Abstract
Background: Opioid misuse is a leading health care concern within the United States. In many cases, opioid misuse and opioid use disorder are associated with pain, a secondary health condition affecting individuals with spinal cord injury (SCI). Further, substance use is a known risk factor for SCI, resulting in the potential for a substance-related risk trajectory running from pre- to post-SCI. However, little research has examined substance use prior to SCI since the opioid epidemic began, and so the relative risk of opioids to patients with SCI is unclear. Objective: To determine whether individuals with SCI tested positive for substance use at the time of injury and identify the primary substances used at the time of injury. Methods: This study retrospectively reviewed all medical charts of individuals ages 18 and older who had sustained an SCI during an identified 18-month period and received medical care at a selected level 1 trauma center in the Midwest. Results: Data revealed an 80% combined positive toxicology and/or self-report of substance use immediately prior to the onset of the SCI. Twenty-five percent of males were positive for more than one substance at time of injury. Substances used prior to injury, listed most to least prevalent, were opioids (37.5%), alcohol (25%), marijuana (25%), methamphetamines (12.5%), benzodiazepines (12.5%), followed by cocaine (6.25%) and synthetic cathinone (6.25%). Conclusion: Although opioids were the most common substance used prior to SCI, none of the individuals positive for opioids at the time of injury were identified by the reviewing medical professional as having pain as a secondary health condition either prior to or after injury. However, pain is commonly listed as the primary health concern among individuals living with SCI, and the possibility of opioid use prior to injury likely warrants pain management planning that includes careful pharmacological and nonpharmacological interventions.
Keywords: pain, spinal cord injury, substance use
Substance use is among a small group of behaviors that can function both as a precipitating factor and as a source of postinjury difficulty for adults with spinal cord injury (SCI). As such, it occupies a unique place in SCI rehabilitation research, a field that focuses not only on the SCI itself but also on the factors leading up to the injury and the postinjury period.1–6 Although multiple studies have examined the relationship of substance use and SCI in both of these contexts, in the United States the national substance use environment has rapidly evolved to become substantially different than in the past. In particular, opioid use, including prescription pain medication, has become a leading health care concern.7,8 Jeff Sessions, US Attorney General, oversaw a formal federal declaration of opioid abuse as a national crisis in 2018.9 This emerging epidemic has the potential to alter established knowledge about the intersection of SCI and substance use.
Substance Use Prior to SCI
Studies have shown that substance use prior to injury is related to the likelihood of acquiring an SCI,10–12 with one recent study finding that up to 34% of SCI patients are intoxicated at the time of the injury.12 Historically, alcohol has been identified as the primary substance associated with SCI incidence,13 although other studies have argued that the exact distributive prevalence of substance use at the time of SCI has not been definitively determined.13 Research has not yet begun to unpack the substance-derived etiology of SCI in the current national substance use climate. Furthermore, such analysis is complicated by a lack of uniformity in how and whether patients are assessed for substance use at the time of injury either using objective toxicology measures or self-report items.14
Substance Use After SCI
Researchers have found that substance use is a common factor among people adjusting to life after SCI,15 along with other factors such as religion, seeking emotional support, recreational pursuits, or positive reframing.16 Individuals living with an SCI report more pain and lower satisfaction of life than other individuals, and many also experience issues with alcohol and/or illicit drug use or prescription drug use for nonmedical reasons.13 In such individuals, secondary health conditions such as pain can become complex and influence daily life,17 including their ability to actively and meaningfully participate in desired activities.1,18 Further, post-SCI pain is often inadequately controlled, and individuals living with SCI perceive opioids to be the most effective pharmacological agent that can be prescribed to reduce pain.19 At the same time, individuals using such agents actually report significantly more intense pain.19 Chronic noncancer pain is a well-established correlate of opioid use disorder, with one study observing a 50% increase in the likelihood of such a disorder in individuals being treated for chronic noncancer pain with opioids.20
Continued Research
There is likely a synergistic risk among individuals living with SCI in cases where chronic postinjury pain is coupled with an extant substance use history.21–23 Given that (a) chronic pain is a common secondary health condition among individuals living with SCI, (b) chronic noncancer pain is often treated with opioids and is associated with increased likelihood of development of opioid use disorder, and (c) substance intoxication has been associated with SCI incidence, this is an area of research that merits renewed attention.
This pilot study was designed to provide an up-to-date, preliminary understanding of substance use at the time of SCI in the modern US substance use climate. Researchers examined the prevalence of substance use prior to SCI using an 18-month comprehensive chart pull (2016 to 2018) at a level 1 trauma center in the Midwest region of the United States. All patients' charts with documented Cervical (C)2-C7 (International Classification of Disease [ICD-10] code S14, injury of nerves and spinal cord at neck level), Thoracic (T)1-T12 (ICD-10 code S24, injury of nerves and spinal cord at thorax level), and Lumbar (L)1-L5 (ICD-10 code S34, injury of lumbar and sacral spinal cord and nerves at abdomen, lower back, and pelvis level) were extracted for analysis of substance use prior to injury. This study was designed to support continued exploration and dialogue regarding substance use at SCI incidence and the management of secondary chronic pain in SCI patients with a history of substance use.
Methods
The planned research protocol called for a simple random sample of 50 adult (age 18+) patient charts with C2-7, T1-12, and L1-5 injuries (S14, S24, or S34 ICD-10 codes) from a mid-size safety-net hospital located in a Midwest metropolitan city. This hospital was one of only three level 1 trauma centers in the state that provides care to adult patients, where a level 1 designation represents the most acute level of patient care. During the abstraction period, researchers learned that only 20 patients met sampling criteria (as described subsequently), and records were not accessible prior to October 1, 2016 (implementation of the current medical record system), so all eligible and available patient charts were used. Researchers developed an abstraction sheet and key prior to data access to provide necessary guidelines regarding the data. The key included instructions for coding age, sex, injury information, toxicology screens, self-report of substance use, categories of substances used, employment status (full-time 32 hours or more, part-time less than 32 hours), education level, relationship status, military service, and any nonpharmacological pain treatment methods (Table 1). The data were analyzed to determine whether substance use had occurred 24 hours prior to injury and, if so, what types of substances had been used. Due to the small population of eligible individuals with SCI, interpretive analyses were exclusively descriptive.
Table 1.
Participant demographics (N = 20)
| Demographics | Mean (SD) or percent |
|---|---|
| Age, years | 45.05 (13.843) |
| 18–28 | 10% |
| 29–38 | 30% |
| 39–48 | 10% |
| 49–58 | 40% |
| 59–68 | 5% |
| 69–78 | 5% |
| Sex | |
| Male/Female | 85%/15% |
| Employment status | |
| Unemployed | 80% |
| Full time (≥32 hours) | 10% |
| Part time (<32 hours) | 10% |
| Cause of injury | |
| Falls | 45% |
| Violence | 25% |
| Vehicular | 25% |
| Other | 5% |
All adult patient charts in the hospital medical record system (emergency department admissions as well as inpatient admissions that occurred due to patient transferring institutions) from October 1, 2016 to March 7, 2018 with newly onset C2-7, T1-12, and L1-5 injuries (S14, S24, and S34 ICD-10 codes) were reviewed for eligibility. A medical professional (physician hospitalist) worked with his staff to locate and pull the charts for the study. That individual removed all patient identifiers immediately subsequent to sampling and provided de-identified data to the principal investigator. All aspects of the research protocol were approved by the Institutional Review Board at the researchers' institution.
All available charts were included in the preliminary screening. Charts that were omitted included those for individuals under the age of 18; this resulted in exclusion of infants with brachial plexus injuries, which typically are coded as S14, as well as individuals who were admitted for an issue unrelated to SCI but who had previously experienced an SCI (so an eligible code was still used in the record).
Using the abstraction guide and key, the reviewer inspected each chart's ICD-10 codes, progress notes, admission and discharge paperwork, and laboratory results. The medical billing codes were the primary source of data. If requested information was not noted in the medical codes, the reviewer obtained the information from looking at the qualitative physician notes and other indicated sources of information. All data were protected in a Box Health account associated with the researcher's university, although no patient identifiers were included in the dataset.
Descriptive statistical analyses were performed using Statistical Package for the Social Sciences (SPSS v.25).
Results
A retrospective chart review was completed with a total of 20 participant records, representing 17 males and 3 females between the ages of 27 and 76 (M = 45.05, SD = 13.843). Data indicated that 45% of SCIs were due to a fall (compared with the national average of 28.3%), 25% were due to violence (compared with the national average of 14.6%), 25% were due to vehicular incidents (compared with the national average of 39.2%), and 5% were attributable to other causes (compared with the national average of 9.7%).24 The rate of unemployment prior to injury was 80% for the total population sampled and 81.25% for individuals with substance use reported immediately prior to injury.
Data revealed an 80% positive toxicology screen (85%) or self-report (15%) of substance use immediately prior to the onset of the SCI. In addition, 25% of males with positive toxicology screen tested positive for more than one substance at time of injury. The following substances were identified as having been used prior to SCI, listed most to least prevalent: opioids (37.5%, 6 charts), alcohol (25%, 4 charts), marijuana (25%, 4 charts), methamphetamines (12.5%, 2 charts), benzodiazepines (12.5%, 2 charts), cocaine (6.25%, 1 chart), and synthetic cathinone (6.25%, 1 chart).
Discussion
This study found that the majority (80%) of adult patients seen for SCI at one of the three adult-serving level 1 trauma centers in a Midwestern state had used one or more substances, including opioids, alcohol, marijuana, methamphetamines, benzodiazepines, cocaine, and synthetic cathinone, immediately prior to SCI onset. Although previous research indicated that alcohol was the most common substance used prior to SCI, these data identified opioids as the most common substance used prior to SCI, followed by alcohol.10,25 Given the noted changes in the US substance use climate – specifically the opioid epidemic – since the prior studies were conducted, this finding stands to reason.
Interestingly, none of the individuals who were positive for opioids at the time of injury were identified by the medical professional as having pain as a secondary health condition either prior to or immediately after the SCI. Since pain has been identified as one of the secondary health conditions that prevents individuals with SCI in participating in their social interaction,1 it would be surprising if these patients did not report secondary pain in future visits, although this is speculative given the limits of the current dataset. As previously described, this pain, if and when it manifests, is also likely to be poorly controlled, with a preferred patient solution being opioids.19 The state in which the study took place is also one of the 13 states with the highest prescription rates for opioids.26 For the six individuals using opioids immediately prior to SCI and the additional patients who used other substances (especially benzodiazepines), there is likely an increased risk of substance dependence if pain is managed with opioid prescription. Thus, it seems important that SCI patients, especially those with substance use prior to onset, receive a thorough medical history review prior to being transferred to rehabilitation to avert potentially avoidable iatrogenic substance-related outcomes from treatment.
Figure 1.
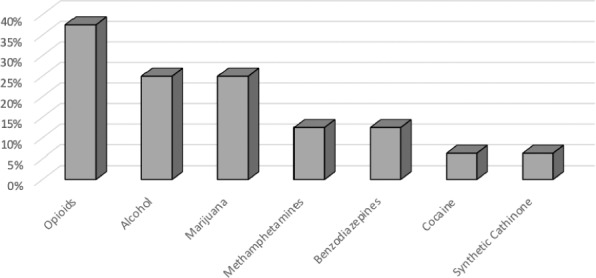
Prevalence of substance use prior to onset of spinal cord injury (N = 20).
Therefore, it is likely the case that a thorough assessment of risk for substance use should occur immediately upon admission for acute care for the sustained SCI. The assessment should include the individual's current and past substance use along with family history of substance use in combination with a standard toxicological panel. The individual should be asked to disclose all current and past prescribed medications taken as well as any medications they have acquired without a prescription.27
Limitations
The findings in this article should be interpreted with caution due to a few limitations. First, SCI is not a common injury, so the sample size for this study, despite being a comprehensive chart pull from one of only three level 1 trauma centers serving adults in the state, is small. This means that data were especially subject to potential bias from the specific characteristics of the study hospital (eg, 4 in 5 patients in the study sample were unemployed, which is higher than the national average). Although the data produced in this study are still important and useful, care should be taken not to overgeneralize the findings. Second, the assessment of substances was relatively comprehensive, using both toxicology data and review of all qualitative notes for patient self-report, but the possibility still remains that the data are not fully accurate.
Implications for future research
This study provides a starting point for understanding substance use and the onset of SCI. Additional research is needed, such as replication of the study with a national sample, to determine more definitively whether opioids are overrepresented relative to other substances immediately prior to SCI. Research exploring how to effectively facilitate communication between emergency rooms and general health practitioners regarding risk factors for potential misuse or dependence is also a reasonable next step. If additional research indicates that opioid misuse or dependence are common among individuals prior to SCI, then it should be seen as especially important to research nonpharmaceutical pain control methods for people living with SCI. Such work would potentially prepare care providers to provide referrals to the appropriate providers to improve quality of care of the individual leading into rehabilitation and community reintegration.
Acknowledgments
The authors report no conflicts of interest. This research was unfunded.
REFERENCES
- 1.Piatt JA, Nagata S, Zahl M, Li J, Rosenbluth JP. Problematic secondary health conditions among adults with spinal cord injury and its impact on social participation and daily life [published online ahead of print December 15, 2015] J Spinal Cord Med. doi: 10.1080/10790268.2015.1123845. doi: 10.1080/10790268.2015.1123845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piatt J, Compton DM, Sara Wells M, Bennett JL. Interventions that effect active living among individuals with spinal cord injury. Therapeut Recreation J. 2012;46(1):9. [Google Scholar]
- 3.Sherman JE, DeVinney DJ, Sperling KB. Social support and adjustment after spinal cord injury: Influence of past peer-mentoring experiences and current live-in partner. Rehabil Psychol. 2004;49(2):140. [Google Scholar]
- 4.van Diemen T, Crul T, van Nes I, SELF-SCI Group. Geertzen JH, Post MW. Associations between self-efficacy and secondary health conditions in people living with spinal cord injury: A systematic review and meta-analysis. Arch Phys Med Rehabil. 2017;98(12):2566–2577. doi: 10.1016/j.apmr.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 5.Wyndaele M, Wyndaele JJ. Incidence, prevalence and epidemiology of spinal cord injury: What learns a worldwide literature survey? Spinal Cord. 2006;44(9):523. doi: 10.1038/sj.sc.3101893. [DOI] [PubMed] [Google Scholar]
- 6.DeVivo MJ. Epidemiology of traumatic spinal cord injury: Trends and future implications. Spinal Cord. 2012;50(5):365. doi: 10.1038/sc.2011.178. [DOI] [PubMed] [Google Scholar]
- 7.Kolodny A, Courtwright DT, Hwang CS et al. The prescription opioid and heroin crisis: A public health approach to an epidemic of addiction. Ann Rev Publ Health. 2015;36:559–574. doi: 10.1146/annurev-publhealth-031914-122957. [DOI] [PubMed] [Google Scholar]
- 8.Compton WM, Volkow ND. Major increases in opioid analgesic abuse in the United States: Concerns and strategies. Drug Alcohol Dependence. 2006;81(2):103–107. doi: 10.1016/j.drugalcdep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 9.The White House, Department of Justice Justice Department to File Statement of Interest in Opioid Case. 2018 Feb 27; https://www.justice.gov/opa/pr/justice-department-file-statement-interest-opioid-case.
- 10.Kolakowsky-Hayner SA, Gourley EV, 3rd, Kreutzer JS, Marwitz JH, Cifu DX, Mckinley WO. Pre-injury substance abuse among persons with brain injury and persons with spinal cord injury. Brain Inj. 1999;13(8):571–581. doi: 10.1080/026990599121313. [DOI] [PubMed] [Google Scholar]
- 11.Davis JF, Cao Y, Krause JS. Changes in alcohol use after the onset of spinal cord injury. J Spinal Cord Med. 2018;41(2):230–237. doi: 10.1080/10790268.2017.1319996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crutcher CL, Veith J, Tender GC. Alcohol intoxication and traumatic spinal cord injury: Basic and clinical science. In: Watson R, Zibadi S, editors. Addictive Substances and Neurological Disease. London: Academic Press; 2017. pp. 39–46. [Google Scholar]
- 13.Tate DG, Forchheimer MB, Krause JS, Meade MA, Bombardier CH. Patterns of alcohol and substance use and abuse in persons with spinal cord injury: Risk factors and correlates. Arch Phys Med Rehabil. 2004;85(11):1837–1847. doi: 10.1016/j.apmr.2004.02.022. [DOI] [PubMed] [Google Scholar]
- 14.Stroud MW, Bombardier CH, Dyer JR, Rimmele CT, Esselman PC. Preinjury alcohol and drug use among persons with spinal cord injury: Implications for rehabilitation. J Spinal Cord Med. 2011;34(5):461–472. doi: 10.1179/2045772311Y.0000000033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kolakowsky-Hayner SA, Gourley EV, Kreutzer JS, Marwitz JH, Mead MA, Cifu DX. Post-injury substance abuse among persons with brain injury and personal with spinal cord injury. Brain Inj. 2002;16(7):583–592. doi: 10.1080/02699050110119475. [DOI] [PubMed] [Google Scholar]
- 16.Anderson CJ, Vogel LC, Chlan KM, Betz RR. Coping with spinal cord injury: Strategies used by adults who sustained their injuries as children or adolescents. J Spinal Cord Med. 2008;31(3):290–296. doi: 10.1080/10790268.2008.11760725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cao Y, Walker EA, Krause JS. Environmental barriers and subjective health among people with chronic spinal cord injury: A cohort study. J Spinal Cord Med. 2015;38(4):526–531. doi: 10.1179/2045772314Y.0000000275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization International Perspectives on Spinal Cord Injury. 2013 http://apps.who.int/iris/bitstream/handle/10665/94190/9789241564663_eng.pdf;jsessionid=9A3B79C174B90F9F3A8060769227E30B?sequence=1.
- 19.Widerström-Noga EG, Turk DC. Types and effectiveness of treatments used by people with chronic pain associated with spinal cord injuries: Influence of pain and psychosocial characteristics. Spinal Cord. 2003;41(11):600. doi: 10.1038/sj.sc.3101511. [DOI] [PubMed] [Google Scholar]
- 20.Højsted J, Nielsen PR, Eriksen J, Hansen OB, Sjøgren P. Breakthrough pain in opioid treated chronic non malignant pain patients referred to a multidisciplinary pain centre: A preliminary study. Acta Anaesthesiologica Scand. 2006;50(10):1290–1296. doi: 10.1111/j.1399-6576.2006.01154.x. [DOI] [PubMed] [Google Scholar]
- 21.Rivers CS, Fallah N, Noonan VK et al. Health conditions: Effect on function, health-related quality of life, and life satisfaction after traumatic spinal cord injury. A prospective observational registry cohort study. Arch Phys Med Rehabil. 2018;99(3):443–451. doi: 10.1016/j.apmr.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 22.Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. New Engl J Med. 2016;374(2):154–163. doi: 10.1056/NEJMra1508490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.United States Department of Health and Human Services Substance Abuse and Mental Health Services Administration. Center for Behavioral Health Statistics and Quality. 2017 National Survey on Drug Use and Health. https://www.samhsa.gov/data/report/2017-nsduh-annual-national-report.
- 24.National Spinal Cord Injury Statistical Center Facts and Figures at a Glance. Birmingham, AL: University of Alabama at Birmingham; 2017. [Google Scholar]
- 25.Garrison A, Glifford K, Gleason S, Tun C, Brown R, Garshick E. Alcohol use associated with cervical spinal cord injury. J Spinal Cord Med. 2004;27(2):111–115. doi: 10.1080/10790268.2004.11753740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Center for Disease Control and Prevention 2017 Vital Statistics Rapid Release. Provisional Drug Overdose Death Counts. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm.
- 27.Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: A rational approach to the treatment of chronic pain. Pain Med. 2005;6:107–112. doi: 10.1111/j.1526-4637.2005.05031.x. [DOI] [PubMed] [Google Scholar]


