Abstract
Background
Psychological characteristics, such as depression, anxiety or negative illness perception are highly prevalent in patients with several types of OA. It is unclear whether there are differences in the clinical and psychological characteristics of patients with thumb carpometacarpal (CMC-1) osteoarthritis (OA) scheduled for nonsurgical treatment and those with surgical treatment.
Questions/purposes
(1) What are the differences in baseline sociodemographic characteristics and clinical characteristics (including pain, hand function, and health-related quality of life) between patients with thumb CMC-1 OA scheduled for surgery and those treated nonoperatively? (2) What are the differences in psychological characteristics between patients scheduled for surgery and those treated nonsurgically, for treatment credibility, expectations, illness perception, pain catastrophizing, and anxiety and depression? (3) What is the relative contribution of baseline sociodemographic, clinical, and psychological characteristics to the probability of being scheduled for surgery?
Methods
This was a cross-sectional study using observational data. Patients with CMC-1 OA completed outcome measures before undergoing either nonsurgical or surgical treatment. Between September 2017 and June 2018, 1273 patients were screened for eligibility. In total, 584 participants were included: 208 in the surgery group and 376 in the nonsurgery group. Baseline sociodemographic, clinical, and psychological characteristics were compared between groups, and a hierarchical logistic regression analysis was used to investigate the relative contribution of psychological characteristics to being scheduled for surgery, over and above clinical and sociodemographic variables. Baseline measures included pain, hand function, satisfaction with the patient’s hand, health-related quality of life, treatment credibility and expectations, illness perception, pain catastrophizing, and anxiety and depression.
Results
Patients in the surgery group had longer symptom duration, more often a second opinion, higher pain, treatment credibility and expectations and worse hand function, satisfaction, HRQoL, illness perception and pain catastrophizing compared with the non-surgery group (effect sizes ranged from 0.20 to 1.20; p values ranged from < 0.001 to 0.044). After adjusting for sociodemographic, clinical, and psychological factors, we found that the following increased the probability of being scheduled for surgery: longer symptom duration (standardized odds ratio [SOR], 1.86; p = 0.004), second-opinion visit (SOR, 3.81; p = 0.027), lower satisfaction with the hand (SOR, 0.65; p = 0.004), higher treatment expectations (SOR, 5.04; p < 0.001), shorter perceived timeline (SOR, 0.70; p = 0.011), worse personal control (SOR, 0.57; p < 0.001) and emotional response (SOR, 1.40; p = 0.040). The hierarchical logistic regression analysis including sociodemographic, clinical, and psychological factors provided the highest area under the curve (sociodemographics alone: 0.663 [95% confidence interval 0.618 to 0.709]; sociodemographics and clinical: 0.750 [95% CI 0.708 to 0.791]; sociodemographics, clinical and psychological: 0.900 [95% CI 0.875 to 0.925]).
Conclusions
Patients scheduled to undergo surgery for CMC-1 OA have a worse psychological profile than those scheduled for nonsurgical treatment. Our findings suggest that psychological characteristics should be considered during shared decision-making, and they might indicate if psychological interventions, training in coping strategies, and patient education are needed. Future studies should prospectively investigate the influence of psychological characteristics on the outcomes of patients with CMC-1 OA.
Level of Evidence
Level III, therapeutic study.
Introduction
Thumb carpometacarpal (CMC-1) osteoarthritis (OA) is common, with a symptomatic prevalence of 7% and 2% among women and men aged at least 50 years, respectively [3, 7, 16]. Patients with CMC-1 OA often have thumb pain and limitations to activities of daily life and present with clinical features such as thenar muscle wasting or a thumb deformity [7, 25]. Usually, initial treatment is nonsurgical (for example, hand therapy), including exercises, orthotics, or both [2, 19, 28, 29, 34, 38, 42, 46]. Increasing evidence shows that nonoperative treatment decreases pain and improves hand function and patient satisfaction [2, 19, 38, 41, 46, 50]. When nonsurgical treatment does not alleviate symptoms, surgery may be considered [43, 47]. Tsehaie et al. [41] reported that after nonsurgical treatment, 15% of the patients eventually underwent surgical treatment after a mean period of 2.2 years, indicating that most patients with CMC-1 OA respond well to nonsurgical treatment. In another study, Tsehaie et al. [40] found that baseline sociodemographic and clinical variables (such as pain intensity or hand function) account for 31% to 42% of the variance in outcome when predicting the results of nonsurgical treatment and subsequent surgery, indicating that not all relevant covariates were covered.
During the past decade, studies have demonstrated that psychological characteristics such as depression, anxiety, negative illness perception, and pain catastrophizing are highly prevalent in patients with several types of OA [1, 8, 9, 11-13, 15, 35, 36, 49]. However, little is known about differences in psychological characteristics and treatment expectations between patients with CMC-1 OA who have nonsurgical treatment and those with surgical treatment. Hypothetically, when a nonsurgical treatment fails (perhaps repeatedly), this suggests that a different psychological profile may be present at the start of surgical treatment. Only one study, by Lozano-Calderon et al. [24], evaluated differences between patients electing to undergo surgical and those choosing to undergo nonsurgical treatment, using a relatively small sample of 72 participants and evaluating DASH scores, pain anxiety, catastrophizing, and depression. However, important domains such as illness perception, treatment credibility and expectations, and health-related quality of life were not studied, and the study might have been underpowered to determine between-group differences or predictors of whether a patient would elect to undergo surgery. More insight into the psychological profiles and treatment expectations of patients with CMC-1 OA treated nonsurgically and those treated surgically is needed. This would provide clinicians and patients with valuable information for shared decision-making; decrease the number of surgeries performed; improve the outcomes of surgery; or indicate if psychological interventions, training in coping strategies, and patient education are needed.
Therefore, we formulated the following research questions: (1) What are the differences in baseline sociodemographic characteristics and clinical characteristics (including pain, hand function, and health-related quality of life) between patients with thumb CMC-1 OA scheduled for surgery and those treated nonoperatively? (2) What are the differences in psychological characteristics between patients scheduled for surgery and those treated nonsurgically, for treatment credibility, expectations, illness perception, pain catastrophizing, and anxiety and depression? (3) What is the relative contribution of baseline sociodemographic, clinical, and psychological characteristics to the probability of being scheduled for surgery?
Patients and Methods
Study Design
This was a cross-sectional study using baseline data collected before nonsurgical or surgical treatment in a large observational cohort, following the STROBE statement [44].
Setting
Data were collected as part of routine outcome measurements using GemsTracker electronic data capture tools (Erasmus MC and Equipe Zorgbedrijven, Rotterdam/Eindhoven, The Netherlands) [14]. GemsTracker is a secure web-based application for distributing questionnaires and documents during clinical research and quality registration [51, 52]. Data were collected at 18 outpatient hand surgery and therapy clinics in the Netherlands between September 2017 and June 2018. The study was approved by the local medical research ethical committee. Following the Dutch treatment guideline [27], all patients with CMC-1 OA diagnosed by a certified hand surgeon were initially referred for hand therapy and nonsurgical treatment. Follow-up with the hand surgeon occurred after approximately 3 months, after which the decision to proceed to further (surgical) treatment could be made, based on persistent symptoms and patient preference. We classified patients who started with the nonsurgical, hand therapy treatment as the nonsurgery group, and patients who proceeded to surgical treatment were classified as the surgery group.
Participants
Participants were eligible for inclusion if they were adults with CMC-1 OA diagnosed by a Federation of European Societies for Surgery of the Hand (FESSH)-certified hand surgeon and if they were scheduled for either nonsurgical or surgical treatment. Nonsurgical treatment included an orthosis combined with exercise therapy, which consisted hand therapy sessions (guided by an physical/occupational hand therapist, nationally certified in most cases) and exercises performed at home by the patient to improve active stability of the CMC-1 [26, 34, 41, 42, 50]. Surgical procedures included ligament reconstruction and tendon interposition as described by Burton and Pellegrini [5] and Weilby [48] (using either the flexor carpi radialis or abductor pollicis longus tendon) [48], simple trapeziectomy, and arthrodesis. Participants were excluded from this study if they had a comorbidity (such as de Quervain’s tenosynovitis) that interfered with the treatment or outcome, prior surgery of the CMC-1 in the same hand, steroid injection in the affected hand or wrist within 6 weeks, surgery that targeted multiple pathologies (for example, an additional carpal tunnel release in the same session), or missing data for any measure being studied. Additionally, 13 patients were excluded because they completed the same measures both before their nonsurgical and their subsequent surgical treatment. After applying the eligibility criteria, 584 participants were included: 208 in the surgery group and 376 in the nonsurgery group (Fig. 1).
Fig. 1.
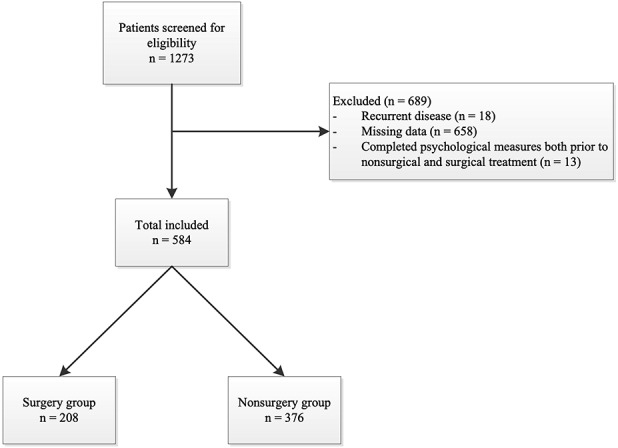
This flowchart illustrates the exclusions criteria for this study.
Variables, Data Sources, and Measurement
Similar to other studies [30-32], we classified variables into three categories: sociodemographic, clinical, and psychological. All data represented baseline values before nonsurgical or surgical treatment. Sociodemographic characteristics included age, sex, symptom duration, treatment side, dominance, type of work, whether the patient was seen for a second opinion, and type of surgery (for the surgery group).
Clinical characteristics included pain, hand function, satisfaction, and health-related quality of life. We used the VAS [17] to measure pain (VAS score ranges from 0 to 100; higher scores indicate more pain) and the patients’ satisfaction with their hand (exact question: “How satisfied are you with your hand at this moment?”; higher scores indicate better satisfaction). To assess hand function, we used the Michigan Hand outcomes Questionnaire (MHQ, range 0 to 100; higher scores indicate better performance, except for the subscale of pain), which is particularly applicable to patients with OA of the hand [33]. Health-related quality of life was measured using the EuroQol-5D-5L (EQ-5D-5L) [18].
Psychological characteristics included treatment credibility, treatment expectations, illness perception, pain catastrophizing, and anxiety and depression. Treatment credibility and expectations were measured using the Credibility/Expectancy Questionnaire (CEQ), consisting of a credibility and expectancy subscale (score range is 3 to 27; higher scores indicate higher credibility or expectations) [10]. Illness perception was measured using the brief Illness Perception Questionnaire ([IPQ]; item scores range from 0 to 10; higher scores indicate worse illness perception) [4]. Pain catastrophizing was measured with the Pain Catastrophizing Scale ([PCS]; score range is 0 to 52; higher scores indicate more catastrophizing) [39]. Furthermore, anxiety and depression were measured with the Patient Health Questionnaire for anxiety and depression ([PHQ-4]; score range: 0 to 6 for the subscales of anxiety and depression; higher scores indicate more anxiety and depression), which is a tool for detecting depressive disorders [20]. Scores of 3 or higher for the subscales indicate a potential anxiety or depression disorder [20].
Study Size
A power analysis using an independent sample t-test (the primary analysis) with a conventional effect size [6] of 0.25 and power of 0.80 (α = 0.05) and an allocation ratio of 0.57 showed that 546 participants were needed, which was well below the sample of 584 participants we were able to include.
Statistical Methods
We compared baseline sociodemographic, clinical, and psychological characteristics between patients with CMC-1 OA scheduled for nonsurgical treatment and those with surgical treatment, using independent sample t-tests and chi-square tests. Additionally, to more specifically investigate the relative contribution of sociodemographic, clinical, and psychological characteristics to the probability of being scheduled for surgery, we used a hierarchical logistic regression analysis with the treatment group as a dependent variable. Using this method, the relative contribution of psychological characteristics can be studied in more detail after adjusting for sociodemographic characteristics (for example, symptom duration) and clinical characteristics (such as VAS pain levels). Variables were added to this hierarchical model in separate steps. To illustrate the fit of the different models, we determined the area under the curve, Nagelkerke’s r2, and receiver operating characteristic curves for these different models. In this analysis, we carefully selected each variable for inclusion in every step based on the construct it measures. This means that not all variables from the primary analysis were used in the hierarchical model; we excluded variables for which there was overlap in the measured construct (for example, the EQ-5D-5L anxiety/depression index and PHQ-4). All available variables are reported in the primary analyses to provide an overview of both groups that was as clear as possible.
In the first step of the hierarchical model, only sociodemographic characteristics including age, sex, symptom duration, treatment side, dominance, type of work, and second-opinion visit were added. In the second step, we added clinical characteristics, including VAS scores for pain at rest and during physical loading; VAS satisfaction; MHQ subscales of hand function, activities of daily life, work, and aesthetics; and the EQ-5D-5L index score. In the third step, we added psychological characteristics, including the CEQ subscales of credibility and expectancy; IPQ items of consequences, timeline, personal control, identity, concern, coherence, and emotional response; the PCS; and the PHQ anxiety and depression subscales. We evaluated multicollinearity using correlation coefficients and the variance inflation factor. A variance inflation factor greater than 10 was considered an indication of multicollinearity [22].
Results
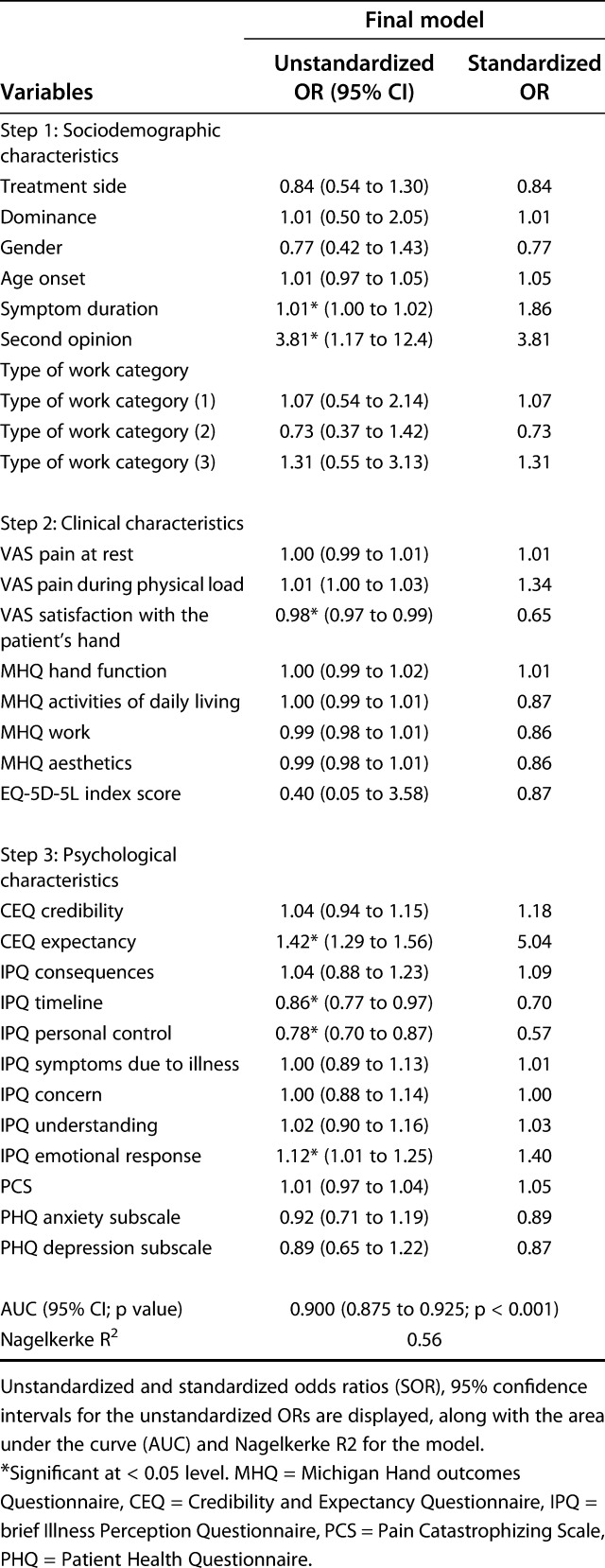
After adjusting for sociodemographic, clinical, and psychological factors, we found that longer symptom duration (standardized odds ratio [SOR], 1.86; p = 0.004), second-opinion visit (SOR, 3.81; p = 0.027), lower satisfaction with the hand (SOR, 0.65; p = 0.004), higher treatment expectations (SOR, 5.04; p < 0.001), shorter perceived timeline (SOR, 0.70; p = 0.011), worse personal control (SOR, 0.57; p < 0.001) and emotional response (SOR, 1.40; p = 0.040) increased the probability of being scheduled for surgery to an area under the curve (AUC) of 0.900 (Table 1).
Table 1.
Final model following hierarchical logistic regression analyses (n = 594) using sociodemographic, clinical and psychological characteristics explaining the relative contribution of being in the surgery group
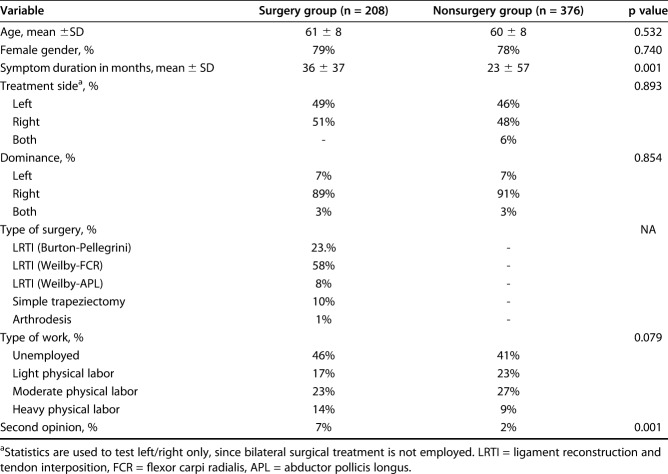
In an examination of sociodemographics alone, we found that patients in the surgery group reported a longer symptom duration (36 months) than did those in the nonsurgery group (23 months; p = 0.001) and visited our center more often for a second opinion (7% versus 2%; p = 0.001). There were no other between-group differences in sociodemographic characteristics (Table 2).
Table 2.
Sociodemographic characteristics for the surgery group (n = 208) and the nonsurgery group (n = 376)
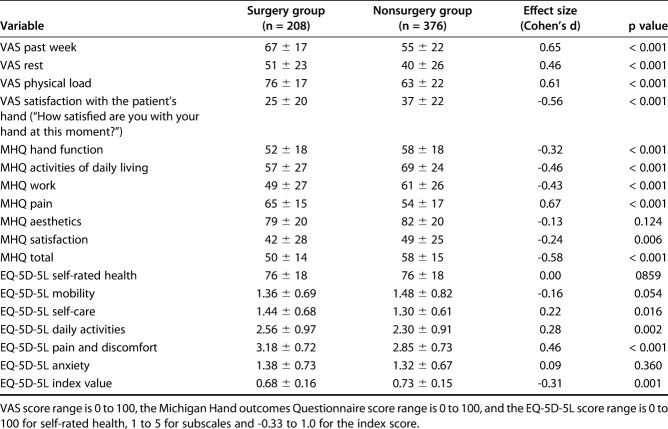
Considering clinical characteristics, patients in the surgical treatment group reported worse symptom severity scores for the VAS and MHQ (except for the subscale of aesthetics) than did those in the nonsurgical treatment group (p < 0.001 to 0.006; absolute effect sizes ranging from 0.24 to 0.67) (Table 3). Additionally, patients in the surgery group reported worse scores for the EQ-5D-5L domains of self-care, daily activities, pain and discomfort indexes, and total index score (p < 0.001 to 0.016; absolute effect sizes ranging from 0.22 to 0.46) (Table 2).
Table 3.
Baseline mean ± SD values for clinical characteristics and symptom severity for the VAS, the Michigan Hand outcomes Questionnaire, and the EQ-5D-5L
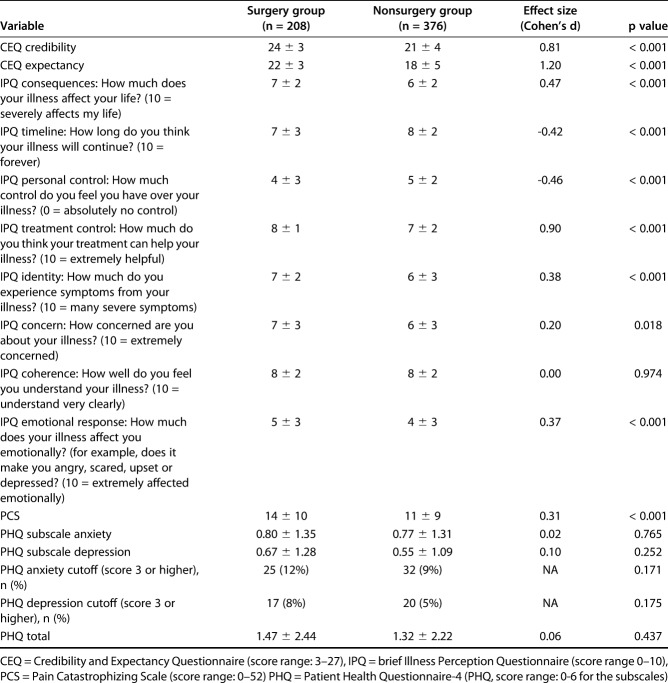
When we compared the groups in terms of psychological characteristics, patients in the surgery group reported higher credibility and expectancy of their treatment than did those in the nonsurgery group (p < 0.001), with effect sizes of 0.81 and 1.20, respectively (Table 4). For the IPQ, patients in the surgery group reported having worse consequences, identity, concern, and emotional response because of their illness and a shorter expected timeline of their illness than did those in the nonsurgery group (p < 0.001 to 0.018; absolute effect sizes ranging from 0.20 to 0.47). Additionally, patients in the surgery group reported less personal control but more treatment control than did those in the nonsurgery group, suggesting a more external locus of control (p < 0.001; absolute effect sizes 0.46 and 0.90, respectively). Furthermore, patients in the surgery group reported more pain catastrophizing on the PCS (p < 0.001; effect size = 0.31) than did those in the nonsurgical treatment group. No differences were found in PHQ scores (Table 3).
Table 4.
Baseline mean ± SD scores on psychological questionnaires for treatment expectations, illness perception, pain catastrophizing and anxiety and depression
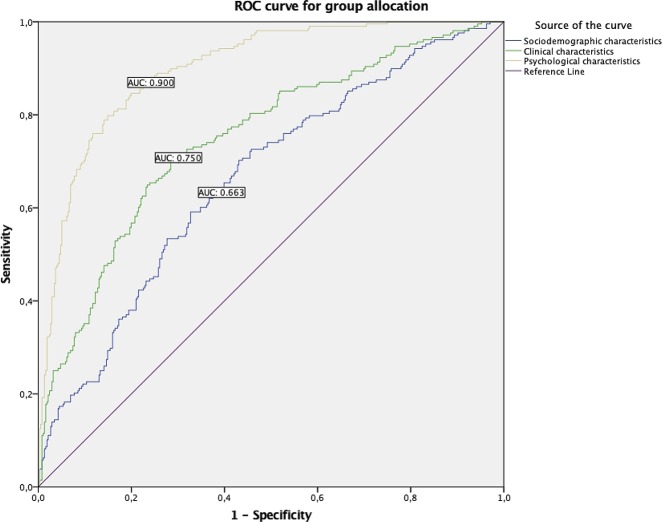
When analyzing the different models resulting from our hierarchical regression, the model including sociodemographic, clinical, and psychological factors provided the highest areas under the curve (sociodemographics alone: 0.663 [95% CI 0.618 to 0.709]; sociodemographics and clinical: 0.750 [95% CI 0.708 to 0.791]; sociodemographics, clinical and psychological: 0.900 [95% CI 0.875 to 0.925], see Table, Supplemental Digital Content 1, http://links.lww.com/CORR/A212). The ROC curve indicates that the probability of being scheduled for surgery is for the largest part explained by the last model, including sociodemographic, clinical, and psychological characteristics (Fig. 2).
Fig. 2.
Receiver operating characteristic curve for the hierarchical models, with AUCs of 0.663, 0.750, and 0.900 for sociodemographic, plus clinical and plus psychological characteristics, respectively, indicating that the probability of being in the surgery group is for the largest part of explained by the model with sociodemographic, clinical and psychological characteristics. ROC = receiver operating characteristic; AUC = area under the curve.
Discussion
Psychological characteristics, such as depression, anxiety or negative illness perception are highly prevalent in patients with OA. Before our study, it was unclear whether there are differences in the clinical and psychological characteristics of patients with CMC-1 OA scheduled for nonsurgical or surgical treatment. More insight in psychological profile of these patients would provide clinicians and patients with valuable information for shared decision-making and indicate if psychological interventions, training in coping strategies, and patient education are needed. We found that patients with CMC-1 OA scheduled for surgery have a worse psychological profile than do those undergoing nonsurgical treatment. Additionally, the probability of being scheduled for surgery is best explained by our model, including sociodemographic, clinical, and psychological characteristics.
Limitations
The results of these between-group comparisons should be interpreted with caution because patients undergoing surgical treatment usually receive nonsurgical treatment first but do not improve. In the present study, we do not know whether between-group differences occurred because of deterioration in clinical and psychological characteristics over time after initiating nonsurgical treatment or if these differences were predetermined and predictors of conversion to surgery. Furthermore, the amount of missing data that lead to our final sample (n = 584 patients) and surgeon’s preferences may have resulted in selection bias. Hence, our sample may be a different representation compared with the target population of patients with CMC-1 OA. Another limitation is that although we reported effect sizes, which allow comparisons across populations and measurement instruments, the between-group differences in this study should be interpreted in light of minimal clinical important difference values established in other disease populations, such as for the VAS and the MHQ [17, 23, 37].
Differences in Baseline Characteristics between Patients Treated Surgically and Those Treated Nonoperatively
We found that patients scheduled for surgical treatment had longer symptom duration, more often sought a second opinion, had higher pain, treatment credibility and expectations and worse hand function, satisfaction, HRQoL, illness perception, and pain catastrophizing compared with those scheduled for nonsurgical treatment. We did not find between-group differences in anxiety or depression.
Although several studies investigated the psychological profiles of patients with OA [1, 8, 9, 11-13, 15, 35, 36, 49], only one other study [24] specifically compared the psychological profiles of patients with CMC-1 OA scheduled for surgical or nonsurgical treatment. However, the study by Lozano-Calderon et al. [24] had a sample that was too small to find any between-group differences, and many different measurement tools were used compared with our study (that is, the DASH versus the MHQ for evaluating hand function), making it difficult to compare findings. Our study confirms prior reports [1, 8, 9, 11-13, 15, 35, 36, 49], which showed that psychological characteristics are of major importance in patients with chronic musculoskeletal diseases such as OA, and these characteristics influence clinical decision-making, although perhaps unconsciously [1, 8, 9, 11, 12, 15, 35, 36, 49]. Because the underlying pathology of OA of the CMC-1 is chronic, our study results might be generalizable to patients scheduled to undergo surgical or nonsurgical treatment of other chronic diseases or body regions; for example, hip or knee OA. Therefore, future research should address other chronic diseases or body regions.
In the present study, we did not find between-group differences in anxiety or depression. However, Becker et al. [1] found differences in depression between patients visiting a clinician for CMC-1 OA and patients with coincidentally diagnosed CMC-1 OA. Becker et al. [1] used the nine-item version of the PHQ, which is a more extensive screening tool than the four-item tool used in the present study. However, a score of 5 or higher on the nine-item version of the PHQ indicates mild depression [21], and in the study by Becker et al. [1], a mean score of 4.5 was found in the group visiting a clinician for CMC-1 OA. This indicates that on average, no depression was present, which is comparable to our results.
Factors Contributing to the Probability of Being Scheduled for Surgery
Our findings suggest that patients with CMC-1 OA scheduled for surgical treatment have a worse psychological profile compared with patients scheduled for nonsurgical treatment. The decision to undergo surgery might be influenced by potentially modifiable psychological characteristics, and addressing these factors may decrease the number of surgeries performed or improve the outcomes of surgery. Psychological interventions, training in coping strategies, and more extensive patient education may be indicated before surgical treatment is performed. However, although the correlation of psychological characteristics with the outcome of nonsurgical or surgical treatment of CMC-1 OA is currently unknown, this correlation is known in patients who undergo surgery for carpal tunnel syndrome or trigger finger [45]. Future longitudinal studies should address the correlation of psychological characteristics with the outcomes of both nonsurgical and surgical treatment of CMC-1 OA.
We found that patients in the nonsurgery group expected to have a longer illness duration and had more personal control, less treatment control (IPQ scores), and lower treatment expectations (CEQ scores) than did those in the surgical group. Patients scheduled for nonsurgical treatment may cope with chronic disease differently than those with surgical treatment, implying that they are more willing to accept aging processes and adapt to daily life than patients who undergo surgery. Furthermore, the participants in the surgery group reported having higher treatment credibility and expectations but worse clinical and other psychological characteristics, suggesting that more research on how to manage treatment credibility and expectations is needed, especially in this population.
In the final model, we found a relatively large OR for whether a second opinion contributed to the probability of surgery. This finding may be explained by the theory that patients seeking a second opinion already had a relatively long clinical course, and they may have postponed surgery for a longer time period. However, this hypothesis cannot be confirmed with the present cross-sectional study design and should be investigated in a longitudinal setting.
Conclusions
In conclusion, we found worse clinical and psychological characteristics in patients scheduled for surgical treatment of CMC-1 OA than in patients at the initiation of nonsurgical treatment. Furthermore, the probability of being scheduled for surgery was mostly explained by the model including sociodemographic, clinical, and psychological characteristics. A more thorough psychological evaluation might be considered before surgery is performed, especially in patients with high expectations, worse illness perception, and pain catastrophizing. Additionally, addressing these factors might decrease the number of surgeries performed, improve the outcomes of surgery or indicate if psychological interventions, training in coping strategies, and patient education might be indicated before converting to surgery. Future studies should investigate the influence of psychological characteristics on the outcomes of patients with CMC-1 OA.
Acknowledgments
We thank all patients who participated and allowed their data to be anonymously used in the present study.
Footnotes
The members of The Hand-Wrist Study Group are R. A. M. Blomme, B. J. R. Sluijter, C. Schouten, D. J. J. C. van der Avoort, E. T. Walbeehm, G. M. van Couwelaar, G. M. Vermeulen, J. P. de Schipper, J. F. M. Temming, J. H. van Uchelen, H. L. de Boer, K. P. de Haas, O. T. Zöphel, R. Feitz, J. S. Souer, S. E. R. Hovius, T. M. Moojen, X. Smit, R. van Huis, P. Y. Pennehouat, K. Schoneveld, Y. E. van Kooij, R. M. Wouters, P. Zagt, F. J. van Ewijk, Frederik Moussault, J. J. Veltkamp, A. F. te Velde, A. Fink, W. A. de Ridder, H. P. Slijper, R. W. Selles, J. T. Porsius, K. R. Spekreijse, C. Zhou, J. Tsehaie, R. Poelstra, M. C. Janssen, M. J. W. van der Oest, S. Evers, P. O. Sun, V. J. M. M. Schrier, Jak Dekker, Matijs de Jong, Jasper van Gestel, Marloes ter Stege, Menno Dekker, Roel Faber, Frank Santegoets, Monique Sieber-Rasch, and Ton Gerritsen.
The institution of one or more of the authors (RW, MO, JP) has received, during the study period, funding from Handtherapie Nederland, Xpert Clinic, Erasmus MC, Geert Geertsen Foundation, Netherlands Organisation for Scientific Research, and Medical Delta. Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Erasmus MC, University Medical Center Rotterdam, The Netherlands.
References
- 1.Becker SJ, Makarawung DJ, Spit SA, King JD, Ring D. Disability in patients with trapeziometacarpal joint arthrosis: incidental versus presenting diagnosis. J Hand Surg Am. 2014;39:2009-2015.e2008. [DOI] [PubMed] [Google Scholar]
- 2.Bertozzi L, Valdes K, Vanti C, Negrini S, Pillastrini P, Villafane JH. Investigation of the effect of conservative interventions in thumb carpometacarpal osteoarthritis: systematic review and meta-analysis. Disabil Rehabil. 2015;37:2025-2043. [DOI] [PubMed] [Google Scholar]
- 3.Bijlsma JWJ, Berenbaum F, Lafeber FPJG. Osteoarthritis: An update with relevance for clinical practice. Lancet. 2011;377:2115-2126. [DOI] [PubMed] [Google Scholar]
- 4.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631-637. [DOI] [PubMed] [Google Scholar]
- 5.Burton RI, Pellegrini VD., Jr. Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am. 1986;11:324-332. [DOI] [PubMed] [Google Scholar]
- 6.Cohen J. Statistical power analysis for the behavioral sciences, second edition. New York, New York: Lawrence Erlbaum Associates, Publishers; 1988:20-42. [Google Scholar]
- 7.Dahaghin S, Bierma-Zeinstra SMA, Ginai AZ, Pols HAP, Hazes JMW, Koes BW. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study). Ann Rheum Dis. 2005;64:682-687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Damman W, Liu R, Kaptein AA, Evers AWM, van Middendorp H, Rosendaal FR, Kloppenburg M. Illness perceptions and their association with 2 year functional status and change in patients with hand osteoarthritis. Rheumatology (Oxford). 2018; Dec 1;57(12):2190-2199. 10.1093/rheumatology/key231. [DOI] [PubMed] [Google Scholar]
- 9.Dave AJ, Selzer F, Losina E, Klara KM, Collins JE, Usiskin I, Band P, Dalury DF, Iorio R, Kindsfater K, Katz JN. Is there an association between whole-body pain with osteoarthritis-related knee pain, pain catastrophizing, and mental health? Clin Orthop Relat Res. 2015;473:3894-3902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31:73-86. [DOI] [PubMed] [Google Scholar]
- 11.Duivenvoorden T, Vissers MM, Verhaar JAN, Busschbach JJV, Gosens T, Bloem RM, Bierma-Zeinstra SMA, Reijman M. Anxiety and depressive symptoms before and after total hip and knee arthroplasty: a prospective multicentre study. Osteoarthritis Cartilage. 2013;21:1834-1840. [DOI] [PubMed] [Google Scholar]
- 12.Foster NE, Thomas E, Hill JC, Hay EM. The relationship between patient and practitioner expectations and preferences and clinical outcomes in a trial of exercise and acupuncture for knee osteoarthritis. Eur J Pain. 2010;14:402-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Frouzakis R, Herren DB, Marks M. Evaluation of expectations and expectation fulfillment in patients treated for trapeziometacarpal osteoarthritis. J Hand Surg Am. 2015;40:483-490. [DOI] [PubMed] [Google Scholar]
- 14.GemsTracker c, Erasmus MC, Zorgbedrijven Equipe, latest release at 2017, version 1.8.2, open source (new BSD licence), https://gemstracker.org.
- 15.Glette M, Landmark T, Jensen MP, Woodhouse A, Butler S, Borchgrevink PC, Stiles TC. Catastrophizing, solicitous responses from significant others, and function in individuals with neuropathic pain, osteoarthritis, or spinal pain in the general population. J Pain. 2018;19:983-995. [DOI] [PubMed] [Google Scholar]
- 16.Haugen IK, Englund M, Aliabadi P, Niu J, Clancy M, Kvien TK, Felson DT. Prevalence, incidence and progression of hand osteoarthritis in the general population: the Framingham Osteoarthritis Study. Ann Rheum Dis. 2011;70:1581-1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S240-252. [DOI] [PubMed] [Google Scholar]
- 18.Janssen MF, Bonsel GJ, Luo N. Is EQ-5D-5L better than EQ-5D-3L? A head-to-head comparison of descriptive systems and value sets from seven countries. Pharmacoeconomics. 2018;36:675-697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kjeken I, Smedslund G, Moe RH, Slatkowsky-Christensen B, Uhlig T, Hagen KB. Systematic review of design and effects of splints and exercise programs in hand osteoarthritis. Arthritis Care Res. 2011;63:834-848. [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB, Lowe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–621. [DOI] [PubMed] [Google Scholar]
- 21.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kutner M, Nachtsheim CJ, Neter J, Li W. Applied linear statistical models.-5th ed. New York, NY: The McGraw-Hill Companies, Inc; 2005:408-410. [Google Scholar]
- 23.London DA, Stepan JG, Calfee RP. Determining the Michigan Hand Outcomes Questionnaire minimal clinically important difference by means of three methods. Plast Reconstr Surg. 2014;133:616-625. [DOI] [PubMed] [Google Scholar]
- 24.Lozano-Calderon SA, Souer JS, Jupiter JB, Ring D. Psychological differences between patients that elect operative or nonoperative treatment for trapeziometacarpal joint arthrosis. Hand (N Y). 2008;3:271-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marshall M, van der Windt D, Nicholls E, Myers H, Dziedzic K. Radiographic thumb osteoarthritis: frequency, patterns and associations with pain and clinical assessment findings in a community-dwelling population. Rheumatology. 2011;50:735-739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Neumann DBT. The carpometacarpal joint of the thumb: stability, deformity, and therapeutic intervention. J Orthop Sports Phys Ther. 2003;33:386-399. [DOI] [PubMed] [Google Scholar]
- 27.NVPC NVvH. Dutch Plastic (NVPC) and Hand (NVvH) Surgery Societies: Guideline for conservative and surgical treatment for primary osteoarthritis of the thumb base joint (Richtlijn Conservatieve en Chirurgische Behandeling van Primaire Artrose van de Duimbasis) . Amsterdam, N-Holland, The Netherlands: NVvH; 2014:6. [Google Scholar]
- 28.O'Brien VH, Giveans MR. Effects of a dynamic stability approach in conservative intervention of the carpometacarpal joint of the thumb: A retrospective study. J Hand Ther. 2013;26:44-52. [DOI] [PubMed] [Google Scholar]
- 29.Osteras N, Kjeken I, Smedslund G, Moe RH, Slatkowsky-Christensen B, Uhlig T, Hagen KB. Exercise for hand osteoarthritis. Cochrane Database Syst Rev. 2017;1:Cd010388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pinto PR, McIntyre T, Araujo-Soares V, Costa P, Ferrero R, Almeida A. A comparison of predictors and intensity of acute postsurgical pain in patients undergoing total hip and knee arthroplasty. J Pain Res. 2017;10:1087-1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pinto PR, McIntyre T, Ferrero R, Almeida A, Araujo-Soares V. Predictors of acute postsurgical pain and anxiety following primary total hip and knee arthroplasty. J Pain. 2013;14:502-515. [DOI] [PubMed] [Google Scholar]
- 32.Pinto PR, Vieira A, Pereira D, Almeida A. Predictors of Acute Postsurgical Pain After Inguinal Hernioplasty. J Pain. 2017;18:947-955. [DOI] [PubMed] [Google Scholar]
- 33.Poole J. Measures of hand function: Arthritis Hand Function Test (AHFT), Australian Canadian Osteoarthritis Hand Index (AUSCAN), Cochin Hand Function Scale, Functional Index for Hand Osteoarthritis (FIHOA), Grip Ability Test (GAT), Jebsen Hand Function Test (JHFT), and Michigan Hand Outcomes Questionnaire (MHQ). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S189-S199. [DOI] [PubMed] [Google Scholar]
- 34.Poole JU, Pellegrini VD., Jr Arthritis of the thumb basal joint complex. J Hand Ther. 2000;13:91-107. [DOI] [PubMed] [Google Scholar]
- 35.Riddle DL, Wade JB, Jiranek WA, Kong X. Preoperative Pain Catastrophizing Predicts Pain Outcome after Knee Arthroplasty. Clin Orthop Relat Res. 2010;468:798-806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sharma A, Kudesia P, Shi Q, Gandhi R. Anxiety and depression in patients with osteoarthritis: impact and management challenges. Open Access Rheumatol. 2016;8:103-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shauver MJ, Chung KC. The minimal clinically important difference of the Michigan hand outcomes questionnaire. J Hand Surg Am. 2009;34:509-514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spaans AJ, van Minnen LP, Kon M, Schuurman AH, Schreuders AR, Vermeulen GM. Conservative treatment of thumb base osteoarthritis: a systematic review. 2015. [DOI] [PubMed] [Google Scholar]
- 39.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychol Assess. 1995;7:524-532. [Google Scholar]
- 40.Tsehaie J, Spekreijse KR, Wouters RM, Feitz R, Hovius SER, Slijper HP, Selles RW. Predicting outcome after hand orthosis and hand therapy for thumb carpometacarpal osteoarthritis: a prospective study. Arch Phys Med Rehabil. 2019;100:844-850. [DOI] [PubMed] [Google Scholar]
- 41.Tsehaie J, Spekreijse KR, Wouters RM, Slijper HP, Feitz R, Hovius SER, Selles RW. Outcome of a hand orthosis and hand therapy for carpometacarpal osteoarthritis in daily practice: a prospective cohort study. J Hand Surg Am. 2018;43:1000-1009.e1001. [DOI] [PubMed] [Google Scholar]
- 42.Valdes K, Von Der Heyde R. An exercise program for carpometacarpal osteoarthritis based on biomechanical principles. J Hand Ther. 2012;25:251-262. [DOI] [PubMed] [Google Scholar]
- 43.Vermeulen G, Slijper H, Feitz R, Hovius SER, Moojen T, Selles R. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am. 2011;36:157-169. [DOI] [PubMed] [Google Scholar]
- 44.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453-1457. [DOI] [PubMed] [Google Scholar]
- 45.Vranceanu AM, Jupiter JB, Mudgal CS, Ring D. Predictors of pain intensity and disability after minor hand surgery. J Hand Surg Am. 2010;35:956-960. [DOI] [PubMed] [Google Scholar]
- 46.Wajon A, Ada L. No difference between two splint and exercise regimens for people with osteoarthritis of the thumb: a randomised controlled trial. Aust J Physiother. 2005;51:245-249. [DOI] [PubMed] [Google Scholar]
- 47.Wajon A, Vinycomb T, Carr E, Edmunds I, Ada L. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2015;2:Cd004631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Weilby A. Tendon interposition arthroplasty of the first carpo-metacarpal joint. J Hand Surg Br. 1988;13:421-425. [DOI] [PubMed] [Google Scholar]
- 49.Wood TJ, Thornley P, Petruccelli D, Kabali C, Winemaker M, de Beer J. Preoperative predictors of pain catastrophizing, anxiety, and depression in patients undergoing total joint arthroplasty. J Arthroplasty. 2016;31:2750-2756. [DOI] [PubMed] [Google Scholar]
- 50.Wouters RM, Tsehaie J, Slijper HP, Hovius SER, Feitz R, Selles RW. Exercise therapy in addition to an orthosis reduces pain more than an orthosis alone in patients with thumb base osteoarthritis: a propensity score matching study. Arch Phys Med Rehabil. 2018. [DOI] [PubMed] [Google Scholar]
- 51.Zhou C, Hovius SE, Slijper HP, Feitz R, Van Nieuwenhoven CA, Pieters AJ, Selles RW. Collagenase Clostridium histolyticum versus limited fasciectomy for Dupuytren's contracture: Outcomes from a multicenter propensity score matched study. Plast Reconstr Surg. 2015;136:87-97. [DOI] [PubMed] [Google Scholar]
- 52.Zhou C, Selles RW, Slijper HP, Feitz R, van Kooij Y, Moojen TM, Hovius SE. Comparative effectiveness of percutaneous needle aponeurotomy and limited fasciectomy for Dupuytren's contracture: a multicenter observational study. Plast Reconstr Surg. 2016;138:837-846. [DOI] [PubMed] [Google Scholar]