Myocarditis in children and adolescents is rare, with an estimated incidence of 1 to 2 per 100 000, and it can have a variety of presentations ranging from subclinical to severe cardiac dysfunction.1 Viruses, including Epstein-Barr virus (EBV), are the most common cause of myocarditis in children.1 Thus, physicians usually look for a viral prodrome preceding any cardiac signs or symptoms.1 While the typical features of EBV infection are those of infectious mononucleosis, including fatigue, fever, pharyngitis, splenomegaly, and prominent lymphadenopathy, any organ system can be affected, including the myocardium.2 Here we report a case of EBV infection presenting initially as myocarditis, followed 7 days later by the typical symptoms of infectious mononucleosis.
Case
A 17-year-old male patient contacted the on-call family physician with a complaint of sudden-onset, throbbing, bilateral shoulder and arm pain that woke him from sleep, without a clear trigger or any focal neurologic symptoms. He had taken ibuprofen once without any relief. He also described slight discomfort in the upper chest, bilaterally near the collarbone, and central back pain. He reported a recent upper respiratory tract infection and had a residual mild cough, but no other respiratory symptoms or sore throat. The patient was also experiencing generalized weakness and reduced appetite.
The medical history of the patient was relevant only for a diagnosis of attention deficit disorder for which he was taking methylphenidate. He was active in sports without any recent hospitalizations or substantial illness. Although the patient was initially advised to attend the clinic for assessment, he presented to the pediatric emergency department owing to considerable concern about his pain.
On examination, the patient was afebrile with normal vital signs, and findings of cardiovascular, respiratory, and neurologic examinations were normal. He was noted to have a slight cervical lymphadenopathy and mild left upper quadrant abdominal tenderness. Based on the initial assessment, he was believed to have a nonspecific viral illness, but a workup was initiated.
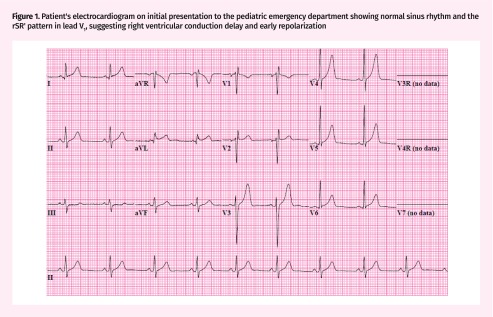
Laboratory investigations revealed normal complete blood count, electrolyte levels, and creatinine level, but a troponin I level of 14 762 ng/L (normal level < 30.9 ng/L) and a creatine kinase level of 747 U/L (normal level 55 to 370 U/L), as well as slight elevations in liver enzyme levels (Table 1). A 12-lead electrocardiogram (ECG) showed normal sinus rhythm and the rSR’ pattern in lead V1, suggesting right ventricular conduction delay and early repolarization (Figure 1). Findings of a chest x-ray scan were normal. Transthoracic echocardiography was performed, findings of which showed good biventricular systolic function with no regional wall abnormalities and no pericardial effusion. Ultrasound of the abdomen was not performed.
In the emergency department, he received 1000 mg of acetaminophen and 162.5 mg of acetylsalicylic acid. He was assessed by a cardiologist and was discharged home with ibuprofen for pain control. In follow-up, he was seen by another cardiologist who made a diagnosis of myocarditis, presumed to be viral in cause.
When he was seen 5 days later in the family medicine clinic, his pain had markedly improved, with complete resolution of chest and back pain but some persistence of the bilateral shoulder and arm pain with movement. He also continued to complain of generalized fatigue. On examination at that time, he had persistent cervical lymphadenopathy but no other findings. He presented again 2 days later with a worsening sore throat and was found to have increased lymphadenopathy, tonsillar hypertrophy, and exudates. Repeat bloodwork showed a normal white blood cell count with a slight increase in lymphocytes, a return of troponin I and creatine kinase to normal levels, and continued mild elevation of liver enzyme levels (Table 1). Findings of a throat swab culture were negative for streptococcus, but mononuclear spot test results for EBV were positive.
The final diagnosis made was EBV infection with initial presentation as myocarditis, followed 1 week later by the more typical picture of infectious mononucleosis.
Table 1.
Patient’s selected laboratory investigation results, at presentation to the pediatric ED and in clinic follow-up 7 d later
| LABORATORY INVESTIGATION | PEDIATRIC ED VISIT | CLINIC FOLLOW-UP 7 D LATER* |
|---|---|---|
| Troponin I | 14 762 ng/L (normal < 30.9 ng/L) | NA |
| Troponin T | NA | 14 ng/L (normal < 15 ng/L) |
| Creatine kinase | 747 U/L (normal 55–370 U/L) | 105 U/L (normal < 247 U/L) |
| Alanine aminotransferase | 61 U/L (normal < 42 U/L) | 94 U/L (normal < 40 U/L) |
| Aspartate aminotransferase | 94 U/L (normal < 41 U/L) | 48 U/L (normal < 37 U/L) |
ED—emergency department, NA—not applicable.
Different institution and laboratory.
Figure 1.
Patient’s electrocardiogram on initial presentation to the pediatric emergency department showing normal sinus rhythm and the rSR’ pattern in lead V1, suggesting right ventricular conduction delay and early repolarization
Discussion
Several diagnostic challenges were highlighted in this case. The patient was initially assessed by 2 different clinicians as having a nonspecific viral illness, before a shift to focus on his chest pain. While EBV was part of the differential diagnosis, it was not tested for at that time, although cardiac investigations were pursued.
The criterion standard for the diagnosis of myocarditis is endomyocardial biopsy, but it is often not practical or reasonable to perform this test, as in this case.3 The European Society of Cardiology Working Group on Myocardial and Pericardial Diseases has proposed diagnostic criteria for suspected myocarditis.3 These include at least 1 clinical feature (acute chest pain, new-onset or worsening dyspnea or fatigue, and palpitations and arrhythmia or cardiogenic shock) and at least 1 diagnostic feature (ECG or Holter monitor findings, elevated troponin T or I levels, functional or structural cardiac abnormalities on imaging, or tissue characterization by cardiovascular magnetic resonance imaging).3 In our case, the diagnosis was made based on acute chest pain and an elevated troponin I level; however, the diagnosis is not definitive without invasive testing. Likewise, it cannot be confirmed that the underlying cause is EBV, given the presence of another upper respiratory infection before the myocarditis. The mononuclear spot test has a specificity of 95% to 100%.4 It can be falsely positive for some other viruses and has the limitation that low levels of heterophile antibodies can persist for 9 to 12 months after EBV infection.4 However, our patient went on to exhibit the classic features of mononucleosis and his previous upper respiratory tract symptoms might have been the early stages of the EBV infection itself. Additionally, there are several other case reports of EBV infection causing myocarditis.5–7 In one of these cases, the patient, also a 17-year-old, had a concurrent nonspecific viral illness, later identified as EBV infection, in addition to chest pain and pericardial effusion.5 In 2 other cases, as in our patient, myocarditis preceded the typical symptoms of infectious mononucleosis by at least several days.6,7 In one case, a 23-year-old presented with symptoms, cardiac enzyme levels, and ECG findings that were sufficiently concerning for myocardial ischemia that coronary angiography was performed before the diagnosis of myocarditis was made. Myocardial biopsies revealed EBV and the symptoms of mononucleosis appeared 10 days later.6 Similarly, in a less severe case, a 20-year-old man presented initially with chest pain with radiation into both arms, ST changes on ECG, and elevated cardiac and liver enzyme levels.7 The symptoms of sore throat, fever, and cervical lymphadenopathy appeared 3 days later and EBV infection was confirmed as the cause.7
Conclusion
As EBV infection is common in the young adult population, it is important for clinicians to look for symptoms beyond those of typical mononucleosis, as well as follow up on any subsequent clinical changes.
Editor’s key points
▸ Epstein-Barr virus infection in young adults can present as myocarditis and not with the classic features of pharyngitis, lymphadenopathy, fever, and fatigue.
▸ The signs and symptoms of infectious mononucleosis might follow, rather than precede, a presentation of Epstein-Barr virus infection as myocarditis.
▸ Diagnosing myocarditis requires a high index of suspicion, and the diagnosis might not be definitive without invasive testing, although diagnostic criteria have been proposed. Invasive testing is often not practical or reasonable.
Points de repère du rédacteur
▸ Chez les jeunes adultes, l’infection au virus d’Epstein-Barr peut se présenter sous la forme d’une myocardite plutôt que sous les caractéristiques habituelles comme la pharyngite, la lymphadénopathie, la fièvre et la fatigue.
▸ Les signes et les symptômes de la mononucléose infectieuse peuvent suivre, au lieu de précéder, la présentation d’une infection au virus d’Epstein-Barr sous forme de myocardite.
▸ Le diagnostic d’une myocardite exige un fort degré de suspicion, et il pourrait ne pas être définitif sans des tests invasifs, quoique des critères diagnostiques aient été proposés. Les tests invasifs ne sont souvent pas pratiques ni raisonnables.
Footnotes
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.Allan CK, Fulton DR. Clinical manifestations and diagnosis of myocarditis in children. Waltham, MA: UpToDate; 2019. Available from: https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-myocarditis-in-children. Accessed 2019 Apr 9. [Google Scholar]
- 2.Sullivan JL. Clinical manifestations and treatment of Epstein-Barr virus infection. Waltham, MA: UpToDate; 2019. Available from: https://www.uptodate.com/contents/clinical-manifestations-and-treatment-of-epstein-barr-virus-infection. Accessed 2019 Apr 9. [Google Scholar]
- 3.Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34(33):2636–48. doi: 10.1093/eurheartj/eht210. 2648a–d. Epub 2013 Jul 3. [DOI] [PubMed] [Google Scholar]
- 4.Stuempfig ND, Seroy J. Monospot test. Treasure Island, FL: StatPearls Publishing; 2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539739/. Accessed 2019 May 13. [PubMed] [Google Scholar]
- 5.Roubille F, Gahide G, Moore-Morris T, Granier M, Davy JM, Vernhet H, et al. Epstein Barr virus (EBV) and acute myopericarditis in an immunocompetent patient: first demonstrated case and discussion. Intern Med. 2008;47(7):627–9. doi: 10.2169/internalmedicine.47.0691. Epub 2008 Apr 1. [DOI] [PubMed] [Google Scholar]
- 6.Walenta K, Kindermann I, Gärtner B, Kandolph R, Link A, Böhm M. Dangerous kisses: Epstein-Barr virus myocarditis mimicking myocardial infarction. Am J Med. 2006;119(5):e3–6. doi: 10.1016/j.amjmed.2005.11.033. [DOI] [PubMed] [Google Scholar]
- 7.Zabala López S, Vicario JM, LerÍn FJ, Fernández A, Pérez G, Fonseca C. Epstein-Barr virus myocarditis as the first symptom of infectious mononucleosis. Intern Med. 2010;49(6):569–71. doi: 10.2169/internalmedicine.49.2719. Epub 2010 Mar 15. [DOI] [PubMed] [Google Scholar]