Abstract
Background
Depression, anxiety, and pain catastrophizing have been associated with worse pain and function in studies of patients with de Quervain’s tenosynovitis. Illness perceptions are the patient’s thoughts and feelings about their illness. More negative perceptions of the illness such as the illness having a long duration or serious consequences are associated with worse physical function in patients with hand osteoarthritis. It is currently unknown whether these psychological factors play a similar role in de Quervain’s. We chose to study patients who have tried nonoperative management and have chosen surgical decompression due to persistent symptoms. Psychological factors may be associated with their ongoing pain and impaired function, so it is particularly important to investigate the role of psychosocial factors that may be targeted with non-invasive interventions.
Questions/purposes
Which psychological variables are independently associated with baseline pain and function in patients undergoing surgical treatment for de Quervain’s tenosynovitis, after controlling for clinical and demographic variables?
Methods
This cross-sectional study included data from a longitudinally maintained database on 229 patients who had surgery for de Quervain’s tenosynovitis between September 2017 and October 2018. All management options were discussed with patients, but many had already tried nonoperative management and chose surgery once referred to our institution. Our database included 958 patients with de Quervain’s, with 69% (659) managed nonoperatively and 34% (326 of 958) who underwent surgical decompression. A total of 70% (229 of 958) completed all questionnaires and could be included in the study. With the numbers available, we found no differences between those included and those not analyzed in terms of age, gender, duration of symptoms, BMI, smoking status, and workload.
Patients completed the Patient-Rated Wrist/Hand Evaluation (PRWHE), Patient Health Questionnaire for emotional distress, Pain Catastrophizing Scale (PCS), and the Brief Illness Perception Questionnaire. We investigated the relative contribution of patient demographics and individual psychosocial factors using a hierarchical multivariable linear regression model. In the first step we considered how demographic factors were associated with the baseline PRWHE score. In the second step we investigated the effect of pain catastrophizing and emotional distress on the baseline PRWHE score after accounting for confounding demographic factors. In the final step, the effect of illness perceptions on baseline PRWHE were considered after accounting for the confounding effects of demographic factors as well as pain catastrophizing and emotional distress.
Results
After controlling for confounding variables including workload and emotional distress, a more negative patient perception of the consequences of their condition and worse pain catastrophizing were associated with worse pain and function (consequences, β = 0.31; p < 0.01, pain catastrophizing β = 0.17; p = 0.03). A hierarchical multivariable regression analysis found that 11% of variance in baseline pain and function was explained by pain catastrophizing and emotional distress. Illness perceptions brought the total explained variance of the final model to 34%.
Conclusions
More negative perceptions of the consequences of de Quervain’s tenosynovitis and worse pain catastrophizing are associated with worse pain and reduced function at baseline in patients awaiting surgical decompression of de Quervain’s tenosynovitis. In light of these findings, future studies might explore interventions to reduce pain catastrophizing and lower the perceived consequences of the condition. This may reduce the number of patients choosing surgical decompression or may also improve surgical outcomes. Further work should consider if these psychological factors are also associated with postoperative patient-reported outcomes.
Level of Evidence Level
III, therapeutic study.
Introduction
De Quervain’s tenosynovitis is an idiopathic condition characterized by pain on the radial (thumb) side of the wrist. Treatment options include NSAIDs, orthoses, corticosteroid injections, and surgery. Although most patients start with nonoperative management, some may undergo surgical decompression if their symptoms do not resolve. However, dissatisfaction rates with surgery are as high as 19% [16], with complication rates of up to 8% [9, 10, 25].
Studies have shown that emotional distress affects patient-reported outcome measures of patients with de Quervain’s tenosynovitis [7, 21, 22]. In cross-sectional studies of patients with de Quervain’s tenosynovitis, worse baseline pain and function correlated with symptoms of depression, pain catastrophizing, kinesiophobia, and pain-related anxiety [7, 21, 22]. A stepwise regression analysis showed that pain catastrophizing accounted for the greatest proportion of variability in DASH scores [7]. Furthermore, the patient’s perception of his or her condition is known to influence outcomes like pain and function [2]. Illness perceptions are the thoughts and feelings of the patient about their illness [6]; more negative perceptions of the illness, such as a long duration or having serious consequences are associated with worse disability in patients with hand osteoarthritis [5].
Although it is accepted that psychological aspects play a similar role in all hand conditions, a large number of patients are needed to study the relationship between psychosocial factors and most orthopaedic conditions. However, de Quervain’s tenosynovitis is a condition where psychological factors seem to be more commonly coincident, and because of this, smaller cohorts are sufficient for study. In addition, particular to this study, there is evidence that suggests that in many cases, de Quervain’s tenosynovitis is self-resolving and the decision to undergo surgery may have a stronger relationship to psychological factors than other surgeries [19, 20, 24].
We chose to study patients who elect to undergo surgical decompression due to persistent symptoms because psychological factors may be associated with their ongoing pain and impaired function. It is particularly important to investigate the role of these psychosocial factors that may be targeted with noninvasive interventions, as some patients who are refractory to conservative treatment may not benefit from surgery alone or may benefit from intervention without undergoing surgery.
Therefore, we asked: Which psychological variables are independently associated with baseline pain and function in patients undergoing surgical treatment for de Quervain’s tenosynovitis, after controlling for clinical and demographic variables?
Patients and Methods
Study Design
This was a cross-sectional study that used data from a longitudinally maintained electronic database of patients at Xpert Clinic and Handtherapie Nederland, comprising 18 outpatient clinics for hand surgery and therapy in the Netherlands. Patients were invited to be part of a routine outcome measurement system after the first consultation with a surgeon. If they agreed, they received web-based questionnaires at baseline and follow-up after interventions. The study was performed between September 2017 and October 2018 and was approved by the local medical research ethical committee (NL/sl?MEC-2018-1088). All patients gave informed consent for anonymized analysis of their data.
Participants
We included all adult patients with a diagnosis of de Quervain’s tenosynovitis who elected to undergo surgical treatment. Xpert Clinic and Handtherapie Nederland receive referrals from many sources, and usually patients undergo a period of nonoperative management for de Quervain’s before referral. Upon initial presentation to our system, doctors present all management options, and in general offer a steroid injection and splint to see if this improves symptoms over the next 6 weeks. However, if this fails or patients do not wish further nonoperative management, surgical decompression is offered. In light of previous nonoperative management, a relatively large proportion choose surgical decompression.
Our database included 985 patients who were seen with a diagnosis of de Quervain’s tenosynovitis during the study period. Of these, 67% of patients (659 of 985) were managed with nonoperative treatment, and 33% (326 of 985) were managed with surgical decompression (Fig. 1). Although we have a routine outcome measurement system, not all patients chose to complete the questionnaires. At baseline, 81% of patients (263 of 326) completed the baseline Patient-Rated Wrist/Hand Evaluation (PRWHE) questionnaire, but only 70% (229 of 326) completed all questionnaires. Therefore, we included 229 patients in this study.
Fig. 1.
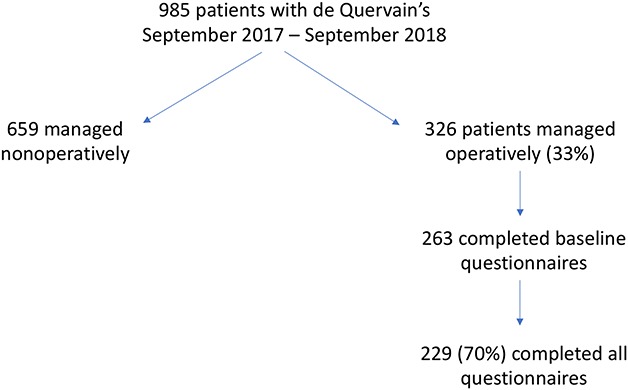
Flow diagram shows the patients in the study.
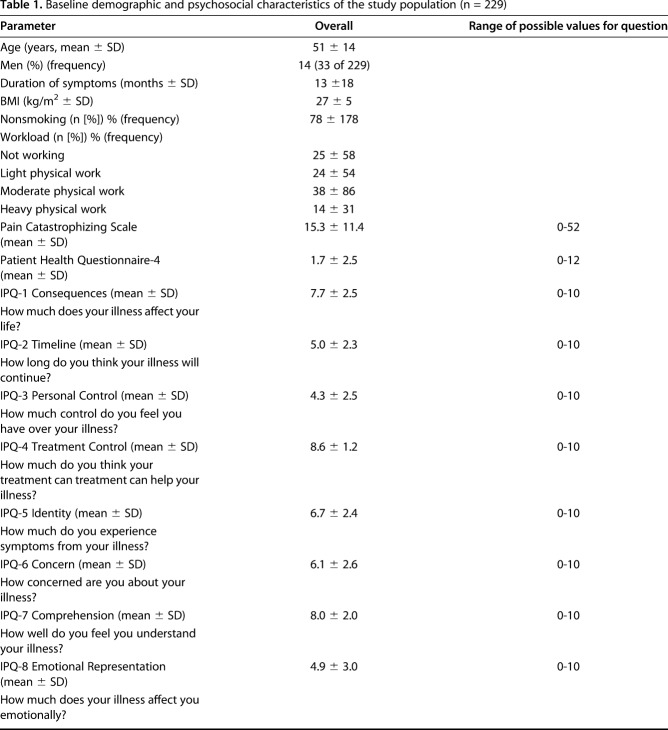
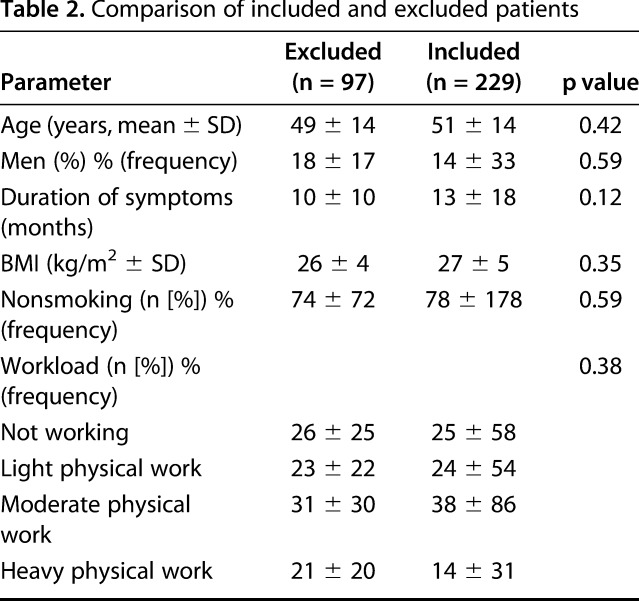
The mean age of our study patients was 51 ± 14 years and 86% (196 of 229) were women. They reported symptoms lasting an average of 13 ± 18 months and 78% (178 of 229) were currently non-smokers (Table 1). We compared the demographic factors of those included in the study with those who were not included to see if there were any differences between them (Table 2). With the numbers available, we found no differences between those included and those not analyzed in terms of age, gender, duration of symptoms, BMI, smoking status and workload.
Table 1.
Baseline demographic and psychosocial characteristics of the study population (n = 229)
Table 2.
Comparison of included and excluded patients
Variables and Study Outcomes
Study data were collected and managed using GEneric Medical Survey Tracker (Erasmus MC, Netherlands) electronic data capture tools. GEneric Medical Survey Tracker is a secure internet-based application for distributing questionnaires and forms during medical research and quality registrations.
We collected demographic variables (age, gender, reported duration of symptoms, BMI, smoking status, and workload) for all patients. Nonsmoking status meant the patient was currently a nonsmoker. Patient’s self-classified work status as not working, light physical work such as office work, moderate physical work such as working in a shop, or heavy physical work (for example, construction work).
We measured baseline pain and function with the PRWHE [18]. The PRWHE is a validated questionnaire for hand and wrist problems and consists of 15 questions: five for pain and 10 for function. Both subscales are rated on a scale from 0 (no pain or disability) to 50 (severe pain or disability), and the total score is calculated as the sum of both subscales. In this study, we used the validated Dutch translation of the PRWHE [28].
Additionally, we asked patients to complete three psychological questionnaires. To assess emotional distress, we used the Patient Health Questionnaire (PHQ-4). This questionnaire consists of two questions about depression and two about anxiety, and results in a score from 0 (no anxiety or depression) to 12 (severe anxiety and depression) [14]. The items of the PHQ-4 are made up of the PHQ-2 (the 2-item version of the PHQ-9) measuring depression and the GAD-2 measuring anxiety (the 2-iteam version of the GAD-7). Although the combination of these two scales (PHQ-4) has not been specifically validated in Dutch, the two subscales have [8, 30].
The Pain Catastrophizing Scale (PCS) comprises 13 questions that ask about rumination, magnification, and helplessness with respect to pain [4, 26]. The total score is calculated on a scale from 0 (no pain catastrophizing) to 52 (severe pain catastrophizing).
The Brief Illness Perceptions Questionnaire (B-IPQ) consists of eight questions scored on a 0 to 10 scale to measure how patients perceive their illness [3]. For questions about how much control (Personal Control) patients feel they have over their illness, how well they understand their illness (Comprehension), and how much they think their treatment will help their illness (Treatment Control), a higher score is better. For all other questions, a higher score indicates more-negative illness perceptions. This includes questions about how much illness affects their life (Consequences), how long they expect their illness to last (Timeline), how often they have symptoms because of their hand condition (Identity), how concerned they are (Concern), and how much their illness affects them emotionally (Emotion).
Study Size
We performed a power calculation for a multiple linear model with 20 covariates to determine the sample size. With a power of 0.8 and a significance level of 0.05, we needed at least 119 patients to detect a medium effect size (f 0.15) of expectations, illness perceptions, or psychological distress on outcomes. This calculation was made a priori to the database query and allowed us to determine if studying 1 year of patients treated with surgery for de Quervain’s tenosynovitis would be sufficient.
Statistical Analysis
We analyzed the baseline pain and function in terms of the PRWHE score. We performed univariable analyses to investigate the associations between all patient demographic and psychosocial variables and the baseline PRWHE score (see Table, Supplemental Digital Content 1, http://links.lww.com/CORR/A235).
We investigated the relative contribution of patient demographics and individual psychosocial factors using a hierarchical multivariable linear regression model. In this analysis, variables were added to the model in stages. After each step, we calculated the explained variance (r2). The difference in r2 between two steps was the relative contribution of the set of variables to the baseline PRWHE score. In this study, we started the model by adding patient demographics. In the second step, the PCS and PHQ-4 were entered into the model. In the final step, illness perceptions were added to the model.
All assumptions of the linear model were investigated for any possible biases. A p value of 0.05 or lower was considered statistically significant. All analyses were performed using R, version 3.4.4 (R Foundation, Vienna, Austria).
Results
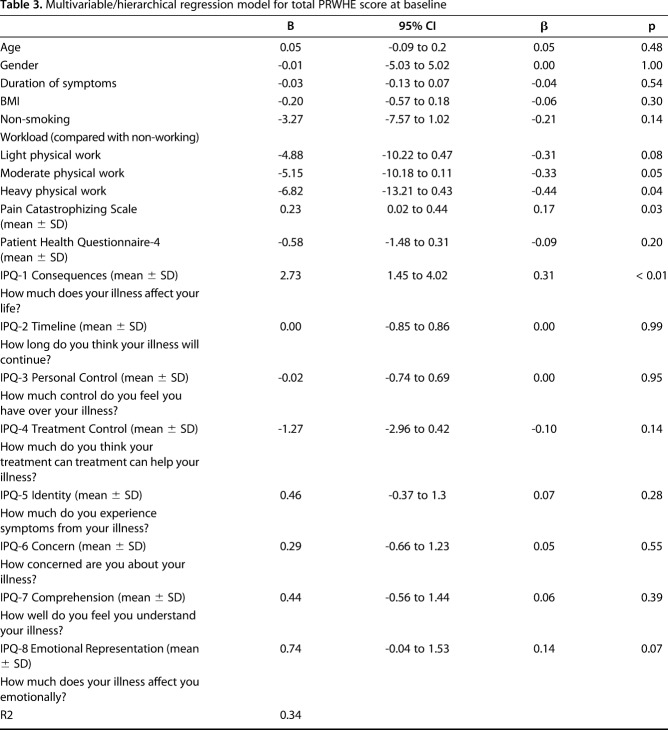
Patients who perceived more severe consequences from their condition (that is, worse IPQ-1 scores about Consequences) were likely to have modestly more severe pain and somewhat poorer function than patients with better IPQ-1 scores, even after we controlled for clinical, demographic and psychological variables like age, duration of symptoms, workload and pain catastrophizing. (Consequences include answers to such questions as “How much does your illness affect your life?” B = 2.73 [95% CI 1.45 to 4.02], ß = 0.31, p < 0.01). Patients who reported worse pain catastrophizing were likely to have worse pain and function than patients with better PCS scores, even after we controlled for clinical and demographic variables like gender and smoking status (B = 0.23 [95% CI 0.02 to 0.44], ß = 0.17, p = 0.03) (Table 3).
Table 3.
Multivariable/hierarchical regression model for total PRWHE score at baseline
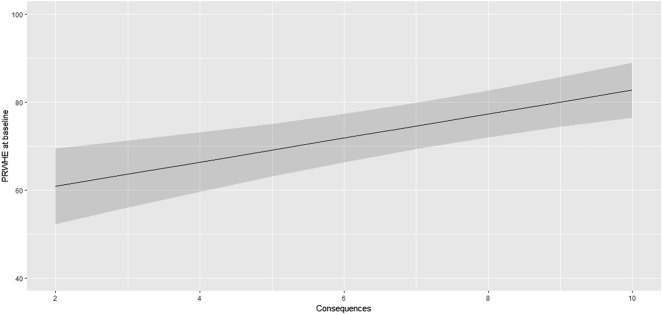
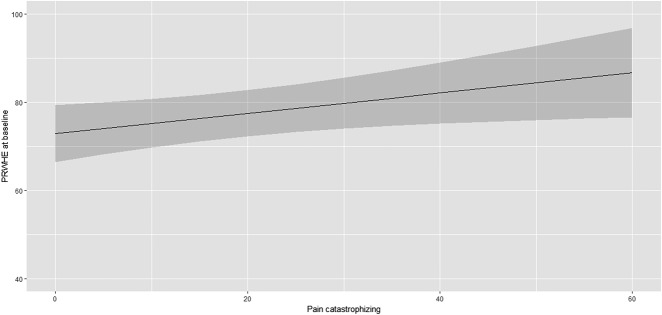
After controlling for confounding variables such as age, duration of symptoms and workload, we found that higher scores of perceptions of negative consequences were associated with lower PRWHE scores by about one-third magnitude (ß = 0.31). Similarly, higher pain catastrophizing scores were also associated with lower PRWHE scores of about one-fifth magnitude (ß = 0.17). Further, they were associated with a 0.31 SD worse PRWHE score (Fig. 2), whereas one SD increase in pain catastrophizing was associated with a 0.17 SD worse PRWHE score (Fig. 3). Our analysis showed that patient characteristics such as age, gender, and smoking status explained 7% of variance in baseline pain and function. Patients who were more prone to pain catastrophizing and who had emotional distress had poorer function and worse pain; these factors explained an additional 11% of variance in baseline pain and function, after having controlled for demographic and clinical confounding factors, such as gender and workload. We found that the more negative a patient’s perception of their condition, the worse their baseline pain and function; these factors explained an additional 16% of variance, after having controlled for demographic and clinical confounding factors as well as emotional distress and pain catastrophizing. The total explained variance of the final model was 34% (see Table, Supplemental Digital Content 2, http://links.lww.com/CORR/A236) with patient characteristics such as workload, psychological factors such as pain catastrophizing and a more negative perception of their condition associated with worse baseline pain and function.
Fig. 2.
This graph displays how a patient’s perception of the consequences of his or her de Quervain’s tenosynovitis (IPQ-1) is associated with the Patient-rated Wrist/Hand
Evaluation (PRWHE) score at baseline, corrected for patient characteristics and other psychosocial factors. The graph also shows the 95% CI of this association.
Fig. 3.
This graph displays how a patient’s pain catastrophizing is associated with the Patient-rated Wrist/Hand Evaluation (PRWHE) score at baseline, corrected for patient characteristics and other psychosocial factors. The graph also shows the 95% CI of this association.
Discussion
Psychological factors are associated with worse baseline pain and function scores in de Quervain’s tenosynovitis [7, 21, 22]. Some surgeons feel that de Quervain’s tenosynovitis is self-resolving and surgical release is discretionary; subsequently, psychological factors may be strongly related to why some patients elect surgery and some do not. In our cohort, patients with worse pain catastrophizing and more negative perceptions of the consequences of their condition (that is, higher scores in the IPQ-1 Consequences: How much does your illness affect your life?) were more likely to have worse baseline pain and function. Therefore, understanding pain catastrophizing and the perception of consequences of the condition, may help patients decide whether to engage in psychological interventions, elect surgical treatment, or both. In addition, this understanding may improve our ability to help reduce the dissatisfaction rates after de Quervain’s release and offer other interventions for those who are dissatisfied postoperatively.
This study had a number of limitations. First, because our study was cross-sectional in design, it was not possible to determine the direction of the association between psychological variables and baseline pain and function. Worse pain may lead to more negative illness perceptions and pain catastrophizing, or the association may arise because these patients are undergoing nonoperative treatment without pain relief and as a consequence, they feel more anxiety and worry. Second, our model explains 34% of the variance in baseline pain and function, suggesting that other unmeasured factors may play a role as well. Other psychological factors found to influence baseline pain and function in studies of patients with de Quervain’s tenosynovitis include kinesiophobia [7] and anxiety about pain [7, 22]. In a study of 319 patients with upper limb conditions, a multivariable model of gender, diagnosis, employment status, pain catastrophizing, and kinesiophobia explained 55% of the variance in disability [7]. However, diagnosis appeared to explain a large amount of the variation in their study; this may clarify why the 55% variance differs from the contribution of variance we found in our study of patients with only de Quervain’s tenosynovitis. Third, only 70% of our patient group completed all questionnaires. There were no apparent differences between those who completed questionnaires and those who did not (Table 2). However, it is unclear whether the group that chose not to complete the questionnaires had greater or less negative perception or pain catastrophizing, which could affect the strength of the associations we identified [9, 10, 12, 13, 15-17, 24, 25, 27, 29].
Fourth, a high proportion of our patients opted for surgical decompression (33%). This is higher than other studies, with proportions that varied between 0 and 25% [11, 13]. Because of the referral nature of our practice, some of the results may not be generalizable to other practices because the group studied may select those with greater degrees of pain catastrophizing or a more negative perception of consequences.
A more negative perception of the consequences of their condition by a patient was associated with worse baseline pain and function scores. In our cohort of patients who elected surgery, more pain catastrophizing was associated with poorer baseline function and worse pain. A cross-sectional study of patients with upper extremity problems, including de Quervain’s tenosynovitis, found that in a multivariable analysis, pain catastrophizing accounted for the greatest proportion of variation in disability [7]. In prospective randomized controlled trials that involved patients with de Quervain’s tenosynovitis, baseline pain catastrophizing was also associated with pain and function after treatment, including use of a splint [20] or steroid injection [19]. In studies of rheumatoid arthritis, these worries about one’s health condition were associated with worse quality of life [1]. However, these worries are modifiable: A randomized controlled trial found that an intervention targeting patient perceptions of the consequences of myocardial infarction changed illness perceptions and hastened patients’ return to work [23]. Similarly, targeting an intervention at improving patient perceptions of the consequences of de Quervain’s may reduce pain and improve function.
Conclusions
Overall, in patients who elected surgery for de Quervain’s tenosynovitis, more negative perceptions of the consequences and worse pain catastrophizing were associated with worse pain and reduced function at pre-surgery baseline. Recognizing this association may be beneficial in two ways: Some patients may benefit from psychological intervention and avoid surgery altogether, while some patients may benefit from psychological intervention in conjunction with surgery to reduce the rate of unsatisfactory outcomes.
Acknowledgments
Julia Blackburn completed this work during a Fulbright Scholarship to do research with Dr Chen at the Hand and Arm Center and Dr Vranceanu at the Integrated Brain Health Clinical & Research Program, Massachusetts General Hospital. We thank the Royal College of Surgeons of England and the US-UK Fulbright Commission for the opportunity.
Footnotes
One of the authors certifies that he (JTP) has received a grant, during the study period, in an amount of USD 10,000 to USD 100,000 from the Netherlands Organisation for Scientific Research (The Hague, the Netherlands); and a grant, during the study period, in an amount of USD 10,000 to USD 100,000 from Medical Delta (Delft, the Netherlands).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Xpert Clinic, The Netherlands.
References
- 1.Berner C, Erlacher L, Fenzl KH, Dorner TE. A cross-sectional study on self-reported physical and mental health-related quality of life in rheumatoid arthritis and the role of illness perception. Health Qual Life Outcomes. 2018; 16:238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bethge M, Bartel S, Streibelt M, Lassahn C, Thren K. [Illness perceptions and functioning following total knee and hip arthroplasty] [in German]. Z Orthop Unfall. 2010; 148:387-392 [DOI] [PubMed] [Google Scholar]
- 3.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006; 60:631-637. [DOI] [PubMed] [Google Scholar]
- 4.Crombez G, Vlaeyen J, Heuts P, Lysens R. Pain-related fear is more disabling than pain itself: Evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999; 80:329-339. [DOI] [PubMed] [Google Scholar]
- 5.Damman W, Liu R, Kaptein AA, Evers AWM, van Middendorp H, Rosendaal FR, Kloppenburg M. Illness perceptions and their association with 2 year functional status and change in patients with hand osteoarthritis. Rheumatology (Oxford). 2018;57:2190-2199. [DOI] [PubMed] [Google Scholar]
- 6.Damman W, Liu R, Kaptein AA, Evers AWM, van Middendorp H, Rosendaal FR, Kloppenburg M. Illness perceptions and their association with 2 year functional status and change in patients with hand osteoarthritis. Rheumatology (Oxford). 2018; 57:2190-2199. [DOI] [PubMed] [Google Scholar]
- 7.Das De S, Vranceanu AM, Ring DC. Contribution of kinesophobia and catastrophic thinking to upper-extremity-specific disability. J Bone Joint Surg Am. 2013; 95:76-81. [DOI] [PubMed] [Google Scholar]
- 8.Donker T, van Straten A, Marks I, Cuijpers P. Quick and easy self-rating of generalized anxiety disorder: Validity of the Dutch web-based GAD-7, GAD-2 and GAD-si. Psychiatry Research. 2011; 188:58-64. [DOI] [PubMed] [Google Scholar]
- 9.Faithfull D, Lamb D. De Quervain’s disease - a clinical review. Hand. 1971; 3:23-30. [DOI] [PubMed] [Google Scholar]
- 10.Garcon JJ, Charruau B, Marteau E, Laulan J, Bacle G. Results of surgical treatment of de Quervain's tenosynovitis: 80 cases with a mean follow-up of 9.5 years. Orthop Traumatol Surg Res. 2018; 104:893-896. [DOI] [PubMed] [Google Scholar]
- 11.Kachooei A, Nota S, Menendez ME, Dyer G, Ring D. Factors associated with operative treatment of De Quervain tendinopathy. Arch Bone Jt Surg. 2015; 3:198-203. [PMC free article] [PubMed] [Google Scholar]
- 12.Kang H, Koh I, Jang J, Choi Y. Endoscopic versus open release in patients with De Quervain’s tenosynovitis. Bone Joint J. 2013; 95:947-951. [DOI] [PubMed] [Google Scholar]
- 13.Kazmers NH, Liu TC, Gordon JA, Bozentka DJ, Steinberg DR, Gray BL. Patient- and disease-specific factors associated with operative management of De Quervain tendinopathy. J Hand Surg Am. 2017; 42:931 e931-931 e937. [DOI] [PubMed] [Google Scholar]
- 14.Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: The phq-4. Psychosomatics. 2009; 50:613-621. [DOI] [PubMed] [Google Scholar]
- 15.Lamphier TA, Gilmore Long N, Dennery T. De Quervain’s disease an analysis of 52 cases. Ann Surg. 1953; 138:832-841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lapidus PW, Fenton R. Stenosing tenovaginitis at the wrist and fingers report of 423 cases in 269 patients with 354 operations. AMA Arch Surg. 1952; 64:475-487. [DOI] [PubMed] [Google Scholar]
- 17.Lee H-J, Kim P-T, Aminata I, Hong H-P, Yoon J-P, Jeon I-H. Surgical release of the first extensor compartment for refractory De Quervain’s tenosynovitis: Surgical findings and functional evaluation using DASH scores. Clin Orthop Surg. 2014; 6:405-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: A reliable and valid measurement tool. J Orthop Trauma. 1998; 12:577-586. [DOI] [PubMed] [Google Scholar]
- 19.Makarawung DJ, Becker SJ, Bekkers S, Ring D. Disability and pain after cortisone versus placebo injection for trapeziometacarpal arthrosis and de Quervain syndrome. Hand (N Y). 2013; 8:375-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Menendez ME, Thornton E, Kent S, Kalajian T, Ring D. A prospective randomized clinical trial of prescription of full-time versus as-desired splint wear for de Quervain tendinopathy. Int Orthop. 2015; 39:1563-1569. [DOI] [PubMed] [Google Scholar]
- 21.Molleman J, Janssen SJ, Overbeek CL, Ring D. A threshold disability score corresponds with an estimated diagnosis of clinical depression in patients with upper extremity disease. Hand (N Y). 2015; 10:168-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niekel MC, Lindenhovius AL, Watson JB, Vranceanu AM, Ring D. Correlation of DASH and QuickDASH with measures of psychological distress. J Hand Surg Am. 2009; 34:1499-1505. [DOI] [PubMed] [Google Scholar]
- 23.Petrie KJ, Cameron LD, Ellis CJ, Buick D, Weinman J. Changing illness perceptions after myocardial infarction: An early intervention randomized controlled trial. Psychosom Med. 2002; 64:580-586. [DOI] [PubMed] [Google Scholar]
- 24.Ring D, Schnellen A. Patient-centered care of De Quervain's disease. J Hand Microsurg. 2009; 1:68-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scheller A, Schuh R, Honle W, Schuh A. Long-term results of surgical release of de quervain's stenosing tenosynovitis. Int Orthop. 2009; 33:1301-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: Development and validation. Psychol Assess. 1995; 7:524. [Google Scholar]
- 27.Ta KT, Eidelman D, Grant Thomson J. Patient satisfaction and outcomes of surgery for De Quervain’s tenosynovitis. J Hand Surg Am. 1999; 24:1071-1077. [DOI] [PubMed] [Google Scholar]
- 28.Videler A, Schreuders T. [The Netherlands version of the Patient Rates Wrist/Hand Evaluation]. [in Dutch] Nederlands tijdschrift voor Handtherapie. 2008; 17:8-11. [Google Scholar]
- 29.Younghusband O, Black J., De Quervain’s disease: Stenosing tenovaginitis at the radial styloid process. Can Med Assoc J. 1963; 89:508-512. [PMC free article] [PubMed] [Google Scholar]
- 30.Zuithoff N, Vergouwe Y, King M, Nazareth I, van Wezep M, Moons K, Geerling M. The patient health questionnaire-9 for detection of major depressive disorder in primary care: Consequences of current thresholds in a crossectional study. BMC Family Practice. 2010; 11:98-104. [DOI] [PMC free article] [PubMed] [Google Scholar]