Abstract
Background:
Pruritus has been associated with cancer. However, limited data are available on the types of underlying malignancies associated with pruritus.
Objective:
We sought to characterize the association between pruritus and different cancer types, as well as variations by racial group.
Methods:
Cross-sectional study of patients ≥18 years of age seen at the Johns Hopkins Health System during 2013–2017. Patients with pruritus were compared with patients without pruritus. Analyses were stratified by race.
Results:
Patients with pruritus were more likely to have concomitant malignancy than those without pruritus (odds ratio 5.76, 95% confidence interval 5.53–6.00). Most strongly associated were cancers of the liver, gallbladder and biliary tract, hematopoietic system, and skin. Compared with white patients, black patients more frequently had soft tissue, dermatologic, and hematologic malignancies and less frequently had liver, respiratory, gastrointestinal, and gynecologic malignancies.
Limitations:
The cross-sectional design precludes analysis of the temporal association between pruritus and malignancy. The study is limited to a single tertiary care center.
Conclusion:
Pruritus is most strongly associated with cancers of the liver, skin, and hematopoietic system. Black patients with pruritus have a higher likelihood of skin, soft tissue, and hematologic malignancies than white patients, while whites have higher likelihoods of liver, respiratory, gastrointestinal, and gynecologic malignancies.
Keywords: cancer, itch, malignancy, paraneoplastic, pruritus
Pruritus is a significant source of morbidity in cancer patients. In a study of 700 cancer patients, generalized pruritus was present in 13% of patients.1 Pruritus is most frequently described in the setting of hematologic malignancy, particularly Hodgkin disease,2,3 bile duct and breast malignancies,4,5 and nonmelanoma skin cancer.6,7 Paraneoplastic itch has been recognized in the setting of numerous other malignancies, although the true prevalence of this phenomenon remains unknown.
More studies are needed to elucidate the association of pruritus with malignancy in other populations. In particular, little is known about the association between pruritus and malignancy among different racial/ethnic groups. This study aims to determine the association between pruritus and a variety of malignancies in a diverse US patient population at a tertiary care center.
METHODS
Institutional review board approval was waived because only anonymous aggregatelevel data were used. Retrospective data were collected by using the SlicerDicer feature of the Johns Hopkins Health System (JHHS) electronic medical record system, EPIC. JHHS has a diverse referral base, including the city of Baltimore as well as surrounding suburban areas in Maryland and neighboring states. In addition, many patients travel domestically and internationally to receive care at JHHS.
Population with pruritus
EPIC SlicerDicer was used to identify 16,925 patients aged ≥18 years who sought treatment at JHHS during April 4, 2013-December 31, 2017, with a visit diagnosis, billing diagnosis, or active problem list entry of itching or pruritus (systematized nomenclature of medicine–clinical terms [SNOMED-CT] term). The comparison population was composed of 4,679,528 patients aged ≥18 years without a diagnosis of itching who attended JHHS during the same time interval. See Table I for the demographic breakdown of the groups. To identify patients with skin eruption, the SNOMED-CT term eruption of skin was used.
Table I.
Demographics
| Characteristic | Pruritus group, N = 16,925, % | Nonpruritus group, N = 4,679,528, % |
|---|---|---|
| Sex | ||
| Male | 29.2 | 45.6 |
| Female | 70.8 | 54.5 |
| Race | ||
| White | 47.8 | 54.4 |
| Black | 37.7 | 19.1 |
| Asian | 5.8 | 3.3 |
| American Indian or Alaskan Native | 0.4 | 0.2 |
| Native Hawaiian or other Pacific Islander | 0.1 | 0.04 |
| Other | 8.7 | 5.7 |
| Unknown | 1.0 | 7.2 |
| Declined to answer | 0.3 | 0.2 |
| Age, y | ||
| 18–29 | 12.3 | 16.6 |
| 30–39 | 14.2 | 14.6 |
| 40–49 | 15.9 | 15.5 |
| 50–59 | 19.9 | 17.1 |
| 60–69 | 16.9 | 14.5 |
| 70–79 | 12.0 | 9.5 |
| 80–89 | 7.0 | 6.4 |
| 90–99 | 1.7 | 4.2 |
| 100–109 | 0.1 | 1.6 |
Identification of malignancies
EPIC SlicerDicer was used to identify patients with a diagnosis of primary malignant neoplasm (using appropriate SNOMED-CT terms for each malignancy type). Anatomic grouping was used to define solid organ malignancy categories and subcategories. For hematologic and dermatologic malignancies, disease-specific subcategorizes were used. For malignancies of the male and female genital tracts, only patients of the relevant sex were included in the analysis. For all other malignancies, both sexes were included. The odds ratio (OR) of each malignancy among the pruritus group compared with the group without pruritus was calculated, with additional stratification by race. As white and black were the largest racial groups in the cohort, these 2 groups were used for racial stratification. Sample sizes for other ethnic groups were small with inadequate statistical power for analysis.
Statistical analysis
ORs and 95% confidence intervals (CIs) were calculated with standard statistical methods by using Microsoft Excel software (Microsoft Corporation, Redmond, WA). P values for ORs were calculated by using chi-squared statistics with 1 degree of freedom, and P values for comparisons of ORs between groups were calculated using a z test. A Bonferroni correction was applied to the alpha level to account for multiple comparisons (alpha = 0.05/[number of independent comparisons]).
RESULTS
Pruritus is positively associated with malignancy
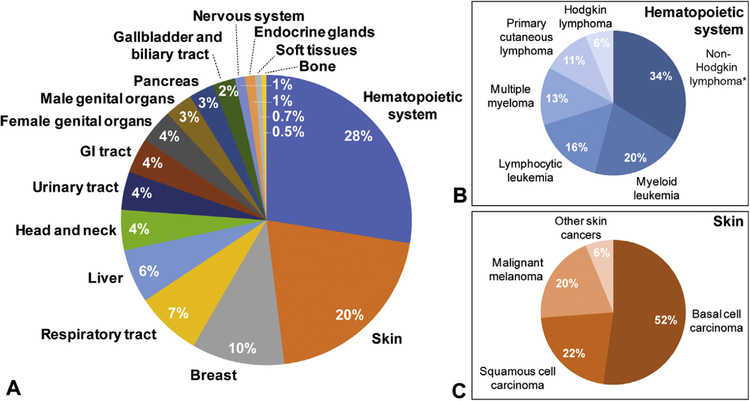
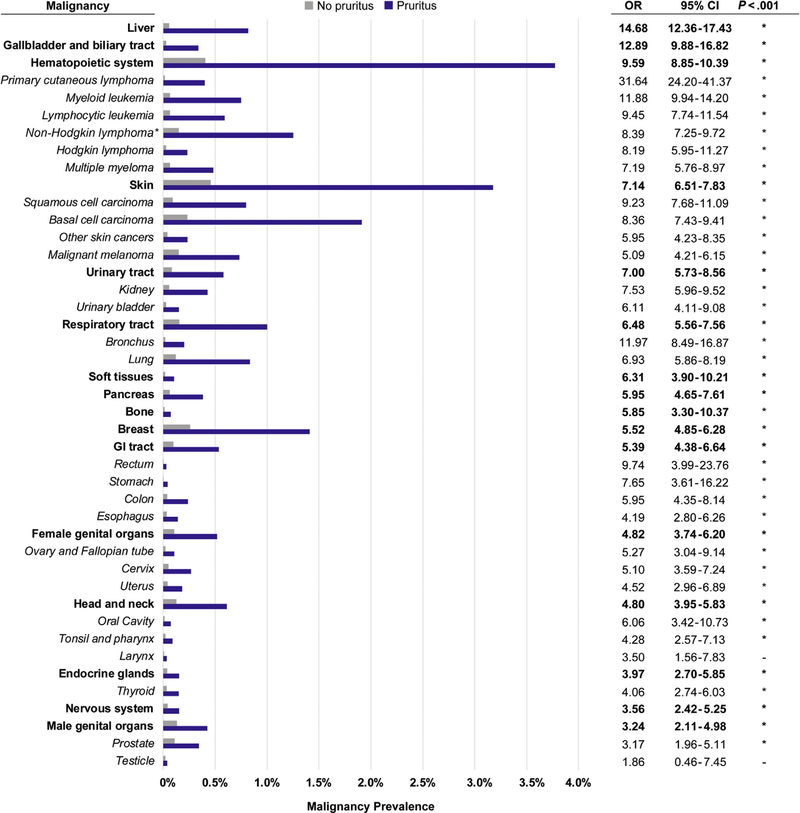
Of 16,925 patients given pruritus diagnoses at JHHS during 2013–2017, a total of 2,903 were also given diagnoses of malignancy during the same time frame (Fig 1). Patients seeking treatment at JHHS for pruritus were 5.76 times more likely to have a concomitant malignancy compared with patients without pruritus (OR 5.76, 95% CI 5.53–6.00). Pruritus was most strongly associated with cancers of the liver, gallbladder and biliary tract, hematopoietic system, and skin (Fig 2). Hematologic malignancies were divided into Hodgkin lymphoma, noncutaneous non-Hodgkin lymphoma, primary cutaneous lymphoma, lymphocytic leukemia, myeloid leukemia, and multiple myeloma. Pruritus was significantly associated with all 6 subtypes and was most strongly associated with primary cutaneous lymphoma and myeloid leukemia. Skin cancers were categorized as squamous cell carcinoma, basal cell carcinoma, malignant melanoma, and other skin cancers (which includes all primary malignant neoplasms of the skin excluding the preceding 3 diagnoses). Among skin cancers, pruritus was significantly associated with all subtypes and most strongly associated with squamous The OR for any malignancy was higher in white cell carcinoma (Fig 2).
Fig 1.
Distribution of malignancy among patients with pruritus. A, Breakdown of malignancy diagnoses among patients ≥18 years of age who received a diagnosis of pruritus and malignancy at Johns Hopkins Health System during 2013–2017 (n = 2903).
B, Breakdown of hematologic malignancies among pruritus patients. The non-Hodgkin lymphoma group excludes primary cutaneous lymphomas, which are considered separately.
C, Breakdown of dermatologic malignancies among pruritus patients. GI, Gastrointestinal.
*Noncutaneous.
Fig 2.
Association between pruritis and malignancy. Prevalence of malignancy among patients with pruritus (blue) compared with patients without pruritus (gray) in the Johns Hopkins Health System population. ORs and 95% CIs for each malignancy type are tabulated. *P <.001 (chi-squared test). CI, Confidence interval; GI, gastrointestinal; OR, odds ratio.
Racial differences in pruritus and malignancy
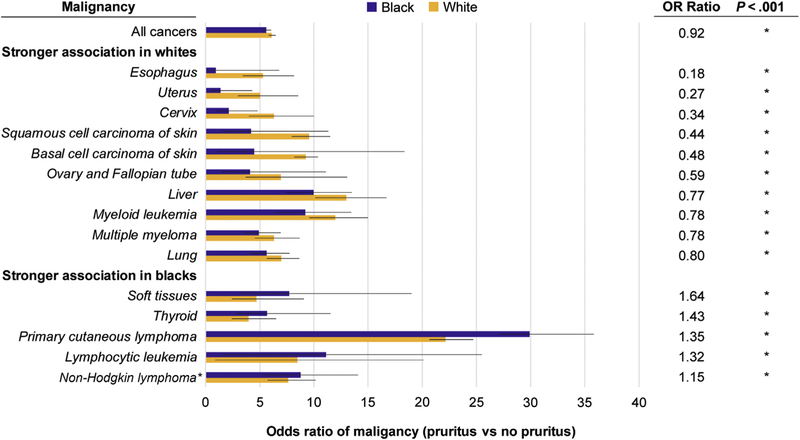
The OR for any malignancy was higher in white patients with pruritus (OR 6.12, 95% CI 5.81–6.46) than black patients with pruritus (OR 5.61, 95% CI 5.21–6.04) (P <.001). In addition, there were racial differences in the associations between pruritus and specific cancer subtypes (Fig 3). Compared with white patients with pruritis, black patients with pruritus had lower ORs for malignancies of the liver, skin, respiratory tract, gastrointestinal tract, and female genital organs. Black persons with pruritus had higher ORs for hematologic and soft tissue malignancies (including muscle, fat, and peripheral nerves). Among hematologic malignancies, black persons with pruritus had higher ORs for primary cutaneous lymphoma, noncutaneous non-Hodgkin lymphoma, and lymphocytic leukemia and lower ORs for myeloid leukemia and multiple myeloma than white persons with pruritus (Fig 3).
Fig 3.
Racial/ethnic differences in association between pruritus and malignancy. ORs for malignancies (patients with pruritus vs patients without pruritus) in black patients (blue) and white patients (orange) in the Johns Hopkins Health System population. Only malignancies in which there was a statistically significant difference between the ORs for black and white patients are included. Error bars represent 95% confidence intervals. The ratios of the ORs (black/white) are tabulated on the right. *P <.001 (z test). OR, Odds ratio.
Skin eruption in pruritus patients with malignancy
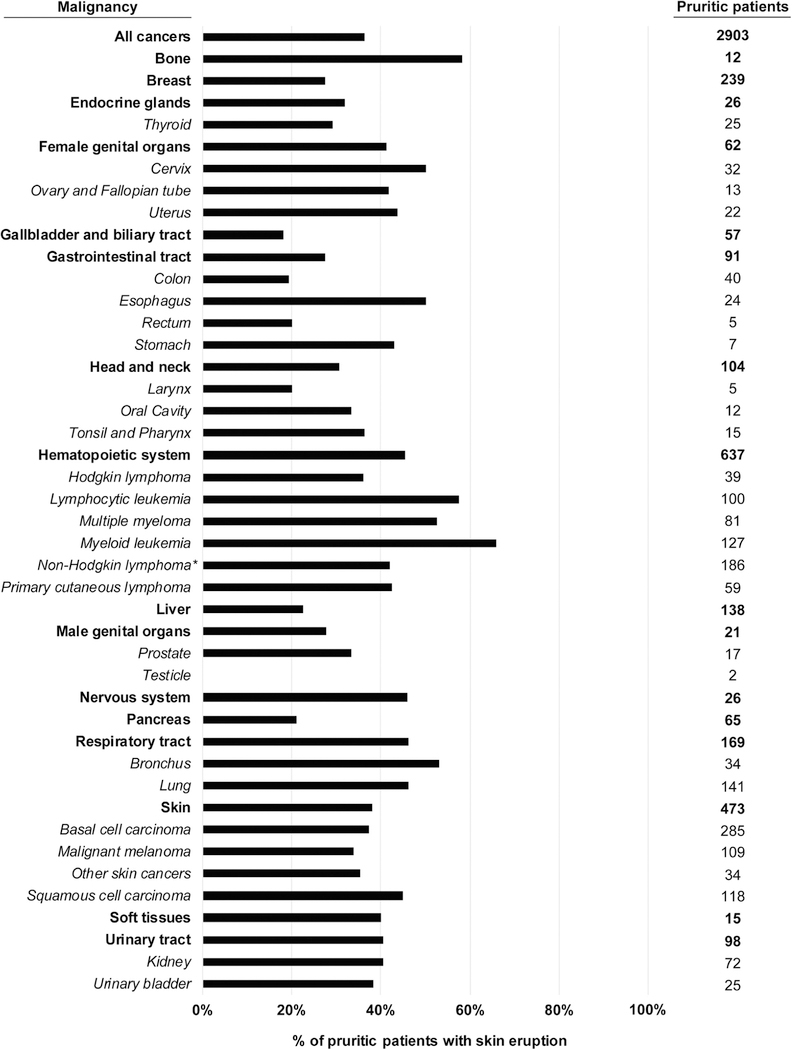
To further characterize the nature of pruritus in patients with malignancy, those patients with a concomitant skin eruption were identified. Of 16,925 patients with pruritus diagnoses given at JHHS during 2013–2017, 31% had a documented skin eruption. Of the 2,903 patients with both pruritus and a malignancy, 36% had a documented skin eruption. The rate of skin eruption among patients with different malignancies was variable (Fig 4). The malignancies with the lowest rate of skin eruption included gallbladder and biliary tract (18%), colon (19%), pancreas (21%), and liver (23%). Those with the highest prevalence of skin eruption included myeloid leukemia (66%), bone tumors (58%), lymphocytic leukemia (57%), bronchial malignancies (53%), and multiple myeloma (53%). Overall, hematologic malignancies with pruritus were accompanied by a skin eruption in 45% of cases.
Fig 4.
Skin eruptions in patients with pruritus and malignancy. Prevalence of skin eruption among patients with pruritus and a diagnosis of malignancy during 2013–2017 (n = 2903).
DISCUSSION
In this study, we demonstrate that patients who present with pruritus at a tertiary care center have an increased likelihood of concomitant malignancy compared with nonpruritic patients. Our findings are in agreement with literature showing an association of pruritus with malignancies of the liver, biliary system, skin, and hematopoietic system2–8; these malignancies were the most strongly associated with pruritus in our cohort.
We also show a stronger association with a wider variety of cancers than have been previously reported.4,5 The main difference is that prior studies focused on diagnosis of malignancy after the onset of pruritus, while our study includes malignancies diagnosed before or after pruritus onset. These previous studies were also population-based studies with lower overall incidence of malignancy, compared with our study, which was performed at a tertiary care center and features a greater variety of represented malignancies.
We also found several notable differences between black and white pruritus patients. Among the malignancies most highly associated with pruritus, black patients with pruritus had a higher OR for hematologic malignancies than whites, while white patients had higher ORs for liver and skin malignancies than blacks.
We have shown that most patients with pruritus and malignancy diagnoses do not have a documented skin eruption. In particular, cancers affecting the biliary tract, liver, pancreas, and colon had a low rate of skin eruption. These malignancies are likely to cause pruritus through cholestasis, either due to the primary tumor or to metastases and, therefore, would not be expected to cause skin eruption. In contrast, many hematologic malignancies, particularly leukemias, were associated with higher rates of skin eruption in pruritic patients, indicating that the mechanism of pruritus might involve an inflammatory reaction in the skin.
There are several limitations to our study. First, as noted previously, given the cross-sectional design, we are unable to establish causality or temporality between the diagnosis of pruritus and malignancy, so we cannot draw conclusions about the predictive value of pruritus in detecting malignancy. Second, the rate of malignancy that we detect in pruritus patients might not be generalizable to the general population, as this population is reflective of a tertiary referral center. Third, the pruritus group was predominantly women and contained a higher proportion of black patients compared with the nonpruritus group, which could confound the total population analysis. Fourth, in the case of skin cancers, the association with pruritus might be confounded by the fact that patients with skin cancer are seen by dermatologists, and dermatologists are more likely to diagnose and document findings of pruritus. Last, there might be additional unknown confounders, such as differences in socioeconomic status or medical comorbidities, in the pruritus group that could explain the differences in malignancy diagnoses.
We conclude that pruritus is associated with a wide variety of malignancies, including hematologic, dermatologic, and solid organ tumors. With regard to racial/ethnic differences, black persons were more likely to have soft tissue, dermatologic, and hematologic malignancies and less likely to have liver, respiratory, gastrointestinal, and gynecologic malignancies. The prevalence of skin eruption is variable by malignancy type and points to differing underlying mechanisms of pruritus.
CAPSULE SUMMARY.
Pruritus has been associated with underlying malignancy. This article provides a comprehensive analysis of the association between pruritus and a diverse array of malignancies, with additional stratification by race.
Knowledge of this association can guide clinicians in pursuing a malignancy workup for patients with unexplained pruritus.
Abbreviations used:
- CI
confidence interval
- JHHS
Johns Hopkins Health System
- OR
odds ratio
- SNOMED-CT
systematized nomenclature of medicine-clinical terms
Footnotes
Conflicts of interest: Dr Kwatra is an advisory board member for Menlo and Trevi Therapeutics. All other authors have no conflicts of interest to disclose.
REFERENCES
- 1.Kilic A, Gül Ü, Soylu S. Skin findings in internal malignant diseases. Int J Dermatol. 2007;46(10):1055–1060. [DOI] [PubMed] [Google Scholar]
- 2.Gobbi PG, Attardo-Parrinello G, Lattanzio G, Rizzo SC, Ascari E. Severe pruritus should be a B-symptom in Hodgkin’s disease. Cancer. 1983;51(10):1934–1936. [DOI] [PubMed] [Google Scholar]
- 3.Rubenstein M, Duvic M. Cutaneous manifestations of Hodgkin’s disease. Int J Dermatol. 2006;45(3):251–256. [DOI] [PubMed] [Google Scholar]
- 4.Fett N, Haynes K, Propert KJ, Margolis DJ. Five-year malignancy incidence in patients with chronic pruritus: a population-based cohort study aimed at limiting unnecessary screening practices. J Am Acad Dermatol. 2014; 70(4):651–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johannesdottir SA, Farkas DK, Vinding GR, et al. Cancer incidence among patients with a hospital diagnosis of pruritus: a nationwide Danish cohort study. Br J Dermatol. 2014;171(4):839–846. [DOI] [PubMed] [Google Scholar]
- 6.Mills KC, Kwatra SG, Feneran AN, et al. Itch and pain in nonmelanoma skin cancer: pain as an important feature of cutaneous squamous cell carcinoma. Arch Dermatol. 2012; 148(12):1422–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vij A, Duvic M. Prevalence and severity of pruritus in cutaneous T cell lymphoma. Int J Dermatol. 2012;51(8): 930–934. [DOI] [PubMed] [Google Scholar]
- 8.Ingis DA, Farmer RG. Adenocarcinoma of the bile ducts: relationship of anatomic location to clinical features. Am J Dig Dis. 1975;20(3):253–261. [DOI] [PubMed] [Google Scholar]