Abstract
Objective
To assess the quality of point-of-care ultrasound (POCUS) training in family medicine residency programs and to obtain the opinions of current family medicine residents on the role of ultrasound in primary care.
Design
A 23-question online survey conducted using SurveyMonkey between March 15 and June 30, 2017.
Setting
Canada.
Participants
All family medicine residents of the 17 Canadian family medicine residency programs were included in the study but all enhanced skills residents were excluded.
Main outcome measures
The quality and relevance of POCUS to primary care as perceived by residents and reported in the survey.
Results
A total of 854 Canadian family medicine residents responded, for a national response rate of 32.3%. Most respondents (94.3%) believe that POCUS training should be included in family medicine residency programs; however, only 18.4% of respondents currently receive formal training within their residency. Among those without POCUS training, 91.7% are interested in receiving formal training and 29.7% resorted to taking external POCUS courses. Most (77.5%) would consider using ultrasound in their future practice if they were competent in POCUS. The most useful applications for family medicine were considered to be the FAST (Focused Assessment with Sonography in Trauma) examination for free fluid and ascites (95.1%), procedural guidance (92.4%), and identifying an intrauterine pregnancy (88.6%).
Conclusion
This is the largest survey identifying the perceived needs of family medicine residents for POCUS. Very few Canadian family medicine residents currently receive POCUS training. Consistent with our recent family medicine program director survey, there is overwhelming interest by family medicine residents to begin incorporating POCUS training into the family medicine curriculum.
Résumé
Objectif
Évaluer la qualité de la formation en échographie au point de service (FEPS) dans les programmes de résidence en médecine familiale, et solliciter les opinions des actuels résidents en médecine familiale sur le recours à l’échographie en soins primaires.
Type d’étude
Un sondage en ligne comportant 23 questions, effectué à l’aide de SurveyMonkey entre le 15 mars et le 30 juin 2017.
Contexte
Canada.
Participants
Tous les résidents en médecine familiale des 17 programmes canadiens de résidence en médecine familiale ont été inclus dans l’étude, sauf les résidents en compétences avancées.
Principaux paramètres à l’étude
La qualité de la formation et la pertinence de l’échographie au point de service en soins primaires telles que perçues par les résidents selon leurs réponses au sondage.
Résultats
Au total, 854 résidents en médecine familiale au Canada ont répondu au sondage, soit un taux de réponse national de 32,3 %. La plupart des répondants (94,3 %) croyaient qu’une FEPS devrait être incluse dans les programmes de résidence en médecine familiale; par ailleurs, seulement 18,4 % des répondants recevaient actuellement une formation formelle dans le cadre de leur résidence. Parmi ceux qui ne suivaient pas une telle formation, 91,7 % ont dit souhaiter recevoir une formation formelle, et 29,7 % recouraient à des cours en échographie au point de service offerts à l’extérieur du programme. La plupart d’entre eux (77,5 %) envisageraient d’utiliser l’échographie dans leur pratique future s’ils avaient la compétence pour ce faire. Ils ont indiqué que les applications les plus utiles en médecine familiale sont l’examen FAST (sigle anglais pour évaluation ciblée par échographie en cas de traumatisme) pour détecter des épanchements de liquides et des ascites (95,1 %); l’orientation vers les interventions nécessaires (92,4 %); et la confirmation d’une grossesse intra-utérine (88,6 %).
Conclusion
Il s’agit du sondage de la plus grande envergure visant à cerner les perceptions qu’ont les résidents en médecine familiale de leurs besoins en FEPS. Conformément aux résultats obtenus dans le récent sondage de la direction de notre programme en médecine familiale, l’intérêt des résidents en médecine familiale à l’égard de l’intégration d’une FEPS dans le cursus en médecine familiale est considérable.
Point-of-care ultrasound (POCUS) has become an essential clinical tool in numerous medical specialties including emergency medicine, anesthesia, and critical care.1–4 Improved diagnostic accuracy, increased patient satisfaction, and decreased complications from invasive procedures have all been associated with its use.5–12
In family medicine clinics, ultrasound has been used for a multitude of clinical applications such as assessment for abdominal aortic aneurysms (AAAs), confirmation of intrauterine pregnancy, guidance for joint injections, and many more.13–16 Evidence supports that POCUS use by family physicians can lead to a reduced number of hospital scans, emergency department admissions, and hospital visits.17
In the United States, a 2015 survey by Hall et al demonstrated that a small but rapidly increasing number of family medicine residency programs were incorporating POCUS training.18 In 2016, the American Academy of Family Physicians published recommended curriculum guidelines for family medicine residents for POCUS, including specific criteria for family medicine residents to achieve competency in its use.19 Following this, in 2017 the University of South Carolina in Columbia published a paper describing their development of a family medicine POCUS curriculum.20
In Canada, a 2016 survey of family medicine residency program directors and academic leads revealed that there is no broadly accepted POCUS curriculum to train family medicine residents and numerous barriers to its implementation exist. However, almost all program directors (93%) believed that POCUS should be integrated into family medicine residency curricula, and 71% believed that POCUS could be used in family medicine clinics to alter clinical decision making.21
Family medicine residents are an important source of information for curriculum development and understanding the perceived needs of the learner.22–24 We aim to assess the quality of POCUS training in family medicine residency programs across Canada and obtain the opinion of current family medicine residents on the role of ultrasound in primary care.
METHODS
A bilingual (English and French) online survey of Canadian family medicine residents was administered between March and June 2017. The survey was developed by a group of 8 POCUS experts, including ultrasound academic leads with extensive teaching experience and publications related to POCUS, as well as input from family medicine residents and a medical student. Our group included physicians from McGill University in Montreal, Que; the University of Ottawa in Ontario; the University of Manitoba in Winnipeg; Memorial University of Newfoundland in St John’s; the University of Toronto in Ontario; and Western University in London, Ont. This survey was designed to ask similar questions to our survey of family medicine program directors to allow for direct comparison.21 Both of these surveys also had strong influence from previous surveys conducted by Steinmetz et al and Hall et al, which were each independently validated, and so we did not repeat external validation and pilot testing of this survey.18,25 The questions were reviewed internally by our group of POCUS experts and altered multiple times to maximize their clarity and avoid any biased language. The survey and study design were approved by the provincial Health Research Ethics Board of Memorial University. The final survey consisted of 3 sections: current training status, perceived relevance of POCUS to primary care, and demographic characteristics. There are 23 items in the survey, including multiple-choice questions with single or multiple answers, rating-scale questions, and Likert-type scales.
All family medicine residents of the 17 Canadian family medicine residency programs were included in the study. Enhanced skills residents were excluded from the study, as many of these programs, such as emergency medicine, already have an integrated POCUS curriculum.
The target population was estimated to be 2645 first- and second-year family medicine residents nationwide based on Canadian Resident Matching Service data and verified by respective site administrators. Survey participants were entered into a random draw for gift cards of $50.
The first survey invitation was sent out via e-mail on March 15, 2017, with reminder e-mails sent 1 and 2 months after the original invitation. The survey was closed on June 30, 2017, at midnight to avoid changes in our survey population associated with the new cohort of residents who started on July 1. The invitation contained a short cover letter, an abstract describing the objectives of the study, and a link to the online consent form and survey. The survey link was sent to the study population through individual e-mail using a private e-mailing list sent by respective resident site coordinators and program administrators; individual e-mail using a private e-mailing list sent by respective resident representatives of the College of Family Physicians of Canada Section of Residents; a survey link included in the e-newsletter of the residency program; a survey link posted on Facebook groups of the residency program; and a private e-mailing list of the Society of Rural Physicians of Canada. To ensure multiple surveys were not completed by the same respondent, only 1 survey submission was accepted from a single IP (Internet protocol) address.
The survey was distributed by SurveyMonkey. Raw data were exported from SurveyMonkey into a Microsoft Excel spreadsheet. A single data abstractor analyzed the survey responses and reported them as percentages in tabular format. Responses were kept anonymous and all data were reported in aggregate.
RESULTS
After removing responses from enhanced skills residents, 854 responses out of a total 2645 first- and second-year Canadian family medicine residents were obtained, for an overall national response rate of 32.3%.
Demographic characteristics
Surveyed population demographic characteristics are summarized in Table 1. We received 672 (78.7%) English responses and 182 (21.3%) French responses. Respondents identified their residency sites as rural (29.6%), urban or community (38.2%), or academic teaching (32.2%). Most residents (91.5%) identified general family practice as their anticipated practice focus, followed by emergency medicine (48.6%), hospitalist medicine (39.0%), and maternal, newborn, and obstetric care (27.2%).
Table 1.
Demographic characteristics of family medicine resident respondents: N = 854 but denominators vary owing to missing data.
| CHARACTERISTIC | N (%)* |
|---|---|
| Year of residency† | |
| • First | 414 (51.7) |
| • Second | 387 (48.3) |
| Preferred language | |
| • English | 672 (78.7) |
| • French | 182 (21.3) |
| University-affiliated residency program‡ | |
| • University of Montreal | 94 (11.8) |
| • University of Alberta | 87 (10.9) |
| • University of Toronto | 86 (10.8) |
| • University of Manitoba | 72 (9.0) |
| • Laval University | 61 (7.6) |
| • McGill University | 48 (6.0) |
| • Dalhousie University | 48 (6.0) |
| • Memorial University of Newfoundland | 46 (5.8) |
| • McMaster University | 45 (5.6) |
| • Northern Ontario School of Medicine | 43 (5.4) |
| • Western University | 38 (4.8) |
| • University of British Columbia | 28 (3.5) |
| • Queen’s University | 28 (3.5) |
| • University of Saskatchewan | 26 (3.3) |
| • University of Ottawa | 19 (2.4) |
| • University of Calgary | 18 (2.3) |
| • University of Sherbrooke | 13 (1.6) |
| International medical graduate§ | |
| • Yes | 95 (11.6) |
| • No | 721 (88.4) |
| Primary site of residency | |
| • Urban or community | 306 (38.2) |
| • Academic teaching unit | 258 (32.2) |
| • Rural area | 237 (29.6) |
| Anticipated focus of clinical practice (select all that apply)† | |
| • General family medicine | 733 (91.5) |
| • Emergency medicine | 389 (48.6) |
| • Hospitalist medicine | 312 (39.0) |
| • Maternal, newborn, and obstetric care | 218 (27.2) |
| • Palliative medicine | 184 (23.0) |
| • Care of the elderly | 158 (19.7) |
| • Child and adolescent health | 136 (17.0) |
| • Sport and exercise medicine | 115 (14.4) |
| • Mental health | 106 (13.2) |
| • Other | 58 (7.2) |
| • Chronic pain | 54 (6.7) |
| • Not sure | 30 (3.7) |
Percentages might not add to 100 owing to rounding.
A total of 801 respondents answered these questions.
A total of 800 respondents answered this question.
A total of 816 respondents answered this question.
Current training status
Most residents (94.3%) believe that POCUS training should be included in family medicine residency programs; however, only 18.4% currently receive formal training. Table 2 summarizes the most commonly reported training experiences among those who have received formal training. Of those who did not receive formal POCUS training, most (91.7%) reported that they are interested in receiving training as part of their residency. Many respondents (29.7%) have sought formal training through external POCUS courses, although most (72.3%) did not receive funding from their residency programs. Most residents (91.6%) believe that funding should be offered to attend an external POCUS course if the residency program does not offer ultrasound training.
Table 2.
Training experiences with POCUS in family medicine residency programs: N = 151. Only the respondents who indicated that they had received formal training in POCUS as part of their family medicine residency were included in this question.
| IN WHAT WAYS HAVE YOU RECEIVED TRAINING IN POCUS DURING YOUR FAMILY MEDICINE RESIDENCY? (SELECT ALL THAT APPLY) | N (%) |
|---|---|
| Practical hands-on teaching with ultrasound equipment | 124 (82.1) |
| Shadowing or observing clinicians or technicians who perform ultrasound | 92 (60.9) |
| Review of ultrasound technique and imaging with didactic teaching | 77 (51.0) |
| Audiovisual instructional material on POCUS | 75 (49.7) |
| External POCUS course paid for by the residency program | 52 (34.4) |
| Residents submit a log of complete ultrasound examinations | 42 (27.8) |
POCUS—point-of-care ultrasound.
Perceived relevance of POCUS to primary care
Most respondents (77.6%) believe that POCUS can enhance clinical decision making in family medicine clinics. Perceived benefits are summarized in Table 3. Most (65.0%) believed that POCUS does not negatively affect patient safety. Most residents (77.5%) responded affirmatively to the statement, “If I had POCUS training during my residency, was competent to use it, and had access to an ultrasound machine, I would use POCUS regularly in my practice.” Upon being presented with the statement “I am familiar with the literature on POCUS,” 33.2% either agreed or strongly agreed, 27.7% indicated they were neutral, and the remainder (39.0%) either disagreed or strongly disagreed.
Table 3.
Resident perceptions on the benefits of POCUS to primary care: N = 812.
| ARE ANY OF THE FOLLOWING POTENTIAL BENEFITS OF POCUS IN PRIMARY CARE? (SELECT ALL THAT APPLY) | N (%) |
|---|---|
| Useful adjunct to the physical examination | 689 (84.9) |
| More rapid diagnoses | 569 (70.1) |
| Reduction in health care costs | 442 (54.4) |
| Improved patient outcomes | 401 (49.4) |
| Improved patient satisfaction | 363 (44.7) |
| Not sure | 26 (3.2) |
| Other | 18 (2.2) |
| No perceived benefit | 10 (1.2) |
POCUS—point-of-care ultrasound.
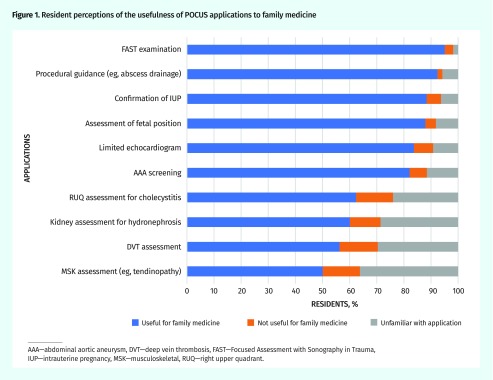
From a list of 10 POCUS applications, residents were asked if they believed specific applications were useful in family medicine; results are summarized in Figure 1. Those believed to be most useful included the Focused Assessment with Sonography in Trauma (FAST) examination for free fluid and ascites (95.1%), procedural guidance (92.4%), and obstetric ultrasound for confirmation of intrauterine pregnancy (88.6%). Point-of-care ultrasound applications most unfamiliar to current residents are identified as the following: musculoskeletal ultrasound (36.2%), assessment for deep vein thrombosis in lower extremities (29.6%), and renal ultrasound (28.6%).
Figure 1.
Resident perceptions of the usefulness of POCUS applications to family medicine
AAA—abdominal aortic aneurysm, DVT—deep vein thrombosis, FAST—Focused Assessment with Sonography in Trauma, IUP—intrauterine pregnancy, MSK—musculoskeletal, RUQ—right upper quadrant.
Most residents observed staff physicians using ultrasound in the emergency department (79.3%) or in the context of prenatal, labour, and delivery care (50.8%). A minority of residents had observed staff physicians using ultrasound in family medicine clinics to evaluate patients (17.7%) and perform procedures (36.6%). A small proportion of residents (13.2%) reported that they had never observed a family physician using ultrasound.
DISCUSSION
Our survey results demonstrate that most residents express a strong interest in POCUS training and support the use of POCUS in primary care practice. However, a formal POCUS curriculum has not yet been incorporated into most Canadian family medicine residency programs. This reiterates the results of our recent study of family medicine program directors, who also expressed an interest in establishing a POCUS curriculum. Despite this desire for training, currently only 3 family medicine residency programs in Canada offer an established ultrasound curriculum.21
Implementing POCUS training in family medicine residency programs has several potential barriers, including limited access to ultrasound machines and qualified instructors.21 Aside from a mandatory POCUS curriculum in residency programs, our results suggest a POCUS elective or funding to take external POCUS training are potential solutions. However, this can pose a substantial financial burden to residents, as these electives and courses can cost between $1000 and $5000. Most residents (91.6%) believed funding should come from residency programs to take these courses if formal ultrasound training is unavailable. Increasingly, residency training programs are facing budgetary constraints. Developing in-house training programs or local POCUS electives would help mitigate these costs.
Most residents supported the inclusion of POCUS in primary care practice and identified its main benefits as being a useful adjunct to the physical examination and a rapid diagnostic tool, as well as having the potential to reduce health care spending. Most residents would also consider using POCUS regularly in their clinical practice if both the appropriate training and access to an ultrasound machine were provided. These views are similar to those in the previous study of family medicine program directors, who also expressed favourable views of POCUS in primary care.21 Although most evidence supporting POCUS use comes from emergency medicine, the movement toward the inclusion of ultrasound in family medicine is supported by the growing body of literature highlighting that POCUS use in primary care is accurate, is safe, and has numerous applications for family practice.26–34
In conjunction with the results from our previous survey, both residents and program directors believe ultrasound is useful in clinical practice for AAA screening, obstetric indications, and procedural guidance.21 The use of ultrasound for these applications in primary care is well supported by evidence. Research has demonstrated long-term mortality benefits associated with ultrasound screening of asymptomatic patients for AAA. A recent Canadian prospective study showed that office-based scans for AAA screening had a high degree of correlation with hospital-based scans.13 The use of ultrasound in primary care obstetrics is well documented, and the American Academy of Family Physicians endorsed obstetric ultrasound as a core skill for maternity care.35 A plethora of literature supports the use of ultrasound by clinicians to guide a variety of procedures commonly performed in primary care such as drainage of subcutaneous abscesses, joint aspiration, intra-articular injection, confirmation of intrauterine device placement, and paracentesis.15,36–39
Contrary to the results of the survey of program directors, residents also considered the FAST examination and limited echocardiography as useful applications. Although the FAST examination is well established in the context of abdominal trauma to identify free fluid, it can also be used in the primary care clinic to identify ascites.9 Residents might consider it to be a useful POCUS application owing to their familiarity with its use, as it is often the first application taught as an introduction to bedside ultrasound. Evidence supporting the use of limited echocardiography in primary practice is currently lacking. A study from Norway has demonstrated that after undergoing an 8-hour training program, general practitioners were able to assess left ventricular function using pocket-sized ultrasound with a sensitivity and specificity of 78% and 83%, respectively.29 This skill could be useful for family physicians to help determine the cause of patients presenting with dyspnea including heart failure and pleural effusions.
Many primary care physicians work in a variety of practice settings, including in community emergency departments, in palliative care settings, and as hospitalists. This is also reflected in the residents’ responses (Table 1). The use of POCUS is helpful in the many different practice settings in which family physicians work.
Limitations
A limitation of this study was the overall response rate of only 32.3% of Canadian family medicine residents. Previous research on large population survey studies reported an average response rate of 30% to e-mail surveys and our results are comparable.40,41 Similarly, the 2007 National Physician Survey of Canadian physicians and residents achieved an e-mail response rate of 29.9%.42 In a meta-analysis of Web- and Internet-based surveys, Cook et al suggested that response representativeness is more important than response rate.43 Representativeness refers to how well the sample drawn for the questionnaire reflects the greater population attributes. Overall, responses were fairly evenly distributed across rural, urban or community, and academic teaching units, with 29.6%, 38.2%, and 32.2% response rates, respectively. Another limitation to our survey study is the lack of flexibility in response format. In our study of this large population, multiple-choice responses, binary responses, and Likert scales better quantify the predominant opinions of the surveyed population, but in doing so, we lose certain nuances in the opinions expressed. When possible, we allowed for an “other (please specify)” option for individual responses. However, a qualitative study on the views of family medicine residents and physicians would help to further our understanding of the role of POCUS in primary care.
Finally, it is important to note that most of our resident respondents do not have any formal training in POCUS. Only 33.2% agreed or strongly agreed that they were familiar with the literature on POCUS use. This is higher than family medicine program directors and academic leads, of whom only 21% either agreed or strongly agreed.21 Thus, most family medicine residents and program directors are not entirely familiar with the current literature available on POCUS use, and so opinions on POCUS being used to alter clinical decision making or having no negative effect on patient care might not be evidence based. A future goal will be educating both residents and program directors on the emerging evidence for POCUS use in family medicine.
Conclusion
This is the largest survey identifying the perceived need of family medicine residents for POCUS training. There is overwhelming support for and interest in POCUS by family medicine residents across Canada. Despite this, only 18.4% of residents currently receive formal POCUS training through their residency programs. Consistent with our recent family medicine program directors’ survey on POCUS, most believe training should be incorporated into their residency curricula. Most residents believe that POCUS would positively affect primary care and would consider using ultrasound regularly in their clinical practice if they had the proper training.
Editor’s key points
▸ In this study, most residents expressed a strong interest in point-of-care ultrasound (POCUS) training and supported the use of POCUS in primary care practice. However, a formal POCUS curriculum has not yet been incorporated into most Canadian family medicine residency programs; only 18.4% of residents currently receive formal POCUS training through their residency programs.
▸ Most residents supported the inclusion of POCUS in primary care practice and identified its main benefits as being a useful adjunct to the physical examination and a rapid diagnostic tool, as well as having the potential to reduce health care spending.
▸ Potential solutions to the lack of training, aside from a mandatory POCUS curriculum, include a POCUS elective or funding to take external POCUS training. Most residents believed funding should come from residency programs if formal ultrasound training is unavailable.
Points de repère du rédacteur
▸ Dans cette étude, la majorité des résidents ont dit souhaiter fortement suivre une formation en échographie au point de service (FEPS), et étaient en faveur de l’utilisation de l’échographie au point de service dans les cliniques de soins primaires. Par ailleurs, un cursus officiel pour la FEPS n’a pas encore été intégré dans la plupart des programmes de résidence en médecine familiale au Canada; seulement 18,4 % des résidents reçoivent actuellement de la formation formelle en échographie au point de service durant leur résidence.
▸ La majorité des résidents étaient favorables à l’inclusion de l’échographie au point de service dans la pratique des soins primaires, et ont indiqué que ses principaux avantages résidaient dans son utilité comme auxiliaire à l’examen physique et dans sa rapidité en tant qu’outil diagnostique, sans compter les possibilités qu’elle offre de réduire les dépenses en santé.
▸ Comme solutions possibles au manque de formation, exception faite d’un cursus obligatoire en échographie au point de service, les résidents ont mentionné un stage optionnel dans ce domaine ou du financement pour suivre une FEPS à l’extérieur. La plupart des résidents croyaient que le financement devrait être assuré par les programmes de résidence si une formation formelle en échographie n’était pas accessible.
Footnotes
Contributors
The survey was mainly developed and the manuscript was mainly written by Drs Peng, Braganza, and Micks. Drs Sue, Woo, Rogers, Freedman, Lewis, Hu, Varner, Patel, Hameed, and Steinmetz were all instrumental in survey design, pilot testing, and distribution. They also provided substantial contributions to manuscript review and editing. Dr Steinmetz was the overall project lead.
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749–57. doi: 10.1056/NEJMra0909487. [DOI] [PubMed] [Google Scholar]
- 2.Kendall JL, Hoffenberg SR, Smith RS. History of emergency and critical care ultrasound: the evolution of a new imaging paradigm. Crit Care Med. 2007;35(5 Suppl):S126–30. doi: 10.1097/01.CCM.0000260623.38982.83. [DOI] [PubMed] [Google Scholar]
- 3.Ma OJ, Mateer JR, Ogata M, Kefer MP, Wittmann D, Aprahamian C. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38(6):879–85. doi: 10.1097/00005373-199506000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Marhofer P, Chan VW. Ultrasound-guided regional anesthesia: current concepts and future trends. Anesth Analg. 2007;104(5):1265–9. doi: 10.1213/01.ane.0000260614.32794.7b. [DOI] [PubMed] [Google Scholar]
- 5.Howard ZD, Noble VE, Marill KA, Sajed D, Rodrigues M, Bertuzzi B, et al. Bedside ultrasound maximizes patient satisfaction. J Emerg Med. 2014;46(1):46–53. doi: 10.1016/j.jemermed.2013.05.044. Epub 2013 Aug 12. [DOI] [PubMed] [Google Scholar]
- 6.Bagheri-Hariri S, Yekesadat M, Farahmand S, Arbab M, Sedaghat M, Shahlafar N, et al. The impact of using RUSH protocol for diagnosing the type of unknown shock in the emergency department. Emerg Radiol. 2015;22(5):517–20. doi: 10.1007/s10140-015-1311-z. Epub 2015 Mar 21. [DOI] [PubMed] [Google Scholar]
- 7.Mantuani D, Frazee BW, Fahimi J, Nagdev A. Point-of-care multi-organ ultrasound improves diagnostic accuracy in adults presenting to the emergency department with acute dyspnea. West J Emerg Med. 2016;17(1):46–53. doi: 10.5811/westjem.2015.11.28525. Epub 2016 Jan 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lamperti M, Bodenham AR, Pittiruti M, Blaivas M, Augoustides JG, Elbarbary M, et al. International evidence-based recommendations on ultrasound-guided vascular access. Intensive Care Med. 2012;38(7):1105–17. doi: 10.1007/s00134-012-2597-x. Epub 2012 May 22. [DOI] [PubMed] [Google Scholar]
- 9.Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and paracentesis. Chest. 2013;143(2):532–8. doi: 10.1378/chest.12-0447. [DOI] [PubMed] [Google Scholar]
- 10.Nazeer SR, Dewbre H, Miller AH. Ultrasound-assisted paracentesis performed by emergency physicians vs the traditional technique: a prospective, randomized study. Am J Emerg Med. 2005;23(3):363–7. doi: 10.1016/j.ajem.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Nomura JT, Leech SJ, Shenbagamurthi S, Sierzenski PR, O’Connor RE, Bollinger M, et al. A randomized controlled trial of ultrasound-assisted lumbar puncture. J Ultrasound Med. 2007;26(10):1341–8. doi: 10.7863/jum.2007.26.10.1341. [DOI] [PubMed] [Google Scholar]
- 12.Das SK, Choupoo NS, Haldar R, Lahkar A. Transtracheal ultrasound for verification of endotracheal tube placement: a systematic review and meta-analysis. Can J Anaesth. 2015;62(4):413–23. doi: 10.1007/s12630-014-0301-z. Epub 2014 Dec 24. [DOI] [PubMed] [Google Scholar]
- 13.Blois B. Office-based ultrasound screening for abdominal aortic aneurysm. Can Fam Physician. 2012;58:e172–8. Available from: www.cfp.ca/content/cfp/58/3/e172.full.pdf. Accessed 2019 Oct 17. [PMC free article] [PubMed] [Google Scholar]
- 14.Steinmetz P, Oleskevich S. The benefits of doing ultrasound exams in your office. J Fam Pract. 2016;65(8):517–23. [PubMed] [Google Scholar]
- 15.Greenlund LJS, Merry SP, Thacher TD, Ward WJ. Primary care management of skin abscesses guided by ultrasound. Am J Med. 2017;130(5):e191–3. doi: 10.1016/j.amjmed.2016.11.040. Epub 2016 Dec 22. [DOI] [PubMed] [Google Scholar]
- 16.Coris EE, Pescasio M, Zwygart K, Gonzalez E, Farrar T, Bryan S, et al. Office-based ultrasound in sports medicine practice. Clin J Sport Med. 2011;21(1):57–61. doi: 10.1097/JSM.0b013e31820758aa. [DOI] [PubMed] [Google Scholar]
- 17.Wordsworth S, Scott A. Ultrasound scanning by general practitioners: is it worthwhile? J Public Health Med. 2002;24(2):88–94. doi: 10.1093/pubmed/24.2.88. [DOI] [PubMed] [Google Scholar]
- 18.Hall JW, Holman H, Bornemann P, Barreto T, Henderson D, Bennett K, et al. Point of care ultrasound in family medicine residency programs: a CERA study. Fam Med. 2015;47(9):706–11. [PubMed] [Google Scholar]
- 19.American Academy of Family Physicians . Recommended curriculum guidelines for family medicine residents. Point of care ultrasound. AAFP Reprint no. 290D. Leawood, KS: American Academy of Family Physicians; 2016. [Google Scholar]
- 20.Bornemann P. Assessment of a novel point-of-care ultrasound curriculum’s effect on competency measures in family medicine graduate medical education. J Ultrasound Med. 2017;36(6):1205–11. doi: 10.7863/ultra.16.05002. Epub 2017 Feb 16. [DOI] [PubMed] [Google Scholar]
- 21.Micks T, Braganza D, Peng S, McCarthy P, Sue K, Doran P, et al. Canadian national survey of point-of-care ultrasound training in family medicine residency programs. Can Fam Physician. 2018;64:e462–7. Available from: www.cfp.ca/content/cfp/64/10/e462.full.pdf. Accessed 2019 Oct 17. [PMC free article] [PubMed] [Google Scholar]
- 22.Heard JK, O’Sullivan P, Smith CE, Harper RA, Schexnayder SM. An institutional system to monitor and improve the quality of residency education. Acad Med. 2004;79(9):858–64. doi: 10.1097/00001888-200409000-00011. Erratum in: Acad Med 2004;79(11):1055. [DOI] [PubMed] [Google Scholar]
- 23.Roth LM, Severson RK, Probst JC, Monsur JC, Markova T, Kushner SA, et al. Exploring physician and staff perceptions of the learning environment in ambulatory residency clinics. Fam Med. 2006;38(3):177–84. [PubMed] [Google Scholar]
- 24.Sherbino J, Lockyer J. Mind the gap: educational needs assessment. In: Sherbino J, Frank JR, editors. Educational design. A CanMEDS guide for the health professions. Ottawa, ON: Royal College of Physicians and Surgeons of Canada; 2011. pp. 21–8. [Google Scholar]
- 25.Steinmetz P, Dobrescu O, Oleskevich S, Lewis J. Bedside ultrasound education in Canadian medical schools: a national survey. Can Med Educ J. 2016;7(1):e78–86. [PMC free article] [PubMed] [Google Scholar]
- 26.Micks T, Smith A, Parsons M, Locke T, Rogers P. Point-of-care ultrasonography training for rural family medicine residents—its time has arrived. Can J Rural Med. 2016;21(1):28–9. [PubMed] [Google Scholar]
- 27.Micks T, Sue K, Rogers P. Barriers to point-of-care ultrasound use in rural emergency departments. CJEM. 2016;18(6):475–9. doi: 10.1017/cem.2016.337. Epub 2016 Jul 25. [DOI] [PubMed] [Google Scholar]
- 28.Lindgaard K, Riisgaard L. Validation of ultrasound examinations performed by general practitioners. Scand J Prim Health Care. 2017;35(3):256–61. doi: 10.1080/02813432.2017.1358437. Epub 2017 Aug 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mjølstad OC, Snare SR, Folkvord L, Helland F, Grimsmo A, Torp H, et al. Assessment of left ventricular function by GPs using pocket-sized ultrasound. Fam Pract. 2012;29(5):534–40. doi: 10.1093/fampra/cms009. Epub 2012 Feb 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bornemann P, Bornemann G. Military family physician’s perceptions of a pocket point-of-care ultrasound device in clinical practice. Mil Med. 2014;179(12):1474–7. doi: 10.7205/MILMED-D-14-00241. [DOI] [PubMed] [Google Scholar]
- 31.Siu T, Chau H, Myhre D. Bedside ultrasonography performed by family physicians in outpatient medical offices in Whitehorse, Yukon. Can J Rural Med. 2013;18(2):43–6. [PubMed] [Google Scholar]
- 32.Bornemann P, Jayasekera N, Bergman K, Ramos M, Gerhart J. Point-of-care ultrasound: coming soon to primary care? J Fam Pract. 2018;67(2):70–80. [PubMed] [Google Scholar]
- 33.Bornemann P, Barreto T. Point-of-care ultrasonography in family medicine. Am Fam Physician. 2018;98(4):200–2. [PubMed] [Google Scholar]
- 34.Flick D. Bedside ultrasound education in primary care. J Ultrasound Med. 2016;35(7):1369–71. doi: 10.7863/ultra.15.08073. Epub 2016 May 20. [DOI] [PubMed] [Google Scholar]
- 35.American Academy of Family Physicians . Recommended curriculum guidelines for family medicine residents: maternity care. AAFP Reprint no. 261. Leawood, KS: American Academy of Family Physicians; 2018. [Google Scholar]
- 36.Squire BT, Fox JC, Anderson C. ABSCESS: applied bedside sonography for convenient evaluation of superficial soft tissue infections. Acad Emerg Med. 2005;12(7):601–6. doi: 10.1197/j.aem.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 37.Qvistgaard E, Kristoffersen H, Terslev L, Danneskiold-Samsøe B, Torp-Pedersen S, Bliddal H. Guidance by ultrasound of intra-articular injections in the knee and hip joints. Osteoarthritis Cartilage. 2001;9(6):512–7. doi: 10.1053/joca.2001.0433. [DOI] [PubMed] [Google Scholar]
- 38.Raza K, Lee CY, Pilling D, Heaton S, Situnayake RD, Carruthers DM, et al. Ultrasound guidance allows accurate needle placement and aspiration from small joints in patients with early inflammatory arthritis. Rheumatology (Oxford) 2003;42(8):976–9. doi: 10.1093/rheumatology/keg269. Epub 2003 Apr 16. [DOI] [PubMed] [Google Scholar]
- 39.Hayes JL, Cwiak C, Goedken P, Zieman M. A pilot clinical trial of ultrasound-guided postplacental insertion of a levonorgestrel intrauterine device. Contraception. 2007;76(4):292–6. doi: 10.1016/j.contraception.2007.06.003. Epub 2007 Aug 6. [DOI] [PubMed] [Google Scholar]
- 40.Sheehan KB. E-mail survey response rates: a review. J Comput Mediat Commun. 2001;6(2) [Google Scholar]
- 41.James KM, Ziegenfuss JY, Tilburt JC, Harris AM, Beebe TJ. Getting physicians to respond: the impact of incentive type and timing on physician survey response rates. Health Serv Res. 2011;46(1 Pt 1):232–42. doi: 10.1111/j.1475-6773.2010.01181.x. Epub 2010 Sep 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grava-Gubins I, Scott S. Effects of various methodologic strategies. Survey response rates among Canadian physicians and physicians-in-training. Can Fam Physician. 2008;54:1424–30. [PMC free article] [PubMed] [Google Scholar]
- 43.Cook C, Heath F, Thompson RL. A meta-analysis of response rates in Web- or Internet-based surveys. Educ Psychol Meas. 2000;60(6):821–36. [Google Scholar]