Supplemental Digital Content is available in the text.
Background:
Augmentation mastopexy is one of the most difficult challenges plastic surgeons face, especially concerning sustainability of upper pole fullness and lower pole ptosis correction. We describe our technique for augmentation mastopexy that provides inferolateral muscular support for the implant and standardizes a sequence of surgical stages to resolve multiple situations and present the outcomes of patients who underwent such an approach.
Methods:
Our technique proposes the following: (a) modified subpectoral pocket, with muscular inferolateral support for the implant; (b) independent approaches to the submuscular (implant) pocket and parenchymal resection/reshaping; and (c) pre-established 4-step surgical sequence. Data from office files of our private practice were collected for 266 patients who underwent the technique from October 2015 to January 2019. Patient perception about esthetic outcomes, photographs from multiple postoperative follow-ups, and surgical complications/reoperation rates were analyzed.
Results:
Overall mid-term and long-term results (39 months) were positive for lift and augmentation at single time mastopexy; >90% of patients reported satisfaction with their esthetic outcomes, including absence of ptosis. No major complications occurred. The total revision rate was 16%, but it became <5% in 2018 as the learning curve progressed.
Conclusions:
Augmentation mastopexy is complex, and the myriad of approaches and possibilities may cause confusion when selecting the most suitable one. The 4-step sequence provides a reliable option, offering a predefined execution plan, whereas inferolateral muscular support prevents recurrence of lower pole ptosis. Other surgeons’ experience with lift and augmentation at single time mastopexy and further studies are necessary to validate these findings.
BACKGROUND
Augmentation mastopexy is one of the most difficult challenges that plastic surgeons face. A common question asked by patients is “how long will my breast lift last?” We have learned that women are concerned about how long upper pole fullness will last and how long will it take for the lower pole ptosis to recur. These events may happen very soon, especially in women with highly mobile parenchyma and/or saggy skin.
We describe an alternative approach for performing a breast lift combined with silicone implant augmentation: lift and augmentation at single time (LAST). In our experience, it has shown a high rate of patient satisfaction at the mid-term and long-term follow-ups, especially concerning upper pole fullness and absence of lower pole ptosis. Herein, we describe our technique and present the outcomes of patients who underwent such an approach.
METHODS
The study was performed in full conformity with ethical norms and standards in the Declaration of Helsinki. Informed consent statement was obtained from all the 266 patients.
Description of the 4-step LAST Surgical Technique
With the patient in the sitting position, the projected new position of the nipple–areolar complex (NAC) is marked preoperatively. A useful landmark for the new NAC site projection is a measurement of 1/10 of the patient’s height (in centimeters) from the clavicle or parallel to the middle length of the patient’s arm. The marking is transferred to the contralateral breast. These markings mainly serve as a guide for symmetry because the final NAC positions will not always match the preoperative markings.
Step 1: Modified Subpectoral Pocket Creation
With the patient in the supine position, an incision is made through the inframammary fold, and tissue is divided until the fibers of the pectoralis major muscle are found. Cranial and medial electrocautery dissection is performed through the muscle surface, exposing the pectoralis costal and inferior sternal origins (Fig. 1).
Fig. 1.

Exposure of the distal pectoralis muscle. The vertical blue dye indicates the dissection preserving a lateral muscular strip, and the horizontal blue dye indicates the line of pectoralis division medially.
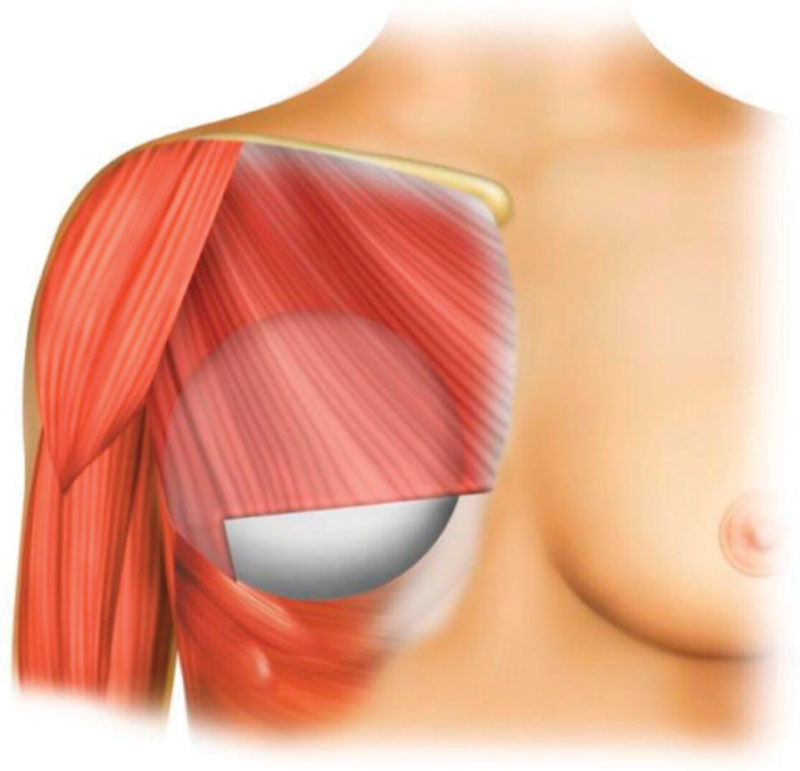
Although most submuscular pocket techniques completely release these costal origins, this technique preserves a 1- to 2-cm width pectoralis lateral border strip, and from that line, the submuscular pocket is dissected. This strip, sometimes in conjunction with some fibers from the anterior serratus muscle, will provide inferolateral support for the implant as a muscular sling (Fig. 2).
Fig. 2.
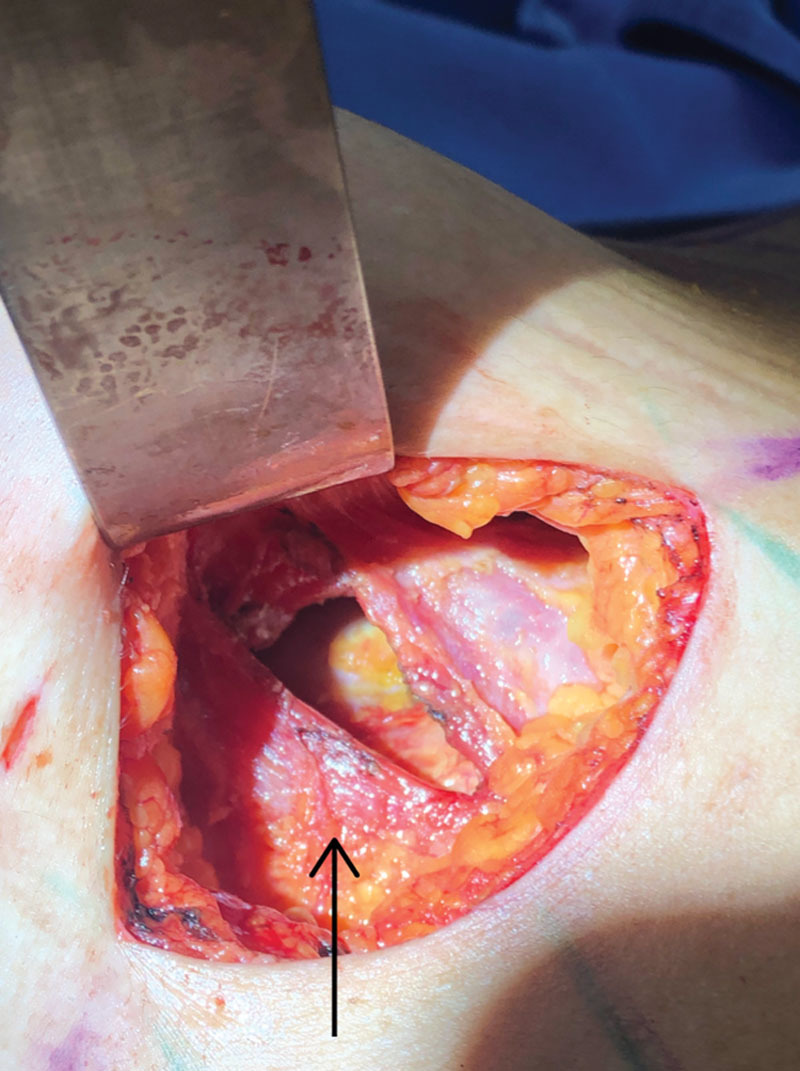
Dissection of the subpectoral pocket. Costal insertions of the lateral muscular strip are kept intact (arrow).
To prevent severe animation deformity related to the total submuscular pockets and to make sufficient room for the inferomedial pole of the implant, the pectoralis inferomedial fibers are divided up to muscle sternal origins, which are never divided.1 The upward muscular retraction results in a triangular-shaped area that lacks the pectoralis layer (Fig. 3). It is necessary to ensure that the subpectoralis pocket is tight enough to avoid undesired implant lateral or cranial displacement.
Fig. 3.
Inferomedial triangular-shaped area created by muscular retraction after division of the inferomedial pectoralis costal origins.
Step 2: Pocket Sealing and Markings for Mastopexy
Then implants are inserted and accommodation inside the pocket is made (Fig. 4). The patient is moved to the sitting position to check upper pole symmetry, and adjustments of the implant position/accommodation inside the pockets are made. At this point, the preoperative NAC markings are altered if necessary. The markings for vertical and horizontal skin and breast tissue resection are determined by manually pinching the skin; these markings can be made conservatively, allowing for minimum tension on the suture lines (Fig. 5).
Fig. 4.
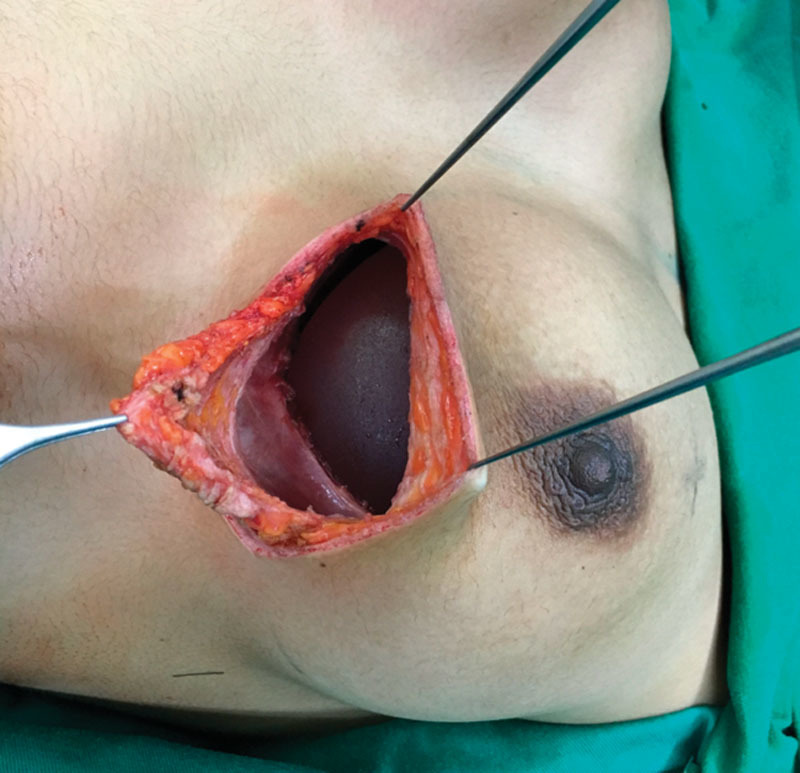
Implant inside of the subpectoral pocket. The preserved lateral muscular sling provides inferolateral support, and the inferomedial pole does not protrude through the triangular-shaped area.
Fig. 5.

Manual pinching is used to mark the vertical and horizontal areas of tissue resection.
The patient is returned to the supine position, and sutures are used to completely seal the implant pocket. The upper breast parenchyma is sutured to the muscular sling laterally and to the caudal edge fascia medially (Fig. 6).
Fig. 6.
The breast parenchyma is sutured laterally to the muscular sling and medially to the fascia at the caudal edge of the incision.
At this point, the implants are symmetrically placed and sealed. Mastopexy will now be performed over these steady bases.
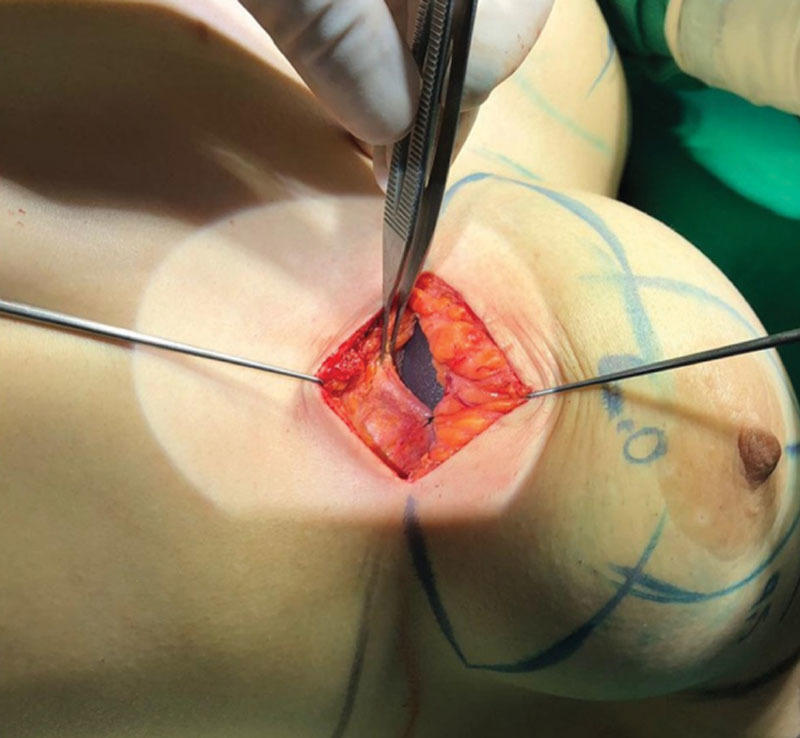
Step 3: Resection and Volume Symmetry
The marked periareolar area is deepithelialized.2 Resection of the parenchyma is performed from the lateral lower pole (where the muscle overlies the implant) to the medial lower pole through a plane slightly superficial to the muscle, thus preserving a thin parenchymal flap over the implant and pectoralis muscle. This flap ensures that the implant remains completely sealed. The implant inferolateral portion will be covered by muscle/parenchymal flap/fascia, and the inferomedial portion will be covered by the thin parenchymal flap and fascia (Fig. 7).
Fig. 7.

Parenchyma resection is performed in a plane slightly superficial to the pectoralis major muscle. The implant is covered laterally and cranially by muscular/parenchyma/fascia layers (M) and inferomedially by parenchyma/fascia layers (F). The implant pocket is previously completely sealed by suture shown on Figure 6.
If the remaining tissue on the retroareolar, lateral, and medial limbs is thicker than 2 cm, additional resection is performed to prevent the snoopy nose deformity3 (Fig. 8).
Fig. 8.

Further parenchyma resection may be necessary so the remaining breast tissue is not >2-cm thick.
With the patient in the sitting position, volume symmetry is assessed. Extra parenchymal resection is performed if necessary.
Step 4: Areolar Lift and Refinements
With the patient still in the sitting position, after both augmentation and tissue resection are completed, final markings of the NAC are determined. It is important to stress that the NAC position at the end of surgery will be very similar to the long-term position, so it should be placed at the center of the breast mound. On average, the final length from the sternal notch to the superior border of the NAC is approximately 16 cm, and the length of the inferior border of the NAC to the inframammary fold is about 6–7 cm. Lifting of the NAC most commonly requires rotation flaps. The superomedial pedicle areolar flap is used in most cases.4–6
At this point, the need for refinements, such as complementary liposuction, fat grafting, and resection of excess medial and lateral skin, is evaluated and performed (Fig. 9). The final sutures are placed in 3 layers: the parenchymal, subdermal, and intradermal layers.
Fig. 9.

The final position of the NAC is marked at the center of the breast mound, and possible areas requiring refinement are marked (eg, liposuction, fat grafting, and excess skin resection).
RESULTS
The LAST technique was performed in 266 augmentation mastopexy procedures from October 2015 to January 2019. The authors always comprised the surgical team, taking turns as surgeon and assistant. All patients were women with age ranging from 19 to 63 years (average age, 36.3 years); of these, 16% of patients (n = 40) underwent massive weight loss before surgery.
In all cases, round silicone implants were used, and identical implants were used in both breasts. The average implant volume was 334.54 mL (range, 220–450 mL). Texturized surface implants accounted for most cases, and nanotexture (Motiva SilkSurface) implants were used in 14.6% of patients (n = 39).
The average weight of resected breast tissue (bilateral) was 323.85 g (range 20g–1,610 g).
Postoperative follow-up ranged from 3 to 39 months. All cases were photographically documented at preoperative and several postoperative stages [See Supplemental Digital Content 1, (http://links.lww.com/PRSGO/B242), which displays a 47-year-old patient after massive weight loss (51 kg) presents with severe skin laxity (left side). Photograph from the 38-month follow-up (Mentor Siltex Round HP 375-mL Implants) (right side)] [See Supplemental Digital Content 2, (http://links.lww.com/PRSGO/B243), which displays a 61-year-old patient after massive weight loss (41 kg) with severe skin laxity (left column). Photograph from the 24-month follow-up (Mentor Siltex Round HP 275-mL Implants) (right column)] [See Supplemental Digital Content 3, (http://links.lww.com/PRSGO/B244), which displays a 32-year-old patient presents with severe skin laxity (left column). Photograph at the 34-month follow-up (Mentor Siltex Round HP 350-mL Implants) (right column)] [See Supplemental Digital Content 4, (http://links.lww.com/PRSGO/B245), which displays a 28-year-old patient after massive weight loss (40 kg) (left column). Photograph from the 24-month follow-up (Lifesil Absolute BDI 350-mL Implants) (right column)] [See Supplemental Digital Content 5, [http://links.lww.com/PRSGO/B246], which displays a 40-year-old patient preoperatively (left column) and at the 10-month (central column) and 36-month (right column) follow-ups (Polytech POLYtxt Meme THS 360-mL Implants)].
All patients were interviewed about their personal satisfaction with the esthetic outcome of their surgery. Overall, 90.2% of patients (n = 240) reported that they were “satisfied,” and 9.8% of patients (n = 26) reported that they were “unsatisfied.”
In this series of 266 cases, no major adverse health events or infection occurred. Two patients presented with unilateral partial areolar epidermolysis with no full-thickness necrosis. Four patients presented with unilateral hematomas that required reoperation.
The total reoperation rate was 16% (n = 43). Most reoperations were performed in the early months of the technique development (eg, a low NAC position, excess medial/lateral skin, and snoopy nose deformity). The reoperation rates for surgery were 33.3% in 2015 and only 4.45% in 2018.
DISCUSSION
Several authors have already proposed the concept of implant support in augmentation mastopexy, with or without the pectoralis muscle.7–11 We do not consider LAST to be a brand-new technique; instead, we consider it to be a combination of previous maneuvers and concepts1,2,4,6–12 in which 2 points stand out: a modification to the creation of the subpectoral pocket (the inferolateral muscular sling) and the straightforward sequence of performing the surgery. On the literature review for writing this article, we found a previous description of the modified subpectoral pocket12 for breast reconstruction using acellular dermal matrix, so this feature is also not new; we have not found, however, any articles correlating the pocket to esthetic procedures or mastopexy.
In such a complex surgery,13–16 it divides the surgeon’s tasks into smaller obstacles that will be solved one at a time in a pre-established sequence. Once the learning curve was achieved, the proposed 4-step surgical sequence enabled us to reproduce the operation in various situations, even in those we considered difficult (eg, severe asymmetry, severe skin laxity, highly mobile parenchyma, and ptotic tuberous breasts).
Once most of the breast weight is held by the supporting lateral muscle, the final tension on the skin sutures is low. We believe that this feature of the technique causes the low incidence of minor wound healing complications (eg, suture extrusions, punctual dehiscence, and epidermolysis).
The breast fascia, ligaments, and attachments17–19 may be stretched or loosen and fail to provide proper implant support; the long-lasting upper pole fullness results from implant stability because its lateral and caudal displacement are limited by the inferolateral muscular sling. This feature was present even with nanosurface implants, and although no smooth surface implants were used in this series, we believe that they would behave in a similar way. The reliable muscle resistance, which holds the weight of the implant, and significant parenchyma resection (few/thin tissue remaining on the lower pole) contribute to minimizing/postponing lower pole ptosis, even with compliant skin envelopes. A total submuscular pocket would also provide implant support, but it keeps the implants too high, do not fit bigger implants (we were able to use up to 450-mL implants) and present important animation deformities. The lateral muscular sling should serve only as a “shelf”—if too tick/wide/strong, may also cause cranial implant displacement and severe animation deformities.
The degree of ptosis had no influence on implant volume selection; it was based on patients result expectation (of course breast footprint and personal anatomic limits are respected). We evaluate how much soft tissue will be resected (everything but a 2-cm thickness flap parenchyma), and patients may choose if they wish the breasts to be bigger, similar, or smaller; respectively, the implant volume should outrange, replace, or be lesser than the volume of parenchyma resected. The average implant volume was 334,54 mL versus average tissue resection weight of 161,9 g per breast (on average about 173,5 g augmentation).
The steady, symmetric bases—the identical implants supported by muscle—favor independent parenchyma manipulation in each breast and allows for management of even severe asymmetric breasts. It is also a reliable solution for tuberous breasts with ptosis.
The implants are minimally manipulated and exposed in the surgical field for a very short time and covered by 2 separated tissue pockets. This offers an additional protection in case any skin healing problems occur; we experienced no case of implant exposure in this series.
Some patients have origins of the inferolateral pectoralis, which will ultimately determine the position of the lower pole of the implant, more cranial than the natural inframammary fold.20–23 The following drawbacks derive from this issue: (1) The whole breast should be proportionally lifted, including longer cranial dislocation of the NAC. We noticed that the breast tissue characteristics rather than the absolute distance of displacement are the most determining feature concerning the risk of ischemia of the NAC (denser/bulkier parenchyma are at higher risk compared with soft/mobile ones). (2) The final breast position on the torso is slightly cranial to what may be considered the anatomical standard. This feature may be seen as a disadvantage; however, the high level of patient satisfaction about this feature questions this viewpoint. Patients seem to value much more upper pole fullness and the absence of lower pole ptosis.24–26 (3) Extended horizontal skin resection is most commonly required, which always leads to T-shaped scars and somewhat longer horizontal scars.
The intact lateral muscular sling does cause some animation on breasts [See Supplemental Digital Content 6, (http://links.lww.com/PRSGO/B247), which displays patient shown on Figure 13 with relaxed (left column) and contracted (right column) pectoralis muscle; mild animation is noticed] [See Supplemental Digital Content 7, (http://links.lww.com/PRSGO/B248), which displays patient shown on Figure 14 with relaxed (left column) and contracted (right column) pectoralis muscle at 45-month follow-up; mild animation is noticed]. However, it is mild and limited to the inferolateral pole; patients did not notice it until we showed on examination and pictures. Even after alerted, animation was not an important issue for most patients.
Additionally, in a few patients, we found the pectoralis costal origins may be located too cranially (fifth rib), so the lateral muscular strip has to be released or the implants would sit too high on the thorax.
Adequate parenchymal resection is of utmost importance for good results; therefore, patients who are young/nulliparous and/or present with dense/bulky breasts are not ideal candidates for LAST mastopexy. If the remaining parenchyma overlying the implants is too thick, the probability of undesired snoopy nose/waterfall effect is significant.
The first year’s high (33%) reoperation percentage (although the absolute number of procedures was only 15, hence, reoperation n = 5) dropped as we progressively learned how to prevent its main causes (medial/lateral dog ears; NAC malposition) down to under 5% in 2018 (procedure n = 90, reoperation n = 4).
CONCLUSIONS
We were able to apply LAST mastopexy in various situations (eg, cases of asymmetry, tuberous ptotic breasts, massive weight loss, and multiparous women); therefore, we consider it to be a versatile option. Because we were able to apply the same 4-step surgical sequence for these multiple situations and obtained similar outcomes, we also consider LAST mastopexy to offer good reproducibility. The longer follow-up period (up to 39 months) showed long-lasting results regarding upper pole fullness and recurrence of lower pole ptosis. The absence of major complications and low reoperation rates (<5% in 2018) suggest that it is a safe approach. Additionally, the patient approval rate was high (>90% of patients reported satisfaction with the esthetic results).
The selection of patients with breast types that favors application of this technique optimizes the risk/benefit tradeoff. In our experience, the breast characteristics that are more suitable for LAST mastopexy are precisely the same that caused us difficulty in achieving good lasting results with former techniques: a saggy/fragile skin envelope and soft/highly mobile parenchyma.27,28 Other surgeons’ experience with LAST mastopexy and further prospective comparative studies are necessary to validate our outcomes.
STATEMENT OF CONFORMITY
This study was conducted in accordance with the Declaration of Helsinki.
Supplementary Material
Footnotes
Published online 27 November 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2001;107:1255–1272. [DOI] [PubMed] [Google Scholar]
- 2.Schwarzmann E. Die Technic der Mammaplastik. Chirurgica. 1930;2:932–943. [Google Scholar]
- 3.Ricci JA, Driscoll DN. Removing the ambiguity from the double bubble. Plast Reconstr Surg. 2015;136:864e–865e. [DOI] [PubMed] [Google Scholar]
- 4.Neto ES. Mastoplastia redutora setorial com pedículo areolar interno. In: Anais do XIII Congresso Brasileiro de Cirurgia Plástica e I Congresso Brasileiro de Cirurgia Estética, Abr 1976; Porto Alegre, RS, Brasil EMMA. [Google Scholar]
- 5.le Roux CM, Pan WR, Matousek SA, et al. Preventing venous congestion of the nipple-areola complex: an anatomical guide to preserving essential venous drainage networks. Plast Reconstr Surg. 2011;127:1073–1079. [DOI] [PubMed] [Google Scholar]
- 6.Skoog T. A technique of breast reduction; transposition of the nipple on a cutaneous vascular pedicle. Acta Chir Scand. 1963;126:436–365. [PubMed] [Google Scholar]
- 7.Mansur JR, Bozola AR. Mastopexia e aumento das mamas com proteção e suporte inferior da prótese com retalho de pedículo inferior. Rev Bras Cir Plást. 2009;24:304–309. [Google Scholar]
- 8.Daher JC, Di Lamartini J, do Amaral G, et al. Mastopexy associated with submuscular or subglandular silicone implants: indications and complications. Rev Bras Cir Plást. 2012;27:294–300. [Google Scholar]
- 9.Soares AB, Franco FF, Rosim ET, et al. Mastopexy with breast implants and the pectoralis major muscle flap: a technique adopted by the department of plastic surgery of unicamp. Rev Bras Cir Plást. 2011;26:659–663. [Google Scholar]
- 10.Daniel MJB. Inclusion of the breast prosthesis in double space. Rev Bras Cir Plást. 2005;20:82–87. [Google Scholar]
- 11.Spear SL, Sinkin JC, Al-Attar A. Porcine acellular dermal matrix (strattice) in primary and revision cosmetic breast surgery. Plast Reconstr Surg. 2013;131:1140–1148. [DOI] [PubMed] [Google Scholar]
- 12.Kolker AR, Piccolo PP. Extended submuscular implant-based breast reconstruction with pectoralis-serratus sling and acellular dermal matrix. Aesthet Surg J. 2017;37:485–491. [DOI] [PubMed] [Google Scholar]
- 13.Calobrace MB, Herdt DR, Cothron KJ. Simultaneous augmentation/mastopexy: a retrospective 5-year review of 332 consecutive cases. Plast Reconstr Surg. 2013;131:145–156. [DOI] [PubMed] [Google Scholar]
- 14.Beale EW, Ramanadham S, Harrison B, et al. Achieving predictability in augmentation mastopexy. Plast Reconstr Surg. 2014;133:284e–292e. [DOI] [PubMed] [Google Scholar]
- 15.Spear SL, Boehmler JH, Clemens MW. Augmentation/mastopexy: a 3-year review of a single surgeon’s practice. Plast Reconstr Surg. 2006;1187 suppl136S–147S; discussion 148S-149S, 150S-151S. [DOI] [PubMed] [Google Scholar]
- 16.Spear SL. Augmentation/mastopexy: “surgeon, beware.” Plast Reconstr Surg. 2006;118:133S–134S. [DOI] [PubMed] [Google Scholar]
- 17.Matousek SA, Corlett RJ, Ashton MW. Understanding the fascial supporting network of the breast: key ligamentous structures in breast augmentation and a proposed system of nomenclature. Plast Reconstr Surg. 2014;133:273–281. [DOI] [PubMed] [Google Scholar]
- 18.Maclin MM, II, Deigni OA, Bengtson BP. The laminated nature of the pectoralis major muscle and the redefinition of the inframammary fold: clinical implications in aesthetic and reconstructive breast surgery. Clin Plast Surg. 2015;42:465–479. [DOI] [PubMed] [Google Scholar]
- 19.Rehnke RD, Groening RM, Van Buskirk ER, et al. Anatomy of the superficial fascia system of the breast: a comprehensive theory of breast fascial anatomy. Plast Reconstr Surg. 2018;142:1135–1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baek WY, Byun IH, Seok Kim Y, et al. Variance of the pectoralis major in relation to the inframammary fold and the pectoralis minor and its application to breast surgery. Clin Anat. 2017;30:357–361. [DOI] [PubMed] [Google Scholar]
- 21.Sanchez ER, Sanchez R, Moliver C. Anatomic relationship of the pectoralis major and minor muscles: a cadaveric study. Aesthet Surg J. 2014;34:258–263. [DOI] [PubMed] [Google Scholar]
- 22.Madsen RJ, Jr, Chim J, Ang B, et al. Variance in the origin of the pectoralis major muscle: implications for implant-based breast reconstruction. Ann Plast Surg. 2015;74:111–113. [DOI] [PubMed] [Google Scholar]
- 23.Gil YC, Lee KW, Chang DY, et al. Positional relationship between the pectoralis major and external abdominal oblique muscles for consideration during dual-plane breast augmentation. Clin Anat. 2018;31:339–346. [DOI] [PubMed] [Google Scholar]
- 24.Mallucci P, Branford OA. Population analysis of the perfect breast: a morphometric analysis. Plast Reconstr Surg. 2014;134:436–447. [DOI] [PubMed] [Google Scholar]
- 25.Swanson E. Ideal breast shape: women prefer convexity and upper pole fullness. Plast Reconstr Surg. 2015;135:641e–643e. [DOI] [PubMed] [Google Scholar]
- 26.Hammond DC, O’Connor EA. The lower island flap transposition (LIFT) technique for control of the upper pole in circumvertical mastopexy. Plast Reconstr Surg. 2014;134:655–660. [DOI] [PubMed] [Google Scholar]
- 27.Coombs DM, Srivastava U, Amar D, et al. The challenges of augmentation mastopexy in the massive weight loss patient: technical considerations. Plast Reconstr Surg. 2017;139:1090–1099. [DOI] [PubMed] [Google Scholar]
- 28.Losken A. Breast reshaping following massive weight loss: principles and techniques. Plast Reconstr Surg. 2010;126:1075–1085. [DOI] [PubMed] [Google Scholar]


