Supplemental Digital Content is available in the text.
Background:
Women report difficulty understanding and personalizing breast reconstruction information during the complex and time-limited period of cancer treatment planning. Patient decision aids can help patients become well informed, form realistic expectations, prepare to communicate with the surgical team, and be more satisfied with their decision-making process.
Methods:
We engaged patients, providers, and stakeholders in a user-centered design process to develop an online patient decision aid video and interactive workbook for breast reconstruction after mastectomy. The video and workbook introduce breast reconstruction and compare the risks and benefits of 3 key decisions: reconstruction versus no reconstruction, immediate versus delayed, and tissue- versus implant based. Pilot testing using cognitive interviews and pre-/postdecision aid questionnaires assessed acceptability, knowledge, and decision-making values.
Results:
After viewing the decision aid, patients (n = 20) scored 97.5% correct on a knowledge test; however, the factors driving their decisions were varied. All (n = 40) patients and providers/stakeholders provided over 80% positive acceptability ratings. 97.5% said they would recommend the video and workbook to other women with breast cancer.
Conclusions:
The Considering Breast Reconstruction after Mastectomy patient decision aid video and workbook show potential for improving informed decision-making. Delivery before the initial plastic surgery consultation was well supported as a way to give women time to process the information and prepare to talk with the surgical team about their options. The Personal Decision Worksheet shows potential for assessing patients’ knowledge and the factors driving their personal decision-making process.
INTRODUCTION
Each year, over 120,000 women in the United States are diagnosed with breast cancer and undergo mastectomy.1 Many of these women are candidates for more than 1 type of breast reconstruction, and the “best” decision often depends on personal preferences regarding the timing of reconstruction, use of autologous tissue versus implants, potential out-of-pocket costs, and short- versus long-term outcomes.2 In previous studies, patients reported multiple challenges to engaging in these complex, personal decisions, including difficulty understanding the terminology, personalizing the information, and weighing risk/benefit trade-offs during the stressful time between diagnosis and mastectomy.3,4 Providers report the need for addressing misinformation, improving patients’ realistic expectations, and having tools that can be delivered alongside the consultation to reinforce comprehension without impacting the clinical care flow.4
Over 105 randomized trials show that patient decision aids improve patients’ knowledge, realistic expectations, clarity about what matters most to them, preparation for making well-informed decisions, and satisfaction with the decision.5 Patient decision aids are evidence-based tools that provide up-to-date, balanced information about the options and structured support to improve deliberation and communication.5,6 They may be provided before, during, or after a consultation as brochures, videos, or websites.5,7 The goal of patient decision aids is to improve decision quality—the degree to which decisions are well informed and congruent with patients’ highest rated decision-making values.5 They also seek to reduce patients’ decisional conflict, ie, anxiety due to feeling uninformed, unclear, unsupported, or unsure.8 Studies show that for every unit increase in decisional conflict, patients are 3 times more likely to fail a knowledge test, 59 times more likely to change their minds, 5 times more likely to express regret, and 19% more likely to blame doctors for bad outcomes.8
Recent legislation has begun to provide reimbursement for shared decision-making consultations; however, relatively few patient decision aids have been successfully implemented in clinical care. Therefore, the International Patient Decision Aid Standards collaboration and the National Quality Forum are establishing guidelines for the systematic development and certification of patient decision aids.9,10 These guidelines emphasize rigorous development of high-quality, unbiased tools that are meaningful and understandable by diverse patients, as well as ready for rapid, scalable, and sustainable dissemination.7,11,12 They also recommend publishing formative work so that providers, patients, and policymakers can assess the quality of the patient decision aid. The purpose of this paper is therefore 2-fold: (1) to illustrate a systematic, user-centered process that clinical researchers can use to develop patient decision aids that align with the international guidelines and (2) to provide the results of the development and pilot testing of a patient decision aid video and interactive workbook entitled, Considering Breast Reconstruction after Mastectomy: A Video and Workbook for Women with Breast Cancer©. We hypothesized that engaging patients, providers, and other stakeholders in the codevelopment of a tool to address their identified decision-making needs would result in a tool that was understandable and acceptable.
MATERIALS AND METHODS
This study involved 3 phases: (1) formative development with a stakeholder team; (2) iterative cognitive interviews with female breast cancer survivors to produce and refine a prototype; and (3) pilot testing the acceptability of the video and workbook. The underlying theories of the Ottawa Decision Support Framework and a modified user-centered design approach guided the study.13,14 The University of Texas MD Anderson Cancer Center Institutional Review Board provided ethical review and approval for this study. All participants provided informed consent.
Formative Development and Codesign with Stakeholders
Figure 1 illustrates the design process, which was selected based on the international guidelines to ensure rigorous content development, support usable design, and maximize the likelihood feasible implementation. We purposefully engaged a stakeholder advisory panel of 3 female breast cancer survivors, 8 plastic surgeons, 6 breast surgeons, 2 radiation oncologists, a clinical ethicist, and a patient education specialist to guide development. Building on previous decision-making needs assessment studies,3,5 the team worked with the advisory panel to identify priority decision-making needs and map the clinical care and decision-making pathways from the perspectives of patients, clinicians, and stakeholders. The research team reviewed the most recent Cochrane Collaboration systematic review of patient decision aids and conducted an environmental scan to identify and evaluate any previously developed patient decision aids.
Fig. 1.
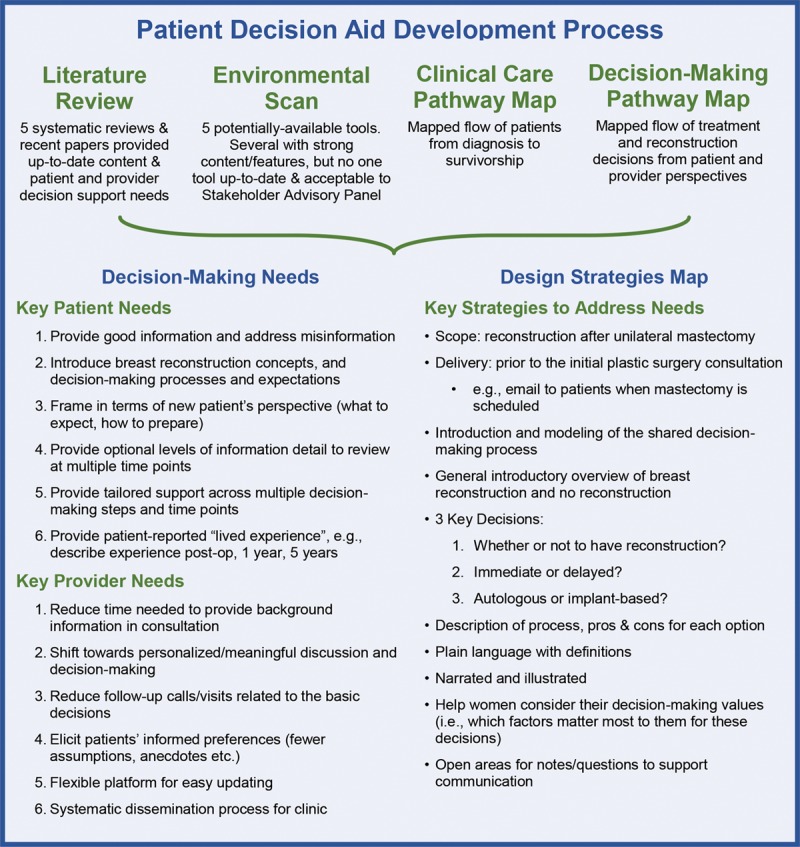
Formative development process and outcomes that guided patient decision aid content, structure, and features.
Partnering with a team of graphic designers, the research team created a map of proposed design strategies to meet each need, a script, and initial storyboards (paper drafts of the content and medical illustrations). Clinical content was based on recent systematic reviews. The research team iteratively reviewed and revised the storyboards with the stakeholder advisory group, then approved them for “storyboarding”—quick cycles of test–revise–test with providers and survivors.
A trained facilitator (A.S.H.) presented the storyboards at 4 clinical research meetings and elicited feedback on clinical content, decision support content, graphics, and delivery within the care flow. The facilitator repeated the process with female cancer survivors using the think-aloud approach15—survivors narrated what they were thinking as they viewed each page and directly edited the draft. Based on feedback from the first cycle of storyboarding, the team created a paper workbook summarizing the video and providing a personal decision-making worksheet similar to the Ottawa Personal Decision Guide and Decision Quality Indices.16,17 Three more internal storyboarding cycles yielded saturation of feedback, then a final cycle of external providers and patient advisors reviewed the storyboards.
After final revisions, the design team produced the video with a professional voice artist. The video was iteratively reviewed and revised 4 times, then approved for pilot testing.
Pilot Test for Acceptability
The primary purpose of the pilot test was to confirm acceptability with providers and established patients before launching an efficacy study with newly diagnosed patients and to inform future implementation. Exploratory analyses also assessed patients’ knowledge and decision-making values.
Participants included breast cancer providers and English-speaking, adult women who were 6 months to 3 years post mastectomy—whether or not they underwent reconstruction—recruited from the MD Anderson Center for Reconstructive Surgery. The interviewer invited patients to review the video and workbook while discussing their impressions, then asked patients open-ended questions about the strengths of the materials and opportunities for improvement. Patients completed a questionnaire containing 15 demographic characteristics items, 25 items adapted from the Ottawa Acceptability Scale,19 3 open-ended questions about their recommendations for optimal delivery, and the Personal Decision Worksheet. Because these were established patients who had already made reconstruction decisions, only 2 components of the Personal Decision Worksheet were explored. The Knowledge subscale included 10 True/False items. The Decision-Making Values subscale included 10 Leaning Scales20 that assessed how important each factor was in their decision from 0 (not important) to 10 (very important).
In parallel, the team e-mailed the video, workbook, and questionnaire (without the Personal Decision Worksheet questions) to a diverse group of providers and stakeholders. The interviewer also presented the video and workbook at 3 departmental meetings and invited open feedback.
Data Analysis
SPSS Statistics 24 (2016 IBM Corporation, Armonk, New York, https://www.ibm.com/products/spss-statistics) was used to tabulate responses to the acceptability items. The a priori criterion for acceptability was that 80% of women would rate the video and workbook favorably (ie, strongly agree/agree, balanced/just right).12 Exploratory analyses included calculating mean correct responses on the 10 True/False knowledge items, and medians and box plots of the 10 Decision-Making Values items. The research team reviewed interview notes and responses to open-ended questions for themes that might improve the design or delivery.
RESULTS
Formative Development
The primary results of the formative interviews (Fig. 1) were that the patient decision aid should provide a high-level introduction to the overall process of breast reconstruction, then focus on preparing women to discuss 3 key decisions: (1) Should I have breast reconstruction?, (2) Should I start immediately or delay?, and (3) Should I use a flap of my own tissue or an implant? In addition, the tool would need to be able to be delivered before the plastic surgery consultation, at home (eg, by e-mail when a mastectomy is scheduled) or in the clinic waiting room, so as not to delay clinic flow.
The most recent Cochrane Collaboration systematic review included 1 paper and 1 abstract about breast reconstruction decision aids; however, the environmental scan identified 5 existing patient decision aids. The advisory panel noted that they had many strengths (eg strong presentation of risks and benefits, patient-friendly language, supportive graphics), but some contained outdated information, were not applicable to current practice, and/or were not rated favorably by patient advisors. The panel unanimously agreed that a new patient decision aid was needed.
The team decided to focus on reconstruction after unilateral mastectomy for the initial video. Modules for other types of reconstruction (eg, segmental, contralateral prophylactic) will be created later. Survivors emphasized that the video should be narrated and illustrated to avoid “gory” images. The goals of the video and workbook would be to (1) provide an introductory overview of breast reconstruction and no reconstruction; (2) explain key medical terminology; and (3) prepare women to have an informed conversation with their surgical team about their preferences among medically appropriate options.
Iterative Storyboarding and Production
Twelve plastic surgeons, 3 breast surgeons, 2 patient education specialists, and 5 female breast cancer survivors reviewed the storyboards. Suggestions for improvement focused on addressing common misconceptions and providing “hindsight” about areas that survivors felt were relevant downstream (eg, axillary management, lymphedema). Reviewers suggested breaking up the video into modules that could be rereviewed after the consultation and easily updated in the future.
Production resulted in a 24-minute video and a 20-page workbook (see figure, Supplemental Digital Content 1, which displays selected images from the video and workbook, http://links.lww.com/PRSGO/B241). The video includes 5 modules, 60 custom graphics, and 26 custom medical illustrations. The workbook summarizes the clinical content and provides side-by-side comparison charts for each decision, a Myths and FAQs (frequently asked questions) page, Tips from Survivors and Nurses, a glossary, and the Personal Decision Worksheet. The worksheet contains the 10 True/False knowledge items, 10 Decision-making Values Scales, an item where women can circle the options they are interested in discussing, and places for writing notes and questions to discuss with their plastic surgeon.
Pilot Testing
Acceptability
Table 1 summarizes the participant characteristics. Patients, providers, and stakeholders rated the video and workbook as acceptable (ie, greater than 80% favorable responses) (Table 2). Both groups (patients, providers/stakeholders) reported that the video focused more on reconstruction than no reconstruction; however, comments noted that this was appropriate given the need to explain the reconstructive terminology and that the module on whether or not to have reconstruction presented both options clearly. Providers/stakeholders were concerned about the video upsetting women; however, patients emphasized that any distress would be minimal compared with their fears about diagnosis and treatment. Notably, 19 of 20 patients and all 20 providers/stakeholders said they would recommend the video and workbook to other women.
Table 1.
Pilot Test Participant Characteristics
| n, % | n, % | ||
|---|---|---|---|
| Race | Had breast reconstruction | 15, 75.0% | |
| Black or African American | 2, 10.0% | Type: | |
| White | 14, 70.0% | One breast | 2, 10.0% |
| Other | 2, 10.0% | Both breasts | 16, 80.0% |
| Hispanic | 6, 30.0% | Immediate | 5, 25.0% |
| Highest education | Delayed | 8, 40.0% | |
| High school graduate (or equivalent) | 1, 5.0% | Tissue | 5, 25.0% |
| Associate’s degree | 1, 5.0% | Implant | 12, 60.0% |
| Bachelor’s degree | 8, 40.0% | Nipple reconstruction | 3, 15.0% |
| Master’s degree | 5, 25.0% | 3D nipple tattoo | 4, 20.0% |
| Stage: | |||
| Professional school degree | 1, 5.0% | Completed the initial surgery | 5, 35.7% |
| Doctoral degree | 1, 5.0% | Have had 1 revision surgery | 3, 21.4% |
| High literacy† | 14, 82.4% | Have had 2 or more revision surgeries | 4, 28.6%* |
| Relationship status | 3, 15.0% | Have had nipple reconstruction or 3D tattoo | 1, 7.1% |
| Single | 13, 65.0% | Finished with my reconstruction | 4, 28.6% |
| Married | 1, 5.0% | Had a complication | 8, 57.1% |
| Divorced | Other (eg, paused/stopped) | 3, 21.4% | |
| Religion | Did not have reconstruction | 5, 25.0% | |
| Christianity | 16, 80.0% | Wear a breast prosthesis | 1, 20.0% |
| Other | 2, 10.0% | Silicone | 1, 20.0% |
| Providers and Stakeholders (n = 20) | Had a complication | 1, 20.0% | |
| Female | 14, 70.0% | Type of insurance | |
| Race | Private | 16, 80.0% | |
| American Indian or Alaskan Native | 1, 5.0% | Medicare or Medicaid | 4, 20.0% |
| Asian, including Indian | 7, 35.0% | Specialty | |
| Black or African American | 3, 15.0% | Plastic surgeons | 7, 35.0% |
| Native Hawaiian or Pacific Islander | 0, 0.0% | Other surgeon/provider | 1, 5.0% |
| White | 13, 65.0% | Decision scientist | 3, 15.0% |
| Other | 0, 0.0% | Behavioral scientist | 3, 15.0% |
| Hispanic | 1, 5.0% | Graphic designer or informatician | 6, 30.0% |
| Months since mastectomy, mean (min, max) | 25.1 (6, 36) | Researcher | 18, 90.0% |
| Health education specialist | 4, 20.0% | ||
| Other | 1, 5.0% | ||
| Master’s degree or greater | 17, 85.0% |
*Three patient participants did not respond to the literacy item (n = 17).
†High literacy = score of 0 on the Single Item Literacy Scale.
3D, three-dimensional; max, maximum; min, minimum.
Table 2.
Acceptability Ratings*
| Items | Patients (n = 20) | Providers and Stakeholders (n = 20) |
|---|---|---|
| The video and workbook are/present… | ||
| Clear | 20, 100.0% | 20, 100.0% |
| Easy to understand | 20, 100.0% | 20, 100.0% |
| Useful | 20, 100.0% | 20, 100.0% |
| Easy to use | 20, 100.0% | 19, 95.0% |
| Visually attractive | 18, 90.0% | 17, 85.0% |
| Interesting | 18, 90.0% | 19, 95.0% |
| The right length | 16, 80.0% | 17, 85.0% |
| The right amount of information | 14, 70.0% | 17, 85.0% |
| The pros and cons in a balanced way | 16, 80.0% | 18, 90.0% |
| Decision 1: Reconstruction or no reconstruction | 16, 80.0% | 15, 75.0% |
| Decision 2: Immediate or delayed | 20, 100.0% | 18, 90.0% |
| Decision 3: Tissue or implant | 20, 100.0% | 18, 90.0% |
| The video and workbook will help women… | ||
| Who are considering breast reconstruction | 20, 100.0% | 19, 95.0% |
| Feel empowered to make a decision | 19, 95.0% | 19, 95.0% |
| Feel ready to talk to their doctor | 19, 95.0% | 15, 75.0% |
| The video and workbook will make women… | ||
| Feel upset | 1, 5.0% | 2, 10.0% |
| Feel nervous | 0, 0.0% | 4, 20.0% |
| Overall… | ||
| Would you have found this video and workbook helpful when making decision(s) about breast reconstruction? | 20, 100.0% | 20, 100.0% |
| Do you think the video and workbook provide enough information to prepare a woman to talk with her doctor(s) about breast reconstruction? | 14, 70.0% | 20, 100.0% |
| Would you recommend this video and workbook to women thinking about breast reconstruction? | 19, 95.0% | 20, 100.0% |
*Number who responded “yes” or “agree/strongly agree.”
Delivery
Overall, responses favored e-mailing access to the video and workbook to women before their plastic surgery consultation so that they could process the information (Table 3). Both patients and providers/stakeholders also recommended providing access after the consultation for rereview and ensuring it was viewable on multiple devices. Several women commented that they would view it on their cell phones while waiting for other appointments and that they preferred to have the website address sent to a personal e-mail rather than through the patient portal. Providers wanted the worksheet saved to their electronic medical record.
Table 3.
Recommendations for Implementing in Clinical Care
| Patients (n = 20) | Providers and Stakeholders (n = 20) | |
|---|---|---|
| When do you think is the best time to offer this video and workbook to women? | ||
| As soon as possible after her diagnosis | 8, 40.0% | 10, 50.0% |
| When reviewing her treatment plan with her breast surgeon | 10, 50.0% | 15, 75.0% |
| Before meeting with her plastic (reconstructive) surgeon | 11, 55.0% | 17, 85.0% |
| After meeting with her plastic (reconstructive) surgeon | 10, 20.0% | 11, 55.0% |
| Offered/available throughout the process | 11, 55.0% | 10, 50.0% |
| Other | 1, 5.0% | 3, 15.0% |
| What do you think is the best way to offer this video and workbook to women? | ||
| At the doctor’s office | 14, 70.0% | 9, 45.0% |
| On the hospital website | 14, 70.0% | 18, 90.0% |
| E-mail the link to women through the patient portal | 12, 60.0% | 20, 100.0% |
| Other | 10, 20.0% | 4, 20.0% |
| Where do you think women will want to view this video and workbook? | ||
| On the computers at the hospital (eg, in the waiting room) | 3, 15.0% | 9, 45.0% |
| On a computer at a library or community center | 1, 5.0% | 4, 20.0% |
| On their home computer or laptop | 17, 85.0% | 18, 90.0% |
| On their tablet (eg, iPad, Nook, Kindle) | 17, 85.0% | 18, 90.0% |
| On their cell phone | 8, 4.0% | 12, 60.0% |
| Other | 2, 10.0% | 2, 10.0% |
Exploring Knowledge and Decision-Making Values
Patients scored an average of 97.5% correct responses on the 10 knowledge items (minimum 90%, maximum 100%). Responses varied on the top 10 factors driving women’s decisions (Fig. 2). Two women commented that items regarding “other health concerns” and “time away from work/home duties” were irrelevant to them; however, the advisory panel recommended keeping those items to inform the consultation.
Fig. 2.
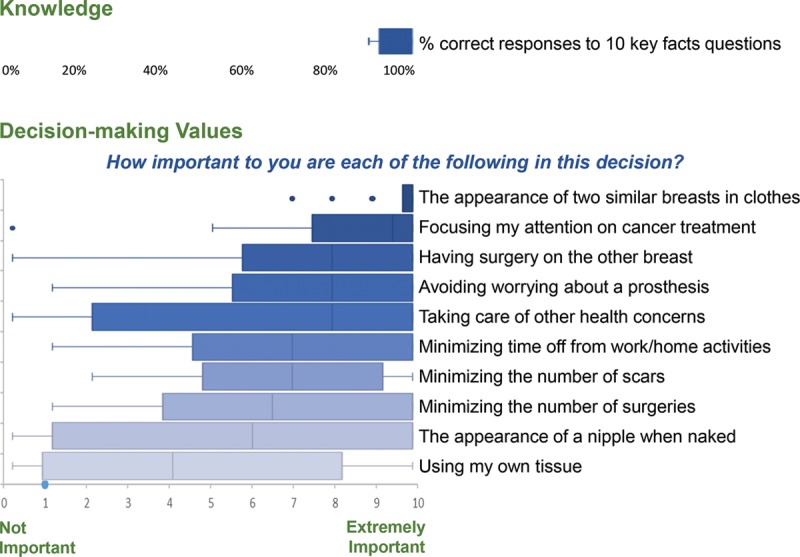
Responses to the Personal Decision Worksheet (n = 20 patients).
Clinical Content
Patient interviews (Table 4) focused on the need to understand the overall reconstruction process and timeline, then weigh which details were meaningful. Patients commented on the importance of presenting pros and cons side by side for each decision, and using consistent, repetitive, plain language to reinforce comprehension. Several women suggested adding examples of postoperative experiences, stating that it would have been more easily manageable if they had more time to prepare mentally.
Table 4.
Selected Quotes from Pilot Test Interviews
|
Acceptability • Really glad you all are doing this and think it is really important. • This video and workbook would have been so helpful to me before my surgery, in particular the pictures and illustrations. |
|
Delivery • Would be good to have it offered as soon as mastectomy and also have the scheduler, PA [physician's assistant], doctor ask you to read it before the pre-op visit. The communication/personal invitation matters, since you have to prioritize which of the bags of booklets you’re going to be able to read. |
|
Knowledge and decision-making values • Tell women to ask what their exercise restrictions will be for each option, at each step in the process. If activity is important to you for stress management, this is very important. • Some women might think all these things are very important. Instead of picking a number, you could have women just circle their Top 3 so they can focus on those. |
|
Clinical content • It will be really good for women to have this video and workbook. There was so much information coming at you that it was near impossible to remember it all, even from the best [consultations]. • Really liked the clear explanations, comparisons between options, use of laymen’s terms, not “medical speak”. • I liked that you frequently reminded the viewer that there is no increase in recurrence. • Add more about what to expect post-op when you wake up. This is very, very important. • Explain the reconstructed breast does not have the same responses as a natural breast. • Mention that using a tissue expander may mean you are not able to sleep on your stomach. • Add Tips from Survivors!! (Don’t make every woman reinvent the wheel.) • The type of scarring that will likely occur as a result of the surgical procedures was shown throughout the video. This is important because women will likely have more realistic expectations of their experiences. |
|
Decision-making content and support • The What Matters Most? questions are really important to clarify for yourself. You’re weighing so many things – you need to be able to rule some out and focus on what is important. • I like that these [side-by-side charts] compare [the options] on the things that matter to patients, so I don’t have to spend energy trying to process and reorganize information in a way that matters to me. • I decided quickly because […] but, I had several people really pressuring me. I really wish I had something to be able to show them on paper why the trade-offs in what was important to me made my decision the obvious choice. • Normalize the process. Introduce the idea that there are several decisions to make, and it’s normal to have multiple pros/cons that you’re trading off in your head. The fear of the unknown is worse than confronting a difficult reality. I can handle difficult. • Acknowledge what is not a decision (this is cancer; you will have months of appointments, treatments, recovery, limitations; you will look different; the insurance determines the costs…) |
|
Design • The procedure depictions were appropriate (realistic but not too gory). • Add real photos to the workbook so women who want them can get them when they’re ready to look, but keep this introduction video “gentle”. • The video was very tastefully presented. • The video font, music, voice-over, and color scheme are calming. • Cadence was slow enough for all patient backgrounds. |
Providers and stakeholders also provided positive feedback on the clinical content, focusing on how it would support comprehension and realistic expectations. Suggestions for improvement focused on creating additional modules for breast conserving therapy, axillary management, etc., and versions in other languages.
Decision-Making Support
All but 1 patient voiced the importance of setting the stage about the decision-making process. Several emphasized the value of an interactive worksheet for organizing their thoughts and personalizing the clinical information. The majority of women commented on how valuable it could be to share the Personal Decision Worksheet with the surgical team or family members.
Suggestions for improvement centered on providing more information about how to manage all the breast cancer decisions. Several women commented on the value of affirming the inherent uncertainty, to reduce time spent worrying about “what if’s.”
Design
Women focused on the importance of illustrations to “gently” introduce the surgical procedures, compared with graphic images on the Internet. Providers recommended adding more medical illustrations with higher body mass index. Both groups recommended adding an optional gallery of photos showing the reconstruction and revision process.
Final Video and Workbook Version
The research and design teams addressed the suggested improvements and approved version 1.0. The video and workbook met 8 of 8 International Patient Decision Aid Standards guidelines21 for high-quality development and 11 of 11 criteria for balanced, up-to-date content.
DISCUSSION
To address women’s information and decision-making needs, the Considering Breast Reconstruction after Mastectomy video and workbook provide an overview of breast reconstruction and no reconstruction; set the stage for shared decision-making; and walk women through the pros and cons of 3 key decisions: (1) whether or not to have reconstruction, (2) immediate or delayed, and (3) tissue- or implant based. The workbook summarizes the video and provides more detailed decision-making support (eg, side-by-side comparison charts, Myths and FAQs, a glossary, and a Personal Decision Worksheet). Pilot testing confirms that the video and workbook are acceptable and can be delivered by e-mail before the initial plastic surgery consultation. Preliminary data suggest the video and workbook improve women’s knowledge and clarity about which decision-making factors matter most to them personally. Providers and patients provided strong support for the video and workbook being helpful and usable and said that they would recommend it to new patients.
These findings align with the literature showing that high-quality patient decision aids improve patients’ knowledge, decisional conflict, ability to form realistic expectations, clarity about what matters most, and preparation for discussing decisions with their providers.5 Additional recent studies of breast reconstruction patient education materials and patient decision aids also show overall improvement in knowledge, decisional conflict, and anxiety.2,22–27 A few studies have shown greater patient satisfaction when receiving breast reconstruction information digitally.22 Larger studies are needed to explore the effects of the video and workbook on consultation length, decision quality, and cost-effectiveness.
Notably, providers were concerned about the video being too long, whereas patients wanted the video to provide more information and describe patients’ lived experiences. As a result, we maintained the length of the video but added more detail to the workbook, including “Tips from Survivors and Nurses.” Both groups emphasized the value of providing the video by e-mail and on the hospital website so that women could learn the terminology in advance for a more meaningful discussion.
Results of this study also emphasize the importance of a general introduction, so that the plastic surgery team could focus on providing the appropriate medical recommendations tailored to each woman’s clinical characteristics. Women specifically commented on the value of having 1 printed source of trusted information to address their worries about unknowns and on the structured guidance of the Personal Decision Worksheet for organizing their thoughts before the consultation. Both groups noted the value of “ruling out” less relevant concerns and misconceptions.
Some potential implications may be considered with caution, as this was a developmental study. Overall, patient and provider feedback reiterated that challenges remain in providing timely and understandable information during the complex period of treatment planning, even at a comprehensive cancer center. Delivering this information before the consultation by e-mail or on the hospital website appears to be acceptable and desirable, but care is needed to ensure it provides enough introduction to inform women, while making it clear that the plastic surgeon will provide the personalized medical recommendations.
Helping women become more well-informed and addressing common misconceptions should address the concepts underlying decisional conflict—feeling uninformed, uncertain, unsupported, or unclear—resulting in more informed and engaged patients. Although decision aids are not designed to improve surgical outcomes, studies are ongoing to assess the link between improved comprehension and engagement with behaviors that support clinical outcomes (eg, adherence to recovery plans, physical therapy, etc.). Studies show that some decision aids reduce consultation time, whereas others have little effect on time but deepen the conversation and/or reduce the number of follow-up calls/visits. Ultimately, the gold standard for the effectiveness of a patient decision aid is Decision Quality, a decision that is well informed, congruent with what matters most to the patient, and actionable.
Providing the video and workbook before the consultation also has implications for optimizing care delivery. Several patients, providers, and stakeholders proposed making the Personal Decision Worksheet a routine, patient-reported “Patient Preferences Lab Report.”12,28 Doing so could help tailor the consultation discussion to address gaps in information comprehension, unrealistic expectations, and mismatches between what patients say is important to them and which treatment(s) they are leaning towards. Documenting delivery of a high-quality patient decision may also support reimbursement models for shared decision-making.9,29
Limitations
Despite purposeful sampling and additional recruitment efforts, this study had difficulty enrolling patients who identified as Black or Asian. The patient participants were also well educated and insured. Research is needed to identify whether variations in interest are warranted (ie, based on well-informed, values-congruent preferences) or indicate a disparity.7,28,30,31 Notably, the majority of participants had reconstruction and several reported having had minor complications; however, feedback was positive and many women discussed the benefits of the video and workbook for all women, whether or not they preferred reconstruction. The video and workbook were developed at a comprehensive cancer center; however, they purposefully focus on the most commonly available options and emphasize that patients speak with their provider and insurance company about which options are available and appropriate. Larger randomized trials are needed to establish effectiveness, validate a decision quality measure, and evaluate the impact of systematic implementation.
CONCLUSIONS
The Considering Breast Reconstruction after Mastectomy patient decision aid video and workbook are acceptable and appear to help women become informed and prepared to discuss reconstruction options with their plastic surgery team. The video and workbook may be e-mailed to help women prepare for their plastic surgery consultation. Improving knowledge and clarity about which decision-making factors are most important to each woman may improve patient centeredness of care.
ACKNOWLEDGEMENTS
The authors would like to thank the women, providers, and other stakeholders who shared their experiences and provided valuable insight to guide the design of the Considering Breast Reconstruction after Mastectomy patient decision aid video and workbook. We also appreciate the support of our colleagues at The University of Texas MD Anderson Cancer Center: David Leos, MS, Department of Plastic Surgery; Colleen Gallagher, PhD, MA, LSW, Integrated Ethics; Dawn Chalaire, Scientific Publications; and the clinical and administrative staff of the Department of Plastic Surgery.
Supplementary Material
Footnotes
Published online 20 November 2019.
This work was supported by a grant from The University of Texas MD Anderson Cancer Center Duncan Family Institute for Cancer Prevention and Risk Assessment. The statements presented in this work are solely the responsibility of the authors and do not necessarily represent the views of The University of Texas MD Anderson Cancer Center or the Duncan Family Institute for Cancer Prevention and Risk Assessment.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Society AC. Breast Cancer Facts & Figures 2017-2018. 2017Atlanta: American Cancer Society, Inc. [Google Scholar]
- 2.Sun CS, Cantor SB, Reece GP, et al. Helping patients make choices about breast reconstruction: a decision analysis approach. Plast Reconstr Surg. 2014;134:597–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sun CS, Cantor SB, Reece GP, et al. Assessing women’s preferences and preference modeling for breast reconstruction decision-making. Plast Reconstr Surg Glob Open. 2014;2:e125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fingeret MC, Nipomnick SW, Crosby MA, et al. Developing a theoretical framework to illustrate associations among patient satisfaction, body image and quality of life for women undergoing breast reconstruction. Cancer Treat Rev. 2013;39:673–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stacey D, Kryworuchko J, Belkora J, et al. Coaching and guidance with patient decision aids: a review of theoretical and empirical evidence. BMC Med Inform Decis Mak. 2013;13suppl 2S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoffman AS, Volk RJ, Saarimaki A, et al. Delivering patient decision aids on the internet: definitions, theories, current evidence, and emerging research areas. BMC Med Inform Decis Mak. 2013;13suppl 2S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O’Connor A. User Manual - Decisional Conflict Scale. 1993. Ottawa, Canada: Ottawa Hospital Research Institute; [revised 2010]. [Google Scholar]
- 9.National Quality Forum. National Standards for the Certification of Patient Decision Aids. 2016Washington DC: National Quality Forum. [Google Scholar]
- 10.Joseph-Williams N, Newcombe R, Politi M, et al. Toward minimum standards for certifying patient decision aids: a modified Delphi consensus process. Med Decis Making. 2014;34:699–710. [DOI] [PubMed] [Google Scholar]
- 11.Witteman HO, Dansokho SC, Colquhoun H, et al. User-centered design and the development of patient decision aids: protocol for a systematic review. Syst Rev. 2015;4:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoffman AS, Llewellyn-Thomas HA, Tosteson AN, et al. Launching a virtual decision lab: development and field-testing of a web-based patient decision support research platform. BMC Med Inform Decis Mak. 2014;14:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Connor AM, Tugwell P, Wells GA, et al. A decision aid for women considering hormone therapy after menopause: decision support framework and evaluation. Patient Educ Couns. 1998;33:267–279. [DOI] [PubMed] [Google Scholar]
- 14.Gustafson DH, Jr, Maus A, Judkins J, et al. Using the NIATx model to implement user-centered design of technology for older adults. JMIR Hum Factors. 2016;3:e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karat J. Helander MG, Landauer TK, Prabhu PV. Chapter 28 - User-Centered Software Evaluation Methodologies. In: Handbook of Human-Computer Interaction (Second Edition). 1997Amsterdam: North-Holland; 689–704. [Google Scholar]
- 16.O’Connor AM, Jacobsen MJ. Ottawa Personal Decision Guide. 2015Ottawa, Canada: Ottawa Hospital Research Institute. [Google Scholar]
- 17.Sepucha KR, Belkora JK, Chang Y, et al. Measuring decision quality: psychometric evaluation of a new instrument for breast cancer surgery. BMC Med Inform Decis Mak. 2012;12:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nielsen J, Clemmensen T, Yssing C. Getting access to what goes on in people’s heads?: reflections on the think-aloud technique. Proceedings of the second Nordic conference on Human-computer interaction; 2002; Aarhus, Denmark. [Google Scholar]
- 19.O’Connor AM, Cranney A. User Manual - Acceptability. 1996. Ottawa, Canada: Ottawa Hospital Research Institute; [Updated 2002]. [Google Scholar]
- 20.O’Connor AM. User Manual - Values Scale. 2004Ottawa, Canada: Ottawa Hospital Research Institute. [Google Scholar]
- 21.Elwyn G, O’Connor AM, Bennett C, et al. Assessing the quality of decision support technologies using the international patient decision aid standards instrument (IPDASI). Plos One. 2009;4:e4705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heller L, Parker PA, Youssef A, et al. Interactive digital education aid in breast reconstruction. Plast Reconstr Surg. 2008;122:717–724. [DOI] [PubMed] [Google Scholar]
- 23.Luan A, Hui KJ, Remington AC, et al. Effects of A novel decision aid for breast reconstruction: A randomized prospective trial. Ann Plast Surg. 2016;76Suppl 3S249–S254. [DOI] [PubMed] [Google Scholar]
- 24.Hui KJ, Liu XX, Luan A, et al. Design and focus test of a preconsultation decision aid for breast cancer reconstruction patients: A quality improvement initiative. Eplasty. 2015;15:e24. [PMC free article] [PubMed] [Google Scholar]
- 25.Manne SL, Topham N, D’Agostino TA, et al. Acceptability and pilot efficacy trial of a web-based breast reconstruction decision support aid for women considering mastectomy. Psychooncology. 2016;25:1424–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Causarano N, Platt J, Baxter NN, et al. Pre-consultation educational group intervention to improve shared decision-making for postmastectomy breast reconstruction: a pilot randomized controlled trial. Support Care Cancer. 2015;23:1365–1375. [DOI] [PubMed] [Google Scholar]
- 27.Sherman KA, Shaw LK, Winch CJ, et al. ; BRECONDA Collaborative Research Group. Reducing decisional conflict and enhancing satisfaction with information among women considering breast reconstruction following mastectomy: results from the BRECONDA randomized controlled trial. Plast Reconstr Surg. 2016;138:592e–602e. [DOI] [PubMed] [Google Scholar]
- 28.Hoffman AS. Teaching Diverse Orthopaedic Patient Populations about Deliberative Decision Making Skills: Testing a Design Strategy for Online Patients’ Decision Aids. 2011Dartmouth College. [Google Scholar]
- 29.Oshima Lee E, Emanuel EJ. Shared decision making to improve care and reduce costs. N Engl J Med. 2013;368:6–8. [DOI] [PubMed] [Google Scholar]
- 30.Dugas M, Trottier MÈ, Chipenda Dansokho S, et al. Involving members of vulnerable populations in the development of patient decision aids: a mixed methods sequential explanatory study. BMC Med Inform Decis Mak. 2017;17:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sampson UKA, Kaplan RM, Cooper RS, et al. Reducing health inequities in the U.S.: recommendations from the NHLBI’S health inequities think tank meeting. J Am Coll Cardiol. 2016;68:517–524. [DOI] [PMC free article] [PubMed] [Google Scholar]


