Abstract
Objective
To describe the experiences of participants in Canadian family medicine maternity care enhanced skills programs: their current practice situation with respect to maternity care; the reasons they pursued enhanced maternity care training; and their perceptions of competencies attained during the program.
Design
Cross-sectional questionnaire.
Setting
Canada.
Participants
Graduates of family medicine enhanced skills programs in maternity care in Canada between 2004 and 2014.
Main outcome measures
Participants’ current engagement in intrapartum care; reasons for participating in the enhanced skills programs; interest in obstetrics at different points in training; and development of maternity care competencies during both core residency and the enhanced skills program.
Results
Eighty-seven graduates (response rate of 44%) participated. At an average of 5 years in practice, 77% of enhanced skills graduates were providing intrapartum care. Sixty-nine percent of respondents took the enhanced skills program because they did not feel ready to practise obstetrics without supervision. More than half (55%) of respondents had intended to include obstetrics in their future practices when they were in medical school. By the end of residency, 99% intended to practise obstetrics; however, this percentage decreased to 87% by the end of fellowship. There was a statistically significant increase in graduates’ perceptions of various maternity care competencies (eg, vacuum-assisted birth, perineal repair) following enhanced skills training. Eighty-two percent of respondents indicated that the ability to access enhanced skills training supported their decision to provide obstetrics care.
Conclusion
This is the first evaluation of graduates of enhanced skills programs in maternity care in Canada. Enhanced skills programs appear to support the education of family medicine maternity care providers; however, these programs might be compensating for residents’ lack of confidence in providing maternity care independently rather than providing truly enhanced skills. This study also confirms that some medical students and family medicine residents change their minds in the direction of wanting to provide full-scope maternity care during the course of their education.
Résumé
Objectif
Décrire les expériences des participants à des programmes de compétences avancées en soins de maternité en médecine familiale : la situation dans leur pratique actuelle en matière de soins de maternité; les raisons ayant motivé la poursuite d’une formation avancée en soins de maternité; et leurs perceptions quant aux compétences acquises durant ce programme.
Type d’étude
Questionnaire transversal.
Contexte
Canada.
Participants
Les diplômés de programmes de formation avancée en soins de maternité en médecine familiale entre 2004 et 2014.
Principaux paramètres à l’étude
La participation actuelle des répondants à des soins intrapartum; les raisons motivant leur participation aux programmes de compétences avancées; leur intérêt face à l’obstétrique à différentes étapes durant leur formation; le perfectionnement de compétences en soins de maternité, tant durant leur résidence de base que dans le programme de compétences avancées.
Résultats
Au total, 87 diplômés ont répondu (taux de réponse de 44 %) au questionnaire. Après 5 années de pratique, en moyenne, 77 % des diplômés en compétences avancées offraient des soins intrapartum. Parmi les répondants, 69 % avaient suivi le programme en compétences avancées parce qu’ils ne se sentaient pas prêts à pratiquer l’obstétrique sans supervision. Plus de la moitié des répondants (55 %) avaient l’intention d’inclure l’obstétrique dans leur future pratique lorsqu’ils étaient étudiants en médecine. À la fin de leur résidence, 99 % avaient l’intention de pratiquer l’obstétrique; par ailleurs, ce pourcentage avait baissé à 87 % à la fin de la formation avancée. Il y avait, selon la perception des diplômés, une augmentation statistiquement significative des compétences dans divers soins de maternité (p. ex. accouchement assisté par ventouse, réparation périnéale) après avoir suivi la formation en compétences avancées. Pour 82 % des répondants, la capacité d’avoir accès à une formation en compétences avancées avait soutenu leur décision de fournir des soins en obstétrique.
Conclusion
Il s’agit de la première évaluation, par les diplômés, des programmes de compétences avancées en soins de maternité au Canada. Les programmes de compétences avancées semblent améliorer la formation des prestataires de soins de maternité en médecine familiale; cependant, ces programmes pourraient compenser le manque de confiance que ressentent les résidents face à la pratique indépendante des soins de maternité, plutôt que développer de véritables compétences avancées. Cette étude confirme aussi que certains étudiants en médecine et résidents en médecine familiale changent d’idée, durant leur formation, quant à la volonté d’offrir la gamme complète des soins de maternité.
The College of Family Physicians of Canada mandates that residents graduate from their 2-year programs with competence in full-scope (prenatal, intrapartum, and postpartum) maternity care.1 However, there is a sense among family medicine educators that programs are struggling to meet this requirement and that residents are not feeling competent or confident when they graduate.2 In fact, although the primary reason for the decline in family physician involvement in intrapartum care is related to lifestyle, another common reason cited is residents’ lack of confidence in their skills.3 This educational deficit has implications for Canadian communities.
There has been a growth in the opportunities for enhanced skills training (sometimes called fellowships) in many areas of family medicine, including maternity care. While the purpose of these training programs is to provide residents with additional competencies they will require in their future practices,1 it appears that many residents might be participating in enhanced skills programs in maternity care to reinforce the skills that they were expected to achieve during residency rather than to acquire new, enhanced skills. An unpublished review of the stated program objectives of maternity care fellowships across Canada describes objectives ranging from reinforcing fellows’ comfort with low-risk care to the development of cesarean delivery competence.4 However, most fellowships focus on low-risk maternity care; therefore, residents might be turning to these training programs to acquire the confidence and competence that they should have attained during their core residency programs.
There are few published studies on the outcomes of enhanced skills training in family medicine maternity care in Canada.5 Most of the literature6–8 is from the United States making generalizability difficult. Critical differences in length of training and expected competencies at the end of training create challenges in extrapolating US data to the Canadian context.6–8 In fact, at 2 years, Canada has the shortest family medicine residency training program of all Western countries by 1 to 3 years9 and is thus in a unique position in terms of paths to maternity care practice. Green et al5 compared the practice patterns of graduates (from 1994 to 2004) of 2-year standard residency and 3-year enhanced skills family medicine programs in Ontario. Although graduates of enhanced skills programs (including but not limited to maternity care) were statistically significantly more likely to practise intrapartum care than the cohort that completed the standard 2-year residency, two-thirds of participants who were practising obstetrics actually had no additional formal training in this area. The authors concluded that
this finding highlights the importance of maintaining adequate educational experiences in intrapartum obstetrics in the core FM [family medicine] training program in addition to providing additional experience through PGY3 [postgraduate year 3] opportunities.5
The purpose of this study was to understand the experiences of participants in family medicine maternity care enhanced skills programs across Canada: their current practice situation with respect to maternity care; the reasons they pursued enhanced training in maternity care; and their perceptions of competencies attained during the program. It is hoped that their experiences can help shape fellowships in maternity care and inform residency program directors how to better prepare all graduates of standard family medicine residency training programs to provide this critical component of comprehensive care.
METHODS
A questionnaire was developed based on a literature review, existing questionnaires relating to maternity care training, and the research team’s questions. The questionnaire was pilot-tested for content and context validity with past fellowship graduates who were not part of the sample owing to their graduation year or working relationships with the authors, and it was formatted for electronic distribution in FluidSurveys, as well as for paper distribution.
Program directors of all family medicine maternity care and women’s health fellowships across Canada were contacted for interviews (a separate study) and to survey their graduates from the previous 10 years (2004–2014). We excluded those programs in which the program directors did not participate in interviews owing to challenges accessing their graduates. There were no other exclusion criteria. The interviews are not reported in this paper.4
Questionnaires were sent out between February and May 2015 primarily through program directors to graduates of their programs; however, some programs permitted direct contact with their graduates and provided e-mail addresses. Most of the graduates received the questionnaire through a link that was e-mailed to them, but graduates of 1 program received paper copies as e-mail addresses were unavailable. Using a modified Dillman method,10 reminders were sent out 2 and 4 weeks after the initial invitation was sent.
Data were analyzed using SPSS, version 23. The data were examined descriptively with frequency distributions and means analysis; CIs were calculated for proportions related to intentions to include obstetrics in future practice; and the McNemar test was used to compare perceived competencies obtained during residency and by the end of enhanced training. Answers to open-ended questions were reviewed and categorized into themes by team members.
Approval was obtained from the Research Ethics Boards at Mount Sinai Hospital and the University of Toronto (U of T).
RESULTS
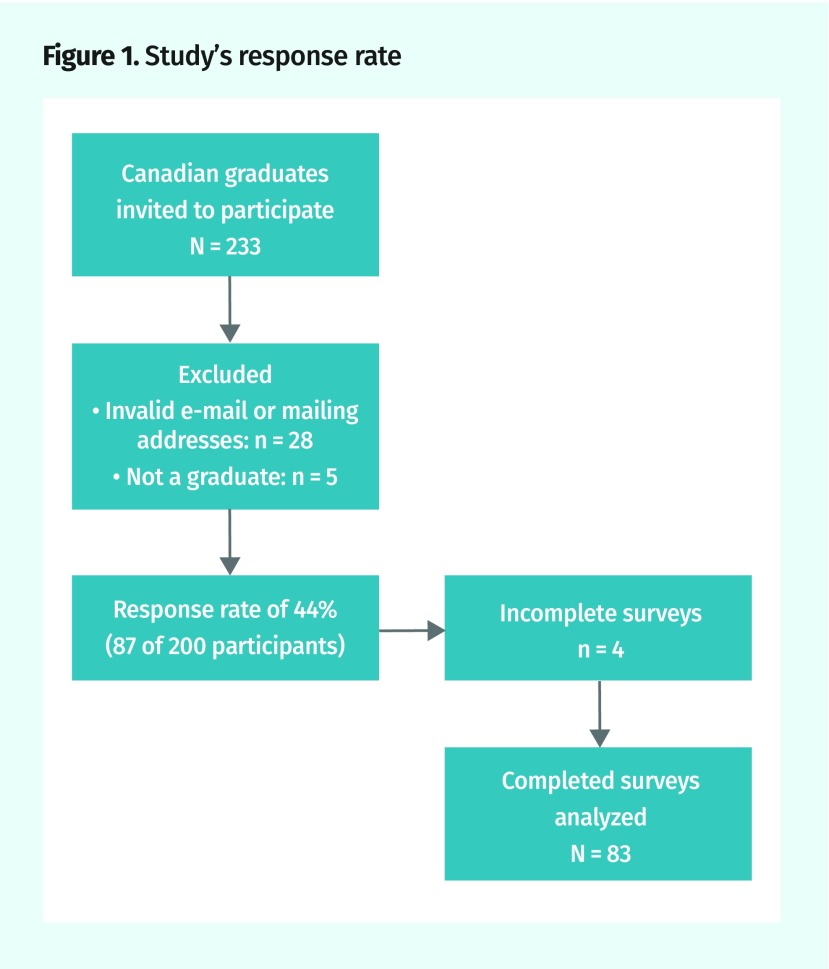
There are 12 fellowship programs in women’s health or obstetrics across Canada. Nine program directors agreed to interviews and their programs were approached about distributing questionnaires to their graduates. One program had only 1 graduate who therefore was not surveyed, and 1 program did not supply any graduate information. Thus, 233 graduates of 7 fellowship programs were included in the survey population; 87 graduates participated for a response rate of 44%, with 83 usable questionnaires (Figure 1).
Figure 1.
Study’s response rate
Graduates were predominantly female and worked in urban group practices (Table 1). Most graduates had academic appointments (69%) and learners in their practices (77%).
Table 1.
Participant demographic characteristics
| CHARACTERISTIC | VALUE* |
|---|---|
| Mean (SD; range) age, y | 34 (5.2; 27–57) |
| Mean (SD; range) no. of years in practice | 5 (4.5; < 1–28) |
| Mean (SD; range) no. of births attended per year | 44 (29.8; 5–188) |
| Female sex, n/N (%) | 71/78 (91) |
| Practice location, n/N (%) | |
| • Urban | 55/80 (69) |
| • Suburban | 13/80 (16) |
| • Rural | 10/80 (12) |
| • Other | 2/80 (2) |
| Practice type, n/N (%) | |
| • Solo | 3/77 (4) |
| • Group | 35/77 (45) |
| • Teaching practice | 30/77 (39) |
| • Other | 9/77 (12) |
| Practice hours, n/N (%) | |
| • Full-time | 54/78 (69) |
| • Part-time | 23/78 (29) |
| • Other | 1/78 (1) |
| Academic appointment, n/N (%) | 53/77 (69) |
| Learners in practice, n/N (%) | 59/77 (77) |
| Currently include intrapartum care, n/N (%) | 60/78 (77) |
| Completed ALSO or ALARM course, n/N (%) | 51/59 (86) |
ALARM—Advances in Labour and Risk Management, ALSO—Advanced Life Support in Obstetrics.
Denominator varies because not all respondents answered all questions and percentages might not add to 100 owing to rounding.
Responses to study questions
Respondents’ surveys revealed the following about various topics.
Obstetrics practice.
A large proportion (77%) of respondents was providing intrapartum care at the time of the survey, while 6 respondents provided intrapartum care initially but stopped. Twelve respondents never provided intrapartum care. For those practising intrapartum care, the median number of births was 40 per year (range 5 to 188) (Table 1).
Why enhanced skills training?
More than two-thirds (69%) of respondents stated that they took the fellowship because they wanted more experience; 69% did not feel ready to practise obstetrics without supervision; 6% wanted to delay going into practice; and 6% needed the fellowship for hospital privileges. Another 8% described reasons such as a desire to enter academic practice and consolidate training.
Obstetrics interest before and by the end of fellowship.
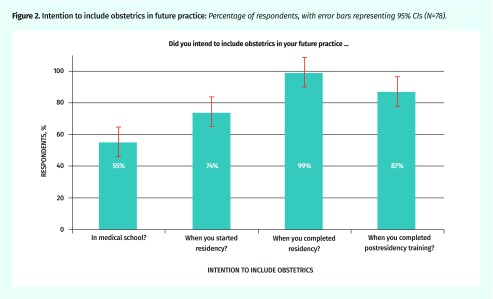
More than half (55%) of respondents had intended to include obstetrics in their future practices when they were in medical school, and 74% had felt that way at the start of family medicine residency. By the end of residency, 99% of this group intended to practise obstetrics; however, this percentage decreased to 87% by the end of fellowship (Figure 2). Fifty-three percent of graduates had only become aware of the possibility of extra training in maternity care during family medicine residency.
Figure 2.
Intention to include obstetrics in future practice: Percentage of respondents, with error bars representing 95% CIs (N=78).
Educational program description.
All enhanced programs included obstetrics and a variety of additional experiences. Most (74%) respondents had 3 months of obstetrics experience, with a range of 1 to 12 months. For 39% of graduates, teaching was included as part of the program. The median number of births attended during fellowship was 100 (mode 100; range 10 to 400) compared with a median of 50 births (mode 50; range 0 to 256) in residency and 20 (mode 20; range 0 to 60) in medical school.
Graduates’ perceptions of maternity care competencies.
Table 2 shows at what point in training these graduates obtained various competencies in maternity care. Ninety-three percent stated that they had achieved competency in spontaneous vaginal delivery during residency. Although 72% of respondents believed that they had achieved competency in second-degree tear or episiotomy repair during residency, this increased to 92% (P < .001) after fellowship. Similarly, competence in management of vacuum-assisted birth increased from 25% after residency to 83% (P < .001) after fellowship. Competence in correcting breastfeeding latch was achieved by only 63% and competency in frenotomy by 40% by the end of fellowship.
Table 2.
Perceived competencies obtained during residency and fellowship among graduates: N = 83.
| COMPETENCY | RESIDENCY, N (%) | FELLOWSHIP (END OF ENHANCED TRAINING), N (%) | P VALUE |
|---|---|---|---|
| Spontaneous vaginal delivery | 77 (93) | 78 (94) | > .99 |
| Vacuum-assisted birth | 21 (25) | 69 (83) | < .001 |
| Forceps-assisted birth | 0 (0) | 4 (5) | NA |
| Cesarean section | 9 (11) | 16 (19) | .016 |
| Management of twins | 4 (5) | 13 (16) | .004 |
| Management of breech | 9 (11) | 20 (24) | .001 |
| Manual removal of placenta | 15 (18) | 50 (60) | < .001 |
| Second-degree tear or episiotomy repair | 60 (72) | 76 (92) | < .001 |
| Third-degree tear repair | 5 (6) | 31 (37) | <.001 |
| Correcting breastfeeding latch | 36 (43) | 52 (63) | < .001 |
| Frenotomy | 10 (12) | 33 (40) | < .001 |
| Neonatal resuscitation | 56 (67) | 66 (80) | .002 |
| Other | 2 (2) | 13 (16) | .001 |
NA—not applicable.
Effect of the program.
Eighty-two percent of participants indicated that the ability to access extra training influenced their decision to practise obstetrics. They cited that the fellowship made them more confident and more comfortable with intrapartum care. When asked if the fellowship was useful to their current practice, 75% rated it a 6 or 7 (on a 7-point scale where 7 was “essential”; mean rating 5.9); 93% said that they would choose to complete the extra training again.
DISCUSSION
This study is the first national evaluation specific to the outcomes of enhanced skills programs in maternity care across Canada. The Canadian programs’ focus on low-risk obstetrics differentiates them from US enhanced skills programs that are more closely aligned with generalist obstetrics and gynecology residencies in Canada.6,7,11–13
The graduates of enhanced skills fellowships were far more likely than the average Canadian family physician to practise intrapartum maternity care. This is hardly surprising, given that enhanced skills graduates committed to extra training in this area. At an average of 5 years in practice, 77% of our respondents are still delivering babies, which is considerably higher than the 12% of Canadian family physicians who have a special interest or focused practice in maternity care.14 Thus, fellowship directors can be reassured that most of their graduates are continuing to practise according to their intentions upon admission to fellowship. The programs might be accomplishing one of their goals: to keep young family physicians active in a practice that includes maternity care. However, most of the respondents in this study have settled into urban practices, raising the question of the ability of maternity care enhanced skills programs to address the need for these skills in rural and remote areas.
Family medicine program directors might be pleased that 93% of our respondents believed that they had achieved competence in spontaneous vaginal delivery during residency, as this is a competence expected for all by the end of the 2-year program. However, most respondents indicated that they did not feel confident enough to practise independently without the enhanced skills program. In fact, more than two-thirds of the participants indicated that they took the enhanced skills training because they did not believe that they were competent to practise obstetrics without supervision after residency. During this training, they showed substantial gains in competence in areas such as vacuum-assisted birth, manual removal of the placenta, perineal repair, and management of breastfeeding issues—skills that most maternity care practitioners would consider essential. It appears that the acquisition of competence in these areas through the additional clinical exposure allows the residents to feel confident to practise independently. This confirms the perception of family medicine maternity care teachers across Canada that fellowship programs are seen by residents as almost essential to the ability to practise low-risk obstetrics rather than opportunities to develop advanced skills. It is congruent with the phenomenon that the number of Canadian family medicine residents undertaking any enhanced skills training doubled from 1995 to 2013.15
Residency programs need to reflect on their ability to meet the College of Family Physicians of Canada’s mandate to graduate residents with competence in full-scope maternity care. Family physicians can and do provide obstetrics care without enhanced skills training5; many current practitioners graduated before the availability of enhanced skills programs. However, it must be acknowledged that the short Canadian family medicine residency program and the wide variations in clinical experience might affect residents’ competence in maternity care. Although there is no “magic number” of births required for competence and confidence, our data would suggest that it resides somewhere between 50 and 100. Our participants finished residency with competence in normal birth, but they needed the additional experience to feel confident.
Some family medicine educators believe that it is unrealistic to aim for competence in intrapartum maternity care for all family medicine residents and that it is preferable to save precious teaching resources for those who enter residency knowing that they want to practise maternity care.2 It is believed that although many residents will change their intentions away from obstetrics, none will change in the direction of practising obstetrics. Even given the inherent bias of surveying maternity care fellowship graduates, it is evident from our data that there can be an increase in interest in intrapartum care during residency. We found an absolute increase of 25% of participants intending to include this aspect of practice between the beginning and end of residency. This argues against educational streaming and the importance of maintaining adequate educational experiences in intrapartum care for core residency programs.
Most of our respondents thought that their fellowship training was essential to their confidence to practise obstetrics. However, when asked in our survey, 53% had first become aware of the possibility of such training during residency. One could hypothesize that increasing awareness of enhanced skills training during medical school might have a positive effect on future career decisions. Family medicine maternity care enhanced skills programs should consider reaching out to undergraduate medical students.
We were struck by how many of these graduates were participating in teaching (42%) despite the fact that only 39% indicated that teaching had been included in their programs. Enhanced skill training in maternity care could be linked to increased opportunities in academic family medicine. Given the difficulty that program chairs express in developing and maintaining a strong family medicine maternity care educational program, there might be preferential hiring of young faculty who have this skill. Programs might want to further emphasize pedagogic skills to prepare enhanced skills trainees, including consideration of ALARM (Advances in Labour and Risk Management) and NRP (Neonatal Resuscitation Program) instructor training as well.
Limitations
It was difficult to determine the true numbers of graduates of enhanced skills maternity care programs, as data were not uniformly collected by the programs. Consequently, we are missing data from graduates who could not be identified in addition to the 56% who did not respond to the questionnaire. The results might also be biased by the possibility that respondents who were still keen on family medicine maternity care would preferentially respond, thus falsely inflating the number of graduates still actively involved in intrapartum care.
The U of T fellowships is the largest program and thus was overrepresented in the responses. We analyzed the data comparing U of T graduates with those of other schools in terms of their experiences and current practices and found a few significant differences: U of T program graduates were less likely to have breastfeeding (25% vs 69%; P < .001) or pediatrics (27% vs 67%; P < .001) in their fellowship training, and reported attending more births (85 vs 53; P < .001) during their fellowship, than those of other schools.
Conclusion
Graduates of enhanced skills programs in maternity care felt competent in attending normal vaginal birth, but did not feel confident to provide independent maternity care at the end of their core residency training. They achieved many other competencies considered critical in obstetrics during their fellowships and most were practising intrapartum care at the time of this survey. Our results confirm the perception that these Canadian fellowships are seen as opportunities to develop competence in core components of low-risk obstetrics rather than truly enhanced skills. Do our residents truly lack the skills required for independent practice or is this a question of lack of clinical courage? Our data cannot answer that question. Would a 3-year residency program enable more clinical exposure, competence, and confidence and thus allow fellowship programs to focus on the attainment of truly enhanced skills? Many leaders support the expansion of the Canadian residency program to be more aligned with our international colleagues.9
Most respondents were practising in urban settings and were involved in teaching, which leads to the following question: If graduating from these programs is often associated with an academic position, how do programs better prepare their learners for teaching and other aspects of academic practice? And, finally, if respondents are not practising in the rural and remote communities where family medicine is often the backbone of the maternity care, how can residency and fellowship programs address obstetrics needs of these communities?
Acknowledgments
Sources of funding include the Ada Slaight and Slaight Family Directorship in Maternity Care at Sinai Health System (personal funding for Dr Biringer and infrastructure costs).
Editor’s key points
▸ There has been a growth in the opportunities for enhanced skills training (sometimes called fellowships) in many areas of family medicine, including maternity care. As most Canadian maternity care fellowships focus on low-risk maternity care, residents might be turning to these training programs to acquire the confidence and competence that they should have attained during their core residency programs.
▸ In this study, two-thirds of respondents indicated that they took the enhanced skills training because they did not believe that they were competent to practise obstetrics without supervision after residency.
▸ During enhanced skills training, graduates showed statistically significant gains in competence in areas such as vacuum-assisted birth, manual removal of the placenta, perineal repair, and management of breastfeeding issues. It appears that the acquisition of competence in these areas through the additional clinical exposure helped residents feel confident to practise independently. This confirms the perception that fellowship programs are seen by residents as almost essential to the ability to practise low-risk obstetrics rather than as opportunities to develop advanced skills.
Points de repère du rédacteur
▸ Les possibilités de suivre une formation en compétences avancées (parfois appelée fellowship ou résidence prolongée) dans de nombreux domaines de la médecine familiale, y compris les soins de maternité, se sont accrues. Puisque la formation avancée en soins de maternité au Canada met l’accent sur l’obstétrique à faible risque, les résidents pourraient se tourner vers ces programmes de formation afin d’acquérir la confiance et les compétences qu’ils auraient dû acquérir durant leur programme de résidence de base.
▸ Dans la présente étude, les 2/3 des répondants ont indiqué qu’ils avaient suivi la formation en compétences avancées parce qu’ils ne croyaient pas avoir acquis les compétences nécessaires pour pratiquer l’obstétrique sans supervision après leur résidence.
▸ Durant la formation en compétences avancées, les diplômés ont accru leurs compétences de manière statistiquement significative dans des domaines comme l’accouchement assisté par ventouse, l’extraction manuelle du placenta, la réparation du périnée et la gestion des questions relatives à l’allaitement. Il semble que l’acquisition de compétences dans ces domaines par l’entremise d’une exposition clinique additionnelle ait aidé les résidents à se sentir en confiance pour pratiquer de façon indépendante. Cela confirme la perception selon laquelle les résidents considèrent les programmes de compétences avancées comme étant presque essentiels à la capacité de pratiquer l’obstétrique à faible risque plutôt que comme des possibilités de développer des compétences avancées.
Footnotes
Contributors
All authors participated to the conception and design of the study. Drs Biringer and Graves and Ms Permaul contributed to the data collection, data analysis, and interpretation. Drs Biringer and Graves drafted the initial paper. All authors contributed to critical revisions and final approval of the version to be published.
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.College of Family Physicians of Canada . Specific standards for family medicine residency programs accredited by the College of Family Physicians of Canada. The red book. Mississauga, ON: College of Family Physicians of Canada; 2016. Available from: www.cfpc.ca/uploadedFiles/RedBookEnglish.pdf. Accessed 2019 Oct 31. [Google Scholar]
- 2.Biringer A, Almond R, Dupuis K, Graves L, Rainsberry P, Wilson L, et al. Report of the Working Group on Family Medicine Maternity Care Training. Mississauga, ON: College of Family Physicians of Canada; 2012. Available from: www.cfpc.ca/uploadedFiles/Directories/Committees_List/Working_Group_on_Maternity_Care_Training_Final_17May12.pdf. Accessed 2019 Oct 31. [Google Scholar]
- 3.Godwin M, Hodgetts G, Seguin R, MacDonald S. The Ontario Family Medicine Residents Cohort Study: factors affecting residents’ decisions to practice obstetrics. CMAJ. 2002;166(2):179–84. [PMC free article] [PubMed] [Google Scholar]
- 4.Boro J, Abells D, Graves L, Permaul JA, Sinha S, Biringer A. A description of family medicine maternity care fellowships across Canada; Poster presented at: Family Medicine Forum, Annual Conference of the College of Family Physicians of Canada; 2016 Nov 9–12; Vancouver, BC. [Google Scholar]
- 5.Green M, Birtwhistle R, MacDonald K, Kane J, Schmelzle J. Practice patterns of graduates of 2- and 3-year family medicine programs. In Ontario, 1996 to 2004. Can Fam Physician. 2009;55:906-7.e1–12. Available from: www.cfp.ca/content/cfp/55/9/906.full.pdf. Accessed 2019 Oct 31. [PMC free article] [PubMed] [Google Scholar]
- 6.Eidson-Ton WS, Nuovo J, Solis B, Ewing K, Diaz H, Smith LH. An enhanced obstetrics track for a family practice residency program: results from the first 6 years. J Am Board Fam Pract. 2005;18(3):223–8. doi: 10.3122/jabfm.18.3.223. [DOI] [PubMed] [Google Scholar]
- 7.Rodney WM, Martinez C, Collins M, Laurence G, Pean C, Stallings J. OB fellowship outcomes 1992–2010: where do they go, who stops delivering, and why? Fam Med. 2010;42(10):712–6. [PubMed] [Google Scholar]
- 8.Chang Pecci C, Leeman L, Wilkinson J. Family medicine obstetrics fellowship graduates: training and post-fellowship experience. Fam Med. 2008;40(5):326–32. [PubMed] [Google Scholar]
- 9.Buchman S. It’s about time: 3-year FM residency training. Can Fam Physician. 2012;58:1045. (Eng), 1046 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 10.Dillman DA. Mail and telephone surveys: the total design method. New York, NY: John Wiley & Sons; 1978. [Google Scholar]
- 11.Heider A, Neely B, Bell L. Cesarean delivery results in a family medicine residency using a specific training model. Fam Med. 2006;38(2):103–9. [PubMed] [Google Scholar]
- 12.Nuovo J, Smith L. Enhanced obstetrics training for family practice residents: a unique collaborative program. J Am Board Fam Pract. 1999;12(5):409–12. doi: 10.3122/jabfm.12.5.409. [DOI] [PubMed] [Google Scholar]
- 13.Acosta DA. Impact of rural training on physician work force: the role of postresidency education. J Rural Health. 2000;16(3):254–61. doi: 10.1111/j.1748-0361.2000.tb00469.x. [DOI] [PubMed] [Google Scholar]
- 14.College of Family Physicians of Canada, Canadian Medical Association, Royal College of Physicians and Surgeons of Canada . National Physician Survey 2013. Mississauga, ON: College of Family Physicians of Canada; 2013. Available from: www.nationalphysiciansurvey.ca. Accessed 2019 Oct 31. [Google Scholar]
- 15.Slade S, Ross S, Lawrence K, Archibald D, Mackay MP, Oandasan IF. Extended family medicine training. Measuring training flows at a time of substantial pedagogic change. Can Fam Physician. 2016;62:e749–57. Available from: www.cfp.ca/content/cfp/62/12/e749.full.pdf. Accessed 2019 Oct 31. [PMC free article] [PubMed] [Google Scholar]