Abstract
Objective
To examine trends in and sociodemographic predictors of the provision of obstetric care within the primary care context among physicians in British Columbia (BC).
Design
Population-based, longitudinal cohort study using administrative data.
Setting
British Columbia.
Participants
All primary care physicians practising in BC between 2005–2006 and 2011–2012.
Main outcome measures
Fee-for-service payment records were used to identify the provision of prenatal and postnatal care and deliveries. The proportions of physicians who attended deliveries and who included any obstetric care provision in their practices were examined over time using longitudinal mixed-effects log-linear models.
Results
The proportion of physicians attending deliveries or providing any obstetric care declined significantly over the study period (deliveries: odds ratio [OR] of 0.92, 95% CI 0.89–0.95; obstetric care: OR = 0.92, 95% CI 0.89–0.95), and obstetric care provision accounted for a smaller proportion of overall practice activity (OR = 0.96, 95% CI 0.94–0.99). Female physicians had higher odds of including obstetric care in their practices (OR = 1.46, 95% CI 1.27–1.69), and by 2011–2012 had significantly higher odds of attending deliveries (OR = 1.22, 95% CI 1.05–1.38). Older physicians and those located in metropolitan centres were less likely to provide obstetric care or attend deliveries.
Conclusion
The provision of obstetric care by primary care physicians in BC declined over this period, suggesting the possibility of a growing access issue, particularly in rural and remote communities where family physicians are often the sole providers of obstetric services.
Résumé
Objectif
Examiner les tendances et les indices démographiques dans la prestation des soins obstétriques dans le contexte des soins primaires chez les médecins en Colombie-Britannique (C.-B.).
Type d’étude
Étude de cohorte longitudinale populationnelle, à l’aide de données administratives.
Contexte
Colombie-Britannique.
Participants
Tous les médecins de soins primaires en pratique active en C.-B. entre 2005–2006 et 2011–2012.
Principaux paramètres à l’étude
Les dossiers de rémunération à l’acte ont servi à cerner la prestation des soins prénatals et postnatals, de même que les accouchements. Les proportions de médecins qui assistaient aux accouchements et qui incluaient la prestation de soins obstétriques, quels qu’ils soient, ont été mesurées au fil des ans à l’aide de modèles log-linéaires longitudinaux à effets mixtes.
Résultats
La proportion de médecins qui procédaient aux accouchements ou offraient des soins obstétriques a baissé de manière significative durant la période à l’étude (accouchements : rapport de cotes [RC] de 0,92, IC à 95 % de 0,89 à 0,95; soins obstétriques : RC = 0,92, IC à 95 % de 0,89 à 0,95), et la prestation des soins obstétriques représentait une proportion plus faible des activités de la pratique dans son ensemble (RC = 0,96, IC à 95 % de 0,94 à 0,99). La possibilité que les femmes médecins incluent les soins obstétriques dans leur pratique était plus élevée (RC = 1,46, IC à 95 % de 1,27 à 1,69), et en 2011–2012, la possibilité de procéder aux accouchements était significativement plus grande (RC = 1,22, IC à 95 % de 1,05 à 1,38). Il était moins probable que les médecins plus âgés et ceux situés dans les centres métropolitains offrent des soins obstétriques ou fassent des accouchements.
Conclusion
La prestation des soins obstétriques par les médecins de soins primaires en C.-B. a connu un déclin au cours de la période étudiée, ce qui laisse présager la possibilité de problèmes d’accès grandissants, surtout dans les collectivités rurales et éloignées où les médecins de famille sont souvent les seuls prestataires de services obstétriques.
Obstetric care provided by primary care physicians, including prenatal (in pregnancy), intrapartum (labour and delivery), and postpartum care (after delivery), is an essential service in Canada,1 providing enhanced continuity of care, which is highly valued by patients.2 There is also some evidence suggesting that rates of cesarean section are lower for family physicians compared with obstetricians3–5 and that deliveries performed by family physicians are more cost-effective5; however, this might be owing to incomplete adjustment for differences in the patient populations.6,7 Rates of perinatal mortality and adverse maternal outcomes are similar.8 Family physicians are also often the only option for obstetric care for women living in rural and remote jurisdictions.9,10
There is some evidence to suggest that family physician–led obstetric care (and attendance at deliveries in particular) is becoming less common.11,12 Since the early 1990s, the proportion of Canadian primary care physicians including obstetric care in their practices has fallen from approximately 86% in 1991–1992 to 71% 2009–2010.11,13–15 This decline might be owing to logistic and financial considerations,16 such as the effect of workload on lifestyle, concerns about legal liability, an insufficient number of cases, or insufficient compensation.17 The Canadian Medical Protective Association, a mutual defence organization for physicians, charges a differential fee for family physicians depending on whether they include labour and deliveries in their practices: $11 150 if these services are included and $4020 if they are not18; however, most of the differential fees are reimbursed in British Columbia (BC) and are therefore unlikely to be a deterrent to obstetric care provision in the context of this study.
For low-risk deliveries, women in the province of BC can seek obstetric care from a midwife, a family physician, or an obstetrician. Between 2007–2008 and 2015–2016, the proportion of deliveries with midwifery-involved care increased from 6.7% to 22.4%,19,20 reflecting increased consumer demand21 and increased supply of midwives largely owing to provincial investment in midwifery education.22 In spite of these investments, demand for midwifery care outstrips supply.23 Over the same period, the proportion of all deliveries attended by obstetricians was largely stable, ranging from 49.9% to 50.7%,19,20,24 and the proportion attended by family physicians fell from 39.7% to 30.9%.19,20,24 (This trend is not specific to low-risk deliveries and instead reflects attendance at all births.)
Primary care physician work force demographic characteristics are shifting. There are more women,25,26 there are more international medical graduates, particularly practising in rural and remote areas,27,28 and the average age of the work force has increased.29 These shifts could help to explain trends in the provision of obstetric care if there are demographic differences in service provision; however, research in this area is limited and dated.30,31
The Ministry of Health and Doctors of BC (the professional association for BC’s physicians) have implemented policy changes aimed at reversing the exodus of primary care physicians from obstetric care, in recognition of the importance of family physicians in ensuring high-quality and accessible obstetric care across the province.12,13 In 2003, an “obstetrical premium” was added to an existing fee code, providing a 50% bonus for deliveries.32 In 2006, a maternity care network payment was introduced, which helps cover the costs of group or network activities for the shared care of obstetric patients.32,33 Most recently, in 2008, the Maternity Care for BC program was launched, which makes training available to primary care physicians wishing to incorporate obstetric care into their practices and to new medical graduates.34,35 A total of $2.5 million was budgeted for the program between 2008 and 2013, and during that period, 74 physicians enrolled (slightly more than 1% of the primary care physician population).34
This study examines trends in both participation in the provision of obstetric care and deliveries and the quantity of such services delivered during the period in which some of these incentives and programs were introduced. We also examine the demographic correlates of obstetric care provision among primary care physicians in BC to assess the possible effect of work force demographic shifts on levels of obstetric care provision.
METHODS
Design, population, and data sources
This population-based retrospective cohort study used administrative physician payment data in BC for the period 2005–2006 to 2011–2012. We used the College of Physicians and Surgeons of British Columbia’s registry to identify all primary care physicians who billed for fee-for-service activity and as a source of demographic data.36 We obtained records of fee-for-service payments from the Medical Services Plan physician payment file, which contains records of all such activity at the level of the individual physician-patient-date combination.37 We also included payments to physicians under non–fee-for-service payment arrangements from an Alternative Payment Program database.38 While this database does not contain information about services delivered to individual patients, we included it to account for the fact that the fee-for-service payments were not a complete measure of clinical activity, and the percentage of activity they represent varies by physician demographic characteristics.39 In order to characterize the demographic and morbidity characteristics of physicians’ patient populations, we included patient data from the Medical Services Plan consolidation file and the Discharge Abstract Database.40,41 We obtained ethics approval for this study from the University of British Columbia Behavioural Research Ethics Board.
The cohort included all physicians in BC who had a primary care specialty and who provided any clinical care during at least 1 study year (2005–2006 to 2011–2012).
Outcome variables: assessment of obstetric care provision
We used specific fee codes to identify obstetric (prenatal, postnatal, intrapartum) care.14 We classified physicians according to whether they were paid for 1 or more deliveries and whether they provided any obstetric care for each study year. Among those physicians who did provide these services, we computed the annual proportion of the care they delivered that was related to obstetric services (number of patient encounters with an obstetric fee code divided by the total number of patient encounters in each year).
Explanatory variables
We included physician demographic and patient population variables to examine trends in obstetric care provision over the study period. We included physician demographic and practice variables: location of practice (metropolitan, urban-dominated, or rural-dominated region, as defined in previous research),42 training (within or outside of Canada), age, and sex. We also included the proportion of each physician’s remuneration that was generated through non–fee-for-service sources. To characterize patient populations, we included the proportion of the physician’s patient contacts that were with women of childbearing age (18–44 years), with patients in the lowest income quintile, and with patients who had considerable morbidity (defined as the presence of 1 or more conditions considered “major” in the Johns Hopkins Aggregated Diagnostic Groups).43,44
Data analyses
We used
 2 tests for unadjusted differences between physicians who provided deliveries and those who did not, and between those who provided any obstetric care and those who provided none, across demographic categories and study years. Among physicians who provided at least some obstetric care, we used ANOVA (analysis of variance) to determine whether the proportion of overall clinical care related to obstetric care varied by study year or across physician and patient demographic characteristic groups.
2 tests for unadjusted differences between physicians who provided deliveries and those who did not, and between those who provided any obstetric care and those who provided none, across demographic categories and study years. Among physicians who provided at least some obstetric care, we used ANOVA (analysis of variance) to determine whether the proportion of overall clinical care related to obstetric care varied by study year or across physician and patient demographic characteristic groups.
We modeled whether a physician received fee-for-service payment for any deliveries in each study year using a mixed-effects logistic model. We included physician sex, other physician demographic characteristics, the proportion of remuneration from alternative sources, and patient demographic characteristics as model covariates.
We used a 2-part modeling strategy to examine the provision of obstetric care overall. First, we modeled whether a physician billed for any obstetric care in each study year using a mixed-effects logistic model. Second, we modeled the proportion of their overall activity that was related to obstetric care only among those physicians whom we identified as providing at least 1 obstetric visit using a logit-transformed outcome and a normal linear mixed-effects model. Both models included the same set of physician and patient covariates.
RESULTS
The cohort used for the study is described in detail elsewhere.42 We identified 6579 physicians who were active for at least some portion of the study period (Table 1).42 Unadjusted, a larger percentage of female physicians received remuneration for prenatal and postnatal care and for deliveries, compared with male physicians (43.8% vs 30.6%, P < .0001, and 18.6% vs 12.2%, P < .0001, respectively). Female physicians also devoted a larger proportion of overall activity to obstetric care (4.6% vs 1.4%, P < .0001).
Table 1.
Demographic characteristics for full study cohort (N = 6579) and bivariate results
| CHARACTERISTIC | MALE PHYSICIANS, N = 4110 (62.7%) | FEMALE PHYSICIANS, N = 2469 (37.3%) | TOTAL, N = 6579 |
|---|---|---|---|
| Mean (SD) age, y, in 2011–2012* | 53.6 (12.7) | 46.6 (11.0) | 51.0 (12.5) |
| Age group in 2011–2012,† n (%) | |||
| • < 35 y | 293 (7.1) | 383 (15.5) | 676 (10.3) |
| • 35 to < 45 y | 761 (18.5) | 712 (28.8) | 1473 (22.4) |
| • 45 to < 55 y | 1115 (27.1) | 769 (31.1) | 1884 (28.6) |
| • 55 to < 65 y | 1102 (26.8) | 463 (18.8) | 1565 (23.8) |
| • ≥ 65 y | 839 (20.4) | 142 (5.8) | 981 (14.9) |
| Trained internationally,‡ % | 1370 (33.3) | 580 (23.5) | 1950 (29.6) |
| Practice rurality in 2011–2012,§ % | |||
| • Metropolitan | 1885 (45.9) | 1269 (51.4) | 3154 (47.9) |
| • Urban dominated | 877 (21.3) | 496 (20.1) | 1373 (20.9) |
| • Rural dominated | 557 (13.6) | 309 (12.5) | 866 (13.2) |
| • Not active | 759 (18.5) | 365 (14.8) | 1124 (17.1) |
| Compensation (averaged for 2005–2006 to 2011–2012) | |||
| • Mean (SD) total compensation,ǁ $ | 232 122 (146 994) | 148 434 (101 222) | 200 715 (137 780) |
| • Mean (SD) alternative payments,¶ $ | 33 486 (59 059) | 28 106 (50 099) | 31 467 (55 922) |
| Attended any deliveries,# n (%) | 503 (12.2) | 458 (18.6) | 961 (14.6) |
| Provided any prenatal or postnatal care,** n (%) | 1256 (30.6) | 1081 (43.8) | 2337 (35.5) |
| Proportion (SD) of care related to obstetrics†† | 1.4 (3.9) | 4.6 (9.8) | 2.7 (7.2) |
Wilcoxon-Mann-Whitney Z = −21.1, P < .0001.
 2 = 452.1, P < .0001.
2 = 452.1, P < .0001.
 2 = 71.7, P < .0001.
2 = 71.7, P < .0001.
 2 = 12.7, P = .0053. Missing: 62 (0.9%)—30 (1.2%) female physicians, 32 (0.8%) male physicians.
2 = 12.7, P = .0053. Missing: 62 (0.9%)—30 (1.2%) female physicians, 32 (0.8%) male physicians.
Wilcoxon-Mann-Whitney, Z = −23.7, P < .0001.
Wilcoxon-Mann-Whitney, Z = −3.3, P = .0006.
 2 = 52.3, P < .0001.
2 = 52.3, P < .0001.
 2 = 128.0, P < .0001.
2 = 128.0, P < .0001.
Computed only for those who included any obstetric care in their practices; ANOVA (analysis of variance) F = 195.5, P < .0001. Demographic data presented were previously published in Hedden et al.42
Deliveries
Adjusting for other physician and patient population characteristics, we found no significant difference in the odds of attending deliveries between male and female primary care physicians at the beginning of the period (combined odds ratio [OR] of 0.89, 95% CI 0.72–1.05*). By 2011–2012, however, female physicians had significantly higher odds of attending deliveries (combined OR = 1.21, 95% CI 1.05–1.38*). The odds of attending deliveries were lower among physicians aged 65 or older (OR = 0.36, 95% CI 0.30–0.44) compared with those younger than 35, and among those located in metropolitan areas (OR = 0.29, 95% CI 0.24–0.35) compared with those in rural areas (Table 2). In general, physicians who trained internationally had higher odds of attending deliveries (OR = 1.30, 95% CI 1.08–1.56); however, this relationship interacted with practice location: among physicians located in metropolitan areas, those who trained internationally had lower odds of attending compared with those who trained within Canada (combined OR = 0.27, 95% CI 0.10–0.43).
Table 2.
Multivariate models for the odds of providing obstetric care (2005–2006 to 2011–2012)
| VARIABLES | MODEL | |
|---|---|---|
|
| ||
| DELIVERIES, OR (95% CI) | ANY OBSTETRIC CARE, OR (95% CI) | |
| Female sex | 0.84 (0.72–0.98)* | 1.46 (1.27–1.69)† |
| Year (continuous) | 0.92 (0.89–0.95)† | 0.92 (0.89–0.95)† |
| Female sex–year interaction | 1.05 (1.02–1.09)‡ | 1.02 (0.99–1.04) |
| Rurality-time interaction | ||
| • Metropolitan | 0.98 (0.94–1.01) | 1.01 (0.98–1.04) |
| • Urban | 0.97 (0.93–1.00) | 0.96 (0.92–1.00)* |
| Age, y | ||
| • 35 to < 45 y | 0.76 (0.69–0.85)† | 0.78 (0.71–0.86)† |
| • 45 to < 55 y | 0.79 (0.70–0.88)† | 0.76 (0.68–0.84)† |
| • 55 to < 65 y | 0.63 (0.55–0.71)† | 0.68 (0.61–0.76)† |
| • ≥ 65 y | 0.36 (0.30–0.44)† | 0.50 (0.44–0.58)† |
| Rurality | ||
| • Metropolitan | 0.29 (0.24–0.35)† | 0.52 (0.43–0.63)† |
| • Urban | 0.71 (0.58–0.87)* | 0.84 (0.68–1.04) |
| International training | 1.30 (1.08–1.56)* | 1.69 (1.39–2.05)† |
| Rurality-training interaction | ||
| • Metropolitan-international | 0.70 (0.55–0.89)* | 0.80 (0.64–0.99)* |
| • Urban-international | 0.80 (0.63–1.02) | 0.87 (0.68–1.10) |
| Higher proportion of alternative payments | 0.35 (0.30–0.41)† | 0.30 (0.27–0.33)† |
| Higher proportion of contacts with female patients aged 18–44 y | 14.26 (10.78–18.87)† | 2.79 (2.18–3.58)† |
| Higher proportion of contacts with patients with ≥ 1 major ADGs | 0.44 (0.73–1.20) | 0.34 (0.28–0.41)† |
| Higher proportion of contacts with patients in the lowest income quintile | 0.48 (0.32–0.60)† | 0.67 (0.53–0.86)* |
ADG—Aggregated Diagnostic Groups, OR—odds ratio.
P < .05.
P < .0001.
P < .001.
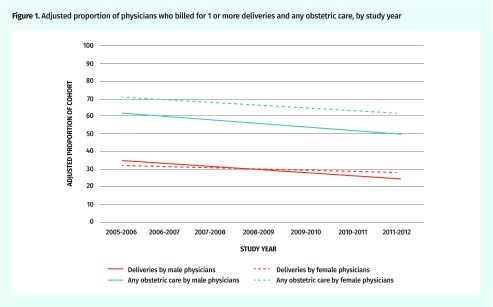
The adjusted odds of attending deliveries declined significantly over the study period (OR = 0.92, 95% CI 0.89–0.95). This reflects 30.2% and 12.4% declines in the proportion of male and female physicians respectively providing deliveries (from 35.1% to 24.5% of men and 32.3% to 28.3% of women) (Figure 1).
Figure 1.
Adjusted proportion of physicians who billed for 1 or more deliveries and any obstetric care, by study year
Any obstetric care provision
Female physicians had higher odds of including obstetric care in their practices (OR = 1.46, 95% CI 1.27–1.69). The odds of including obstetric care in practice declined with successive age groups (eg, OR for physicians aged ≥ 65 vs < 35: 0.50, 95% CI 0.44–0.58) and were also lower for those physicians in metropolitan compared with rural areas (OR = 0.52, 95% CI 0.43–0.63). Internationally trained physicians had higher odds of including obstetric care in their practices (OR = 1.69, 95% CI 1.39–2.05); however, this difference was only statistically significant for those physicians located in rural or urban areas, not in metropolitan centres.
The adjusted proportion of physicians providing any obstetric care declined significantly over the study period for physicians across all demographic groupings (OR = 0.92, 95% CI 0.89–0.95). This corresponds to 19.2% and 12.3% reductions in the adjusted proportion of male and female physicians, respectively, who included obstetric care in their practices.
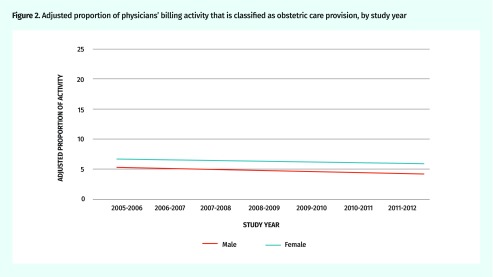
Obstetric care accounted for a significantly larger proportion of overall care provision among female physicians (OR = 1.25, 95% CI 1.09–1.43) (Table 3). Physicians in the older age categories (eg, OR for physicians aged ≥ 65 vs < 35: 0.76, 95% CI 0.66–0.87) devoted a significantly smaller proportion of their practice to the provision of obstetric care; however, we found no difference in the proportion of time spent on obstetric care provision by location of practice or training. We also found a small, borderline statistically significant decline in the proportion of care provision related to obstetrics over the study period (OR = 0.96, 95% CI 0.94–0.99) (Figure 2).
Table 3.
Multivariate model for the proportion of billings related to obstetric care
| VARIABLES | OR (95% CI) |
|---|---|
| Female sex | 1.25 (1.09–1.43)* |
| Year (continuous) | 0.96 (0.94–0.99)* |
| Female sex–year interaction | 1.02 (1.00–1.04) |
| Rurality-time interaction | |
| • Metropolitan | 0.98 (0.95–1.00) |
| • Urban | 0.95 (0.92–0.98)* |
| Age, y | |
| • 35 to < 45 | 0.84 (0.78–0.91)† |
| • 45 to < 55 | 0.80 (0.73–0.88)† |
| • 55 to < 65 | 0.75 (0.68–0.84)† |
| • ≥ 65 | 0.76 (0.66–0.87)‡ |
| Rurality | |
| • Metropolitan | 0.87 (0.73–1.02) |
| • Urban | 1.11 (0.92–1.33) |
| International training | 0.92 (0.76–1.10) |
| Rurality-training interaction | |
| • Metropolitan-international | 0.88 (0.72–1.09) |
| • Urban-international | 0.81 (0.65–1.02) |
| Higher proportion of alternative payments | 1.43 (1.23–1.65)† |
| Higher proportion of contacts with female patients aged 18–44 y | 1329.42 (955.18–1850.29)† |
| Higher proportion of contacts with patients ≥ 1 major ADGs | 1.49 (1.12–1.97)* |
| Higher proportion of contacts with patients in the lowest income quintile | 0.78 (0.56–1.11) |
ADG—Aggregated Diagnostic Groups, OR—odds ratio.
P < .05
P < .0001.
P < .001.
Figure 2.
Adjusted proportion of physicians’ billing activity that is classified as obstetric care provision, by study year
The characteristics of the patient population had a consistent influence on physician attendance at deliveries and provision of obstetric care (Tables 2 and 3). Physicians whose practices had more contacts with female patients of childbearing age were unsurprisingly more likely to provide these services. On the other hand, physicians whose practices included more contacts with patients in the lowest income quintile had significantly lower odds of providing them (deliveries: OR = 0.48, 95% CI 0.32–0.60; obstetric care: OR = 0.67, 95% CI 0.53–0.86).
DISCUSSION
There is robust evidence suggesting that the comprehensiveness of primary care might be declining11,12 and that prenatal, postpartum, and intrapartum care are key areas being phased out in favour of a narrowed scope of practice.11,13–15 Our findings lend support to the existing evidence in this area: between 2005–2006 and 2011–2012, the adjusted proportion of family physicians who attended deliveries or provided any obstetric care declined by 16.1%. By the end of the period, 84.7% of male and 77.2% of female family physicians did not attend deliveries and 61.6% of male and 45.6% of female family physicians provided no obstetric care. This represents a substantial decline from the estimates provided by Lavergne and colleagues, which suggested that 29% of physicians did not include any obstetric care provision in their practices in 2009–2010.12 Furthermore, the fact that physicians who still include obstetric care in their practices are providing this care considerably less often suggests that absolute attrition is not being offset by increased relative activity in this area among physicians still providing these services.
These trends occurred over a period of considerable investment in obstetric care provided by family physicians and the development of a new training program. While we cannot know with certainty whether the observed attrition from obstetric care would have been more substantial without these incentives and investments, at the very least these investments were not able to halt the attrition.
The proportion of family physicians who are women has increased substantially over the past decade.25,26 We found that female family physicians had higher odds of including obstetric care in their practices and, by the end of the study, of attending deliveries. Among those who did provide obstetric care, female family physicians provided it more often. It follows then that should feminization of the work force continue, it could halt or reverse the trends we observed; however, the overall proportion of family physicians whose practices include obstetric care continues to fall because that proportion is still declining (albeit more slowly) among female family physicians.
Family physicians working in rural areas had higher odds of providing obstetric care and attending deliveries, and those who provided these services did so more often compared with their metropolitan counterparts; however, the provision of prenatal, intrapartum, and postnatal care is falling over time even among these physicians. Family physicians are often the only option for women seeking obstetric care in rural and remote regions,9 and the closure of small maternity clinics in rural areas can lead to an increasing travel distance for women who are in labour or seeking obstetric care more generally, which can increase the rate of adverse perinatal outcomes.10 Finally, the fact that family physicians whose practices included more contacts with patients in the lowest income quintile had lower odds of providing obstetric care and attending deliveries points toward the possible emergence of an access challenge among socioeconomically disadvantaged individuals.
Interprofessional team-based primary care, either including nurses45 or midwives,46 has shown some promise in encouraging physicians to include obstetric care in their practices. Examples of successful models include the South Community Birth Program that provides primary obstetric care via midwives and family physicians to underserved patients in urban Vancouver, BC,4 and the Maternity Centre of Hamilton in Ontario.45
Strengths and limitations
This analysis extends the time period used in the paper by Lavergne and colleagues and also includes the amount of obstetric care provided by each physician in addition to head counts.12 Our study also used physician remuneration data from the Alternative Payment Program database, which includes payments for non–fee-for-service clinical activity. This is a considerable strength because it allowed us to examine the independent effects of demographic and location characteristics on obstetric care provision; these are commonly confounded with preferences for alternative remuneration.47 A limitation associated with the use of these data, however, is that we are only able to access the file up to the 2011–2012 fiscal year. We are not aware of any new policy or work force demographic shifts occurring after the study period that would have stalled or reversed the trends we observed.
A second limitation is that we do not include any data on the patient demand for obstetric services over this period. We are not aware of any studies that directly assess patient demand for obstetric services provided by family physicians, midwives, and obstetricians in the Canadian context. However, the birth rate in BC increased marginally over the study period,48 suggesting that, at the very least, the demand for obstetric care overall did not decline. Among “normal labours” in British Columbia in 2015–2016 (eg, no history of cesarean, singleton cephalic infant at term, after spontaneous onset of labour), family physicians attended the most deliveries (41.7%) compared with obstetricians (33.0%) and midwives (22.5%)19; however, this is a substantial drop from attending 64.6% of “normal labours” in 2007–2008.20 This is likely indicative of some redistribution of care between family physicians and midwives, and while midwives are becoming involved in a greater proportion of low-risk obstetric care, consumer demand for this model of care has outpaced availability, particularly in rural communities,23 where family physicians are often the sole source of maternity care. The continued attrition of primary care physicians from care seems likely to reduce access to a model of continuous care that extends from birth to death,49 and Canadian women value autonomous informed choice as a core component of high-quality obstetric care.50
Finally, the interpretation of the trends we observed could be aided by comparison with experiences in other provinces; however, systematic information on policy and programmatic responses outside of BC were not available at the time of writing. The effect of differential policies on retention of family physicians providing maternity care should be the subject of future research.
Conclusion
Over a period of continued, targeted investments to encourage involvement in obstetric care provision, attrition from this clinical area continued among primary care physicians in BC, and those physicians who still provide these services are providing them less often. This trend might have a disproportionately adverse effect on access to obstetric care in rural and remote locations and among socioeconomically disadvantaged individuals. It also undermines the ability of women across the province to choose their source of prenatal, intrapartum, and postpartum care. Additional research is needed to identify policy interventions beyond training and fee increases that might attract and retain family physicians to provide obstetric care in general and to attend deliveries in particular.
Acknowledgments
The funds for this study were provided through a Canadian Institutes of Health Research Doctoral Research Award. Dr Law received salary support through a Canada Research Chair in Access to Medicines and a Michael Smith Foundation for Health Research Scholar Award. All inferences, opinions, and conclusions drawn in this manuscript are those of the authors and do not reflect the opinions or policies of the data stewards.
Editor’s key points
▸ Obstetric care provided by primary care physicians, including prenatal, intrapartum, and postpartum care, is an essential service in Canada, providing enhanced continuity of care, which is highly valued by patients. However, some evidence suggests that family physician–led obstetric care (and attendance at deliveries in particular) is becoming less common. This study aimed to examine trends in and sociodemographic predictors of the provision of obstetric care by family physicians in British Columbia (BC).
▸ The authors found that despite continued, targeted investments in BC to encourage involvement in obstetric care provision, attrition from this clinical area continued among primary care physicians in BC, and those physicians who still provide these services are providing them less often. This trend might have a disproportionately adverse effect on access to obstetric care in rural and remote locations and among socioeconomically disadvantaged individuals. It also undermines the ability of women across the province to choose their source of prenatal, intrapartum, and postpartum care.
Points de repère du rédacteur
▸ Les soins obstétriques fournis par des médecins de soins primaires, notamment les soins prénatals, intra-partum et post-partum, sont un service essentiel au Canada, et ils assurent la continuité des soins, un élément très valorisé par les patientes. Par ailleurs, certaines données font valoir que les soins obstétriques dirigés par des médecins de famille (surtout l’assistance lors de l’accouchement) deviennent de moins en moins courants. Cette étude avait pour but d’examiner les tendances et les facteurs de prédiction sociodémographiques dans la prestation des soins obstétriques par les médecins de famille en Colombie-Britannique (C.-B.).
▸ Les auteurs ont constaté qu’en dépit d’investissements continus et ciblés pour encourager la participation à la prestation des soins obstétriques en C.-B., l’attrition dans ce domaine clinique a persisté chez les médecins de soins primaires de la province, et les médecins qui offrent encore ces services le font moins souvent. Cette tendance pourrait avoir des effets indésirables disproportionnés sur l’accès aux soins obstétriques dans les régions rurales et éloignées, de même que sur les personnes défavorisées sur le plan socioéconomique. Elle nuit aussi à la capacité des femmes de cette province de choisir leur prestataire de soins prénatals, intra-partum et post-partum.
Footnotes
The combined odds ratio reflects the sum of the odds ratios for sex and the sex-year interaction term, compounded over the 7-year study period.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.Society of Obstetricians and Gynaecologists of Canada, Association of Women’s Health, Obstetric and Neonatal Nurses of Canada, the Canadian Association of Midwives, the College of Family Physicians of Canada, the Society of Rural Physicians of Canada Joint policy statement on normal childbirth. J Obstet Gynaecol Can. 2008;30(12):1163–5. [Google Scholar]
- 2.Public Health Agency of Canada . What mothers say: the Canadian Maternity Experiences Survey. Ottawa, ON: Public Health Agency of Canada; 2009. [Google Scholar]
- 3.Avery DM, Graettinger KR, Waits S, Parton JM. Comparison of delivery procedure rates among obstetrician-gynecologists and family physicians practicing obstetrics. Am J Clin Med. 2014;10(1):16–20. [Google Scholar]
- 4.Harris SJ, Janssen PA, Saxell L, Carty EA, MacRae GS, Petersen KL. Effect of a collaborative interdisciplinary maternity care program on perinatal outcomes. CMAJ. 2012;184(17):1885–92. doi: 10.1503/cmaj.111753. Epub 2012 Sep 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walters D, Gupta A, Nam AE, Lake J, Martino F, Coyte PC. A cost-effectiveness analysis of low-risk deliveries: a comparison of midwives, family physicians and obstetricians. Healthc Policy. 2015;11(1):61–75. [PMC free article] [PubMed] [Google Scholar]
- 6.Nicholson JM. Risk adjustment in maternity care: the use of indirect standardization. Int J Womens Health. 2010;2:255–62. doi: 10.2147/IJWH.S9494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dawe RE, Bishop J, Pendergast A, Avery S, Monaghan K, Duggan N, et al. Cesarean delivery rates among family physicians versus obstetricians: a population-based cohort study using instrumental variable methods. CMAJ Open. 2017;5(4):E823–9. doi: 10.9778/cmajo.20170081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aubrey-Bassler K, Cullen RM, Simms A, Asghari S, Crane J, Wang PP, et al. Outcomes of deliveries by family physicians or obstetricians: a population-based cohort study using an instrumental variable. CMAJ. 2015;187(15):1125–32. doi: 10.1503/cmaj.141633. Epub 2015 Aug 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klein MC, Christilaw J, Johnston S. Loss of maternity care: the cascade of unforeseen dangers. Can J Rural Med. 2002;7(2):1201–1. [Google Scholar]
- 10.Grzybowski S, Stoll K, Kornelsen J. Distance matters: a population based study examining access to maternity services for rural women. BMC Health Serv Res. 2011;11:147. doi: 10.1186/1472-6963-11-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chan BTB. The declining comprehensiveness of primary care. CMAJ. 2002;166(4):429–34. [PMC free article] [PubMed] [Google Scholar]
- 12.Lavergne MR, Peterson S, McKendry R, Sivananthan S, McGrail K. Full-service family practice in British Columbia: policy interventions and trends in practice, 1991–2010. Healthc Policy. 2014;9(4):32–47. [PMC free article] [PubMed] [Google Scholar]
- 13.Kaczorowski J, Levitt C. Intrapartum care by general practitioners and family physicians. Provincial trends from 1984–1985 to 1994–1995. Can Fam Physician. 2000;46(3):587–92. 595–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Lavergne R, McGrail K, Peterson S, Sivanathan S, McKendry R, Mooney D. Defining and measuring full service family practice in BC, 1991–2006. Vancouver, BC: UBC Centre For Health Services And Policy Research; 2013. [Google Scholar]
- 15.Canadian Institute for Health Information . Giving birth in Canada: providers of maternity and infant care. Ottawa, ON: Canadian Institute for Health Information; 2004. [Google Scholar]
- 16.Dove M, Dogba MJ, Rodríguez C. Exploring family physicians’ reasons to continue or discontinue providing intrapartum care. Qualitative descriptive study. Can Fam Physician. 2017;63(8):e387–93. Available from: www.cfp.ca/content/cfp/63/8/e387.full.pdf. Accessed 2019 Oct 9. [PMC free article] [PubMed] [Google Scholar]
- 17.Woodward CA, Rosser W. Effect of medicolegal liability on patterns of general and family practice in Canada. CMAJ. 1989;141(4):291–9. [PMC free article] [PubMed] [Google Scholar]
- 18.Canadian Medical Protective Association . The Canadian Medical Protective Association fee schedule 2017. Ottawa, ON: Canadian Medical Protective Association; 2017. [Google Scholar]
- 19.Perinatal Services BC . Perinatal health report: deliveries in British Columbia 2015/16. Vancouver, BC: Perinatal Services BC; 2017. Available from: www.perinatalservicesbc.ca/Documents/Data-Surveillance/Reports/PHR/2015_16/PHR_BC_2015_16.pdf. Accessed 2019 Oct 9. [Google Scholar]
- 20.British Columbia Perinatal Health Program . Perinatal health report 2008. Vancouver, BC: British Columbia Perinatal Health Program; 2010. Available from: www.perinatalservicesbc.ca/Documents/Data-Surveillance/Reports/SurveillanceAnnualReport2008.pdf. Accessed 2019 Oct 9. [Google Scholar]
- 21.Murray-Davis B, McNiven P, McDonald H, Malott A, Elarar L, Hutton E. Why home birth? A qualitative study exploring women’s decision making about place of birth in two Canadian provinces. Midwifery. 2012;28(5):576–81. doi: 10.1016/j.midw.2012.01.013. Epub 2012 Aug 11. [DOI] [PubMed] [Google Scholar]
- 22.Government delivers agreement with midwives. Vancouver, BC: Government of British Columbia; 2014. Available from: https://news.gov.bc.ca/releases/2014HLTH0136-001892. Accessed 2017 Sep 15. [Google Scholar]
- 23.Barclay L, Kornelsen J. The closure of rural and remote maternity services: where are the midwives? Midwifery. 2015;38:9–11. doi: 10.1016/j.midw.2016.03.007. Epub 2016 Mar 20. [DOI] [PubMed] [Google Scholar]
- 24.Perinatal Services BC . Surveillance perinatal indicators: annual report. British Columbia residents delivering in BC. Vancouver, BC: Perinatal Services BC; 2015. Available from: www.perinatalservicesbc.ca/Documents/Data-Surveillance/Indicators/Annual/AnnualIndicatorsResidence_2013_14_BC.pdf. Accessed 2019 Oct 9. [Google Scholar]
- 25.Association of Faculties of Medicine of Canada . Enrolment in Canadian faculties of medicine by sex, 1968/69-2015/16. Ottawa, ON: Association of Faculties of Medicine of Canada; 2016. [Google Scholar]
- 26.Canadian Resident Matching Service . R-1 match reports, 2014. Ottawa, ON: Canadian Resident Matching Service; 2014. Available from: https://www.carms.ca/data-reports/r1-data-reports. Accessed 2019 Oct 9. [Google Scholar]
- 27.Thind A, Freeman T, Cohen I, Thorpe C, Burt A, Stewart M. Characteristics and practice patterns of international medical graduates: how different are they from those of Canadian-trained physicians? Can Fam Physician. 2007;53(8):1330-1.e1–4. Available from: www.cfp.ca/content/cfp/53/8/1330.full.pdf. Accessed 2019 Oct 9. [PMC free article] [PubMed] [Google Scholar]
- 28.Mick SS, Lee SYD, Wodchis WP. Variations in geographical distribution of foreign and domestically trained physicians in the United States: ‘safety nets’ or ‘surplus exacerbation’? Soc Sci Med. 2000;50(2):185–202. doi: 10.1016/s0277-9536(99)00183-5. [DOI] [PubMed] [Google Scholar]
- 29.Royal College of Physicians and Surgeons of Canada . Age distribution of licensed physician workforce. Ottawa, ON: Royal College of Physicians and Surgeons of Canada; 2017. [Google Scholar]
- 30.Carek PJ, King DE, Hunter M, Gilbert GE. Practice profiles, procedures, and personal rewards according to the sex of the physician. South Med J. 2003;96(8):767–71. doi: 10.1097/01.SMJ.0000056659.05183.62. [DOI] [PubMed] [Google Scholar]
- 31.Keane D, Woodward CA, Ferrier BM, Cohen M, Goldsmith CH. Female and male physicians: different practice profiles. Will increasing numbers of female GPs affect practice patterns of the future? Can Fam Physician. 1991;37:72–81. [PMC free article] [PubMed] [Google Scholar]
- 32.General Practice Services Committee . General Practice Services Committee 2011/2012 annual report. Vancouver, BC: General Practice Services Committee; 2012. [Google Scholar]
- 33.Shapiro JL. Satisfaction with obstetric care. Patient survey in a family practice shared-call group. Can Fam Physician. 1999;45:651–7. [PMC free article] [PubMed] [Google Scholar]
- 34.Dr Vicki Foerster Associates . Maternity Care for British Columbia (MC4BC) evaluation report. Vancouver, BC: General Practice Services Committee; 2013. [Google Scholar]
- 35.Ross S, Armitage M. Reconnecting physicians to primary maternity care. B C Med J. 2014;56(9):458. [Google Scholar]
- 36.College of Physicians and Surgeons of British Columbia . Medical Services Plan physician database. Vancouver, BC: Population Data BC; 2013. [Google Scholar]
- 37.British Columbia Ministry of Health . Medical Services Plan (MSP) payment information file. Version 2. Vancouver, BC: Population Data BC; 2013. [Google Scholar]
- 38.British Columbia Ministry of Health . Alternative Payments Program. Vancouver, BC: Population Data BC; 2013. [Google Scholar]
- 39.Hedden LK. Beyond full-time equivalents: gender differences in activity and practice patterns for BC’s primary care physicians [thesis] Vancouver, BC: University of British Columbia; 2015. [Google Scholar]
- 40.British Columbia Ministry of Health . Consolidation file (MSP registration & premium billing), version 2. Vancouver, BC: Population Data BC; 2013. [Google Scholar]
- 41.Canadian Institute for Health Information . Discharge Abstract Database (hospital separations). Vancouver, BC: Population Data BC; 2011. [Google Scholar]
- 42.Hedden L, Barer ML, McGrail K, Law M, Bourgeault IL. In British Columbia, the supply of primary care physicians grew, but their rate of clinical activity declined. Health Aff (Millwood) 2017;36(11):1904–11. doi: 10.1377/hlthaff.2017.0014. [DOI] [PubMed] [Google Scholar]
- 43.Johns Hopkins University . The Johns Hopkins ACG system. Baltimore, MD: Johns Hopkins University; 2012. Available from: www.acg.jhsph.org/index.php?option=com_content&view=article&id=46&Itemid=366. Accessed 2013 Dec 6. [Google Scholar]
- 44.Health Services Research and Development Centre at Johns Hopkins University . The Johns Hopkins ACG system: technical reference guide. Version 10.0. Baltimore, MD: Johns Hopkins University; 2011. [Google Scholar]
- 45.Price D, Howard M, Shaw E, Zazulak J, Waters H, Chan D. Family medicine obstetrics. Collaborative interdisciplinary program for a declining resource. Can Fam Physician. 2005;51:68–74. [PMC free article] [PubMed] [Google Scholar]
- 46.Munro S, Kornelsen J, Grzybowski S. Models of maternity care in rural environments: barriers and attributes of interprofessional collaboration with midwives. Midwifery. 2013;29(6):646–52. doi: 10.1016/j.midw.2012.06.004. Epub 2012 Aug 3. [DOI] [PubMed] [Google Scholar]
- 47.College of Family Physicians of Canada, Canadian Medical Association, Royal College of Physicians and Surgeons of Canada . National Physician Survey, 2010. Provincial results by FP/GP or other specialist, sex, age, and all physicians: BRITISH COLUMBIA. Mississauga, ON: College of Family Physicians of Canada; 2010. Available from: http://nationalphysiciansurvey.ca/wp-content/uploads/2012/09/2010-ProvBC-Q22.pdf. Accessed 2016 May 24. [Google Scholar]
- 48.Statistics Canada . Estimates of the components of demographic growth, annual. Ottawa, ON: Statistics Canada; 2016. Available from: www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/demo04a-eng.htm. Accessed 2017 Sep 20. [Google Scholar]
- 49.Pimlott N. A glimpse of the future. Can Fam Physician. 2013;59:1031. (Eng), 1032 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 50.Sword W, Heaman MI, Brooks S, Tough S, Janssen PA, Young D, et al. Women’s and care providers’ perspectives of quality prenatal care: a qualitative descriptive study. BMC Pregnancy Childbirth. 2012;12(1):29. doi: 10.1186/1471-2393-12-29. [DOI] [PMC free article] [PubMed] [Google Scholar]