Abstract
Acupuncture is a core discipline in traditional Chinese medicine (TCM) and has been practised in China for centuries. In traditional acupuncture, pulse palpation is an important clinical diagnostic technique that guides practitioners in their treatment strategies as they evaluate the effectiveness of the treatment. This paper provides the findings of our investigation of acupuncture's effect on specific radial pulse spectral energies in 41 individuals with lower back pain (LBP), in response to a single acupuncture treatment delivered bilaterally at acupoints BL23, BL25, and BL40. Baseline assessments (vital signs and radial pulse diagnoses), primary outcome measures (radial pulse diagnoses), and secondary outcome measures (the Faces Pain Scale-Revised (FPS-R) and fingertip-to-floor (FTF) tests) were performed at specified intervals before and after the intervention. Our study provides novel information about the effects of acupuncture on the radial pulse spectral energy in individuals with different types of LBP. Our findings suggest that the right Chi pulse is an effective indicator to assess the effects of acupuncture in individuals with fixed, distended, or sharp pain, whereas the left Guan pulse is a potentially useful diagnostic technique to determine acupuncture's effects in individuals with dull, aching pain. The acupoints BL23, BL25, and BL40 provide effective treatment for LBP. Study participants with dull, aching pain had a significant improvement in their lumbar ranges of motion, and their pain rating scores were markedly decreased after acupuncture treatment.
1. Introduction
Acupuncture is a core discipline in traditional Chinese medicine (TCM) and has been practised in China for centuries. In traditional acupuncture, pulse palpation is an important clinical diagnostic technique that guides acupuncture practitioners in their treatment strategy and evaluates the effectiveness of the treatment [1]. The Ling Shu text in Chapter 1 of Huang Di Nei Jing advises that “one must first diagnose the pulse before acupuncture, treat the disease only after perceiving the severity or ease of the Qi” [2].
Conventionally, TCM practitioners palpate the radial pulse with the second, third, and fourth fingers individually or simultaneously, at the three regions of each wrist. These regions, representing the Cun (distal), Guan (middle), and Chi (proximal) pulses (the Pin Yin pulses named Cun, Guan, and Chi are adopted in this article; they are also translated as Chun, Guan, and Chi pulses in some references), correspond to the respective visceral organs in TCM: right Cun (lung and chest), right Guan (stomach and spleen), right Chi (kidney and lower abdomen), left Cun (heart), left Guan (liver and gallbladder), and left Chi (kidney and lower abdomen) [3].
Each radial pulse profile has unique characteristics: depth, rate, waveform, density, and intensity. The ancient texts describe 28 common pulse profiles observed in clinical practice [4]. These are categorised by (1) depth: floating, sunken, Chi (proximal), or Cun (distal); (2) rate: slow, rapid, surging, or intermittent; (3) waveform: long, short, narrow, broad, thick, thin, rough, fine, firm, or gentle; and (4) intensity and density: converging, dispersing, extending, shortening, moving forward, moving backward, moving upward, or moving downward [3]. Each pulse profile provides information about the physiological conditions or disorders in the human body [5]. For example, Jeon et al. studied pulse wave variation during the menstrual cycle and reported that the pulse appeared to be either string-like or slippery and rapid [6].
The accuracy of pulse diagnoses depends on the finger sensitivity of TCM practitioners and their experiential perception. Inconsistencies in diagnoses and treatments can result from subjective assessments by TCM practitioners [7, 8]. Since the 1950s, quantitative analyses of pulse profiles have been studied by researchers [1]. The development of the pulse sphygmograph, providing quantitative and graphical presentations of the radial pulse, is an important milestone in transforming conventional pulse diagnoses into scientific assessments.
This paper provides the findings of our quasi-experimental investigation on the effects of acupuncture on the specific radial pulse spectral energy (SE) in participants with lower back pain (LBP). Using the pulse sphygmograph, we investigated high-frequency SE (SE13–50 Hz) in the radial pulse during the pre- and postintervention stages. An objective assessment of the ranges of motion using the fingertip-to-floor (FTF) test and a subjective assessment of the Faces Pain Scale-Revised (FPS-R) test were included to determine the effectiveness of acupuncture in different types of LBP. In addition, the Health Status Questionnaire, the Oswestry Disability Index (ODI), and the Constitution in Chinese Medicine Questionnaire (CCMQ) were used to determine the overall health status of each study participant. Full details of the methodologies are described in the study protocol “An investigation into the effects of acupuncture on radial pressure pulse waves in patients with low back pain: a protocol for a quasi-experimental study” [1].
2. Materials and Methods
2.1. Study Setting and Design
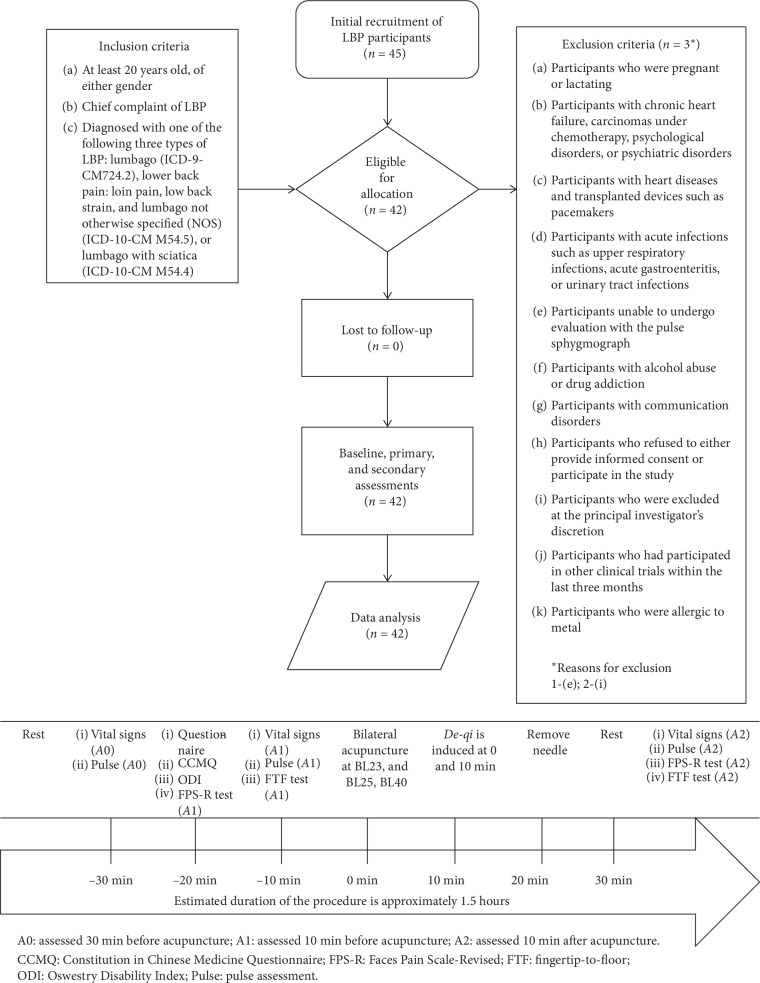
The study was conducted in the Acupuncture Department of the China Medical University Hospital (CMUH), Taichung, Taiwan, from April 2018 through March 2019. The Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) 2013 checklist was used to guide this single-arm, nonrandomised, quasi-experimental study. We adopted the Transparent Reporting of Evaluations with Nonrandomised Designs (TREND) guideline to report the findings. Figure 1 provides details of the study flow diagram and study procedure.
Figure 1.
The study flow diagram and study procedure. All enrolled patients underwent a baseline assessment of the radial pulse spectral energy (SE) and the vital signs and the Faces Pain Scale-Revised (FPS-R) test. The study applied the Health Status Questionnaire, the Oswestry Disability Index (ODI), and the Constitution in Chinese Medicine Questionnaire (CCMQ). The SE, vital signs, and fingertip-to-floor (FTF) test were assessed during the pre- and postinterventions.
2.2. Study Participants
Recruitment into the study was advertised on the hospital's regular internal circulars, bulletin boards, and websites. During the recruitment phase, 42 eligible individuals aged at least 20 years with a primary complaint of LBP, based on the predefined inclusion and exclusion criteria, were invited to participate in the study by the chief attending physician. Informed consent including the study aims, description of the procedures, and potential risks was approved by the CMUH Research Ethics Committee (REC) and was communicated to each individual, who provided written informed consent before the procedure.
2.3. Interventions
Each participant received a single acupuncture treatment in this research study. During the procedure, the participant rested in a prone position while acupuncture needles were inserted bilaterally at acupoints BL23 (Shenshu), BL25 (Dachangshu), and BL40 (Weizhong) as defined in WHO Standard Acupuncture Point Locations in the Western Pacific Region [9]. These locations, at the Bladder meridian of the lower back region and the transverse crease of the popliteal fossa, are common proximal and distal acupoints used in the treatment of LBP. The Ling Shu text in Chapter 51 of Huang Di Nei Jing states that the Shenshu (BL23) acupoint is the Back-Shu point of the kidneys, with functions including tonifying the kidneys and fortifying Yang, nourishing kidney Yin, firming kidney Qi, and strengthening the lumbar regions. The Dachangshu (BL25) acupoint is the Back-Shu point of the large intestine, which strengthens the lumbar regions and legs. The Weizhong (BL40) acupoint is one of the four command acupoints, which indicates “look for the Weizhong (BL40) acupoint to relieve disorders of the waist and back” [10].
The acupuncture needles were inserted within the defined safe range of 12.5–25 mm for BL25 and BL40, and within 12.5–40 mm for BL23 [11]. The needles were retained for 20 min after the needling sensation (De-qi) was manually stimulated with sufficient stimulus intensity during insertion and subsequently repeated 10 min after the insertion. A similar stimulus intensity was applied by the same acupuncturist to all study participants without supplementing or draining techniques [12]. In acupuncture practice, supplementing and draining techniques are generally applied to increase Qi in the deficiency state and decrease Qi in the repletion state after the patient experiences the De-qi sensation [13]. In our study, we avoided using these techniques, which may have resulted in confounding bias in the results.
2.4. Objectives and Hypothesis
Controversial explanations of the relationship between bodily organs and Chi pulse positions are documented in various ancient texts. For instance, the Suwen text in Chapter 17 of Huang Di Nei Jing states that “both Chi pulse positions correspond with the kidney and abdomen” [3, 14]; Nan Jing: The Classic of Difficult Issues documents that the right Chi corresponds with the Mingmen (Gate of Vitality); Jing Yue Quan Shu (Complete Works of Jingyue), published in the Ming dynasty, suggests that the left Chi pulse corresponds with the bladder and large intestine, while the right Chi pulse corresponds with the Triple Energiser, Mingmen, and small intestine. Based on modern studies, the left Chi pulse corresponds with the kidney Yin and the right Chi pulse corresponds with the kidney Qi and Mingmen [3]. We therefore selected LBP as the condition for clarifying the relationship of the kidneys and Chi pulse positions, and for evaluating the effectiveness of the selected acupoints in acupuncture interventions. LBP is a common condition, ranking second amongst all musculoskeletal and connective tissue disorders affecting individuals presenting to Taiwanese TCM outpatient clinics in 2018 [15]. The relationship of the lower back and kidney is explained in the Suwen text in Chapter 17 of Huang Di Nei Jing, which states that the lower back is the “house” of the kidneys [14].
Our preliminary hypotheses were therefore the following: (1) acupuncture significantly influences the Chi pulse in participants with LBP, so it is an effective indicator for assessing outcomes of acupuncture intervention and (2) reduced pain intensity and improved physical movement are reflected in the FPS-R and FTF tests after acupuncture intervention.
2.5. Outcomes
Baseline assessments included vital signs (systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate, and body temperature), the Health Status Questionnaire, the ODI, and the CCMQ, as described in the study protocol.
The primary outcome measure was the effect of acupuncture on radial pulse patterns in individuals with LBP. The secondary outcome measures determined the effectiveness of the acupuncture treatments using the selected acupoints.
The primary outcome measure in this study was the effect of high-frequency SE (SE13–50 Hz) on the radial pulse, which was assessed by the pulse sphygmograph at specific intervals during the procedure. Figure 2 illustrates the assessment of a single study participant using the pulse sphygmograph (Pen Pulse Analysis System Model PPAS-96, Asia Plus Biotech Co., Taiwan). We selected SE13–50 Hz as our primary outcome measure based on the study by Wei et al., which reported large variations in SE above 10 Hz in individuals with various diseases or mental stress [16]. We therefore anticipated significant changes would be found in SE values exceeding 10 Hz.
Figure 2.
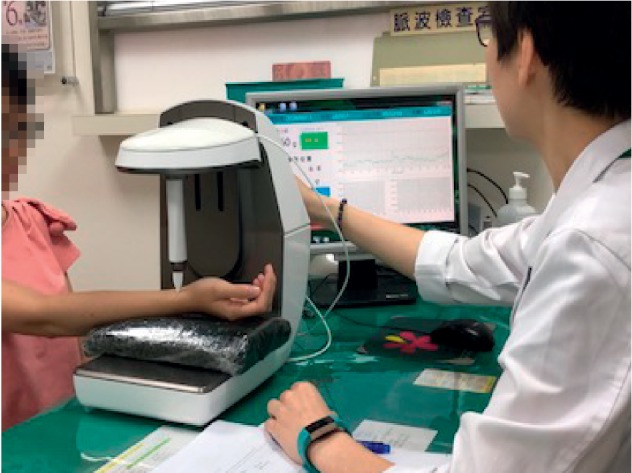
Pulse assessment of a study participant. The high-precision pressure sensor was positioned on each marked position of the Cun, Guan, and Chi pulses of the wrist. The biological signal of the radial pulse was then digitised to provide graphical analysis. The best spectrogram, which displayed the greatest amplitude, was then recorded.
The secondary outcome measures used the FTF and FPS-R tests to evaluate the efficacy of the acupuncture treatments. The FTF test evaluates flexibility in the flexion ranges of motion, while the FPS-R test evaluates pain intensity. Both tests were administered during the pre- and postintervention assessments.
In this study, vital sign assessment and pulse assessment were performed during each of the baseline (A0), preintervention (A1), and postintervention (A2) phases, respectively. The baseline assessments were used as a control to compare the stability of these parameters at the preintervention stage. Each participant was assigned an identification code to protect the privacy of their personal details. Raw data were consolidated in Microsoft Excel 2016 and pivoted to analyse the results.
2.6. Design and Mechanism of the Pulse Sphygmograph
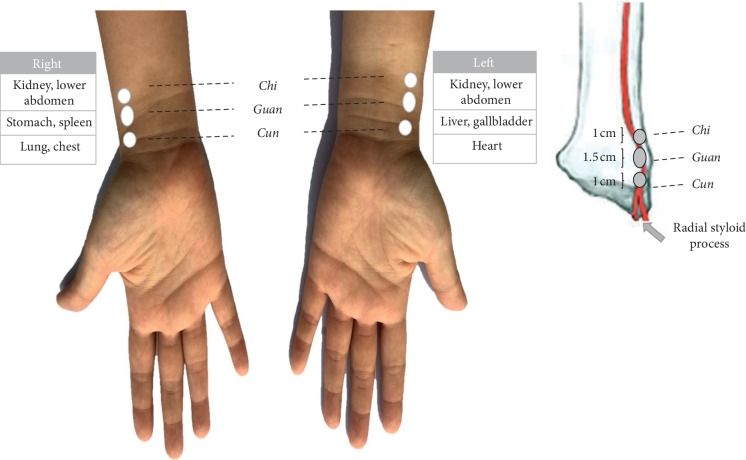
The pulse sphygmograph (PPAS-96) is a noninvasive diagnostic device consisting of a detachable, high-precision pulse detection sensor pen with a stable Y-axial movable framework. It is connected to a pulse signal analyser containing a filter, an amplifier, and a signal-recording card. The device has a sampling rate of 3,000 Hz and frequency response of 0.1–50 Hz. The input voltage uses USB_DC5V. The physiological signals of the radial pulse are digitalised and processed through the fast Fourier transform. The digital output presented in the software application includes a real-time display of the pulse spectrogram and time- and frequency-domain analyses. PPAS-96 is the enhanced model of the Huang-T1 Pulse Sphygmograph [1]. Huang-T1 Pulse Sphygmograph has been used in studies that have investigated the effects of acupuncture in patients with dyspepsia [12]; the influence of radial pulse and heart rate variability (HRV) in heat- and cold-stressed humans [17]; and a comparison of the radial pulse and HRV in normotensive and hypertensive subjects [18]. During this study assessment, we located the Cun, Guan, and Chi pulse positions on the left and right wrists of each study participant. The Guan pulse position, where the radial pulse is palpated, is located at the prominence distal to the radial styloid process (see Figure 3). The Cun pulse position is located at the distal aspect and the Chi pulse position is located at the proximal aspect of the Guan pulse position. An anatomical study in 1994 reported that the length of the Guan pulse position is approximately 1.5 cm and that of the Cun and Chi pulse positions is approximately 1 cm each [3]. In our study, we marked these pulse positions during the baseline assessment so that the same positions were subsequently assessed during the pre- and postintervention study visits.
Figure 3.
Locations of the Cun, Guan, and Chi pulse positions.
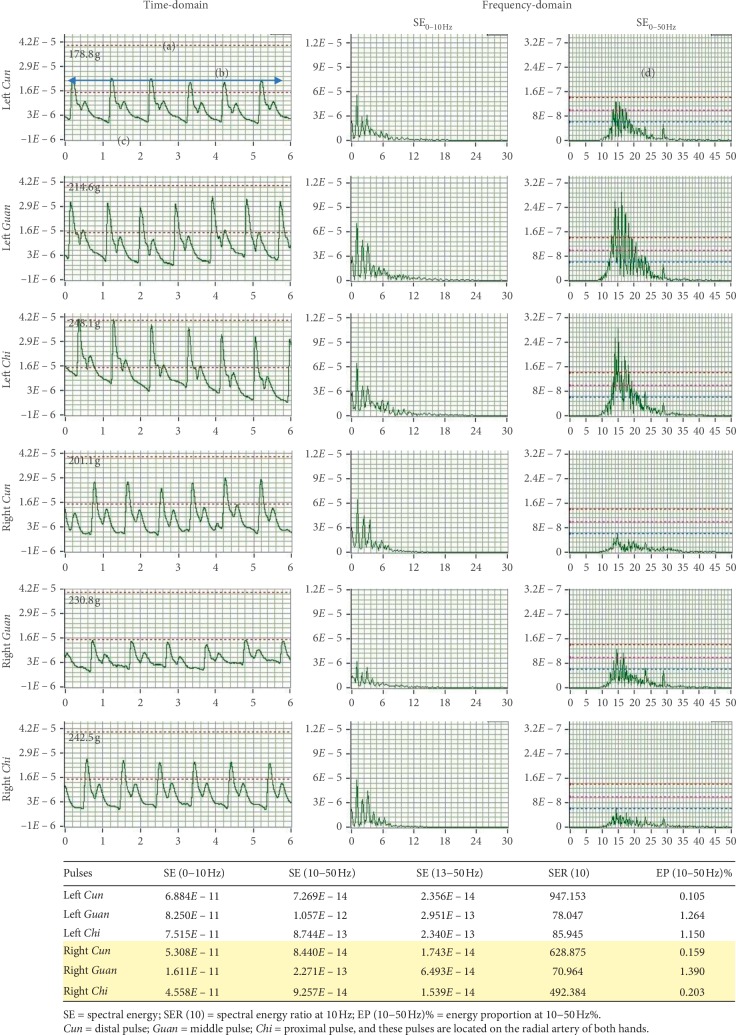
Upon placing the pressure sensor pen on each pulse position, the real-time representation of the time-domain and frequency-domain analyses is displayed in the monitor. The best spectrogram with the greatest amplitude of each pulse position is sequentially recorded. A report is then generated immediately from the software application after assessment of the six pulse positions is completed (see Figure 4). In this study, we assessed the pulse positions in the same order of right Cun, right Guan, right Chi, left Cun, left Guan, and left Chi during the baseline, preintervention, and postintervention phases. There was no time lag between the measurement of each pulse position.
Figure 4.
A typical report of a study participant generated from the pulse sphygmograph providing the time- and frequency-domain analyses of the six pulse positions. Each pulse profile is characterised by the following: (a) depth indicates light (0−60 g), moderate (60−120 g), and heavy (>120 g) pressure on the radial artery; (b) rate indicates the pulse rate, calculated by multiplying the number of waves by 10; (c) waveform provides information on the status of Qi and blood. Twenty-eight common pulse waveforms exist, as described in Introduction; and (d) density provides information on the status of heat, cold, dampness, and Qi stagnation in the body, while intensity indicates the amplitude of these causative factors.
2.7. Sample Size
Shin et al. [19] and Kim et al. [20] estimated a sample size of 25 participants in their single-arm study based on a 5% type 1 error, 80% power, and 5% dropout rates, derived from the mean change and standard deviation in SE13–50 Hz during the pre- and postintervention phases observed in the study by Huang et al. [12]. Huang et al. used the Huang-T1 Pulse Sphygmograph to compare the effects of acupuncture between healthy subjects and patients with dyspepsia [12]. Each study group contained 30 participants, and the reported p value for the difference in SE13–50 Hz between the pre- and postinterventions was 0.0029; the mean difference was −3.38.
As a reference, we performed an interim analysis at the 25th trial, to examine the significant difference (p values) of the mean for the primary outcome. Recruitment into the study was halted after obtaining significant differences (p < 0.05) in SE13–50 Hz and FTF and FPS-R results at the end of the approved trial period (March 2019).
2.8. Assignment Method and Blinding
As all participants received the same pre- and postinterventions, this study did not need to incorporate randomised assignment and blinding procedures.
2.9. Unit of Analysis and Statistical Methods
Analyses were performed at a group level. Baseline characteristics (age, gender, height, body weight, and vital signs), FTF and FPS-R test results, and pulse assessments were compared between A0 (30 min before acupuncture), A1 (10 min before acupuncture), and A2 (10 min after acupuncture). The significance of changes in the SE13–50 Hz and FTF and FPS-R tests induced by the acupuncture intervention was determined using paired t-tests. Wilcoxon signed-rank test analysis was performed (this nonparametric statistical test is used to assess differences from matched-pair designs or repeated measures to determine whether two dependent samples selected from the populations have the same distribution). The two-sided significance level <0.05 was used. Results were analysed using SAS statistical software (Version 9.4; SAS Institute, Cary, NC, USA) and are presented as the means, standard deviations, 95% CIs, and p values.
2.10. Ethical Approval and Consent to Participate
CMUH REC, Taichung, Taiwan, approved the study under protocol nos. CMUH107-REC2-022 and CMUH107-REC2-022 (AR-1). This study was registered at www.clinicaltrials.gov (NCT03501771) on 17 April 2018. Before commencing the study, we obtained written informed consent from each participant.
3. Results
Forty-five individuals were enrolled into the study, and three were subsequently excluded, as they were not able to undergo pulse assessments at the principal investigator's discretion. For analysis, we excluded the data of one individual above 75 years, to reduce the error of experimental results. All study results are therefore for 41 participants. None of the enrolled study participants discontinued the study because of compliance issues or adverse events. No unintended effects or adverse events were reported in any of the assessments.
3.1. Baseline Characteristics
The baseline characteristics of the study population with LBP are described in Table 1. There were 29 female and 12 male participants with an average overall age of 41.63 ± 16.01 years: 48.8% were young adults (20−44 years), 39% were middle-aged (45−64 years), and 12.2% were elderly (65−75 years). LBP was reportedly felt as fixed, distended, or sharp pain by 43.9% of the study cohort; 56.1% experienced dull, aching pain (the intensity of aching was more than the intensity of sharp pain). The majority of study participants (58.5%) had minimal disabilities. Based on the CCMQ self-survey, 56.1% of the participants had balanced constitutions. The correlation between various body constitutions and different types of LBP was not analysed because of the low sample size for each type of nonbalanced constitution.
Table 1.
Baseline characteristics of the study participants with lower back pain.
| Baseline characteristics | Number | Percentage |
|---|---|---|
| Total number of patients | 41 | |
|
| ||
| Gender | ||
| Female | 29 | 70.7 |
| Male | 12 | 29.3 |
|
| ||
| Age (years) | ||
| 20–44 | 20 | 48.8 |
| 45–64 | 16 | 39.0 |
| 65–75 | 5 | 12.2 |
|
| ||
| Types of LBP | ||
| Fixed, distended, or sharp pain (Group 1) | 18 | 43.9 |
| Acute (<4 weeks) | 11 | |
| Subacute (4–12 weeks) | 2 | |
| Chronic (>12 weeks) | 5 | |
| Dull, aching pain (Group 2) | 23 | 56.1 |
| Acute (<4 weeks) | 8 | |
| Subacute (4–12 weeks) | 1 | |
| Chronic (>12 weeks) | 14 | |
|
| ||
| ODI | ||
| Minimal disability | 24 | 58.5 |
| Moderate disability | 13 | 31.7 |
| Severe disability | 4 | 9.8 |
|
| ||
| CCMQ | ||
| Balanced constitution | 23 | 56.1 |
| Nonbalanced constitution (Qi-deficient, Yang-deficient, Yin-deficient, Phlegm-dampness, Damp-heat, Stagnant blood, Stagnant Qi, and Inherited Special Constitutions) | 18 | 43.9 |
ODI: Oswestry Disability Index; CCMQ: Constitution in Chinese Medicine Questionnaire.
3.2. Vital Signs
Table 2 compares the vital signs before and after the intervention. There was no significant difference in body temperature before and after the intervention. However, there were a significant increase in DBP and an extremely significant decrease (p < 0.0001) in the pulse rate after the intervention.
Table 2.
Comparison of the vital signs at baseline and before and after the intervention.
| Parameter | Baseline (A0) | Preintervention (A1) | Postintervention (A2) | p value (A0 vs. A1) | p value (A1 vs. A2) | 95% CI (A0 vs. A1) | 95% CI (A1 vs. A2) |
|---|---|---|---|---|---|---|---|
| Body temperature (°C) | 36.46 ± 0.39 | 36.53 ± 0.42 | 36.45 ± 0.39 | 0.0982 | 0.0704 | −0.1498, 0.0132 | −0.0068, 0.1629 |
| SBP (mmHg) | 116.17 ± 17.56 | 114.46 ± 17.76 | 115.22 ± 16.76 | 0.0593 | 0.5270 | −0.0702, 3.4848 | −3.1504, 1.6382 |
| DBP (mmHg) | 74.76 ± 12.49 | 73.02 ± 12.24 | 76.44 ± 12.54 | 0.0315 ∗ | 0.0039 ∗ | 0.1614, 3.3020 | −5.6698, −1.1594 |
| Pulse rate (beats/min) | 71.87 ± 11.14 | 69.39 ± 11.04 | 65.26 ± 9.53 | 0.0001 ∗∗ | 7.59E − 08 ∗∗ | 1.4612, 4.0022 | 3.1063, 5.8693 |
Values are presented as mean ± SD. ∗p < 0.05; ∗∗p < 0.001. A0 = assessed 30 min before acupuncture; A1 = assessed 10 min before acupuncture; A2 = assessed 10 min after acupuncture; DBP: diastolic blood pressure; SBP: systolic blood pressure; SD = standard deviation. 95% CI is presented as a range from the lower limit to the upper limit.
3.3. Primary Outcome Measure
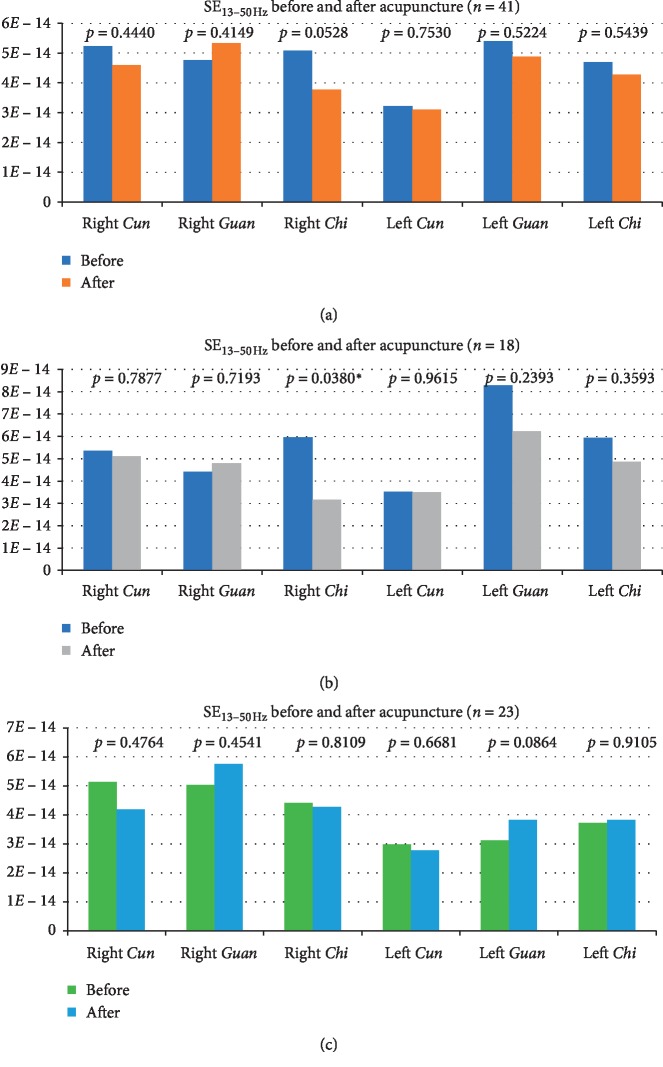
The radial pulse SE13–50 Hz was determined at the Cun, Guan, and Chi pulses before and after the intervention. Table 3 presents the results of these six pulse positions in the overall study population. Group 1 represents study participants with fixed, distended, or sharp LBP (Table 4), and Group 2 represents those with dull, aching LBP (Table 5). Figure 5 presents the graphical data.
Table 3.
SE13–50 Hz of the six pulse positions (all, n=41).
| Pulse position | Baseline (A0) | Preintervention (A1) | Postintervention (A2) | p value (A0 vs. A1) | p value (A1 vs. A2) | 95% CI (A0 vs. A1) | 95% CI (A1 vs. A2) | |
|---|---|---|---|---|---|---|---|---|
| Right Cun | Mean | 4.093E − 14 | 5.235E − 14 | 4.590E − 14 | 0.1696 | 0.4440 | 1.80E − 14, 1.40E − 13 | 1.09E − 13, 7.77E − 14 |
| SD | 5.386E − 14 | 6.165E − 14 | 3.811E − 14 | |||||
|
| ||||||||
| Right Guan | Mean | 4.972E − 14 | 4.758E − 14 | 5.333E − 14 | 0.7599 | 0.4149 | −1.01E − 13, 1.08E − 13 | −7.85E − 14, 1.02E − 13 |
| SD | 4.444E − 14 | 3.004E − 14 | 4.710E − 14 | |||||
|
| ||||||||
| Right Chi | Mean | 5.077E − 14 | 5.086E − 14 | 3.779E − 14 | 0.9794 | 0.0528 | −2.90E − 14, 8.21E − 14 | −1.47E − 13, 1.85E − 14 |
| SD | 5.560E − 14 | 4.643E − 14 | 2.773E − 14 | |||||
|
| ||||||||
| Left Cun | Mean | 3.588E − 14 | 3.219E − 14 | 3.095E − 14 | 0.3809 | 0.7530 | −7.20E − 14, 4.80E − 14 | −4.97E − 14, 4.87E − 14 |
| SD | 3.086E − 14 | 2.271E − 14 | 2.047E − 14 | |||||
|
| ||||||||
| Left Guan | Mean | 4.543E − 14 | 5.394E − 14 | 4.880E − 14 | 0.3432 | 0.5224 | −6.08E − 14, 6.99E − 14 | −3.47E − 14, 7.22E − 14 |
| SD | 4.923E − 14 | 8.254E − 14 | 4.957E − 14 | |||||
|
| ||||||||
| Left Chi | Mean | 4.129E − 14 | 4.696E − 14 | 4.279E − 14 | 0.4741 | 0.5439 | −4.90E − 14, 8.82E − 14 | −4.80E − 14, 7.99E − 14 |
| SD | 3.991E − 14 | 6.041E − 14 | 4.235E − 14 | |||||
∗ p < 0.05. A0 = assessed 30 min before acupuncture; A1 = assessed 10 min before acupuncture; A2 = assessed 10 min after acupuncture; SD = standard deviation. 95% CI is presented as a range from the lower limit to the upper limit.
Table 4.
SE13–50 Hz of the six pulse positions of study participants with fixed, distended, or sharp pain (Group 1, n=18).
| Pulse position | Baseline (A0) | Preintervention (A1) | Postintervention (A2) | p value (A0 vs. A1) | p value (A1 vs. A2) | 95% CI (A0 vs. A1) | 95% CI (A1 vs. A2) | |
|---|---|---|---|---|---|---|---|---|
| Right Cun | Mean | 4.578E − 14 | 5.360E − 14 | 5.104E − 14 | 0.3843 | 0.7877 | –263E − 16, 1.07E − 14 | –171E − 16, 2.23E − 14 |
| SD | 5.672E − 14 | 5.759E − 14 | 4.740E − 14 | |||||
|
| ||||||||
| Right Guan | Mean | 5.681E − 14 | 4.407E − 14 | 4.795E − 14 | 0.3307 | 0.7193 | –141E − 16, 3.96E − 14 | –263E − 16; 1.85E − 14 |
| SD | 5.542E − 14 | 2.905E − 14 | 4.021E − 14 | |||||
|
| ||||||||
| Right Chi | Mean | 6.109E − 14 | 5.961E − 14 | 3.155E − 14 | 0.7264 | 0.0380 ∗ | –731E − 17, 1.03E − 14 | 1.75E − 15, 5.44E − 14 |
| SD | 6.233E − 14 | 5.827E − 14 | 1.772E − 14 | |||||
|
| ||||||||
| Left Cun | Mean | 3.772E − 14 | 3.531E − 14 | 3.497E − 14 | 0.6093 | 0.9615 | –735E − 17, 1.22E − 14 | –145E − 16, 1.52E − 14 |
| SD | 3.532E − 14 | 2.432E − 14 | 2.453E − 14 | |||||
|
| ||||||||
| Left Guan | Mean | 5.728E − 14 | 8.294E − 14 | 6.220E − 14 | 0.2036 | 0.2393 | –666E − 16, 1.53E − 14 | –151E − 16, 5.66E − 14 |
| SD | 6.785E − 14 | 1.180E − 13 | 6.894E − 14 | |||||
|
| ||||||||
| Left Chi | Mean | 5.339E − 14 | 5.929E − 14 | 4.857E − 14 | 0.7167 | 0.3593 | –396E − 16, 2.78E − 14 | –133E − 16, 3.47E − 14 |
| SD | 5.309E − 14 | 8.296E − 14 | 5.285E − 14 | |||||
∗ p < 0.05. A0 = assessed 30 min before acupuncture; A1 = assessed 10 min before acupuncture; A2 = assessed 10 min after acupuncture; SD = standard deviation. 95% CI is presented as a range from the lower limit to the upper limit.
Table 5.
SE13–50 Hz of the six pulse positions of patients with dull, aching pain (Group 2, n=23).
| Pulse position | Baseline (A0) | Preintervention (A1) | Postintervention (A2) | p value (A0 vs. A1) | p value (A1 vs. A2) | 95% CI (A0 vs. A1) | 95% CI (A1 vs. A2) | |
|---|---|---|---|---|---|---|---|---|
| Right Cun | Mean | 3.714E − 14 | 5.137E − 14 | 4.187E − 14 | 0.2852 | 0.4764 | −2.90E − 14, 1.40E − 13 | −1.77E − 13, 1.30E − 13 |
| SD | 5.249E − 14 | 6.593E − 14 | 2.941E − 14 | |||||
|
| ||||||||
| Right Guan | Mean | 4.417E − 14 | 5.032E − 14 | 5.754E − 14 | 0.4033 | 0.4541 | −9.50E − 14, 2.18E − 13 | −1.20E − 13, 1.54E − 13 |
| SD | 3.382E − 14 | 3.116E − 14 | 5.236E − 14 | |||||
|
| ||||||||
| Right Chi | Mean | 4.269E − 14 | 4.402E − 14 | 4.268E − 14 | 0.8138 | 0.8109 | −3.16E − 14, 1.25E − 13 | −1.34E − 13, 1.07E − 13 |
| SD | 4.962E − 14 | 3.441E − 14 | 3.315E − 14 | |||||
|
| ||||||||
| Left Cun | Mean | 3.445E − 14 | 2.975E − 14 | 2.780E − 14 | 0.4826 | 0.6681 | −1.03E − 13, 4.70E − 14 | −4.80E − 14, 5.12E − 14 |
| SD | 2.762E − 14 | 2.160E − 14 | 1.654E − 14 | |||||
|
| ||||||||
| Left Guan | Mean | 3.616E − 14 | 3.125E − 14 | 3.832E − 14 | 0.1119 | 0.0864 | −1.21E − 13, 1.14E − 14 | −3.95E − 15, 1.22E − 13 |
| SD | 2.540E − 14 | 1.987E − 14 | 2.309E − 14 | |||||
|
| ||||||||
| Left Chi | Mean | 3.182E − 14 | 3.731E − 14 | 3.826E − 14 | 0.4207 | 0.9105 | −6.59E − 14, 1.08E − 13 | −8.01E − 14 1.60E − 13 |
| SD | 2.246E − 14 | 3.310E − 14 | 3.246E − 14 | |||||
A0 = assessed 30 min before acupuncture; A1 = assessed 10 min before acupuncture; A2 = assessed 10 min after acupuncture; SD = standard deviation. 95% CI is presented as a range from the lower limit to the upper limit.
Figure 5.
Graphical presentation of the mean SE13–50 Hz determined from the pulse positions before and after acupuncture in the overall group (n=41) (a), Group 1 (n=18) (b), and Group 2 (n=23) (c). ∗p < 0.05.
The results of the radial pulse diagnoses showed that, in general, acupuncture at Shenshu (BL23), Dachangshu (BL25), and Weizhong (BL40) reduced the high-frequency SE at the right Chi pulse after the treatment (p=0.0528). The reduction was significant in Group 1 participants with fixed, distended, or sharp pain (p=0.0380), but not among those in Group 2 with the dull, aching pain (p=0.8109). In contrast, Group 2 displayed an increasing trend close to significance in high-frequency SE at the left Guan pulse after acupuncture treatment (p=0.0864).
Nonparametric analysis revealed no significant differences in SE13–50 Hz during the pre- and postinterventions, except for the right Chi of Group 1 participants. Table 6 provides the results of the nonparametric analysis of SE13–50 Hz values for Group 1 before and after acupuncture (A1 vs. A2).
Table 6.
Comparison of the SE13–50 Hz of Group 1 (n=18) before and after acupuncture.
| Pulse position | Preintervention (A1) | Postintervention (A2) | p value (A1 vs. A2) | |
|---|---|---|---|---|
| Right Cun | Mean | 5.360E − 14 | 5.104E − 14 | 0.551 |
| SD | 5.759E − 14 | 4.740E − 14 | ||
|
| ||||
| Right Guan | Mean | 4.407E − 14 | 4.795E − 14 | 1.000 |
| SD | 2.905E − 14 | 4.021E − 14 | ||
|
| ||||
| Right Chi | Mean | 5.961E − 14 | 3.155E − 14 | 0.043 ∗ |
| SD | 5.827E − 14 | 1.772E − 14 | ||
|
| ||||
| Left Cun | Mean | 3.531E − 14 | 3.497E − 14 | 0.965 |
| SD | 2.432E − 14 | 2.453E − 14 | ||
|
| ||||
| Left Guan | Mean | 8.294E − 14 | 6.220E − 14 | 0.364 |
| SD | 1.180E − 13 | 6.894E − 14 | ||
|
| ||||
| Left Chi | Mean | 5.929E − 14 | 4.857E − 14 | 0.806 |
| SD | 8.296E − 14 | 5.285E − 14 | ||
∗ p < 0.05. A1 = assessed 10 min before acupuncture; A2 = assessed 10 min after acupuncture; SD = standard deviation. Values are presented as mean ± SD.
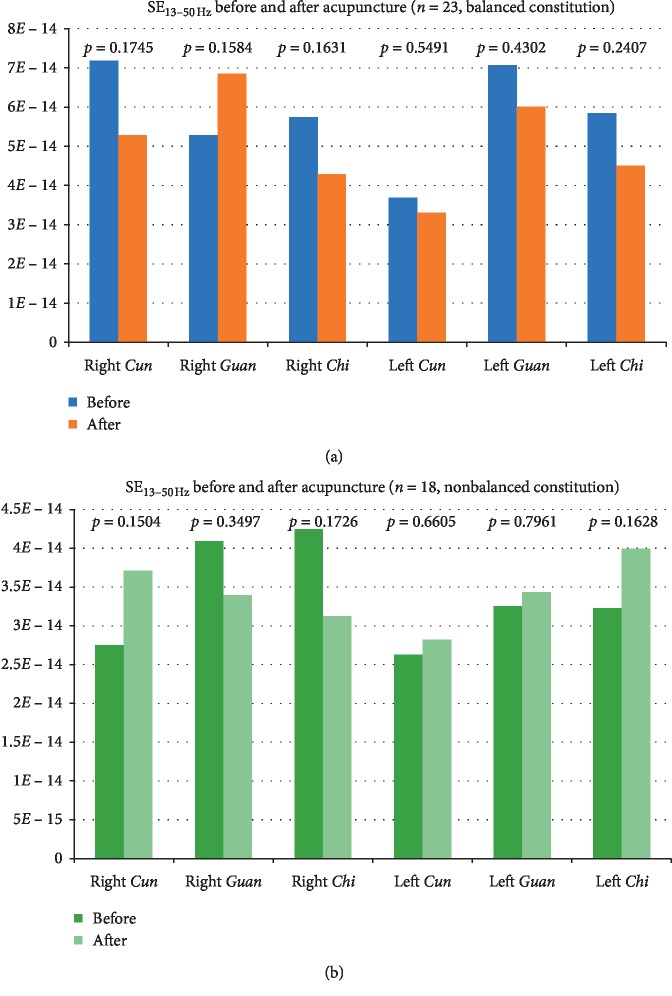
The effects of acupuncture on the radial pulse SE13–50 Hz were compared between the balanced and nonbalanced constitutions. Changes in SE13–50 Hz in study participants with a balanced constitution were similar to those in Group 1 participants, although the decreases in right and left Chi were not significant (Figure 6). In contrast, those with nonbalanced constitutions had a nonsignificant decrease in SE13–50 Hz in the right Guan and Chi and increases in the other pulse positions.
Figure 6.
Comparison of mean SE13–50 Hz values determined from the pulse positions before and after acupuncture between study participants with balanced constitutions (a) and those with nonbalanced constitutions (b).
3.4. Secondary Outcome Measures
Table 7 provides the results of the FTF and FPS-R tests. We observed that both Group 1 and Group 2 study participants had a greater lumbar range of motion, since the distance between the floor and the finger was significantly shorter after the acupuncture session. Group 2 had significantly better lumbar range of motion than Group 1 (p < 0.001). FPS-R test results showed that both groups experienced a significant reduction in pain after the acupuncture procedure (p < 0.001), although the pain rating was significantly better for Group 2 versus Group 1.
Table 7.
Results of the secondary outcome measures, the fingertip-to-floor (FTF) test, and the Faces Pain Scale-Revised (FPS-R) test.
| Parameter | Preintervention (A1) | Postintervention (A2) | p value (A1 vs. A2) | 95% CI (A1 vs. A2) |
|---|---|---|---|---|
| Fingertip-to-floor (FTF) (cm) | 12.59 ± 12.27 | 9.88 ± 10.21 | 0.0001 ∗∗ | 1.4078, 4.0068 |
| Group 1 | 16.36 ± 14.67 | 12.33 ± 11.76 | 0.0070 ∗ | 1.2571, 6.7985 |
| Group 2 | 9.63 ± 8.87 | 7.96 ± 8.28 | 0.0001 ∗∗ | 0.7786, 2.5692 |
|
| ||||
| Faces Pain Scale (FPS-R) | 3.56 ± 1.64 | 1.22 ± 1.67 | 1.24E − 12 ∗∗ | 1.8754, 2.8076 |
| Group 1 | 4.22 ± 1.80 | 1.89 ± 1.88 | 2.25E − 05 ∗∗ | 1.4805, 3.1862 |
| Group 2 | 3.04 ± 1.33 | 0.70 ± 1.29 | 1.55E − 08 ∗∗ | 1.7854, 2.9103 |
Values are presented as mean ± SD. ∗p < 0.05; ∗∗p < 0.001. A1 = assessed 10 min before acupuncture; A2 = assessed 10 min after acupuncture; SD = standard deviation. 95% CI is presented as a range from the lower limit to the upper limit.
4. Discussion
A pulse diagnosis provides information on the physiological and pathological states of the visceral organs and bowels [5]. This tactile method of determining essential information for diagnoses and treatments has been progressively transformed and digitised through the invention of various scientific tools over the last few decades [21]. A few studies have reported the effects of acupuncture intervention on the radial pulse in healthy subjects [20, 22–26], patients with dyspepsia [12], and those with cervical spondylosis [27]. To date, no study has investigated the effect of acupuncture on the radial pulse patterns in individuals with LBP.
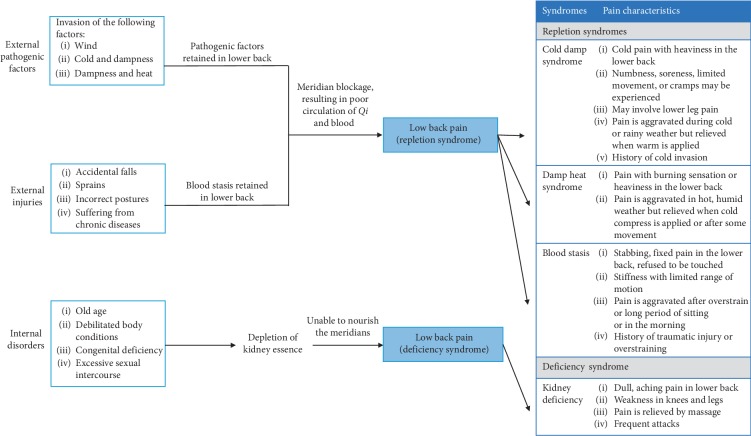
4.1. Demographic Characteristics
Our study contained a higher proportion of younger adults (aged between 20 and 44 years; 48.8%) than other age groups, reflecting findings from another study demonstrating that LBP is especially prevalent among younger adults [28]. Approximately 70% of our study population was female. One study has reported that LBP is more prevalent among females than males, predominantly in occupational groups including industrial workers, white-collar workers, physiotherapists, and hospital staff [29]. As described in our published study protocol, four types of LBP exist, based on the TCM syndrome-aetiology differentiation (see Figure 7) [1].
Figure 7.
Diagrammatic presentation of aetiology and syndrome relationships of LBP. Each syndrome is characterised by the pain characteristics, associated symptoms (e.g., cold extremities in the Cold damp syndrome), and tongue and pulse characteristics.
Each LBP syndrome is identified by characteristic pain sensations and associated symptoms. For instance, a patient with Cold damp syndrome experiences cold extremities in addition to cold pain and heaviness in the lower back; numbness, soreness with limited movement, or cramps may also be experienced; the pain is worse during cold or rainy weather but relieved when warmth is applied; often experiences poor appetite and abdominal distention; has thick white-coating on the tongue; a deep and taut pulse or deep and slow pulse may be felt [30]. Although we had designed our study to recruit the four types of LBP patients, we found that only two types of pain were common in these study participants, i.e., fixed, distended, or sharp pain and dull, aching pain. Thus, to facilitate our statistical analysis, we categorised the data into two sets according to the type of pain described by the study participants, that is, Group 1 (LBP with fixed, distended, or sharp pain) and Group 2 (LBP with dull, aching pain).
About 60% of the Group 1 participants were in the acute stage (<4 weeks), while 60% of the Group 2 participants were in the chronic stage (>12 weeks). Fixed, distended, or sharp pain was experienced by study participants in the acute stage. In the TCM perspective, this was due to the obstruction of the meridians by blood stasis [31]. In contrast, dull, aching pain experienced in the chronic stage was related to kidney deficiency that resulted in poor nourishment of the meridians [32].
Over half of the study participants had a balanced body constitution based on the CCMQ survey. The CCMQ has been published by the China Association of Chinese Medicine since 2008 and is used to determine the body constitution type based on TCM concepts [33, 34]. This questionnaire contains 60 questions that categorise the body constitution into nine types, namely, Normality, Qi-deficiency, Yin-deficiency, Yang-deficiency, Phlegm-dampness, Damp-heat, Blood stasis, Qi-depressed, and Inherited special constitutions. A pilot test was carried out in a Beijing population, and its construct validity and reliability were proven by 2,500 subjects [35]. Our study sample size was not large enough to analyse correlations between types of LBP based on the nine types of body constitutions. Nevertheless, we found that the changes in SE13–50 Hz after acupuncture on the radial pulse in study participants with balanced constitution were similar to the changes in SE13–50 Hz in Group 1 participants. Conversely, changes in SE13–50 Hz in the right Guan and Chi were nonsignificantly decreased after acupuncture in participants with nonbalanced constitutions. These results are inconclusive because of a lack of significance. It may be worthwhile conducting future clinical studies with larger sample sizes.
4.2. Vital Signs
We observed an insignificant elevation in SBP but a significant elevation in DBP within the normal range after bilateral acupuncture intervention at BL23, BL25, and BL40. This phenomenon has not been previously reported by any studies. Flachskampf et al. reported that acupuncture significantly reduced SBP and DBP in hypertensive patients in a randomised controlled trial [36]. In dogs with low blood pressure, electroacupuncture at Zusanli (ST36) or Neiguan (PC6) significantly restored blood pressure to normal levels [37]. To explain this phenomenon using the TCM meridian theory, the Suwen text in Chapter 24 of Huang Di Nei Jing describes how “the Tai-Yang meridians often have more blood and less Qi” [14]. We therefore speculate that when we stimulated the acupoints on the Bladder meridian of the Foot Tai-Yang, blood circulation was improved. Moreover, Wang et al. used a blood perfusion imaging technique to conclude that acupuncture at BL40 can increase skin blood perfusion in the lower back [38]. Further investigations are warranted to obtain more conclusive results on the comparative effects of specific acupoints on blood pressure.
Our findings also show that the pulse rate was significantly reduced within the 20-min interval before the intervention. There was a marked significant decrease after the intervention. Streitberger et al. have pointed out that the decrease in the heart rate after an acupuncture procedure could be due to delayed vagal activation [39].
4.3. Primary Outcome Measure: Radial Pulse Diagnosis
The results of the radial pulse SE13–50 Hz analysis suggest that our primary hypothesis holds true, that is, “acupuncture can significantly influence the Chi pulse in participants with LBP.” The SE13–50 Hz of the right Chi pulse was significantly reduced after the acupuncture treatment at the bilateral BL23, BL25, and BL40 (p=0.0528). However, we observed that Group 1 participants had a more significant reduction (p=0.0380) compared to those in Group 2 (p=0.6903). In contrast, Group 2 participants had a marked trend of increasing SE at the left Guan pulse after the treatment (p=0.0864).
For the subgroup analyses, the only significant difference in SE13–50 Hz was found in the right Chi of Group 1 study participants between the pre- and postinterventions and was probably a result of the small sample size. In further analysis using the Wilcoxon signed-rank test, the nonparametric results showed less significant difference in SE13–50 Hz of right Chi for the overall population (n=41) before and after acupuncture. Subgroup analysis of Group 1 maintained robust significance in the comparison of right Chi. The nonparametric analysis showed the same trend and consistent result as the parametric analysis. Thus, these results provided valuable information and suggested that the right Chi pulse can effectively assess the effect of acupuncture intervention in LBP patients with fixed, distended, or sharp pain, while the left Guan pulse is potentially useful to assess those with dull, aching pain.
We speculated that higher density and intensity of SE were generally found at the right Chi pulse of Group 1 study participants. The high SE corresponded to the increased vasomotion of the peripheral blood vessels. This coincides with Huang et al.'s study, which reported that heat stress subjects had an elevated SE that resulted from an increase in peripheral vascular dilatation and vasomotion [17]. The increased vasomotion was a result of the elevated sympathetic nervous activity stimulated by pain [40]. However, the effects of acupuncture on sympathetic nerve activity are controversial. Middlekauff et al. concluded that acupuncture inhibited sympathetic nerve activity during mental stress in patients with heart failure [41], whereas Kim et al. reported that acupuncture at ST36 increased sympathetic nerve activity in healthy participants [20]. In this study, we speculate that bilateral acupuncture at BL23, BL25, and BL40 attenuated sympathetic nerve activity, reducing the contraction force of local muscles and vasomotion. Thus, pain was relieved, and a high-frequency SE at the right Chi pulse was decreased.
Huang Di Nei Jing states that “both Chi pulse positions correspond to the kidney and the abdomen” and that “the lumbus represents the house of the kidneys” [3, 14]. Interestingly, we found that bilateral acupuncture at BL23, BL25, and BL40 acupoints for treatment of LBP influences high-frequency SE more significantly at the right Chi pulse rather than both Chi pulses. To explain this phenomenon, we revisited the ancient literature. Nan Jing: The Classic of Difficult Issues states that the Chi pulses correspond to the bladder [3]. In clinical practice, the right Chi pulse is more closely associated with the bladder, although some physicians and philosophers have suggested that the left Chi pulse corresponds to the bladder [3]. The Ling Shu text in Chapter 10 states that the Bladder meridian of the Foot Tai-Yang is affiliated with the bladder and connects to the kidneys. In addition, Shang Han Lun (Treatise on Cold Pathogenic Diseases) states that the Tai-Yang meridians dominate the body's exterior. We speculated that fixed, distended, or sharp LBP results from kidney Qi repletion caused by the invasion of pathogenic factors on the body's exterior, mainly influencing pulse density and intensity and causing a large variation in high-frequency SE [16]. Thus, higher density and intensity of SE were found at the right Chi pulse before treatment. Acupuncture at BL23, BL25, and BL40 of the Bladder meridian resulted in decreased density and intensity of SE, reflecting directly on the right Chi pulse. Future studies could investigate the effects of acupoints from other meridians associated with the treatment of LBP on the left and right Chi pulses, to prove our speculation. The Suwen text in Chapter 39 of Huang Di Nei Jing describes how sudden pain occurs when the Qi channel is obstructed [14]. Conversely, a dull, aching pain is caused by Qi and blood insufficiency [42]. Our findings showed an increased high-frequency SE at the left Guan pulse of Group 2 participants after their acupuncture treatment. We speculate that these individuals have a circulatory insufficiency. A significant increase in blood flow during these acupuncture sessions resulted in a higher intensity of the SE in the left Guan, as it corresponds to the liver's blood supply and nervous system in TCM. Takayama et al. reported a significant increase in blood flow through the superior mesenteric artery after acupuncture stimulation at ST36 [43]. Our study also found a significant elevation in DBP within the normal range after the acupuncture. A future study may be warranted to investigate the effect of blood flow in the hepatic artery during stimulation of BL23, BL25, and BL40, to confirm the phenomenon observed in our study.
4.4. Secondary Outcome Measures: Pain Intensity and Physical Flexibility
The results from our assessments of lumbar ranges of motion and pain intensity suggest that our secondary hypothesis holds true, that is, “reduced pain intensity and better physical movement can be reflected in the FTF and FPS-R tests after the acupuncture intervention.” Generally, there were a significant reduction in pain intensity and improvement in the lumbar range of motion after acupuncture stimulation. This observation was also reported by Furlan et al., who found that acupuncture treatments provided a more effective functional improvement and pain relief than sham treatments or no treatment [44]. We observed a marked significant difference (p < 0.001) in Group 2 participants than in Group 1 participants, which suggests that BL23, BL25, and BL40 are effective for the treatment of dull, aching LBP. Studies have shown that the nociceptive pathways, including descending serotonergic and noradrenergic pathways, may be involved in the immediate analgesic effect of acupuncture on various types of pain [45]. More studies are needed to compare the analgesic effects of acupuncture on different types of pain.
4.5. Study Limitations and Solutions
Although quasi-experimental research is more feasible than true experimental research as it requires less time and has fewer logistical constraints, there were several limitations in our study. Because of the small sample size of this pilot study, the lack of random assignments in the quasi-experimental design may have presented a confounding bias that may limit the generalizability of the findings to a larger population. We therefore identified the threats to the validity of our findings in our experimental design to reduce the impact. For instance, we used the baseline assessments of the radial pulse and vital signs as a control to compare the stability of these parameters before the acupuncture intervention; the same acupuncturist applied a consistent acupuncture technique at the same acupoints in the treatment, and the acupuncturist was not informed of the type of LBP experienced by the study participants, in an attempt to avoid bias. Future studies with larger sample sizes and randomisation procedures are warranted to provide more conclusive results. We did not anticipate the outcome demonstrating how acupuncture differentially affects high-frequency SE in different types of LBP. Future research is warranted to compare treatment outcomes between healthy subjects and those with LBP. Another limitation was that no other pulse diagnostic device measures the SE13–50 Hz besides the approved PPAS-96 and Huang-T1 Pulse Sphygmograph in Taiwan. Therefore, we were not able to compare the outcomes with other devices. However, Huang-T1 Pulse Sphygmograph has been used in a few clinical studies [12, 17, 18], as well as in the Taiwanese hospitals and clinics; we therefore used this device in our preliminary study to assess the feasibility of the protocol design before proceeding with PPAS-96 Pulse Sphygmograph [1]. It will be beneficial to conduct future studies to compare and verify the SE measurements with other devices that will be available.
5. Conclusion
Our study provides novel information about the effects of acupuncture on the radial pulse SE in individuals with different types of LBP. Our findings suggest that the right Chi pulse is an effective indicator for assessing the effects of acupuncture intervention in individuals with fixed, distended, or sharp pain, whereas the left Guan pulse is a potentially useful diagnostic technique to determine acupuncture's effects in those with dull, aching pain. The acupoints BL23, BL25, and BL40 provide effective treatment for LBP. Individuals with dull, aching pain had a significant improvement in their lumbar ranges of motion, and they showed a noteworthy decrease in pain ratings after receiving acupuncture treatment.
Acknowledgments
This work was partly supported by the Chinese Medicine Research Center, China Medical University, from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education in Taiwan (grant number CMRC-CHM-0). The authors would also like to thank the support of CMUH for the use of its facilities and all the participants for their collaboration.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Authors' Contributions
Hui-Ping Ng (HPN) and Chin-Ming Huang (CMH) contributed equally to this study as co-first authors. Yu-Chen Lee (YCL) was the principal investigator, and Wen-Chao Ho (WCH) participated in the statistical analysis of the study. HPN, CMH, and YCL were involved in the conception and design of the study. HPN acquired clinical trial data, performed initial analyses, and drafted the manuscript. All authors reviewed and approved the final version of the manuscript.
References
- 1.Ng H.-P., Huang C.-M., Ho W.-C., Lee Y.-C. An investigation into the effects of acupuncture on radial pressure pulse waves in patients with low back pain: a protocol for a quasi-experimental study. Contemporary Clinical Trials Communications. 2019;15 doi: 10.1016/j.conctc.2019.100384.100384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu Y.-H., Cheng C.-S. Discussing the guiding action of pulse-taking on clinical acupuncture and moxibustion from the yellow emperor’s internal classic. Chinese Acupuncture & Moxibustion. 2002;21(1) [Google Scholar]
- 3.Huang C. M. Zhong Yi Mai Zhen Xue [Pulse Diagnosis in Traditional Chinese Medicine] Vol. 33. Taiwan: Zhi Yin Chu Ban She; 2015. [Google Scholar]
- 4.Tang A. C. Y. Review of traditional Chinese medicine pulse diagnosis quantification. In: Saad M., Medeiros R. d., editors. Complementary Therapies for the Contemporary Healthcare. London, UK: IntechOpen; 2012. [Google Scholar]
- 5.Tsai Y.-N., Huang Y.-C., Lin S. J.-S., et al. Different harmonic characteristics were found at each location on TCM radial pulse diagnosis by spectrum analysis. Evidence-Based Complementary and Alternative Medicine. 2018;2018:10. doi: 10.1155/2018/9018271.9018271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeon S. H., Kim K. K., Lee I. S., et al. Pulse wave variation during the menstrual cycle in women with menstrual pain. BioMed Research International. 2016;2016:8. doi: 10.1155/2016/1083208.1083208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coeytaux R. R., Chen W., Lindemuth C. E., Tan Y., Reilly A. C. Variability in the diagnosis and point selection for persons with frequent headache by traditional Chinese medicine acupuncturists. The Journal of Alternative and Complementary Medicine. 2006;12(9):863–872. doi: 10.1089/acm.2006.12.863. [DOI] [PubMed] [Google Scholar]
- 8.Hogeboom C. J., Sherman K. J., Cherkin D. C. Variation in diagnosis and treatment of chronic low back pain by traditional Chinese medicine acupuncturists. Complementary Therapies in Medicine. 2001;9(3):154–166. doi: 10.1054/ctim.2001.0457. [DOI] [PubMed] [Google Scholar]
- 9.WHO. Xi Tai Ping Yang Di Qu WHO Biao Zhun Zhen Jiu Xue Wei [WHO Standards Acupuncture Point Locations in Western Pacific Region] Taipei, Taiwan: Chinese Medical Association of Acupuncture; 2010. [Google Scholar]
- 10.Deadman P., Baker K., Al-Khafaji M. A Manual of Acupuncture. Hove, UK: Journal of Chinese Medicine Publications; 2007. [Google Scholar]
- 11.Lin J.-G. Newly Edited Color Book of Acupuncture and Moxibustion. Taipei, Taiwan: JYIN Publishing Company; 2009. [Google Scholar]
- 12.Huang C.-M., Chang H.-C., Li T.-C., Chen C. C., Liao Y.-T., Kao S.-T. Acupuncture effects on the pulse spectrum of radial pressure pulse in dyspepsia. The American Journal of Chinese Medicine. 2012;40(3):443–454. doi: 10.1142/s0192415x12500346. [DOI] [PubMed] [Google Scholar]
- 13.Wei-San H., Bih-Cheng C. Zhen Jiu Ke Xue [Acupuncture Science] 2nd. Taipei, Taiwan: Cheng Chung Bookstore; 2013. [Google Scholar]
- 14.Unschuld P. U., Tessenow H., Jinsheng Z. Huang Di Nei Jing Su Wen (An Annotated Translation of Huang Di’s Inner Classic—Basic Questions: 2 Volumes) 1st. Berkeley, CA, USA: University of California Press; 2011. [Google Scholar]
- 15.MOHW. National health insurance statistical report for Chinese medicine outpatient clinics. September 2019. https://dep.mohw.gov.tw/DOS/cp-4268-45880-113.html.
- 16.Wei L. Y., Lee C. T., Chow P. A new scientific method of pulse diagnosis. American Journal of Acupuncture. 1984;12(3):205–218. [Google Scholar]
- 17.Huang C. M., Chang H. C., Kao S. T., et al. Radial pressure pulse and heart rate variability in heat- and cold-stressed humans. Evidence-Based Complementary and Alternative Medicine. 2011;2011:9. doi: 10.1155/2011/751317.751317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang C.-M., Chang H.-C., Kao S.-T., et al. Radial pressure pulse and heart rate variability in normotensive and hypertensive subjects. The Journal of Alternative and Complementary Medicine. 2011;17(10):945–952. doi: 10.1089/acm.2010.0326. [DOI] [PubMed] [Google Scholar]
- 19.Shin J. Y., Lee J. H., Ku B., et al. Effects of acupuncture stimulation on the radial artery’s pressure pulse wave in healthy young participants: protocol for a prospective, single-arm, exploratory, clinical study. Journal of Pharmacopuncture. 2016;19(3):197–206. doi: 10.3831/kpi.2016.19.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim T. H., Ku B., Bae J. H., et al. Hemodynamic changes caused by acupuncture in healthy volunteers: a prospective, single-arm exploratory clinical study. BMC Complementary and Alternative Medicine. 2017;17(1):p. 274. doi: 10.1186/s12906-017-1787-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ghasemzadeh N., Zafari A. M. A brief journey into the history of the arterial pulse. Cardiology Research and Practice. 2011;2011:14. doi: 10.4061/2011/164832.164832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kwak K. I., Kang J. H., Lee H. The effects of acupuncture on radial pulse in healthy human subjects: a comparative study on tonifications of kidney and urinary bladder. The Acupuncture. 2015;32(2):105–121. doi: 10.13045/acupunct.2015024. [DOI] [Google Scholar]
- 23.Yoon K. S., Lee H. The effects of spleen-tonifying acupuncture on radial pulse in healthy human subjects. The Acupuncture. 2013;30(4):1–14. doi: 10.13045/acupunct.2013017. [DOI] [Google Scholar]
- 24.Takayama S., Seki T., Sugita N., et al. Radial artery hemodynamic changes related to acupuncture. Explore. 2010;6(2):100–105. doi: 10.1016/j.explore.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 25.Satoh H. Acute effects of acupuncture treatment with baihui (GV20) on human arterial stiffness and wave reflection. Journal of Acupuncture and Meridian Studies. 2009;2(2):130–134. doi: 10.1016/s2005-2901(09)60045-5. [DOI] [PubMed] [Google Scholar]
- 26.Won J. K., Jung S. K., Kim D. E., Lim J. Y., Kwon Y. D., Yeom S. R. Study on the radial pulse wave variables and heart rate variability after acupuncture stimulation. Journal of Physiology & Pathology in Korean Medicine. 2009;23(Suppl 1):237–244. [Google Scholar]
- 27.Zhang H., Guo M., Lu X. Pulse changes in patients with cervical spondylosis before and after acupuncture treatment. Journal of Traditional Chinese Medicine. 2016;36(1):63–70. doi: 10.1016/s0254-6272(16)30010-3. [DOI] [PubMed] [Google Scholar]
- 28.Ramdas J., Jella V. Prevalence and risk factors of low back pain. International Journal of Advances in Medicine. 2018;5(5):1120–1123. doi: 10.18203/2349-3933.ijam20183413. [DOI] [Google Scholar]
- 29.Chou Y., Shih C., Lin J., Chen T., Liao C. Low back pain associated with sociodemographic factors, lifestyle and osteoporosis: a population-based study. Journal of Rehabilitation Medicine. 2013;45(1):76–80. doi: 10.2340/16501977-1070. [DOI] [PubMed] [Google Scholar]
- 30.Yue W. X. Zhong Yi Nei Ke Xue [TCM Internal Medicine] Beijing, China: China Medical Science Press; 2013. [Google Scholar]
- 31.Zhu J., Arsovska B., Kozovska K. Acupuncture treatment in patients with low back pain. Yangtze Medicine. 2018;2(4):203–207. doi: 10.4236/ym.2018.24022. [DOI] [Google Scholar]
- 32.How do you treat back pain in your practice? Part 1. Medical Acupuncture. 2017;29(6):411–419. doi: 10.1089/acu.2017.29068.cpl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Q., Zhu Y. B., Xue H. S., Li S. Primary compiling of constitution in Chinese medicine questionnaire. Chinese Journal of Clinical Rehabilitation. 2006;10(3):12–14. [Google Scholar]
- 34.Wang Q. Classification and diagnosis basis of nine basic constitutions in Chinese medicine. Journal of Beijing University of Traditional Chinese Medicine. 2005;28(4):1–8. [Google Scholar]
- 35.Wong W., Lam C. L. K., Wong V. T., Yang Z. M., Ziea E. T. C., Kwan A. K. L. Validation of the constitution in Chinese medicine questionnaire: does the traditional Chinese medicine concept of body constitution exist? Evidence-Based Complementary and Alternative Medicine. 2013;2013:14. doi: 10.1155/2013/481491.481491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Flachskampf F. A., Gallasch J., Gefeller O., et al. Randomized trial of acupuncture to lower blood pressure. Circulation. 2007;115(24):3121–3129. doi: 10.1161/circulationaha.106.661140. [DOI] [PubMed] [Google Scholar]
- 37.Li P. Acupuncture treatment for low blood pressure and shock. Alternative, Complementary & Integrative Medicine. 2018;4(1):1–3. doi: 10.24966/acim-7562/100047. [DOI] [Google Scholar]
- 38.Wang L. L., Zhang W. B., Xie H. H., Tian Y. Y., Xu Y. H. Experimental verification of “treating lumbar-back problems by puncturing Weizhong (BL 40)” with blood perfusion imaging technique. Zhen Ci Yan Jiu. 2007;32(4):247–251. in Chinese. [PubMed] [Google Scholar]
- 39.Streitberger K., Steppan J., Maier C., Hill H., Backs J., Plaschke K. Effects of verum acupuncture compared to placebo acupuncture on quantitative EEG and heart rate variability in healthy volunteers. The Journal of Alternative and Complementary Medicine. 2008;14(5):505–513. doi: 10.1089/acm.2007.0552. [DOI] [PubMed] [Google Scholar]
- 40.Hamunen K., Kontinen V., Hakala E., Talke P., Paloheimo M., Kalso E. Effect of pain on autonomic nervous system indices derived from photoplethysmography in healthy volunteers. British Journal of Anaesthesia. 2012;108(5):838–844. doi: 10.1093/bja/aes001. [DOI] [PubMed] [Google Scholar]
- 41.Middlekauff H. R., Hui K., Yu J. L., et al. Acupuncture inhibits sympathetic activation during mental stress in advanced heart failure patients. Journal of Cardiac Failure. 2002;8(6):399–406. doi: 10.1054/jcaf.2002.129656. [DOI] [PubMed] [Google Scholar]
- 42.Yong H. Huang Di Nei Jing. Vol. 9. Taiwan: Son Book Service; 2018. [Google Scholar]
- 43.Takayama S., Watanabe M., Kusuyama H., et al. Evaluation of the effects of acupuncture on blood flow in humans with ultrasound color Doppler imaging. Evidence-Based Complementary and Alternative Medicine. 2012;2012:8. doi: 10.1155/2012/513638.513638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Furlan A. D., van Tulder M., Cherkin D., et al. Acupuncture and dry-needling for low back pain: an updated systematic review within the framework of the cochrane collaboration. Spine. 2005;30(8):944–963. doi: 10.1097/01.brs.0000158941.21571.01. [DOI] [PubMed] [Google Scholar]
- 45.Zhao Z.-Q. Neural mechanism underlying acupuncture analgesia. Progress in Neurobiology. 2008;85(4):355–375. doi: 10.1016/j.pneurobio.2008.05.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.