical therapy, based on previous studies, as well as decreasing of cost and side effects of IPL and topical treatment, we used one session IPL on whole of the face. Each patient at the treatment IPL group received IPL therapy with wavelength of 570 nm filter, 15 j/cm2 energy fluence, and 40 ms pulse duration in a single pulse mode. SOLARI™ (Lutronic Corporation, Ilsan, Korea) system was used for IPL administration.[19]
AV lesions criteria (ASI, TLC and AGSS) were measured before, during and the end of treatment and 4 month follow up. Furthermore, the side effects of IPL including pain, burning, postinflammatory pigmentation (PIP) and scar, and topical treatment including dryness, scaling and erythema, photosensitivity, and itching were recorded in each session.
Each patient was also asked to point his/her satisfaction at each visit on a straight line without midpoints ranging from 0: dissatisfied to 10: very satisfied. Then, the length from 0 to the marked point was measured using a ruler and recorded as the patient satisfaction score. Expected complications of pain, burning, postinflammation pigmentation, erythema, scaling, redness, and dryness were also of interest.
Statistical analysis
Data analysis was carried out using SPSS (v18; SPSS Inc. Chicago, IL, USA). The normality of data was determined by Kolmogorov–Smirnov and nonparametrical Chi-square and Fisher's exact tests were used to evaluate the association. P < 0.05 was considered as statistically significant.
RESULTS
Thirty women (mean age ± standard deviation 23.63 ± 5.78, range from 14 to 34 years) with AV disorder were recruited. According to AGSS, 60% of the patients were in grade 3 acne before treatment. TLC was 19.7 ± 5.23 and 19.1 ± 5.41 (P < 0.05) for AD and BPO, respectively, and ASI was 16.27 ± 4.87 and 15.87 ± 5.46 (P < 0.05) for AD and BPO, respectively, before the treatment [Table 1]. There was no significant difference with regard to severity of AV lesions before treatment in the 2 groups (P = 0.8 for grade, P = 0.57 for TLC and P = 0.83 for ASI) [Table 1].
Table 1.
Characteristics for study groups
| ADA and IPL group | BPO and IPL group | P | |
|---|---|---|---|
| Sex:female (%) | 30 (100) | ||
| Age | 23.63±5.78 | ||
| Grade (%) | |||
| Grade 1 | 0 (0.0) | ||
| Grade 2 | 4 (13.3) | ||
| Grade 3 | 18 (60) | ||
| Grade 4 | 8 (26.7) | ||
| AGSS | 2.06±0.59 | 2.19±0.83 | 0.61 |
| ASI | 16.27±4.87 | 15.87±5.46 | 0.57 |
| TLC | 19.7±5.23 | 19.1±5.41 | 0.83 |
BPO=Benzoyl peroxide; AGSS=Acne global severity scale; ASI=Acne severity index; TLC=Total acne lesions counting; IPL=Intense pulsed light
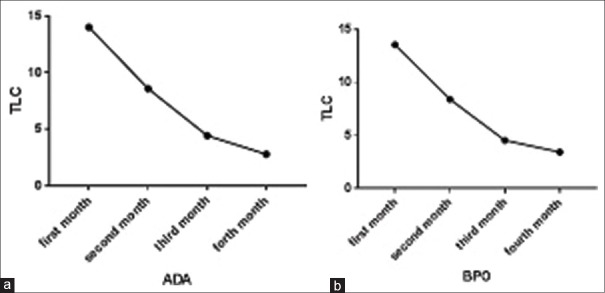
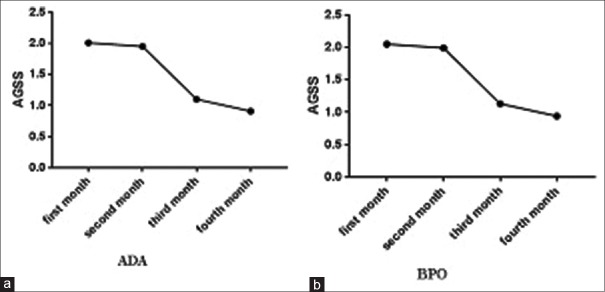
Comparison of acne vulgaris lesions before and after treatment by adapalene plus intense pulsed light
There was significant difference regarding AGSS, TLC, and ASI before and after treatment with AD plus IPL (P < 0.001) [Table 2 and Figures 1–3].
Table 2.
Comparison of various measures between two treatment groups during follow up visits
| ADA and IPL group | BPO and IPL group | P | |
|---|---|---|---|
| AGSS | |||
| Month 1 | 2.01±1.3 | 2.05±1.4 | 0.87 |
| Month 2 | 1.95±1.1 | 1.99±1.2 | 0.72 |
| Month 3 | 1.1±0.9 | 1.13±0.89 | 0.31 |
| Follow-up | 0.91±0.6 | 0.94±0.61 | 0.75 |
| ASI | |||
| Month 1 | 12.08±3.76 | 10.84±4.2 | 0.19 |
| Month 2 | 6.72±3.14 | 6.31±2.86 | 0.52 |
| Month 3 | 3.19±1.9 | 2.95±1.97 | 0.62 |
| Follow-up | 2.8±1.3 | 2.05±1.1 | 0.21 |
| TLC | |||
| Month 1 | 14±3.73 | 13.53±4.32 | 0.66 |
| Month 2 | 8.6±2.96 | 8.4±3.39 | 0.98 |
| Month 3 | 4.43±1.94 | 4.53±2.28 | 0.84 |
| Follow-up | 2.8±1.82 | 3.43±2.62 | 0.34 |
BPO=Benzoyl peroxide; AGSS=Acne global severity scale; ASI=Acne severity index; TLC=Total acne lesions counting; IPL=Intense pulsed light
Figure 1.
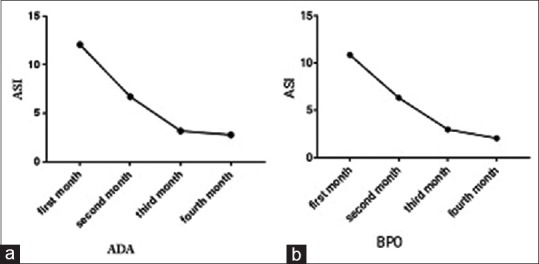
Acne severity index decreasing after 4-month follow-up (a) adapalene, (b) benzoyl peroxide
Figure 3.
Total acne lesions counting decreasing after 4-month follow-up (a) adapalene, (b) benzoyl peroxide
Figure 2.
Acne Global Severity Scale decreasing after 4-month follow-up (a) adapalene, (b) benzoyl peroxide
There was significant difference regarding AGSS, TLC, and ASI before and after treatment with BP plus IPL (P < 0.001) [Table 2].
Comparison between acne vulgaris lesions treated by adapalene plus intense pulsed light and benzoyl peroxide plus intense pulsed light
There was no significant difference regarding AGSS, TLC, and ASI between the 2 groups after treatment (P > 0.05), [Table 2].
Most of the patients (66.7%) reported no difference between efficacy of AD and BPO. However, 13.3 of the patients preferred AD and 29% preferred BPO [Figure 4].
Figure 4.

A 28-year-old patient with acne vulgaris: (a and c) before treatment, (b) 4 months after treatment with adapalene plus intense pulsed light (right side of face), (d) 4 months after treatment with benzoyl peroxide plus intense pulsed light (left side of face)
Side effects of topical treatments
Furthermore, we reported the AD plus IPL and BPO plus IPL side effect such as dryness, scaling, and erythema as a topical treatment. Our results showed there was not any significant difference between AD and BPO in terms of side effect (P > 0.05 for all) [Table 3].
Table 3.
Comparison between adapalene and benzoyl peroxide side effects
| Side effect | AD (%) | BPO (%) | P |
|---|---|---|---|
| Dryness | |||
| Yes | 13 (43.3) | 11 (36.7) | 0.93 |
| No | 17 (76.7) | 19 (63.3) | |
| Scaling | |||
| Yes | 15 (50) | 9 (30) | 0.50 |
| No | 15 (50) | 21 (70) | |
| Erythema | |||
| Yes | 11 (36.7) | 7 (23.3) | 0.17 |
| No | 19 (63.3) | 23 (76.7) |
BPO=Benzoyl peroxide; AD=Adapalene
Side effects of intense pulsed light
Side effects of IPL were similar in the 2 groups. IPL therapy showed several side effects including pain, burning, and PIP. 10 (33.3%) patients had pain in the face during IPL therapy, postinflammatory hyperpigmentation (PIH) occurred in 2 (6.7%) patients, and no patients complained of skin burning after treatment. Our results showed that there were no significant differences for AD and BPO for IPL.
DISCUSSION
Effective treatment of AV is important because of the psychologic problems due to possible scarring.[1] In this study, our aim in this study was to find the preferred combination therapy for AV to reduce the risk of scarring. The results of the present study showed that there were not any significant differences between the two groups with respect to AGSS, ASI, and TLC before and after 4-month treatment period. Although a previous study has shown that treatment with IPL leads to several side effects such as erythema, burning, dryness, pain, and PIH, our data showed safety of IPL for the treatment of AV. It might be due to the conservative selected parameters or long intervals between therapy.
Puttaiah and Jartarkar showed that IPL therapy decreased AV lesions and no side effects were reported in this study.[18] This was in accordance with our results. Combination treatment of IPL with photodynamic therapy with topical 5-aminolevulinic acid showed better and more prolonged response.[22,23,24] On the other hand, there are some studies showed nonsignificant effect of IPL on inflammatory lesions with some effects on noninflammatory lesions.[25] However, our study showed that even monthly intervals could decrease both the inflammatory and noninflammatory lesions.
We showed that AD in combination of IPL can decrease AV lesions after a 4-month period. This might be shorter than each one of these treatments alone. Cost and side effects are reduce more than monotherapy. Chlebus et al. also showed that AD as a maintenance therapy can significantly reduce noninflammatory and inflammatory lesions in patients with mild and moderate AV as a maintenance therapy.[26] Moreover, the combination of AD and BPO had significantly greater efficacy for the treatment of AV than AD alone.[27] Both BP and AD showed enough efficacy in decreasing inflammatory and noninflammatory acne lesions, but addition of these to IPl might ameliorate the response rate in a shorter time.[28,29]
Our data revealed that a 4-month period of AV treatment with the combination of BPO with IPL was sufficient to reduce AV lesions. This observation was consistent with our previous study that showed adding IPL to BPO provides better efficiency compared to BPO alone.[19] BPO alone or combination with other topical agents had a potent activity in the improvements of acne lesions by reducing fatty acid.
Iftikhar et al. found that both AD 0.1% gel and BPO 4% gel have similar efficiency in clearing mild to moderate acne lesions. However, AD was more effective in the reduction of comedones while BPO was more beneficial for inflammatory acne.[30] In addition, Penna et al. and Sittart et al. showed that the AD and BPO treatments were helpful in ameliorating AV and less expensive than other treatments.[31,32] Our study shows the same effects in two groups which is in accordance with the discussed articles.
CONCLUSION
In the present study, we observed that there was no significant difference between AD and BPO efficacy in AV treatment. Regarding the results of our study, we recommend using of IPL in addition to BPO or AD for treatment of the mild and moderate AV.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
The study was financially supported by Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors thank all individuals who participated in the study. This work was supported by Department of Dermatology, Isfahan University of Medical Sciences.
REFERENCES
- 1.Sams WM, Lynch PJ. Principles and Practice of Dermatology. First Edition. New York: Churchill Livingstone. Churchill Livingstone; 1990. pp. 152–3. [Google Scholar]
- 2.Bhate K, Williams HC. Epidemiology of acne vulgaris. Br J Dermatol. 2013;168:474–85. doi: 10.1111/bjd.12149. [DOI] [PubMed] [Google Scholar]
- 3.Benner N, Sammons D. Overview of the treatment of acne vulgaris. Osteopath Fam Physician. 2013;5:185–90. [Google Scholar]
- 4.Tahir CM. Pathogenesis of acne vulgaris: Simplified. J Pak Assoc Dermatol. 2016;20:93–7. [Google Scholar]
- 5.Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945–73.e33. doi: 10.1016/j.jaad.2015.12.037. [DOI] [PubMed] [Google Scholar]
- 6.Hsieh MF, Chen CH. Delivery of pharmaceutical agents to treat acne vulgaris: Current status and perspectives. J Med Biol Eng. 2011;32:215–24. [Google Scholar]
- 7.Mahmood NF, Shipman AR. The age-old problem of acne. Int J Womens Dermatol. 2017;3:71–6. doi: 10.1016/j.ijwd.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simpson NB, Cunliffe WJ. Rook's Textbook of Dermatology. Blackwell Publishing Ltd; 2004. Disorders of the sebaceous glands; pp. 2121–96. [Google Scholar]
- 9.Mills OH, Jr, Kligman AM, Pochi P, Comite H. Comparing 2.5%, 5%, and 10% benzoyl peroxide on inflammatory acne vulgaris. Int J Dermatol. 1986;25:664–7. doi: 10.1111/j.1365-4362.1986.tb04534.x. [DOI] [PubMed] [Google Scholar]
- 10.Faghihi G, Mokhtari F, Fard NM, Motamedi N, Hosseini SM. Comparing the efficacy of low dose and conventional dose of oral isotretinoin in treatment of moderate and severe acne vulgaris. J Res Pharm Pract. 2017;6:233–8. doi: 10.4103/jrpp.JRPP_17_30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mokhtari F, Faghihi G, Basiri A, Farhadi S, Nilforoushzadeh M, Behfar S. Comparison effect of azithromycin gel 2% with clindamycin gel 1% in patients with acne. Adv Biomed Res. 2016;5:72. doi: 10.4103/2277-9175.180641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kosmadaki M, Katsambas A. Topical treatments for acne. Clin Dermatol. 2017;35:173–8. doi: 10.1016/j.clindermatol.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 13.Goyal G, Garg T, Malik B, Chauhan G, Rath G, Goyal AK. Development and characterization of niosomal gel for topical delivery of benzoyl peroxide. Drug Deliv. 2015;22:1027–42. doi: 10.3109/10717544.2013.855277. [DOI] [PubMed] [Google Scholar]
- 14.Irby CE, Yentzer BA, Feldman SR. A review of adapalene in the treatment of acne vulgaris. J Adolesc Health. 2008;43:421–4. doi: 10.1016/j.jadohealth.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Piérard GE, Piérard-Franchimont C, Paquet P, Quatresooz P. Spotlight on adapalene. Expert Opin Drug Metab Toxicol. 2009;5:1565–75. doi: 10.1517/17425250903386269. [DOI] [PubMed] [Google Scholar]
- 16.Kumaresan M, Srinivas CR. Efficacy of IPL in treatment of acne vulgaris: Comparison of single- and burst-pulse mode in IPL. Indian J Dermatol. 2010;55:370–2. doi: 10.4103/0019-5154.74550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barakat MT, Moftah NH, El Khayyat MA, Abdelhakim ZA. Significant reduction of inflammation and sebaceous glands size in acne vulgaris lesions after intense pulsed light treatment. Dermatol Ther. 2017;30:1–5. doi: 10.1111/dth.12418. p.e12418. [DOI] [PubMed] [Google Scholar]
- 18.Puttaiah M, Jartarkar SR. Intense pulsed light: A promising therapy in treatment of acne vulgaris. Our Dermatol Online. 2017;8:6. [Google Scholar]
- 19.Mokhtari F, Gholami M, Siadat AH, Jafari-Koshki T, Faghihi G, Nilforoushzadeh MA, et al. Efficacy of intense-pulsed light therapy with topical benzoyl peroxide 5% versus benzoyl peroxide 5% alone in mild-to-moderate acne vulgaris: A randomized controlled trial. J Res Pharm Pract. 2017;6:199–205. doi: 10.4103/jrpp.JRPP_17_29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barikbin B, Ayatollahi A, Younespour S, Hejazi S. Evaluation of efficacy of Intense Pulsed Light (IPL) system in the treatment of facial acne vulgaris: Comparison of different pulse durations; a pilot Study. J Lasers Med Sci. 2011;2:67. [Google Scholar]
- 21.Faghihi G, Vali A, Asilian A, Radan MR, Esteki H, Elahidoost M. Comparative efficacy of filtered blue light (emitted from sunlight) and topical erythromycin solution in acne treatment: A randomized controlled clinical trial. J Pak Assoc Dermatol. 2016;21:179–84. [Google Scholar]
- 22.Rojanamatin J, Choawawanich P. Treatment of inflammatory facial acne vulgaris with intense pulsed light and short contact of topical 5-aminolevulinic acid: A pilot study. Dermatol Surg. 2006;32:991–6. doi: 10.1111/j.1524-4725.2006.32221.x. [DOI] [PubMed] [Google Scholar]
- 23.Santos MA, Belo VG, Santos G. Effectiveness of photodynamic therapy with topical 5-aminolevulinic acid and intense pulsed light versus intense pulsed light alone in the treatment of acne vulgaris: Comparative study. Dermatol Surg. 2005;31:910–5. doi: 10.1097/00042728-200508000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Gold MH, Bradshaw VL, Boring MM, Bridges TM, Biron JA, Carter LN. The use of a novel intense pulsed light and heat source and ALA-PDT in the treatment of moderate to severe inflammatory acne vulgaris. J Drugs Dermatol. 2004;3:S15–9. [PubMed] [Google Scholar]
- 25.Yeung CK, Shek SY, Bjerring P, Yu CS, Kono T, Chan HH. A comparative study of intense pulsed light alone and its combination with photodynamic therapy for the treatment of facial acne in Asian skin. Lasers Surg Med. 2007;39:1–6. doi: 10.1002/lsm.20469. [DOI] [PubMed] [Google Scholar]
- 26.Chlebus E, Serafin M, Chlebus M. Is maintenance treatment in adult acne important? Benefits from maintenance therapy with adapalene, and low doses of alpha and beta hydroxy acids. J Dermatolog Treat. 2019;30:568–71. doi: 10.1080/09546634.2018.1484874. [DOI] [PubMed] [Google Scholar]
- 27.Thiboutot DM, Weiss J, Bucko A, Eichenfield L, Jones T, Clark S, et al. Adapalene-benzoyl peroxide, a fixed-dose combination for the treatment of acne vulgaris: Results of a multicenter, randomized double-blind, controlled study. J Am Acad Dermatol. 2007;57:791–9. doi: 10.1016/j.jaad.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 28.Fulton JE, Jr, Farzad-Bakshandeh A, Bradley S. Studies on the mechanism of action to topical benzoyl peroxide and Vitamin A acid in acne vulgaris. J Cutan Pathol. 1974;1:191–200. doi: 10.1111/j.1600-0560.1974.tb00628.x. [DOI] [PubMed] [Google Scholar]
- 29.Bassett IB, Pannowitz DL, Barnetson RS. A comparative study of tea-tree oil versus benzoylperoxide in the treatment of acne. Med J Aust. 1990;153:455–8. doi: 10.5694/j.1326-5377.1990.tb126150.x. [DOI] [PubMed] [Google Scholar]
- 30.Iftikhar U, Aman S, Nadeem M, Kazmi AH. A comparison of efficacy and safety of topical 0.1% adapalene and 4% benzoyl peroxide in the treatment of mild to moderate acne vulgaris. J Pak Assoc Dermatol. 2016;19:141–5. [Google Scholar]
- 31.Penna P, Meckfessel MH, Preston N. Fixed-dose combination gel of adapalene and benzoyl peroxide plus doxycycline 100 mg versus oral isotretinoin for the treatment of severe acne: Efficacy and cost analysis. Am Health Drug Benefits. 2014;7:37–45. [PMC free article] [PubMed] [Google Scholar]
- 32.Sittart JA, Costa AD, Mulinari-Brenner F, Follador I, Azulay-Abulafia L, Castro LC. Multicenter study for efficacy and safety evaluation of a fixeddose combination gel with adapalen 0.1% and benzoyl peroxide 2.5% (Epiduo® for the treatment of acne vulgaris in Brazilian population. An Bras Dermatol. 2015;90:1–16. doi: 10.1590/abd1806-4841.20153969. [DOI] [PMC free article] [PubMed] [Google Scholar]