Background:
Lower lip augmentation by filler injection is an aesthetic procedure essential for achieving a feminine look and to enhance attractiveness. Complications as a result of injury to the inferior labial artery can result in undesirable outcomes.
Methods:
The translucent technique was used to study the origin of the inferior labial artery in 11 cadavers. Ultrasonography of the inferior labial artery was also performed in 20 volunteers, which provided supplemental data to this study, in relation to establishing recommendations for filler injection.
Results:
Five different types of inferior labial artery were described. These types were found in various combination patterns. Types 2, 4, and 5 are more vulnerable to arterial injury during filler injection. Ultrasonography revealed a depth of 6 mm and an arterial position at the vermillion border as the dangerous injection plane.
Conclusion:
The origins and courses of the inferior labial artery are classified into 5 types. These types are often found in combination with each other in different faces, resulting in large anatomical variation between people. Types of combination influence severity of lower lip necrosis when arterial injury occurs. The physician should be aware of these anatomical variations during aesthetic treatments and reconstructive procedures to avoid the dangers of accidental arterial injury.
INTRODUCTION
In Asia, improving the facial contour is a current popular trend which impacts greatly on future career opportunities, especially for young women. Small and full lips are more preferable for Asian women than wide plump lips that are widely popular in Europe and the United States. To improve the facial contour from a round or square Asian face to a slim face, masseter muscle reduction and chin augmentation are the recommended combination of treatments. After contouring, the lips may appear smaller and thinner. Therefore, the patient may require lower lip augmentation to match their elongated chin and improved attractiveness. Filler injections within the lower face are relatively safe because the injection site is distant from the eye and brain.1 However, tissue necrosis of the lip and chin may occur, if there is accidental injury to an artery.2–4 Although the incidence is rare, it is essential for awareness of this complication. The inferior labial artery is the primary arterial supply to the lower lip; it also has a close relationship with the blood supply of the chin.5–9 However, previous literature has only described the artery as a single artery in limited detail.6,10,11 This study has investigated the inferior labial artery as a main branch and the combination with accessory arteries, for improvement of filler treatments. The arterial combination of the inferior labial arteries is unique and has not been previously described. Types of combination influence tissue necrosis when arterial injury occurs. These data are also essential for reconstructive surgeons who deal with traumatic and tumor cases, which may involve the inferior labial artery. Surgeons may pay attention to locate the main source of the arterial arch and then the accessory arteries using an available imaging device or surgical dissections. This study has investigated all sources of the inferior labial artery for the improvement of filler treatments. Translucent process from Sihler’s staining macerates fibrous tissues, which allows for the investigation of size, course, branching pattern, and anastomosis of the artery of interest. The size of each artery can be visually compared with other neighboring arteries. One disadvantage of using embalmed cadavers in this study is the occurrence of arterial shrinkage and senility. Ultrasonography reveals the size, depth, and position of the artery, which provides a more accurate picture. Ultrasonography of the inferior labial artery provides a practical and useful aspect for clinical application.
MATERIALS AND METHODS
Translucent Technique Modified from Sihler’s Staining Procedure
Twenty-two hemifaces of 11 cadavers with an average age of 69.9 ± 9.7 years were utilized for modified Sihler’s staining procedure. During living, all body donors took the informed consent for enrolling in medical education and in scientific research with a medical background. Red latex were bilaterally injected into the common carotid arteries to enhance visualization of the arterial system of the face. The skin was dissected superficially as thin as possible to avoid damaging minute cutaneous arteries. Then, the whole flap of facial soft tissue was harvested by elevation of the periosteal layer using surgical blades and periosteal elevators. A circumferential coronal incision was then made, which extended from the hairline, downwards along the preauricular areas to the mandibular angles and margins. Sihler’s stain was modified and utilized for the preparation of the translucent facial flaps. The basis behind this staining technique is maceration of the soft tissues until the anatomy of the arterial system is revealed. To make the tissue transparent, the first 2 steps of the modified Sihler’s protocol were carried out: (1) fixation and (2) maceration and depigmentation. The harvested specimens were first washed with running tap water and then immersed in 10% un-neutralized formalin for approximately 3 weeks or until they became hard. Specimens were then macerated and depigmented with 3% potassium hydroxide (KOH) and 0.2 ml of 3% hydrogen peroxide per 100 ml, respectively. During the staining process, the flaps were monitored on a daily basis and the subcutaneous fat was removed under operating microscopy (M525 F20; Leica Microsystems, Singapore); this prevented accidental cutting of arterial branches. The duration of this step was around 3–6 weeks. Throughout the process, the specimens gradually whitened and became translucent. All arteries, particularly the small arterial branches and their anastomoses, were seen in red. The subcutaneous fatty layer and some of masseter and temporalis were removed as custom tailoring for translucency. Care was taken not to injure the arteries. The translucent flap was set flat in a glass sheet with back illumination. The specimens were inspected under low magnification using an operating microscope and were then photographed. All arterial sources that contributed to the inferior labial artery were identified and recorded. The data were analyzed and are summarized in Tables 1–3.
Table 1.
Frequencies of the Dominant Arterial Sources of the Inferior Labial Artery
| Arterial Sources of the Inferior Labial Artery | N | % |
|---|---|---|
| Labiomental artery | 11 | 50.0 |
| Facial artery | 5 | 22.7 |
| Superior labial artery | 4 | 18.2 |
| Ascending mental artery | 2 | 9.1 |
| Total | 22 | 100 |
Table 3.
Combination of the Arterial Sources (From Arterial Arches) of the Inferior Labial Artery
| Combination of Arterial Sources of the Inferior Labial Artery | N | % |
|---|---|---|
| Labiomental a. + Modiolar a. | 8 | 36.5 |
| Facial a. + Ascending mental a. | 5 | 22.8 |
| Labiomental a. + Ascending mental a. + Modiolar a. | 2 | 9.1 |
| Labiomental a. + Superior labial a. | 2 | 9.1 |
| Facial a. + Modiolar a. | 1 | 4.5 |
| Labiomental a. + Ascending mental a. | 1 | 4.5 |
| Labiomental a. + Modiolar a. + Facial a. + Ascending mental a. | 1 | 4.5 |
| Superior labial a. + Ascending mental a. | 1 | 4.5 |
| Labiomental a. + Superior labial a. + Modiolar a. + Ascending mental a. | 1 | 4.5 |
| Total | 22 | 100 |
Table 2.
Frequencies of the Total Arterial Sources of the Inferior Labial Artery
| Arterial Sources of the Inferior Labial Artery | N | % |
|---|---|---|
| Type 1: Labiomental branch | 15 | 30.6 |
| Type 2: Modiolar branch | 12 | 24.5 |
| Type 3: Ascending mental branch | 12 | 24.5 |
| Type 4: Facial branch | 5 | 10.2 |
| Type 5: Superior labial branch | 5 | 10.2 |
| Total | 49 | 100 |
Ultrasonographic Study
The high-frequency transducer of the ultrasound machine was set to color Doppler mode ((DC-8, Mindray, Shenzhen, P.R.China) with 3 to 13 MHz linear-array transducer (L12-3E, Mindray, Shenzhen, P.R.China)) and was placed on the vermillion of the lower lip between the angle of the mouth and the midline to detect the signal of the inferior labial artery. The diameter and depth of the artery were recorded at the proximal part of the artery at the vermillion; this is summarized in Table 4. However, the ultrasonography was carried out to identify the main artery and discriminate it from accessory artery with actual living depth and diameter. Twenty healthy volunteers with an average age of 33.5 ± 13.6 years (range, 22 – 62 years) were investigated: 14 were male and 6 were female. Average body mass index of the healthy volunteers in the ultrasonographic group was 23.6 kg/M2 (SD, 2.8). These volunteers were not obese and they could represent most Asian patients in clinical practice. This study was approved by the committee of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand; the volunteers gave informed consent for using of their ultrasonographic imaging before their enrollment.
Table 4.
Parameters of the Depth and Diameter of Inferior Labial in Ultrasonographic Study
| N | Diameter, mm (range) | Depth from the skin, mm (range) | |
|---|---|---|---|
| Inferior labial a. at the proximal part in vermillion border | 40 | 1.1 ± 0.35 (0.40 – 1.80) | 5.91 ± 1.42 (2.40–9.65) |
RESULTS
Five arterial sources of the inferior labial artery were identified: the labiomental artery, the facial artery, the modiolar artery, the ascending mental artery, and the superior labial artery. These sources usually present in various combinations and not alone (Figs. 1, 2).
Fig. 1.
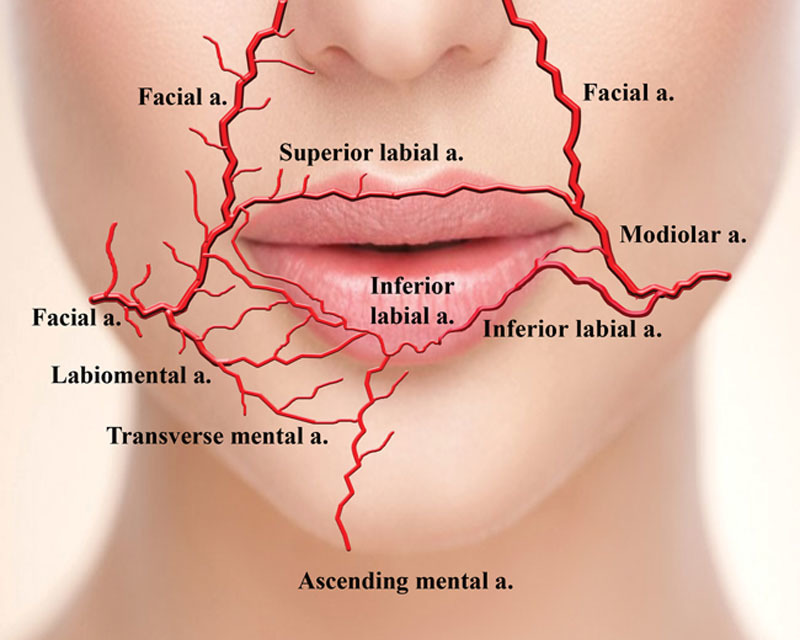
Five arterial sources of the inferior labial artery and their various combinations.
Type 1: The Labiomental Branch, 15 of 49 Cases (30.6%)
The labiomental artery is the commonest type and is usually found bilaterally in most cases (Fig. 2A). The artery arises from the facial artery as a large branch with a more dominant artery present on one side. The labiomental arteries course along and superior to the buccal sulcus, where the mucosa of the oral vestibule attaches to the gum at the alveolar process of the mandible. When the artery approaches the mental foramen, it divides into the inferior labial artery and the transverse mental artery. The inferior labial artery ascends towards the central two-thirds of the lip together with the mental nerve. There may be multiple ascending branches from the labiomental artery, which ascend obliquely and run parallel to each other to supply the lower lip vermillion.
Fig. 2.
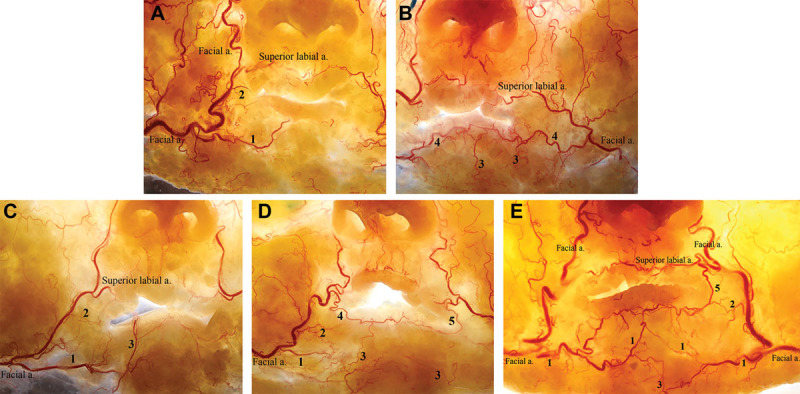
Translucent images of 5 arterial sources of the inferior labial artery and their arterial arches. 1, Type 1: the labiomental branch (A); 2, Type 2: the modiolar branch (A); 3, Type 3: the ascending mental branch (B,C); 4, Type 4: the facial artery branch (D); 5, Type 5: the superior labial branch (E).
Type 2: The Modiolar Branch, 12 of 49 Cases (24.5%)
Apart from the named branches, the facial artery has multiple small and short cutaneous perforators along its course, arising in both medial and lateral directions (Fig. 2B). There may be multiple direct branches from the facial artery, named arteries and perforators, running parallel to each other to supply the upper and lower lip vermillions and also supplying the mentum. This type of artery was usually found in combination. The modiolar artery is a supplementary source to the inferior labial artery. The artery arises as a perforator when the facial artery courses posterior to the modiolus, deep to the insertion of the zygomaticus major, the depressor anguli oris, and the risorius muscles. This artery becomes the inferior labial artery if the artery is found to be long and runs along the inner edge of the lower lip vermillion and continues into the oral mucosa. The labiomental type can be found unilaterally; however, it was found bilaterally in 1 out of 11 cadavers.
Type 3: The Ascending Mental Branch, 12 of 49 Cases (24.5%)
The ascending mental artery emerges from the neck lateral to the insertion of the digastric muscle (Fig. 2B–D). The artery ascends paramedially across the mental protuberance to the chin. This artery may continue superiorly on one side and enter the medial part of the lower lip vermillion as the inferior labial artery. This type was found in 1 out of 11 cadavers.
Type 4: The Facial Artery Branch, 5 of 49 Cases (10.2%)
The facial artery divides directly into the inferior labial artery as a large branch, as it crosses the mandibular margin to the face (Fig. 2B, D). The artery courses obliquely throughout the buccal tissues to the modiolus and enters the lower lip vermilion close to the corner of the mouth. This artery forms a large anastomosis with its counterpart artery on the opposite side.
Type 5: The Superior Labial Branch, 5 of 49 Cases (10.2%)
The superior labial artery may give rise to the inferior labial artery at its proximal part, just above the corner of the mouth (Fig. 2D, E). The inferior labial artery curves around the mouth corner to the lower lip. A common trunk of the labial artery may form if the diameters of both labial arteries are comparable. This type was found unilaterally in 2 out of 11 cadavers.
In each side of the face, the inferior labial artery that supplies the lower lip vermillion is formed by a combination of the many branches from the different possible sources. These combinations form an arterial arch, which communicates with the counterpart arch on the opposite side. The large artery that provides most blood supply to the lower lip is the main artery forming the arterial arch (types 1 and 4), and all small arteries that join the arch are the accessory arteries (types 2, 3, and 5). The different combinations found in this study are presented in Table 3.
Ultrasound technology detected the main inferior labial artery in all cases. Small perforators or accessory arteries were absent and filtered out. The diameters and depths of the inferior labial artery that were measured by ultrasound at the lower lip vermillion or the labiomental sulcus are 1.10 ± 0.35 and 5.91 ± 1.42 mm, respectively (Fig. 4 and Table 4).
Fig. 4.
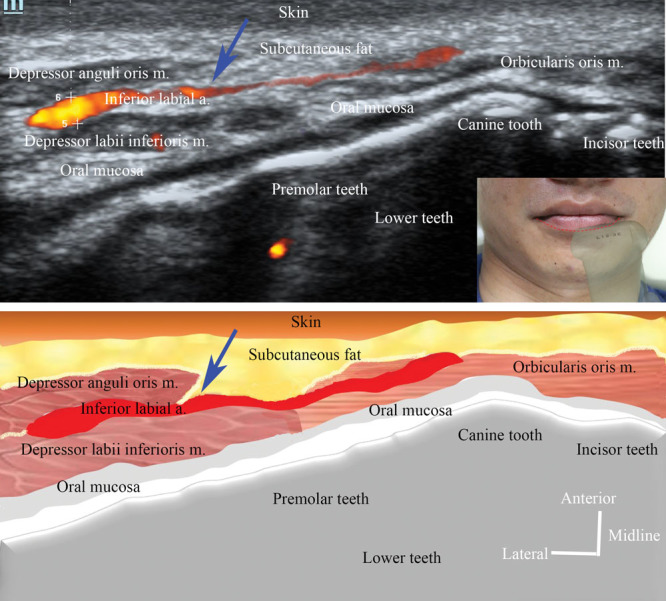
Ultrasound image and relating illustration of the main inferior labial artery at the vermilion border of the lower lip and its depth from the vermilion border.
DISCUSSION
An arterial arch with the diameter of 1.10 ± 0.35 mm is identified at the level of the vermillion border of the lower lip. Fortunately, this arch travels mainly in the deep muscular plane at the depth of 5.91 ± 1.42 mm from the skin. Likely, Lee et al.12 found that the labial artery mostly located in wet mucosa layer (28%–55%) of the lower lip with a depth of 4.2 ± 0.4 mm forms the surface of the vermilion border. Comparing with the study of Koziej et al.,13 the mean diameter of inferior labial artery was 1.00 ± 0.33 mm. Therefore, there was no ethic difference of inferior labial artery parameters. Because of the tortuosity, the arterial arch may enter into the central muscular core and subdermis of the approximating surface at the depth of 2.4 mm or submucosa of the inner surface of the vermilion at the depth of 9.7 mm. All arterial branches of the facial artery in the lower face, primary or secondary, named or unnamed, can form part of this arterial arch of the lower lip, depending on the points and directions that they can reach the arch.
The facial artery divides into multiple branches along its course within the face. The large branches that are usually long and anastomose with the counterpart on the opposite side are named.5,7,9 All short and small branches are unnamed and are called perforators, because they supply small cutaneous areas, which can be used as local flaps.14,15 The modiolar artery is one of the perforators that supplies the composite tissues at the mouth corner. Although this artery is small, it may join the lower lip arterial arch and continue along the inner side of the lower lip vermillion as the inferior labial artery. This artery may arise from the superior labial artery as well. In the study of Crouzet et al.,16 however, the arterial supply of the lower lip derived from only the inferior labial and branches of mental artery. Banks et al.17 described that the lower lip was perfused by single external carotid artery and both carotid artery in 40% and 60%, respectively.
These anatomical findings can emphasize the correct injection technique. If this lower lip arterial arch is injured and occluded at the main artery, survival of the lower lip vermillion depends on the accessory arteries and contralateral anastomosis forming a complete arterial arch. Incomplete arterial arch and few accessory arteries may result in obvious lower lip necrosis (Fig. 2A). On the contrary, numerous accessory arteries and/or complete arterial arch can mitigate severity of tissue necrosis (Fig. 2B–E).
To achieve “dolly lips” for the patient, the lower lip eminences must accommodate the median tubercle of the upper lip. These 2 eminences should be equally enlarged and the vermillion needs a well-defined border. Although the lower lip is usually designed to be bigger than the upper lip, the lateral one-third of the vermillion should be left untouched, except in patients who need a plumper lower lip, which is out of date. Elevation of the mouth corner is obtained by an injection at the lower lip vermillion border of the mouth corner and deep to the skin below the corner using a needle. Needle injections are precise and effective, but they pose a higher risk compared to injection using cannulation. However, the aspiration before injection is highly needed. Moreover, slow injection is crucial and the injection should be immediately stopped when a blanching area appears. Focusing on the possibility of injury to the inferior labial artery at the deep tissue plane, filler injections within the lower face need superficial injections. These are injections within the lower lip, marionette line, and injections for chin augmentation. Similar to Cotofana et al.,6 the subcutaneous injection is a safer location for lower lip paramedian augmentation, while injection into more superficial plane along the midline should be carefully done because of arterial variations.
The lower lip vermillion has 3 surfaces: exposing, approximating, and an inner surface (Fig. 3). Injections performed underneath these 3 surfaces create different results. Injections on each surface elevate and enlarge that surface. Based on typical anatomy of the inferior labial arch, trying to evert the inner surface of the vermillion by injecting along the wet dry border of the vermillion leads to bulging of the inner surface into the teeth and it is also high risk for injury to the inferior labial artery. To enlarge the lower lip vermillion, 3 planes of injections are required. These are the approximating surface, the exposing surface, and injections into the central core along the lip vermillion. Injection at the central core may lead to the needle encountering a tortuous part of the inferior labial artery; rhythmic injections or multiple retrograde injections are therefore needed. The vermillion border is safe for needle injections, because the artery is 2.4 mm deep from the skin. If the vermillion border is injected and the lower lip is not sufficiently projected, pinch the vermillion and puncture from the vermillion border, making parallel columns of filler and strut using a needle at the skin underneath the vermillion to create a lower lip elevation at the side of the transverse labiomental groove. A superficial injection using a needle right at the vermillion corner of the lower lip elevates the lip corner creating a “secret smile.”
Fig. 3.
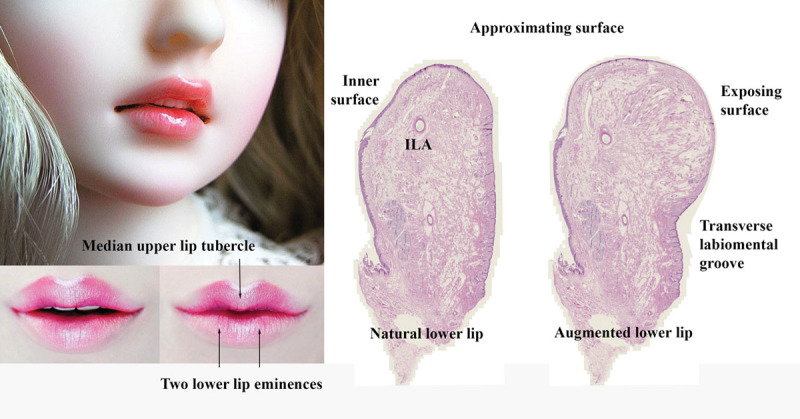
Three surfaces of lower lip vermillion: exposing, approximating, and inner surface.
The upper end of the marionette line poses a risk of injury to the inferior labial artery that arises directly from the facial artery or from the superior labial artery (types 2–4 in Table 1). In general, it is sufficient to inject within the plane of the superficial subcutaneous tissue at the lower lip side of the nasolabial fold. Injections at the deeper plane can also encounter the origin from the facial artery of the inferior labial artery. Injection begins at the groove of the upper end of the marionette line. This line is also named anatomically as the vertical labiomental fold. Care should be taken not to inject on the buccal side of the groove, otherwise a more prominent fold is created. A bridging or railroad technique across the fold using a needle is often performed superficially at the dermal–subcutaneous junction to enhance the skin thickness. Bridging should be performed using a needle in short parallel columns across the marionette groove or short alternative columns from the groove in the ferning technique. Two long columns usually fold at the original marionette groove at a later date and create a lump at the mouth corner with a deep marionette fold. Intradermal injections using a wrong technique can create a lump or an irregularity.
Chin augmentation, either for inferior or anterior projections, can injure the ascending mental artery, which is a possible origin of the inferior labial artery. Midline injection is recommended to avoid arterial injury. Paramedian injections can be performed with care using special techniques. Rhythmic injections or a skipping technique may be more preferable than a large bolus injection, as this reduces the risk of an arterial embolus. Retrograde injections into multiple planes of the chin using the pull-down maneuver facilitate filler placement for extreme chin elongation. Compression at the mandibular margin must be performed during the pull-down maneuver to prevent filler embolising to the tongue and floor of the mouth.
CONCLUSIONS
The origins and courses of the inferior labial artery are classified into 5 types, which can be found in various combinations within different faces. This creates different combination patterns of anatomical variation. The physician should be aware of these variations while performing aesthetic treatments or reconstructive procedures to avoid accidental arterial injury.
ACKNOWLEDGEMENT
This research was supported by Ratchadapisek Somphote Fund for Postdoctoral Fellowship, Chulalongkorn University.
Footnotes
Published online 27 September 2019
Disclosure: None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
REFERENCES
- 1.Beleznay K, Carruthers JD, Humphrey S, et al. Avoiding and treating blindness from fillers: a review of the world literature. Dermatol Surg. 2015;41:1097–1117. [DOI] [PubMed] [Google Scholar]
- 2.Fang M, Rahman E, Kapoor KM. Managing complications of submental artery involvement after hyaluronic acid filler injection in chin region. Plast Reconstr Surg Glob Open. 2018;6:e1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Q, Zhao Y, Li H, et al. Vascular complications after chin augmentation using hyaluronic acid. Aesthetic Plast Surg. 2018;42:553–559. [DOI] [PubMed] [Google Scholar]
- 4.Woodward J, Khan T, Martin J. Facial filler complications. Facial Plast Surg Clin North Am. 2015;23:447–458. [DOI] [PubMed] [Google Scholar]
- 5.Cotofana S, Lachman N. Arteries of the face and their relevance for minimally invasive facial procedures: an anatomical review. Plast Reconstr Surg. 2019;143:416–426. [DOI] [PubMed] [Google Scholar]
- 6.Cotofana S, Pretterklieber B, Lucius R, et al. Distribution pattern of the superior and inferior labial arteries: impact for safe upper and lower lip augmentation procedures. Plast Reconstr Surg. 2017;139:1075–1082. [DOI] [PubMed] [Google Scholar]
- 7.Hwang K, Lee GI, Park HJ. Branches of the facial artery. J Craniofac Surg. 2015;26:1399–1402. [DOI] [PubMed] [Google Scholar]
- 8.Samizadeh S, Pirayesh A, Bertossi D. Anatomical variations in the course of labial arteries: a literature review. Aesthet Surg J. 2018. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Yang HM, Lee JG, Hu KS, et al. New anatomical insights on the course and branching patterns of the facial artery: clinical implications of injectable treatments to the nasolabial fold and nasojugal groove. Plast Reconstr Surg. 2014;133:1077–1082. [DOI] [PubMed] [Google Scholar]
- 10.Lee SH, Gil YC, Choi YJ, et al. Topographic anatomy of the superior labial artery for dermal filler injection. Plast Reconstr Surg. 2015;135:445–450. [DOI] [PubMed] [Google Scholar]
- 11.Al-Hoqail RA, Meguid EM. Anatomic dissection of the arterial supply of the lips: an anatomical and analytical approach. J Craniofac Surg. 2008;19:785–794. [DOI] [PubMed] [Google Scholar]
- 12.Lee KL, Lee HJ, Youn KH, Kim HJ. Positional relationship of superior and inferior labial artery by ultrasonography image analysis for safe lip augmentation procedures. Clin Anat. 2019. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 13.Koziej M, Trybus M, Holda M, et al. Anatomical map of the facial artery for facial reconstruction and aesthetic procedures. Aesthet Surg J. 2019. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 14.Posso C, Delgado Anaya D, Aguilar Henao J, et al. Nasolabial propeller perforator flap: Anatomical study and case series. J Surg Oncol. 2018;117:1100–1106. [DOI] [PubMed] [Google Scholar]
- 15.Guha G, Chatterjee D, Biswas S, et al. Evaluation of facial artery perforator-based flaps in reconstruction of facial defects. Indian J Plast Surg. 2017;50:266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crouzet C, Fournier H, Papon X, et al. Anatomy of the arterial vascularization of the lips. Surg Radiol Anat. 1998;20:273–278. [DOI] [PubMed] [Google Scholar]
- 17.Banks ND, Hui-Chou HG, Tripathi S, et al. An anatomical study of external carotid artery vascular territories in face and midface flaps for transplantation. Plast Reconstr Surg. 2009;123:1677–1687. [DOI] [PubMed] [Google Scholar]


