Supplemental Digital Content is available in the text.
Background:
Although the number of plastic surgery residency positions increased over the past decade, interest among Canadian medical students experienced the opposite trajectory. The aim of this study was to assess the effect of a low intensity, basic surgical skills workshop on medical students’ confidence and interest in surgery in general, and plastic surgery in particular.
Methods:
Before and after participating in a 60-minute suturing workshop, preclinical medical students completed a cloud-based questionnaire that evaluated the changes in their suturing confidence and interest in pursuing a career in different surgical subspecialties.
Results:
Eighty-five medical students (52 females and 33 males), with an average age of 22.9 ± 3.6 years participated in this study. Before the workshop, 95% of participants perceived their suturing ability to be at a beginner’s level and reported that they have not received sufficient suturing training during their medical education to date. Their self-reported confidence in suturing was 1.9 ± 2.1 out of 10. Following the workshop, participants’ confidence in their surgical skills increased by 165% (P < 0.001, partial eta2 = 0.695). Moreover, 82% reported increased interest in a career in surgery associated with their participation in the workshop. Plastic surgery, general surgery, and otolaryngology were the top 3 specialties that experienced an augmented increase in interest following the workshop. Finally, plastic surgery was the specialty perceived as requiring the most surgical skills by the majority of the students.
Conclusion:
A 60-minute basic skills suturing workshop significantly improved preclinical medical students’ confidence in their surgical skills, and increased their interest in surgery.
INTRODUCTION
Historically, medical trainees were surgically trained using Halsted’s principles of training, which emphasize learning through direct exposure to surgical procedures, followed by hands-on practice on real patients.1 Although this apprenticeship model of surgical training has been successful for centuries, recent changes in medical education, coupled with patient safety concerns left medical students with less opportunity to practice their surgical skills.2 Furthermore, although the implementation of competency-based education throughout surgical residency programs has many well-cited merits,3–6 it is forecasted to increase workload on attending surgeons for residents’ assessment and evaluation, potentially leading to less direct supervision and surgical training of medical students.7
Surgery as a career has been declining in popularity among medical students in the last several years.8,9 Plastic surgery, in particular, witnessed a significant decrease in interest among Canadian medical students. A recent study showed that although the number of Canadian plastic surgery residency positions nearly doubled, first choice applicants decreased by over 15% within 6 years.10 Another study confirmed that over the past decade, although American plastic surgery residency programs have experienced no significant change in competitiveness, Canadian programs have observed fewer applicants per available positions.11 Previous studies have identified that the lack of plastic surgery education in the undergraduate medical curriculum, along with the suboptimal technical skills training in preclerkship years are major contributors to the decreased interest in plastic surgery.10 This is demonstrated by a recent qualitative study that showed that the lack of basic surgical skills training in medical school leads to low confidence levels in the operating room and a general reduction in interest in surgery.9 Although the aforementioned reasons are likely not the sole culprit for this decline, they are easily addressable across Canadian medical schools.
To that end, the purpose of the present study was to shed light on the role of peer-led, hands-on surgical skills workshops on altering junior medical students’ confidence in their surgical skills and increasing their interest in pursuing a career in a surgical specialty with the hope of encouraging more undergraduate medical programs to implement such peer-led workshops in their curriculums.
MATERIALS AND METHODS
Participants
This prospective single-arm interventional study targeted preclinical undergraduate medical students. The McGill University research ethics review committee (A05-B29-19A) approved the study. Sixty-minute surgical skills workshops were organized and offered to first and second year medical students—as the aim of these workshops were to improve preclinical students’ skills and prepare them for their surgical rotation.
Given the limited objective evidence regarding the effect of suturing workshops on the comfort and self-perceived confidence in performing different suturing techniques, the sample size was determined by assuming a medium effect size of 0.5, alpha of 0.05, and power of 0.8. The sample size required for the study was estimated to be 35. With an assumption of a 50% response rate, we decided to recruit at least 70 participants for the study.
Protocol
Each workshop consisted of 14–15 medical students and was taught by one surgical resident with the assistance of 2 senior medical students, ensuring a minimum of 5-to-1 trainee-to-instructor ratio for maximum supervision. The participants were introduced to and provided with all the necessary surgical instruments (needle driver, forceps, suture scissors, and scalpel blades), as well as surgical suture threads, surgical gloves and a pig leg. The first 10 minutes of each session consisted of the surgical resident highlighting the appropriate handling techniques and illustrating 2 basic suturing techniques: simple interrupted and simple running. The second part of the session consisted of a 50-minute practical session, where the students were encouraged to practice the techniques on the pig leg using the surgical instruments provided. Acknowledging the heterogeneity in learning abilities and the manual dexterity of the participants, those who were interested, after achieving an adequate level of competency were individually taught additional techniques, such as horizontal and vertical mattresses, as well as a subcuticular technique.
Questionnaire, Data Collection, and Consent
Participants were asked to complete 2 online questionnaires, a 25-item and a 31-item, before and one-week after the workshop, respectively (see appendix, Supplemental Digital Content 1, which displays the questionnaires used in this study, http://links.lww.com/PRSGO/B259). The questionnaires primarily aimed to quantitatively evaluate the change in participants’ self-reported suturing competency and confidence, for which 0-10 likert scales were used. Furthermore, students were asked to rank their top 3 residency choices out of a list containing 18 surgical and nonsurgical options. Participants were asked to select the top 3 reasons they found a career in surgery appealing from a set of predefined answers. To maximize the anonymity, no identifying information was collected. Each participant was provided with a unique identifier to match his or her presession and postsession questionnaires. To ensure accuracy of the answers, participants were made aware that their answers would remain anonymous and would not affect their training or future evaluations. Participants who refused to complete the questionnaire continued the sessions without any repercussions. The survey was conducted using Sogosurvey.com—a secure cloud-based platform that was only accessible to the lead authors of the study. All procedures followed were in accordance with the Helsinki Declaration of 1975, as revised in 2008.12 Informed consent was obtained from all participants included in the study.
Statistical Analyses
The Shapiro–Wilk test verified that the data respected the parameters for normality. The primary outcomes included the effect of a low-intensity suturing workshop on self-perceived ability in performing different suturing techniques and change in self-perceived confidence in doing so. Preworkshop to postworkshop changes were assessed using repeated measures analysis of variance (ANOVA) for continuous variables,13 the McNemar test for dichotomous variables,14 and the Wilcoxon test for ordinal variables.15 The secondary outcomes aimed to investigate the effect of the workshop on the interest in pursuing a career in a surgical specialty. All of the statistical analyses were performed using SPSS statistical program version 25.0 (IBM, New York, NY), with significance level set at P <0.05.
RESULTS
Ninety-three preclinical medical students were recruited and attended the workshops, 85 of whom completed both presession and postsession questionnaires (91% response rate). The population consisted of 52 females (61%) and 33 males (39%), with an average age of 22.9 ± 3.6 years. All participants were preclinical medical students, with 49 (58%) and 36 (42%) in the first- and second-year of their medical studies, respectively (Table 1).
Table 1.
Participants’ Baseline Characteristics and Demographics (n = 85)
| Age | 22.86 ± 3.55 |
| Sex | |
| Male | 33 (38.8%) |
| Female | 52 (61.2%) |
| Study year | |
| First year | 49 (57.6%) |
| Second year | 36 (42.4%) |
| Marital status | |
| Single | 62 (72.9%) |
| In a relationship | 23 (27.1%) |
| Highest academic degree attained | |
| Premedical college diploma | 45 (52.9%) |
| Undergraduate degree | 21 (24.7%) |
| Postgraduate degree | 19 (22.4%) |
| Suturing experience | |
| Beginner | 81 (95.3%) |
| Intermediate | 4 (4.7%) |
The continuous and discrete data are presented as mean ± SD and frequency (percentage), respectively.
Before the workshop, 95% of participants reported their suturing ability as beginner level, 78% were unable to perform any type of suturing, and 95% believed that they had not received adequate suturing training during their medical studies. At baseline, the average number of suturing techniques that the participants reported to be competent at was 0.33 ± 0.70, and the self-reported confidence in suturing and scrubbing-in the operating room, out of 10, were 1.86 ± 2.12 and 3.18 ± 2.95, respectively. In terms of interest in pursuing a surgical specialty, only 30 (35%) reported an interest in pursuing a career in surgery, whereas about half of the participants (48%) were undecided.
A significant effect of a low-intensity suturing workshop on improved self-perceived ability to perform different suturing techniques and confidence was evident on primary analysis with a large effect size. Postsession, participants on average reported to be comfortable performing 2 additional suturing techniques, as the mode number of suturing techniques increased from 0 to 2 (P < 0.001, partial eta2 = 0.685) (Fig. 1). Proportion of students comfortable with performing the simple interrupted technique increased from 22% at baseline to 95% following the workshop (P < 0.001), simple running from 8% to 56% (P < 0.001), horizontal mattress from 2% to 22% (P < 0.001), vertical mattress from 1% to 19% (P < 0.001), and subcuticular from 4% to 7% (P > 0.05) (Fig. 2). Moreover, self-perceived confidence in suturing increased by 165% (P < 0.001, partial eta2 = 0.695) (Fig. 3), and confidence to scrub-in the operating room evidenced a similar trend (P < 0.001, partial eta2 = 0.695) with a strong positive association between the 2 (r = 0.577, P < 0.001). Furthermore, 82% of the participants reported that the suturing session positively affected their decision-making in favor of pursuing a career in surgery (P < 0.001). The increase in surgical interest was found to be more significant among first year students, in comparison to second year students (P = 0.008). None of the other demographic factors such as age, sex, or highest level of education had a significant effect on interest (P > 0.05). Furthermore, the increased interest was more profound in the following surgical specialties: plastic surgery, general surgery, and otolaryngology. Moreover, all the participants believed that plastic surgery was among the top 3 surgical specialties that required the highest technical skills. Finally, all of the participants felt that they were more confident and better prepared for their clinical surgical rotations.
Fig. 1.
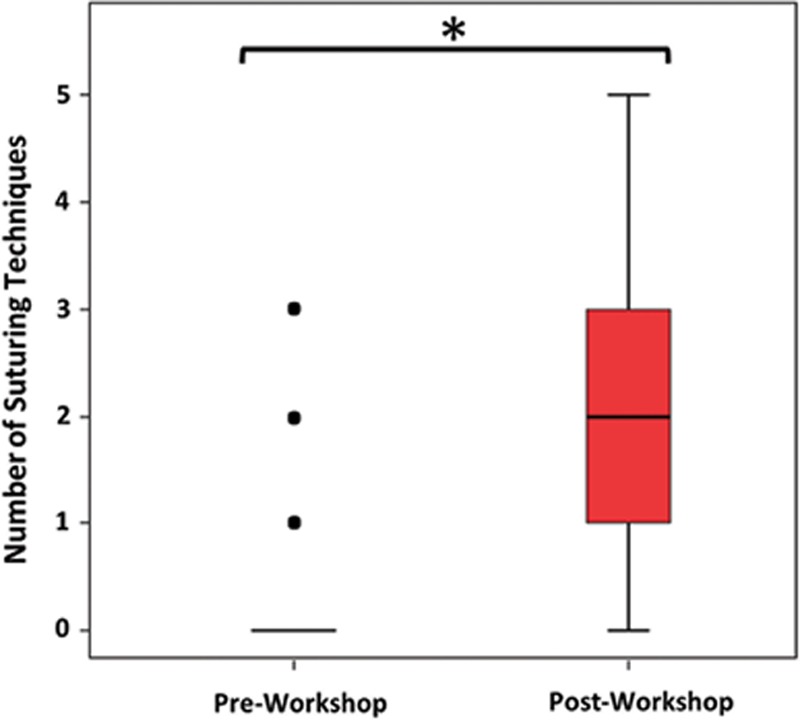
Distribution in number of different suturing techniques participants reported competency in, before and after attending the workshop. The box plot represents the first quartile, median and third quartile of the total suturing techniques participants reported competency in, the whiskers demonstrate the minimum and maximum values, and the dots represent outliers. *Statistical significance at P ≤ 0.001.
Fig. 2.
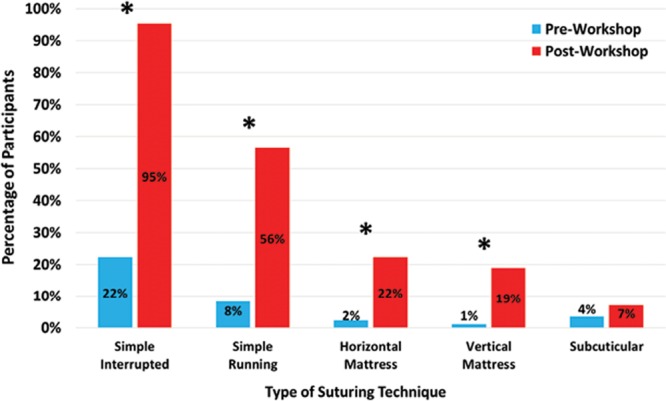
Percentage of participants that are comfortable performing different suturing techniques before and after attending the workshop. *A significant difference at P < 0.001.
Fig. 3.
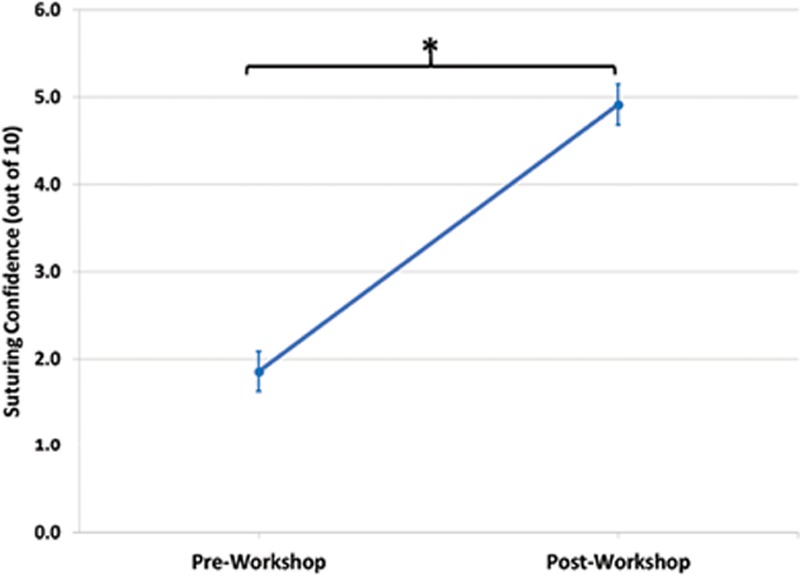
Changes in self-reported suturing confidence before and after attending the workshop. The dot represents the average value and the bars show the standard error of the mean. There was a significant increase in suturing confidence from pre- to post-workshop (P < 0.001, partial eta2 = 0. 695). *Statistical significance at P ≤ 0.001.
The questionnaire also identified that the top 3 reasons for which preclinical medical students found a career in a surgical specialty appealing were its intellectual nature, the manual involvement, and the problem-solving aspect of the work. On the other hand, the long working hours, its competitive nature, and long postgraduate training course were the top three unappealing factors. The instructor-to-student ratio of 1 to 5—one surgical resident and 2 junior clerks for a group of 15 participants—was found to be adequate by all students. All participants were pleased with the quality of the workshops, found the sessions useful, perceived the practice atmosphere as relaxed, and all but 1 rated the teaching quality as good or extremely good. Finally, all students expressed their willingness to participate in future sessions, and 82% of participants believed that ongoing low-intensity suturing workshops should be incorporated early on in the undergraduate medical curriculums.
DISCUSSION
The present study demonstrates that a low-intensity peer-led basic surgical skills workshop was capable of improving junior medical students’ surgical skills acquisition, increase their confidence, and develop their interest in pursuing a career in surgery. The study population was diverse in age, sex, and academic background, representing a typical undergraduate medical cohort. Plastic surgery, which was perceived to require a high level of technical skills, was among the top 3 specialties that experienced an augmented interest amongst students following the workshop. The results showed that the vast majority of junior medical students had no previous suturing skills, and on average felt they had not received adequate surgical training during their medical studies to date. Moreover, all the participants were interested in attending another workshop.
Plastic surgery education in North America is currently undergoing a drastic change from the traditional time-based format to competency-based residency curriculums. Although many studies have explored simulators and other alternative options for surgical skills training for residents, almost none have attempted to address surgical skills training of medical students. Due to the predicted decrease in operating time available for medical students as competency-based curriculums become the mainstay of surgical education, early exposure to basic surgical skills (such as suturing) training will allow medical students to optimize the learning they receive during the limited intraoperative time they get exposed to.
In an era when medical education aims to achieve consistency, and curriculums aspire to provide equal education opportunities to all students, there still lacks standardized surgical skills training in undergraduate medical education.16 The operating room, which can be very intimidating to students, can hinder learning and further decrease interest in surgery.17 Students often have very different experiences in their surgical rotations based on their level of confidence in their surgical skills and how well they navigate the operating room.18 Furthermore, the literature shows that most students develop an interest in surgery before clerkship.19 Therefore, it is important to provide junior medical students with standardized early surgical skills training to develop their confidence in an effort to counteract the often-intimidating environment of the operating room and allow them to gain an interest in surgery.
In the majority of North American medical schools, students are only formally exposed to surgery during their third year for a total of 6–12 weeks.20 Furthermore, most curriculums do not standardly expose them to plastic surgery, which results in the well-documented highly skewed perception of what the field offers.10,21 In fact, a recent study showed that out of all the surgical subspecialties, students feel they receive the least amount of exposure to plastic surgery.10 Moreover, as was seen in our study and in the previous literature, medical students perceive plastic surgery as the subspecialty that requires the most technical skills.21 Given the broad scope of plastic surgery, coupled with the lack of exposure to the field, and the suboptimal surgical skills training in preclinical years,22,23 many students never develop an interest in the field or feel too intimidated to pursue it.20
To address these issues, the current study assessed students’ confidence as a primary outcome. Surgical skills, like all other skills, require regular consistent practice to achieve competence.24,25 Therefore, the main goal of this single 60-minute surgical skills workshop was to improve students’ confidence in their surgical skills, rather than objectively measure increased surgical competency. Confidence has been shown to directly correlate with competence in different domains26; therefore, the authors believe that improving confidence among medical students at an early stage of their education allows them to further explore all career options, and protects them from being deterred from their passion simply because a false sense of insecurity or lack of self-confidence. The authors believe that plastic surgery was among the specialties that experienced the most increase in interest following the suturing session due the fact that students perceive it as a specialty that requires a high level of technical skills. By increasing medical students’ confidence in their own surgical skills, it is possible that they became less intimidated by the specialty and therefore developed an increased interest in it.
Although both first- and second-year medical students became more interested in a career in surgery after the suturing session, the former were more likely to become increasingly interested. This may be due to the fact that first-year medical students are likely less concerned with career-planning at the beginning of their medical education and are more open-minded regarding specialization. Second-year medical students may be further ahead in their career-planning and may perceive it too late to pursue a competitive residency program.
Although plastic surgery remains one of the most competitive surgical specialties, a recent study showed a decline in number of applicants to the Canadian plastic surgery programs over the last 20 years.11 In part, it is thought to be due to the Canadian residency selection process and the applicants’ perception of the significant preparation and qualifications required to successfully match in plastic surgery. Although academic excellence is emphasized in the Canadian match, additional factors such as research productivity and extracurricular activities play a significant role in the selection process. All of these factors reward applicants that have gained interest and commenced their application process as early as possible, and potentially dissuade applicants who became interested in plastic surgery later in their medical training.
It is of significant importance that the primary opportunity to learn and practice surgical skills is in a less intimidating environment than an operating room. The training sessions indeed aimed to provide a relaxing, noncompetitive environment, as to counteract the ORs stereotypical stressful atmosphere. Furthermore, the training of preliminary skills should consist of deliberate practice, which is defined as systematic, focused and goal oriented practice aimed at improving skills.27 Deliberate practice has been shown to improve surgical skills in several domains,28 and therefore, was integrated in the structure of the training sessions. The workshops aimed to provide short and clear instructions, with several demonstrations at the beginning and ample time for practice with instructor guidance.
The current study includes certain limitations, one of which is that it was conducted in a single institution. Although the vast majority of undergraduate medical education curriculums lack standardized basic surgical skills training, there may be minor interinstitutional differences that were not accounted for. Furthermore, despite the majority of the participating students being undecided regarding their interest in a surgical specialty, it can be assumed that their interest in participating in a suturing skills workshop translates to a greater than average interest in surgery. The authors attempted to minimize the selection bias by recruiting participants through universal platforms that targeted all junior medical students, regardless of their career interest. Furthermore, it was made clear that the workshops were open to all students, regardless of their level of expertise or interest in surgery. As one would expect, there were therefore some minor differences in the initial level of suturing ability of the participants. Although all students received teaching and practiced the basic techniques, only those that were more comfortable with their skills received individual instruction on how to perform the more advanced techniques, such as running subcuticular. The latter likely explains the wide variability between confidence in suturing techniques post-session, where 95% of the participants were confident in performing the simple interrupted technique, while only 7% were confident with the subcuticular suture.
A final limitation of this study is the lack of long-term follow-up. Although the authors attempted to bypass the short-lived excitement that follows learning a new skill by asking participants to fill in the postsession questionnaire a week later, there was no long-term follow-up. To comply with the ethics requirements and to ensure anonymity of the participants, the authors did not record any identifying information which could have ultimately allowed us to follow the participants in the long run and study their residency choices. Future studies should investigate whether the increased confidence and interest in surgery following basic surgical skills sessions is maintained at longer follow-ups, and whether they improve performance during clerkship rotations and increase the number of applicants to surgery.
CONCLUSIONS
This study demonstrated that a 60-minute basic surgical skills workshop significantly improved preclinical medical students’ confidence, as well as increased their interest in pursuing a career in surgery, specifically perceived highly technical fields such as plastic surgery and otolaryngology. Due to the surgical education reforms and the implementation of competency-based training, undergraduate medical education curriculums across North America could benefit from implementing similar structured training sessions early in the medical curriculum.
Supplementary Material
Footnotes
Published online 27 November 2019.
Institutional review board of ethics approved this study.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Polavarapu HV, Kulaylat AN, Sun S, et al. 100 years of surgical education: the past, present, and future. Bull Am Coll Surg. 2013;98:22. [PubMed] [Google Scholar]
- 2.Kim FJ, da Silva RD, Gustafson D, et al. Current issues in patient safety in surgery: a review. Patient Saf Surg. 2015;9:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen VT, Losee JE. Time- versus competency-based residency training. Plast Reconstr Surg. 2016;138:527–531. [DOI] [PubMed] [Google Scholar]
- 4.Bhatti NI, Cummings CW. Competency in surgical residency training: defining and raising the bar. Acad Med. 2007;82:569–573. [DOI] [PubMed] [Google Scholar]
- 5.Ten Cate O. Competency-based postgraduate medical education: past, present and future. GMS J Med Educ. 2017;34:Doc69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knox AD, Gilardino MS, Kasten SJ, et al. Competency-based medical education for plastic surgery: where do we begin? Plast Reconstruct Surg. 2014;133:702e–710e. [DOI] [PubMed] [Google Scholar]
- 7.Holmboe ES, Sherbino J, Long DM, et al. The role of assessment in competency-based medical education. Med Teach. 2010;32:676–682. [DOI] [PubMed] [Google Scholar]
- 8.Scott IM, Matejcek AN, Gowans MC, et al. Choosing a career in surgery: factors that influence canadian medical students’ interest in pursuing a surgical career. Can J Surg. 2008;51:371–377. [PMC free article] [PubMed] [Google Scholar]
- 9.Shipper ES, Miller SE, Hasty BN, et al. Determining the educational value of a technical and nontechnical skills medical student curriculum. J Surg Res. 2018;225:157–165. [DOI] [PubMed] [Google Scholar]
- 10.Austin RE, Wanzel KR. Exposure to plastic surgery during undergraduate medical training: a single-institution review. Plast Surg (Oakv). 2015;23:43–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morzycki A, Bezuhly M, Williams JG. How competitive is plastic surgery? An analysis of the canadian and american residency match. Plast Surg (Oakv). 2018;26:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Medical Association. World Medical Association declaration of helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;3102191–2194. [DOI] [PubMed] [Google Scholar]
- 13.Oberfeld D, Franke T. Evaluating the robustness of repeated measures analyses: the case of small sample sizes and nonnormal data. Behav Res Methods. 2013;45:792–812. [DOI] [PubMed] [Google Scholar]
- 14.Fagerland MW, Lydersen S, Laake P. Recommended tests and confidence intervals for paired binomial proportions. Stat Med. 2014;33:2850–2875. [DOI] [PubMed] [Google Scholar]
- 15.Rosnow RL, Rosenthal R. Statistical procedures and the justification of knowledge in psychological science. American Psychologist. 1989;441276–1284. [Google Scholar]
- 16.Liddell MJ, Davidson SK, Taub H, et al. Evaluation of procedural skills training in an undergraduate curriculum. Med Educ. 2002;36:1035–1041. [DOI] [PubMed] [Google Scholar]
- 17.Croghan SM, Phillips C, Howson W. The operating theatre as a classroom: a literature review of medical student learning in the theatre environment. Int J Med Educ. 2019;10:75–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller S, Shipper E, Hasty B, et al. Introductory surgical skills course: technical training and preparation for the surgical environment. Mededportal. 2018;14:10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldin SB, Schnaus MJ, Horn G, et al. Surgical interest and surgical match for third-year students: results of a prospective multivariate longitudinal cohort study. J Am Coll Surg. 2012;215:599–606. [DOI] [PubMed] [Google Scholar]
- 20.Sweeney WB. Teaching surgery to medical students. Clin Colon Rectal Surg. 2012;25:127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fraser SJ, Al Youha S, Rasmussen PJ, et al. Medical student perception of plastic surgery and the impact of mainstream media. Plast Surg (Oakv). 2017;25:48–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fitzpatrick CM, Kolesari GL, Brasel KJ. Surgical origins: new teaching modalities integrating clinical and basic science years–a role for residents as active teachers. Surgery. 2003;133:353–355. [DOI] [PubMed] [Google Scholar]
- 23.Byrd P, Ward O, Hamdorf J. The effect of a surgical skills course on confidence levels of rural general practitioners: an observational study. Surg J (N Y). 2016;2:e109–e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hashimoto DA, Sirimanna P, Gomez ED, et al. Deliberate practice enhances quality of laparoscopic surgical performance in a randomized controlled trial: from arrested development to expert performance. Surg Endosc. 2015;29:3154–3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ericsson KA, Nandagopal K, Roring RW. Toward a science of exceptional achievement: attaining superior performance through deliberate practice. Ann N Y Acad Sci. 2009;1172:199–217. [DOI] [PubMed] [Google Scholar]
- 26.Clanton J, Gardner A, Cheung M, et al. The relationship between confidence and competence in the development of surgical skills. J Surg Educ. 2014;71:405–412. [DOI] [PubMed] [Google Scholar]
- 27.Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;7910 SupplS70–S81. [DOI] [PubMed] [Google Scholar]
- 28.Ericsson KA. Deliberate practice and acquisition of expert performance: a general overview. Acad Emerg Med. 2008;15:988–994. [DOI] [PubMed] [Google Scholar]


