Abstract
Background
Osteosynthesis of distal clavicle fractures can be challenging because of comminution, poor bone quality, and deforming forces at the fracture site. A better understanding of regional differences in the bone structure of the distal clavicle is critical to refine fracture fixation strategies, but the variations in BMD and cortical thickness throughout the distal clavicle have not been previously described.
Purpose
/questions (1) Which distal clavicular regions have the greatest BMD? (2) Which distal clavicular regions have the greatest cortical thickness values?
Methods
Ten distal clavicle specimens were dissected from cadaveric shoulders. Eight specimens were female and two were male, with a mean (range) age of 63 years (59 to 67). The specimens were selected to match known epidemiology, as distal clavicular fractures occur more commonly in older patients with osteoporotic bone, and clavicular fractures in older patients are more common in females than males. The clavicles were then imaged using quantitative micro-CT to create 3-D images. The BMD and cortical thickness were calculated for 10 regions of interest in each specimen. These regions were selected to represent locations where distal clavicular fractures commonly occur and locations of likely bony comminution. Findings were compared between different regions using repeated measures ANOVA with Geiser-Greenhouse correction, followed by Bonferroni method multiple comparison testing. Effect size was also calculated to estimate the magnitude of difference between regions.
Results
The four most medial regions of the distal clavicle contained the greatest BMD (anterior intertubercle space 887 ± 31 mgHA/cc, posterior intertubercle space 879 ± 26 mgHA/cc, anterior conoid tubercle 900 ± 21 mgHA/cc, posterior conoid tubercle 896 ± 27 mgHA/cc), while the four most lateral regions contained the least BMD (anterior lateral distal clavicle 804 ± 32 mgHA/cc, posterior lateral distal clavicle 800 ± 38 mgHA/cc, anterior medial distal clavicle 815 ± 27 mgHA/cc, posterior medial distal clavicle 795 ± 26 mgHA/cc). All four most medial regions had greater BMD than the four most lateral regions, with p < 0.001 for all comparisons. For the BMD ANOVA, η2 was determined to be 0.81, representing a large effect size. The four most medial regions of the distal clavicle also had the greatest cortical thickness (anterior intertubercle space 0.7 ± 0.2 mm, posterior intertubercle space 0.7 ± 0.3 mm, anterior conoid tubercle 0.9 ± 0.2 mm, posterior conoid tubercle 0.7 ± 0.2 mm), while the four most lateral regions had the smallest cortical thickness (anterior lateral distal clavicle 0.2 ± 0.1 mm, posterior lateral distal clavicle 0.2 ± 0.1 mm, anterior medial distal clavicle 0.3 ± 0.1 mm, posterior medial distal clavicle 0.2 ± 0.1 mm). All four most medial regions had greater cortical thickness than the four most lateral regions, with p < 0.001 for all comparisons. For the cortical thickness ANOVA, η2 was determined to be 0.80, representing a large effect size. No differences in BMDs and cortical thicknesses were found between anterior and posterior regions of interest in any given area.
Conclusions
In the distal clavicle, BMD and cortical thickness are greatest in the conoid tubercle and intertubercle space. When compared with clavicular regions lateral to the trapezoid tubercle, the BMD and cortical thickness of the conoid tubercle and intertubercle space were increased, with a large magnitude of difference.
Clinical Relevance
Distal clavicular fractures are prone to comminution and modern treatment strategies have centered on the use of locking plate technology and/or suspensory fixation between the coracoid and the clavicle. However, screw pullout or cortical button pull through are known complications of locking plate and suspensory fixation, respectively. Therefore, it seems intuitive that implant placement during internal fixation of distal clavicle fractures should take advantage of the best-available bone. Although osteosynthesis was not directly studied, our study suggests that the best screw purchase in the distal clavicle is available in the areas of the conoid tubercle and intertubercle space, as these areas had the best bone quality. Targeting these areas during implant fixation would likely reduce implant failure and strengthen fixation. Future studies should build on our findings to determine if osteosynthesis of distal clavicular fractures with targeted screw purchase or cortical button placement in the conoid tubercle and intertubercle space increase fixation strength and decreases construct failure. Furthermore, our findings provide consideration for novel distal clavicular locking plate designs with modified screw trajectories or refined surgical techniques with suspensory fixation implants to reliably capture these areas of greatest bone quality.
Introduction
Surgical treatment of distal clavicle fractures can be challenging because of comminution, poor bone quality, and deforming forces at the fracture site. Various fixation strategies have been proposed, including transacromial K-wires or Knowles pins, hook plating, tension band wiring, coracoclavicular screws, and suture repair [2, 3, 7, 10, 11, 14, 27]. Despite the wide array of treatment options, no specific treatment method has shown obvious long-term superiority. Furthermore, many of these procedures are associated with postoperative complications and a possible need for a second procedure for hardware removal [6, 15, 17, 28]. More recent approaches have included locked plating and distal clavicle-specific plates with or without coracoclavicular ligament fixation [5, 8, 9, 12, 13, 18, 21, 24]. Isolated fixation with cortical button techniques for suspensory coracoclavicular ligament fixation have also been described [25, 27]. The advantages of these osteosynthesis methods may include preservation of the acromioclavicular joint and subacromial space, both of which are violated by older hook plate designs. However, hardware failure of distal clavicular locking plates has been described, particularly in the setting of screw pullout. Brouwer et al. [4] described axial pullout of locking screws in the lateral clavicle in four cases of superior clavicular plating, a standard plating approach. Sajid et al. [22] also described cases of plate pullout after distal clavicular locked plating. The addition of suspensory coracoclavicular fixation partially alleviates this problem, but screw pullout remains a concern when performing locked plating of distal clavicular fractures, especially in the setting of poor bone quality and comminution. Furthermore, isolated coracoclavicular fixation techniques with cortical buttons also have a known risk of the implant pulling through the superior clavicular bony cortex [23].
Although there has been extensive research into novel fixation devices, no studies that we know of have quantified the regional differences in BMD and cortical thickness in the distal clavicle. Given the concerns for screw pullout in modern locked plating designs and cortical button pull through in suspensory coracoclavicular fixation techniques, knowledge of precisely which areas in the distal clavicle have greater bone stock or thicker cortices would be advantageous to surgeons, as implant placement in areas of greater bone quality decreases the likelihood of implant failure. Targeting the areas of the distal clavicle with the best bone quality during internal fixation would logically lead to increased fixation strength.
Therefore, we asked, (1) Which distal clavicular regions have the greatest BMD? (2) Which distal clavicular regions have greatest cortical thickness values?
Materials and Methods
In this study, we used 10 fresh-frozen shoulders from cadavers with a mean (range) age of 63 years (59 to 67). Two cadavers were male and eight were female. The demographics of these specimens were chosen to be representative of the known epidemiology of distal clavicular fractures. These fractures occur commonly in older age groups with osteoporotic bone, with an increase in incidence in patients older than 65 years [16]. Furthermore, beginning in the seventh decade of life and on, clavicular fractures are more common in women than men [16].
We completely dissected the soft tissue on all cadaveric shoulders and isolated the clavicles. Using a 0.60-mm microsagittal saw (CONMED, Utica, NY, USA), we cut all clavicle specimens 3 cm proximal to the conoid tubercle. No specimens had gross evidence of a deformity or fracture. All specimens were scanned using quantitative micro-CT on a microtomography scanner (vivaCT 40, Scanco Medical, Wayne, PA, USA). The resolution was 38 isometric, cubical voxels. Approximately 1024 slices were acquired for each specimen with a 200-ms integration time. The tube current was set at 145 mA and the peak tube voltage was 55 kVp.
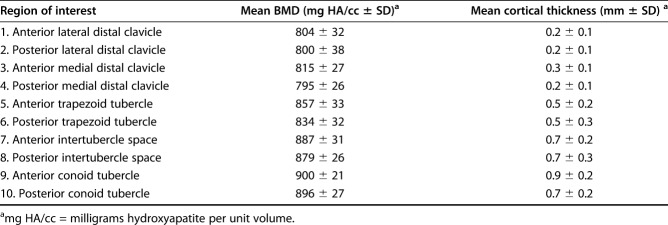
After obtaining the micro-CT images, we created 3-D of each specimen using DICOM software (Scanco 3D software, Ray V4.0, Wayne, PA, USA). Next, the cortical thickness and BMD were calculated using mathematics processing software (MATLAB, Natick, MA, USA) for 10 regions of interest (ROI) (Fig. 1). Values were calculated as an average of the whole ROI. BMD was calculated in units of milligrams of hydroxyapatite per unit volume (mgHA/cc). For each specimen, the 10 ROIs were determined by first isolating the following five areas in the distal clavicle, listed from medial to lateral: the conoid tubercle, intertubercle space (region between the conoid and trapezoid tubercles), trapezoid tubercle, and medial and lateral halves of the remaining distal clavicle. Next, the entire distal clavicle was divided into anterior and posterior halves, thereby creating an anterior and posterior ROI in each of the above-listed five areas for a total of 10 ROIs. The ROIs were then numbered from lateral to medial and from anterior to posterior (Fig. 1). The selection of where to define each ROI was based on common fracture patterns of the distal clavicle as described by Neer [19]. Briefly, distal clavicular fracture lines often occur just lateral to the coracoclavicular ligaments, between the conoid and trapezoid ligaments or medial to the conoid ligament. Furthermore, comminution is common lateral to the trapezoid tubercle. Our selected ROI represent areas of common fracture fragments and areas prone to comminution, as seen in clinical practice.
Fig. 1.
This image shows the distal clavicle regions of interest (ROI). The areas of the conoid tubercle, intertubercle space, trapezoid tubercle, and medial and distal halves of the remaining distal clavicle (distal to the trapezoid tubercle) were identified and each were divided into the anterior and posterior zones. This yielded 10 ROI that were isolated in a similar fashion in each specimen. Each anatomic ROI was assigned a number for simplicity.
Descriptive statistics for each ROI were determined using Prism 7 (GraphPad, La Jolla, CA, USA). We compared BMD and cortical thickness by ROI to determine differences by first using repeated measures ANOVA with Geiser-Greenhouse correction, followed by Bonferroni method multiple comparison testing to correct for the multiple comparisons problem. We calculated ANOVA effect size using η2, with a values > 0.25 representing a large effect size. Alpha was set at 0.05 for all statistical testing.
Results
BMD of Regions of the Distal Clavicle
The four most medial regions of the distal clavicle (ROIs 7 to 10) contained the greatest BMD (anterior intertubercle space 887 ± 31 mgHA/cc, posterior intertubercle space 879 ± 26 mgHA/cc, anterior conoid tubercle 900 ± 21 mgHA/cc, posterior conoid tubercle 896 ± 27 mgHA/cc), while the four most lateral regions (ROI 1 to 4) contained the least BMD (anterior lateral distal clavicle 804 ± 32 mgHA/cc, posterior lateral distal clavicle 800 ± 38 mgHA/cc, anterior medial distal clavicle 815 ± 27 mgHA/cc, posterior medial distal clavicle 795 ± 26 mgHA/cc) (Table 1). All four most medial regions had greater BMD than the four most lateral regions, with p < 0.001 for all comparisons (Fig. 2). Furthermore, the region of the posterior trapezoid tubercle (ROI 6) had less BMD than the regions of the posterior intertubercle space (ROI 8) and the posterior conoid tubercle (ROI 10), with both p < 0.001. There was no difference in the BMD of anterior and posterior ROIs in any given area. η2 was determined to be 0.81, representing a large effect size.
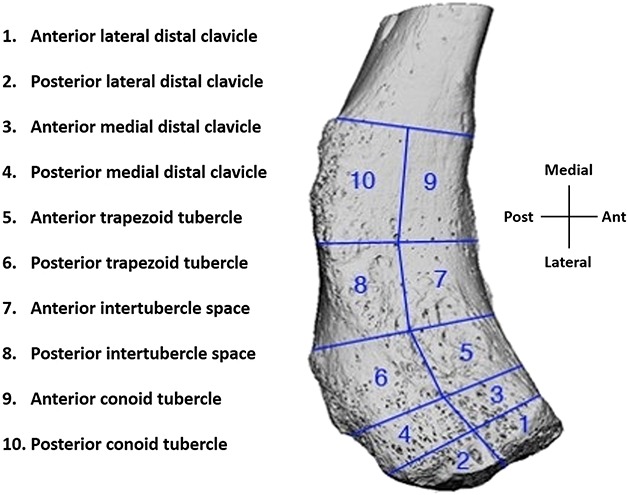
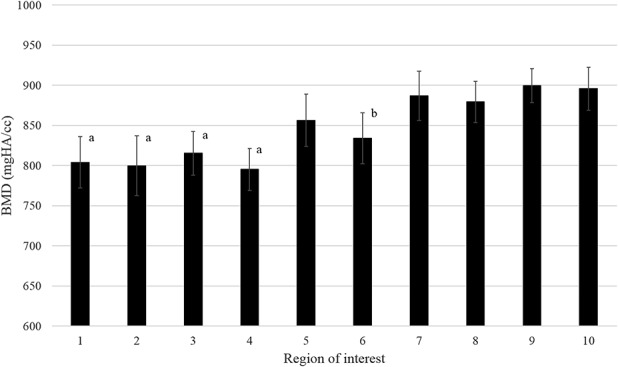
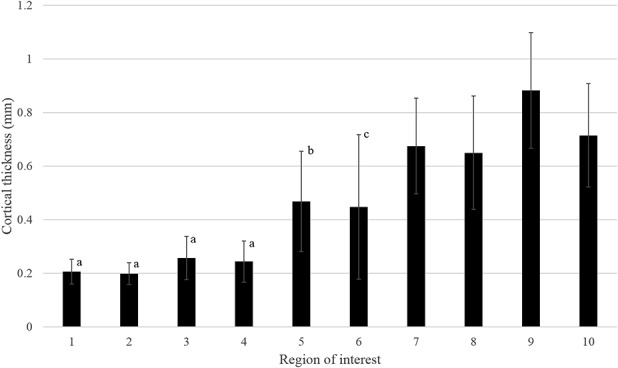
Table 1.
BMDs and cortical thicknesses of the distal clavicle
Fig. 2.
The mean BMDs (mg HA/cc) for all regions of interest (ROI) are plotted with associated SD bars. The four most-medial ROI demonstrated greater BMDs than the four most-lateral regions (p < 0.001 for all). Furthermore, ROI 8 and ROI 10 both demonstrated greater BMD than ROI 6 (p < 0.001 for both). aless dense than ROIs 7 to 10; bless dense than ROI 8 and ROI 10.
Cortical Thickness of Regions of the Distal Clavicle
Similar to our BMD findings, the four most medial regions of the distal clavicle also had the greatest cortical thickness (anterior intertubercle space 0.7 ± 0.2 mm, posterior intertubercle space 0.7 ± 0.3 mm, anterior conoid tubercle 0.9 ± 0.2 mm, posterior conoid tubercle 0.7 ± 0.2 mm), while the four most lateral regions had the smallest cortical thickness (anterior lateral distal clavicle 0.2 ± 0.1 mm, posterior lateral distal clavicle 0.2 ± 0.1 mm, anterior medial distal clavicle 0.3 ± 0.1 mm, posterior medial distal clavicle 0.2 ± 0.1 mm) (Table 1). All four most medial regions had greater cortical thickness than the four most lateral regions, with p < 0.001 for all comparisons (Fig. 3). The region of the anterior trapezoid tubercle (ROI 5) also had thinner cortical thickness than the regions of the anterior and posterior conoid tubercle (ROI 9 and 10, respectively), with both p < 0.001. Lastly, the region of the posterior trapezoid tubercle (ROI 6) had smaller cortical thickness than the region of the posterior intertubercle space (ROI 8), with p < 0.001. No differences in cortical thicknesses were found between anterior and posterior ROIs in any given area. η2 was determined to be 0.80, representing a large effect size.
Fig. 3.
The mean cortical thickness (mm) for all regions of interest (ROI) is plotted with associated SD bars. The four most-medial ROIs demonstrated greater cortical thicknesses than the four most-lateral regions (p < 0.001 for all). Furthermore, ROI 9 and ROI 10 both demonstrated greater cortical thickness than ROI 5 (p < 0.001 for both). Also, and ROI 8 demonstrated greater cortical thickness than ROI 6 (p < 0.001). athinner cortex than ROIs 7 to 10. bthinner cortex than ROI 9 and ROI 10. cthinner cortex than ROI 8.
Discussion
Fixation of distal clavicle fractures continues to challenge orthopaedic surgeons, especially in the setting of poor bone quality and comminution. Currently, locking plate technology and/or suspensory fixation with cortical buttons are often used for internal fixation of these fractures, but screw pullout or cortical button pull through remain a concern and the ideal fixation method has yet to be determined. Quantification of the areas of best and worst bone quality throughout the distal clavicle has not been previously described. Using quantitative micro-CT to characterize variations in the bone quality of the distal clavicle, we found that the areas of the conoid tubercle and intertubercle space had greater BMD and cortical thickness than the lateral-most areas of the distal clavicle. The large magnitude of difference between these areas suggests a substantial contrast in bone quality throughout the distal clavicle. As greater bone quality is directly related to better implant purchase, and given the logical goal of placing implants in the best bone available, the findings of this study could potentially help surgeons by identifying which regions of the distal clavicle to target during internal fixation to maximize fixation strength.
This study was potentially limited by certain factors. Importantly, although our findings showed differences between both BMD and cortical thickness in the four most-medial regions of the distal clavicle (areas of the conoid tubercle and intertubercle space) compared with the four most-lateral regions (area lateral to the trapezoid tubercle), the clinical relevance is yet to be determined. However, effect size calculations for BMD and cortical thickness suggest a large and substantial difference in bone quality between the different distal clavicle regions, with η2 ≥ 0.80 in both cases. We believe that these findings imply clinical relevance because, intuitively, internal fixation of distal clavicle fractures should take advantage of the best bone possible. Our study demonstrates that this area of best available bone in the distal clavicle is reliably located within the conoid tubercle and intertubercle space. Further limitations include the demographics of the selected cadavers. Most of the tested cadaveric clavicles were female (eight of 10). Although commonly an equal age distribution of tested samples would be preferred, given that distal clavicular fractures have a higher frequency in the older female population with osteoporotic bone, we believe that our selection of cadaveric samples better represents the observed epidemiology of this specific fracture type and is therefore justified. Next, the age of the cadavers ranged from 59 to 67 years, potentially skewing our findings to represent an older population. These variables could have changed the absolute values of the mean BMD and cortical thickness in each ROI. However, the age of our cadavers again matched the known epidemiology of distal clavicular fractures, which are more common in the older population. Furthermore, each specimen showed a similar relative increase in BMD and cortical thickness in the regions medial to the trapezoid tubercle when compared with the regions lateral to the trapezoid tubercle, and therefore, the relative relationship of bone quality throughout the distal clavicle would likely remain similar if other cadaver studies were to seek to replicate our study using cadaver donors of different ages.
This study found that the area of the distal clavicle containing the highest BMD and greatest cortical thickness was at least 2 cm from the lateral edge of the clavicle, in the areas of the conoid tubercle and intertubercle space. The distal clavicular bone lateral to the trapezoid tubercle demonstrated a distinct decrease in BMD and cortical thickness. Anatomically, the conoid tubercle is located approximately 4 cm proximal to the acromioclavicular joint, and the trapezoid tubercle is located around 2 cm proximal to the acromioclavicular joint [20]. The intertubercle space is therefore approximately 2 cm. Our findings showed increased BMD and cortical thickness in bone greater than 2 cm proximal to the acromioclavicular joint and decreased bone quality in the distal clavicle less than 2 cm from the acromioclavicular joint.
Given the growth of osteosynthesis options for distal clavicular fractures, an exact knowledge of the anatomic variations in bone quality along the distal clavicle would be helpful to refine implant placement and construct design. BMD measurements represent the mechanical integrity of bone [1]. Greater BMD and cortical thickness values are desirable for screw placement because they enhance screw purchase and strengthen fixation. In an osteoporotic bone model, Thiele et al. [26] demonstrated that the overall bone mass, cortical thickness, and BMD of the cortical layer are the primary factors that affect screw stability in cortical bone. Because screw purchase is dependent on bone quality, it is intuitive that to achieve greater screw purchase and decrease the likelihood of screw pullout, screws should be placed in the areas of the best bone possible. Using similar logic, cortical buttons for suspensory coracoclavicular fixation are at risk for pull through if placed in weaker bone, or areas with thinner cortices, and should also be preferentially placed in the best bone available. Our study did not specifically study osteosynthesis of distal clavicular fractures, but our findings imply that because there is substantially better bone quality in the areas of the conoid tubercle and intertubercle space, screw or cortical button placement during internal fixation of distal clavicle fractures should target these areas to achieve improved implant fixation strength. This knowledge guides appropriate plate placement during surgery to ensure that screw purchase is achieved in these areas, as well as appropriate cortical button placement to ensure that the button is not placed too laterally, in areas known to have weaker bone and thinner cortices. This study also paves the way for future innovation of locking plate designs with screw trajectories specifically positioned to ensure fixation of these areas. Future studies of distal clavicle fractures investigating the relationship between locking plate screw placement/suspensory fixation placement and fixation strength and construct failure, as well as investigation of new locking plate screw configurations, are warranted to translate our findings clinically.
From clinical experience, fractures of the very distal extent of the clavicle have a propensity for comminution, likely secondary to low BMD. Our findings suggest that clavicular fractures within 2 cm of the acromioclavicular joint are likely more difficult to successfully stabilize with a plate and screw construct because screw purchase is compromised. Given the biomechanical weakness of the bone in this area, thinking about techniques to augment fixation could be considered for these specific fractures. Potential options include acromioclavicular joint spanning techniques or coracoclavicular ligament reconstruction [8, 12, 18]. Furthermore, adjunctive measures such as cement or calcium phosphate bone void fillers may augment osteosynthesis of the distal clavicle in the most-distal 2 cm of the clavicle, given low BMD. Further studies specifically investigating these techniques in distal clavicle fractures lateral to the trapezoid tubercle are warranted.
In conclusion, the areas of the conoid tubercle and intertubercle space had the greatest BMD and cortical thickness in the distal clavicle. When compared with clavicular regions lateral to the trapezoid tubercle, the BMD and cortical thickness of the conoid tubercle and intertubercle space were increased, with a large and substantial magnitude of difference. To achieve increased fixation strength, it seems intuitive that screw or cortical button placement during internal fixation of distal clavicle fractures should take advantage of the best-available bone. Our study suggests that the best site for implant placement in the distal clavicle is available in the areas of the conoid tubercle and intertubercle space, as these locations had the best bone quality. Targeting these areas during implant fixation through deliberate plate and screw or suspensory fixation placement would likely reduce implant failure and strengthen overall fixation. Future studies should build on our findings to determine if osteosynthesis of distal clavicular fractures with targeted implant placement in the conoid tubercle and intertubercle space increases fixation strength and decreases construct failure. Furthermore, our findings provide consideration for novel distal clavicular locking plate designs with modified screw trajectories to reliably capture these areas of greatest bone quality.
Acknowledgments
We thank Michael Thullen BS, for his technical assistance with micro-CT imaging.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Augat P, Schorlemmer S. The role of cortical bone and its microstructure in bone strength. Age Ageing . 2006;35:27-31. [DOI] [PubMed] [Google Scholar]
- 2.Ballmer FT, Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle: a report of five cases. J Bone Joint Surg Br . 1991;73:291-294. [DOI] [PubMed] [Google Scholar]
- 3.Bezer M, Aydin N, Guven O. The treatment of distal clavicle fractures with coracoclavicular ligament disruption: a report of 10 cases. J Orthop Trauma . 2005;19:524-528. [DOI] [PubMed] [Google Scholar]
- 4.Brouwer KM, Wright TC, Ring DC. Failure of superior locking clavicle plat by axial pull-out of the lateral screws: A report of four cases. J Shoulder Elbow Surg. 2009;18:e22-e25. [DOI] [PubMed] [Google Scholar]
- 5.Fleming MA, Dachs R, Maqungo S, du Plessis J, Vrettos BC, Roche SJL. Angular stable fixation of displaced distal-third clavicle fractures with superior precontoured locking plates. J Shoulder Elbow Surg . 2015;24:700-704. [DOI] [PubMed] [Google Scholar]
- 6.Flinkkilä T, Ristiniemi J, Hyvönen P, Hämäläinen M. Surgical treatment of unstable fractures of the distal clavicle: a comparative study of Kirschner wire and clavicular hook plate fixation. Acta Orthop Scand . 2002;73:50-53. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg JA, Bruce WJ, Sonnabend DH, Walsh WR. Type 2 fractures of the distal clavicle: a new surgical technique. J Shoulder Elbow Surg . 1997;6:380-382. [DOI] [PubMed] [Google Scholar]
- 8.Han L, Hu Y, Quan R, Fang W, Jin B, Huang L. Treatment of Neer IIb distal clavicle fractures using anatomical locked plate fixation with coracoclavicular ligament augmentation. J Hand Surg . 2017;42:1036.e1-1036.e6. [DOI] [PubMed] [Google Scholar]
- 9.Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury . 2009;40:236–239.. [DOI] [PubMed] [Google Scholar]
- 10.Hsu K, Tzeng Y, Chang M, Chiang C. Comparing the coracoclavicular loop technique with a hook plate for the treatment of distal clavicle fractures. J Shoulder Elbow Surg . 2018;27:224-230. [DOI] [PubMed] [Google Scholar]
- 11.Jin CZ, Kim HK, Min BH. Surgical treatment for distal clavicle fracture associated with coracoclavicular ligament rupture using a cannulated screw fixation technique. J Trauma . 2006;60:1358-1361. [DOI] [PubMed] [Google Scholar]
- 12.Johnston PS, Sears BW, Lazarus MR, Frieman BG. Fixation of unstable type II clavicle fractures with distal clavicle plate and suture button. J Orthop Trauma . 2014;28:e269-e272. [DOI] [PubMed] [Google Scholar]
- 13.Kalamaras M, Cutbush K, Robinson M. A method for internal fixation of unstable distal clavicle fractures: early observations using a new technique. J Shoulder Elbow Surg. 2008;17:60-62. [DOI] [PubMed] [Google Scholar]
- 14.Kao FC, Chao EK, Chen CH, Yu SW, Chen CY, Yen CY. Treatment of distal clavicle fracture using Kirschner wires and tension-band wires. J Trauma . 2001;51:522-525. [DOI] [PubMed] [Google Scholar]
- 15.Kashii M, Inui H, Yamamoto K. Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res . 2006;447:158-164. [DOI] [PubMed] [Google Scholar]
- 16.Kihlstrom C, Moller M, Lonn K, Wolf O. Clavicle fractures: epidemiology, classification and treatment of 2422 fractures in the Swedish Fracture Register; an observational study. BMC Musculoskelet Disord. 2017;18:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lyons FA, Rockwood CA., Jr Migration of pins used in operations on the shoulder. J Bone Joint Surg Am . 1990;72:1262-1267. [PubMed] [Google Scholar]
- 18.Madsen W, Yaseen Z, LaFrance R, Chen T, Awad H, Maloney M, Voloshin I. Addition of a suture anchor for coracoclavicular fixation to a superior locking plate improves stability of type IIB distal clavicle fractures. Arthroscopy . 2013;29:998-1004. [DOI] [PubMed] [Google Scholar]
- 19.Neer CS., 2nd Fractures of the distal third of the clavicle. Clin Orthop Relat Res . 1968;58:43-50. [PubMed] [Google Scholar]
- 20.Renfree KJ, Riley MK, Wheeler D, Hentz JG, Wright TW. Ligamentous anatomy of the distal clavicle. J Shoulder Elbow Surg . 2003;12:355-359. [DOI] [PubMed] [Google Scholar]
- 21.Rieser GR, Edward K, Gould GC, Markert RJ, Goswami T, Rubino LJ. Distal-third clavicle fracture fixation: a biomechanical evaluation of fixation. J Shoulder Elbow Surg . 2012;22:845-855. [DOI] [PubMed] [Google Scholar]
- 22.Sajid S, Fawdington R, Sinha M. Locking plates for displaced fractures of the lateral end of clavicle: Potential pitfalls. Int J Shoulder Surg. 2012;6:126-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schliemann B, Roßlenbroich SB, Schneider KN, Theisen C, Petersen W, Raschke MJ, Weimann A. Why does minimally invasive coracoclavicular ligament reconstruction using a flip button repair technique fail? An analysis of risk factors and complications. Knee Surg Sports Traumatol Arthrosc. 2015;23:1419-25. [DOI] [PubMed] [Google Scholar]
- 24.Shin S, Ko Y, Lee J, Park M. Use of plate fixation without coracoclavicular ligament augmentation for unstable distal clavicle fractures. J Shoulder Elbow Surg . 2016;25:942-948. [DOI] [PubMed] [Google Scholar]
- 25.Struhl S, Wolfson TS. Closed-loop double Endobutton technique for repair of unstable distal clavicle fractures. Orthop J Sports Med . 2016;4:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thiele OC, Eckhardt C, Linke B, Schneider E, Lill CA. Factors affecting the stability of screws in human cortical osteoporotic bone: A cadaver study. J Bone Joint Surg Br . 2007;89:701-705. [DOI] [PubMed] [Google Scholar]
- 27.Yagnik GP, Porter DA, Jordan CJ. Distal clavicle fracture repair using cortical button fixation with coracoclavicular ligament reconstruction. Arthroscopy Tech . 2018;7:e411-e415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang C, Huang J, Luo Y, Sun H. Comparison of the efficacy of a distal clavicular locking plate versus a clavicular hook plate in the treatment of unstable distal clavicle fractures and a systematic literature review. Int Orthop . 2014;38:1461-1468. [DOI] [PMC free article] [PubMed] [Google Scholar]