Abstract
We previously reported that at 1-and-4 weeks of sobriety, those who relapsed after treatment demonstrated significantly smaller total frontal cortical volume than individuals who maintained abstinence for at least 12 months post treatment. The segmentation method employed did not permit examination of frontal subregions that serve as nodes of the executive, salience and emotional regulation networks; structural abnormalities in these circuits are associated with relapse in those seeking treatment for alcohol use disorders (AUD). The primary goal of this study was to determine if frontal cortical subregion volume recovery during early abstinence is associated with long-term abstinence from alcohol. We compared bilateral components of the dorsal prefrontal cortex, orbitofrontal cortex, anterior cingulate cortex and insula volumes, at 1 and 4 weeks of abstinence, between individuals who resumed drinking within 12 months of treatment (Relapsers) those who showed sustained abstinence over 12 months following treatment (Abstainers) and healthy Controls. At 1 and 4 weeks of sobriety, Relapsers demonstrated significantly smaller volumes than Controls in the 15 of 20 regions of interest, while Abstainers only had smaller volumes than Controls in 5 of 20 regions. In Relapsers, increasing volumes over 1 month in multiple frontal subregions and the insula were associated with longer duration of abstinence after treatment. The persistent bilateral frontal and insula volume deficits in Relapsers over 4 weeks from last alcohol use may have implications for neurostimulation methods targeting anterior frontal/insula regions, and represent an endophenotype that differentiates those who respond more favorably to available psychosocial and pharmacological interventions.
Keywords: alcohol use disorder, brain volumes, relapse, magnetic resonance imaging, neurostimulation
INTRODUCTION
Approximately 60% of individuals with an alcohol use disorder (AUD) will relapse to hazardous alcohol consumption within 6 months of treatment with currently available psychosocial and pharmacological interventions (Witkiewitz, 2011). Non-invasive neurostimulation techniques, such as repetitive transcranial magnetic stimulation (rTMS), are increasingly being evaluated as novel treatments for individuals with AUD and substance use disorders (SUD) (Dunlop, Hanlon, & Downar, 2017; Salling & Martinez, 2016). Studies investigating the neurobiological effects and/or clinical efficacy of rTMS in AUD and SUD have most frequently targeted the dorsolateral prefrontal cortex (DLPFC), dorsomedial prefrontal cortex, ventromedial prefrontal cortex, and insula (Bellamoli et al., 2014; Salling & Martinez, 2016), with the DLPFC and ventromedial prefrontal cortex as the most common rTMS targets in AUD. Magnetic resonance (MR) imaging studies of AUD have demonstrated that those who relapse after treatment, compared to individuals who maintain extended abstinence, exhibit smaller volumes in dorsolateral, dorsomedial, ventromedial and orbitofrontal prefrontal cortical regions during the first month of abstinence (Beck et al., 2012; Cardenas et al., 2011; Durazzo et al., 2011; Rando et al., 2011). The collective MR-based morphometric studies investigating biomarkers for relapse in AUD indicate the macrostructural integrity of anterior frontal regions that are nodes of the executive, salience, reward and emotional regulation networks (Moorman, 2018; Seeley et al., 2007; Williams, 2016) is related to treatment outcome (Seo & Sinha, 2014, 2015). Therefore, the neurobiological effects of rTMS may be influenced by the macrostructural integrity and/or level of atrophy of brain tissue that is the target of stimulation (Stokes et al., 2007). We previously employed a different MR image segmentation method (Durazzo, Mon, Gazdzinski, & Meyerhoff, 2016) in the same cohort used for the current analysis and found that individuals who relapsed within 12 months after treatment, compared to those who had sustained abstinence for at least 12 months, showed significantly smaller bilateral total frontal gray matter (GM) volumes at approximately 1-week of sobriety. Over the ensuing 3-weeks, both abstainers and relapsers demonstrated significant and equivalent rates of change in total frontal GM volume, a macroscopic indicator of adaptive neuroplasticity (Buhler & Mann, 2011; Durazzo, Mon, Gazdzinski, Yeh, & Meyerhoff, 2015); however, only relapsers continued to exhibit smaller total bilateral frontal GM volumes than controls at 4-weeks of monitored sobriety. Given that previous clinical trials evaluating the efficacy of rTMS were logically initiated during the early phase of treatment and targeted anterior frontal lobe subregions, regional differences in volume recovery during this early phase may influence rTMS treatment response. To date, no study has specifically investigated volume changes of anterior frontal cortical regions of future abstainers and relapsers, during the early phase of recovery, that also may serve as rTMS cortical targets.
Our primary goal was to determine if volume changes in frontal cortical and anterior cingulate subregions and the insula of alcohol dependent participants during early abstinence are associated with treatment outcome. Specifically, we compared bilateral anterior cingulate, orbitofrontal, and dorsolateral subregions, as well as bilateral insula and precentral gyrus volumes during early recovery between those who resumed alcohol consumption within 12 months of treatment (Relapsers), those who successfully maintained abstinence over 12 months after treatment (Abstainers) and healthy controls (Controls). This study extends our previous research by investigating functionally distinct subregions of the frontal cortex during early abstinence from alcohol. We hypothesized that: 1) Compared to Controls, both Abstainers and Relapsers demonstrate smaller regional volumes at approximately 1 week (assessment point 1; AP1) and 4 weeks (assessment point 2; AP2) of abstinence; 2) Relapsers show smaller volumes than Abstainers in all regions at AP1 and AP2; 3) Relapsers show less volume recovery in all regions than Abstainers over approximately 4 weeks of sustained abstinence; and 4) In Relapsers, greater regional volume recovery over 4 weeks is related to longer duration of abstinence following treatment.
MATERIALS AND METHODS
Participants
Individuals seeking treatment for AUD (n = 119) were recruited from the San Francisco VA Medical Center (SFVAMC) Substance Abuse Day Hospital and the San Francisco Kaiser Permanente Chemical Dependence Recovery outpatient treatment clinics [for additional information on the treatment program characteristics see (Durazzo, Gazdzinski, Yeh, & Meyerhoff, 2008)]. The predominantly male Veteran treatment-seeking patients were between 28 and 71 years of age and met DSM-IV criteria for alcohol dependence. All alcohol dependent individuals were actively in treatment at the time of assessment, and treatment duration typically ranged from 14–35 days (median of 21 days). Thirty-three non-smoking, light drinking controls (Controls) were recruited from the local community and screened for biomedical or psychiatric conditions known or suspected to influence brain neurobiology. All participants provided written informed consent prior to study. Study procedures were approved by the University of California San Francisco and the SFVAMC and were in accordance with the ethical standards of the Declaration of Helsinki.
Inclusion/exclusion criteria:
Primary inclusion criteria for the alcohol dependent participants were fluency in English, DSM-IV diagnosis of alcohol dependence/abuse at baseline (all met criteria for alcohol dependence), consumption of greater than 150 standard alcohol-containing drinks (i.e., 13.6 grams of pure ethanol) per month for at least 8 years prior to enrollment for males, and greater than 80 drinks per month for at least 6 years prior to enrollment for females. See Table 1 for group demographic data. Alcohol dependent individuals were excluded for any history of the following: dependence on any substance other than alcohol or nicotine in the 5 years immediately prior to enrollment, any intravenous drug use in the 5 years prior to baseline study, opioid agonist therapy, HIV/AIDS, cerebrovascular accident, cerebral aneurysm, arteriovenous malformations, myocardial infarction, medically uncontrolled chronic hypertension (systolic > 180 and/or diastolic > 120 mmHg), type-I diabetes, chronic obstructive pulmonary disease, non-alcohol related seizures, significant exposure to established neurotoxins, intrinsic cerebral masses, demyelinating and neurodegenerative diseases, Wernicke-Korsakoff syndrome, delirium, penetrating head injury, and closed head injury resulting in loss of consciousness > 10 minutes. Psychiatric exclusion criteria were history of schizophrenia-spectrum disorders, bipolar disorder, cyclothymia, PTSD, obsessive-compulsive disorder and panic disorder. Hepatitis C, type-2 diabetes, hypertension, unipolar mood disorders (i.e., major depression, substance-induced mood disorder) were allowed in the alcohol dependent group, given their high prevalence in AUD (Grant et al., 2015; Mertens, Weisner, Ray, Fireman, & Walsh, 2005). Participants were breathalyzed and urine-tested for illicit substances before all assessments. Additionally, the treatment programs regularly tested participants for alcohol and substance use. No participant tested positive for alcohol or substances during treatment or at any AP.
Table 1.
Group Demographics and Clinical Variables
| Measure | Controls (n = 33) | ABS (n = 39) | REL (n = 65) | Group comparisons* |
|---|---|---|---|---|
| Age (years) | 46 (9) | 53 (9) | 51 (8) | CON < ABS, REL |
| Education (years) | 16.7 (2.6) | 14.6 (2.2) | 13.5 (1.9) | CON > ABS, REL; ABS > REL |
| Males (%) | 94 | 90 | 92 | |
| Caucasian (%) | 73 | 79 | 74 | |
| Days abstinent at AP2 | NA | 33 (9) | 33 (10) | |
| Days until relapse | NA | NA | 137 (80) | |
| Lifetime average drinks/month | 16 (14) | 182 (93) | 245 (145) | CON < ABS, REL; ABS < REL |
| Anti-relapse/craving medication (%) | NA | 15 | 22 | |
| Antidepressant s (%) | NA | 5 | 12 | |
| Psychiatric comorbidity (%) | NA | 23 | 49 | ABS < REL |
| Substance use disorder comorbidity (%) | NA | 21 | 15 | |
| Medical comorbidity (%) | NA | 44 | 54 | |
| Smokers (%) | NA | 51 | 62 | |
| FTND | NA | 5 (2) | 5 (2) | |
| Pack years | NA | 27 (19) | 28 (21) | |
| BDI | 4 (3) | 9 (8) | 10 (8) | CON < ABS, REL |
| STAI | 33 (7) | 47 (10) | 50 (13) | CON < ABS, REL |
| Body mass index | 25 (5) | 26 (5) | 27 (5) | |
| Number of previous AUD treatments (median) | NA | 2 | 3 | |
| Intracranial volume (cc) | 1596 (162) | 1599 (132) | 1575 (148) |
Note. ABS: Abstainers. AP2: Assessment point 2; BDI: Anti-relapse/craving medication: use of disulfiram, gabapentin and/or naltrexone; Beck Depression Inventory. CON: Controls. FTND: Fagerstrom Test for Nicotine Dependence. NA: not applicable. REL: Relapsers. STAI: State -trait Anxiety Inventory – Trait.
All listed group comparisons p < .05. Mean (SD).
Seventy-eight alcohol dependent participants (24 Abstainers; 54 Relapsers) completed a magnetic resonance imaging (MRI) study 7 ± 4 days after consumption of their last alcohol drink (AP1); eleven individuals relapsed between AP1 and AP2 and had no AP2 scan. One hundred four alcohol dependent participants (39 Abstainers; 65 Relapsers) completed an MRI after approximately 33 ± 9 days of abstinence (AP2). Sixty-three participants were studied at both AP1 and AP2, but four were excluded at AP2 because of inferior data quality. Forty-one participants were enrolled and first studied at AP2, because they completed acute detoxification at another SFVAMC or Kaiser Permanente sponsored program, precluding their participation at AP1. Control participants completed a single MR study and clinical assessment.
Definition of Abstainers and Relapsers and follow-up procedures:
Participants were followed for 12 months following AP2. Initial follow-up 1 (in person, telephone and/or collateral source interview, and/or medical record review) took place 5–7 months after AP2. Seventy-six of the 119 alcohol dependent participants originally studied at AP2 were revaluated approximately 7 months later with all MR scans, psychiatric and behavioral measures administered at AP1 as well as the Time Line Follow-Back (L. C. Sobell et al., 1988; L. Sobell, Sobell, Maisto, & Cooper, 1985) to specifically assess alcohol consumption patterns during relapse. For the remaining 43 participants, follow-up 1 assessment involved brief in-person and/or telephone contact (n = 25), review of available medical records (n = 17), and/or telephone interview of collateral sources (i.e., family or friends; n = 1), where only relapse status (i.e., any alcohol consumption) and date of relapse onset (if known) was obtained. Abstainers: participants were designated as Abstainers if they met all the following criteria: a) self-reported no alcohol consumption between AP1-AP2 and long-term follow-up; b) there was no report of alcohol consumption between baseline and follow-ups in available medical records; and c) available laboratory indicators of alcohol consumption (gamma glutamyltransferase; GGT) were within normal limits at follow-up. For follow-up 2, all Abstainers were contacted (in-person or via telephone) again approximately 5–7 months after the follow-up 1 to determine if they maintained continuous sobriety over the 12-month observation period. Relapsers: participants were designated as Relapsers if they met any of the following criteria: a) self-report of any alcohol consumption after AP1 or AP2 within 12 months via in-person or telephone interview; b) alcohol consumption or relapse was indicated in available medical records; c) report of participant alcohol use provided by a relative or close friend via telephone contact. In our previous studies, any level of alcohol consumption following treatment was associated with compromised psychosocial functioning (Durazzo et al., 2008). See Figure 1 for summary of participant assessment timeline.
Figure 1.
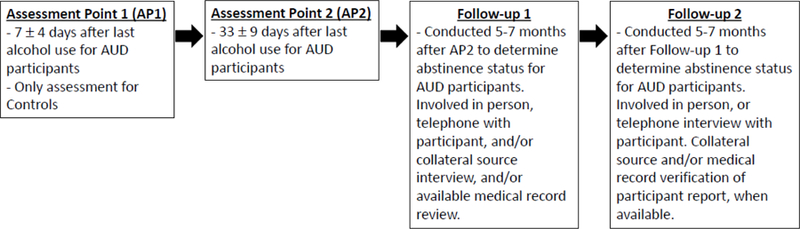
Participant Assessment Timeline
Clinical Measures
Participants completed the Clinical Interview for DSM-IV Axis I Disorders, Version 2.0 (SCID-I/P) and semi-structured interviews for lifetime alcohol consumption (Lifetime Drinking History) and substance use (in-house questionnaire assessing substance type, and quantity and frequency of use). From the Lifetime Drinking History, average number of alcoholic drinks/month over 1 year prior to enrollment, and average number of drinks/month over lifetime were calculated. At AP1 and AP2, participants also completed standardized questionnaires assessing depressive (Beck Depression Inventory, BDI) and anxiety symptomatology (State-Trait Anxiety Inventory, Trait form Y-2, STAI), as well as nicotine dependence via the Fagerstrom Tolerance Test for Nicotine Dependence (FTND). See (Pennington et al., 2013) for corresponding references for the above measures.
MR Data Acquisition and Processing
Structural images were acquired on a 1.5 Tesla MR system (Vision, Siemens Medical Systems, Iselin NJ) with a T1-weighted Magnetization Prepared Rapid Acquisition Gradient Echo sequence (MPRAGE; 1 × 1 mm2 in-plane resolution, 1.5 mm contiguous slabs) oriented orthogonal to the long axis of the hippocampus [see (Mon et al., 2013) for specific imaging parameters]. The publicly available FreeSurfer (v4.5) volumetric segmentation and cortical surface reconstruction methods were used to obtain cross-sectional (Fischl et al., 2004) and longitudinal (Reuter, Schmansky, Rosas, & Fischl, 2012) measures of regional cortical volumes (mm3) from T1-weighted MPRAGE images. First, cross-sectional scans of all participants were processed followed by rigorous quality control and manual editing, if necessary (Durazzo et al., 2014). An unbiased template of each participant was then created from the cumulative cross-sectional data. Longitudinal processing for alcohol dependent participants was performed on the cross-sectional data with the template for each participant that generated 34 anatomical regions of interest per cortical hemisphere. Average cortical volume was obtained for all 34 bilateral cortical regions of interest (ROI), but analyses were confined to frontal and anterior cingulate subregions, and insula (see Table 2). Volumes from the lateral orbitofrontal and pars orbitalis for each hemisphere were summed because these regions are often considered to constitute the lateral orbitofrontal cortex [see (Fettes, Schulze, & Downar, 2017) and references therein]. The precentral gyri was included because the treatment level of rTMS is typically based on the motor threshold (magnitude required by a single TMS pulse to consistently elicit motor activity) of select contralateral upper or lower extremity muscles (George, 2007). All cortical ROI volumes that comprise the frontal neocortex (superior frontal gyri, rostral and caudal middle frontal gyri, frontal pole, precentral gyri, medial and lateral orbitofrontal cortex, and pars triagularis, opercularis and orbitalis), were summed for each hemisphere to form total left and right frontal cortex volumes. Please see Durazzo et al., 2011 for a representative figure of the ROIs used in this study.
Table 2.
Assessment Point 1 Regional Volumes for Controls, Abstainers and Relapsers
| Region | Hemisphere and Subregion | CON (n = 33) | ABS (n = 24) | REL (n = 54) | ES CON vs. ABS | ES CON vs. REL | ES ABS vs. REL |
|---|---|---|---|---|---|---|---|
| Anterior Cingulate | Left Caudal | 1923 (454) | 1755 (451) | 1822 (448) | 0.37 | 0.22 | 0.15 |
| Right Caudal | 2214 (408) | 2100 (402) | 1984 (397)$ | 0.28 | 0.58 | 0.29 | |
| Left Rostral | 2546 (349) | 2330 (344)# | 2221 (344)$ | 0.62 | 0.94 | 0.32 | |
| Right Rostral | 1841 (345) | 1784 (340) | 1726 (341) | 0.17 | 0.34 | 0.17 | |
| Orbitofrontal | Left Medial | 4540 (552) | 4356 (544) | 4290 (550) | 0.34 | 0.46 | 0.12 |
| Right Medial | 5093 (641) | 4676 (632)# | 4620 (639)$ | 0.65 | 0.74 | 0.09 | |
| Left Lateral | 9746 (854) | 9455 (842) | 8998 (843)$, & | 0.34 | 0.89 | 0.54 | |
| Right Lateral | 9881 (835) | 9566 (823) | 9274 (824)$ | 0.42 | 0.74 | 0.36 | |
| Dorsal Prefrontal | Left Caudal Middle Frontal | 6598 (1216) | 6089 (1198) | 5962 (1211) | 0.38 | 0.53 | 0.10 |
| Right Caudal Middle Frontal | 5967 (1050) | 5905 (1198) | 5534 (1046) | 0.06 | 0.42 | 0.36 | |
| Left Rostral Middle Frontal | 15382 (1964) | 14743 (1934) | 13892 (1956)$ | 0.33 | 0.77 | 0.44 | |
| Right Rostral Middle Frontal | 16386 (2071) | 15440 (2039) | 14547 (2063)$ | 0.46 | 0.90 | 0.44 | |
| Left Superior Frontal | 22238 (1899 | 21246 (1870) | 20261 (1891)$ | 0.53 | 1.05 | 0.52 | |
| Right Superior Frontal | 21353 (1956) | 20703 (1926) | 19747 (1948)$, & | 0.34 | 0.83 | 0.49 | |
| Precentral | Left | 12489 (1183) | 12656 (1201) | 11799 (1183)$, & | 0.14 | 0.58 | 0.72 |
| Right | 12742 (1149) | 12868 (1131) | 11862 (1215)$, & | 0.12 | 0.75 | 0.86 | |
| Insula | Left | 6543 (458) | 6182 (1926)# | 6060 (452)$ | 0.79 | 1.07 | 0.27 |
| Right | 6507 (455) | 6146 (448)# | 6047 (449)$ | 0.80 | 1.03 | 0.22 | |
| Total Frontal Cortical | Left | 80291 (5186) | 76883 (5107)# | 73726 (5165)$, & | 0.66 | 1.28 | 0.61 |
| Right | 80259 (5516) | 77329 (5433) | 73999 (5495)$, & | 0.54 | 1.15 | 0.61 |
Note. Mean (SD); ABS: Abstainers; CON: Non-smoking Light Drinking Controls; ES: Effect size; REL: Relapsers;
CON > ABS, p ≤ .026;
CON > REL, p ≤ .026;
ABS > REL, p ≤ .026.
Data Analyses
Demographic and clinical data:
Comparisons of demographic and clinical data between Controls, Abstainers and Relapsers were conducted with univariate analysis of variance and Fishers Exact Test, where indicated. There were no significant differences in demographic or clinical variables between the alcohol dependent cohorts at AP1 and AP2, except for lower BDI and STAI scores at AP2; therefore, values for the larger AP2 sample are reported in all tables.
Cross-sectional regional brain volumetric comparisons between Controls, Abstainers and Relapsers:
Group comparisons on regional GM volumes at AP1 and AP2 were conducted with generalized linear modeling and follow-up pairwise t-tests. Controls were younger and had more years of education than Abstainers and Relapsers (see Table 1). Therefore, age, education and intracranial volume (ICV) were used as covariates in univariate models and pairwise t-tests between Controls and the alcohol dependent groups. Average number of drinks/month over lifetime, years of education and frequency of psychiatric comorbidities (primarily unipolar mood disorders) were significantly higher in Relapsers than Abstainers (see Table 1); these variables, age and ICV were used as covariates in all pairwise t-tests for Abstainers and Relapsers. Effect sizes for pairwise t-tests of group means were calculated with Cohen’s d (Cohen, 1977). Although we specified a priori predictions for frontal GM differences between Abstainers and Relapsers, statistical significance levels (p < .05) for all pairwise t-tests at AP1 and AP2 were corrected for multiple comparisons accounting for the 18 ROIs (left and right total frontal cortical volumes were treated as separate summary measures) and the average intercorrelations among ROIs for all groups combined (r = 0.77). This modified Bonferroni method (Sankoh, Huque, & Dubey, 1997) yielded an adjusted significance level of p ≤ .026 for pairwise t-tests. The same regional volume values for Controls were used for AP1 and AP2 comparisons with Abstainers and Relapsers; this is justified as we previously observed no significant regional volumes changes in this Control cohort over approximately 6 months (Durazzo et al., 2015).
Longitudinal regional brain volumetric comparisons between Abstainers and Relapsers:
Longitudinal ROI volume changes in Abstainers and Relapsers over approximately 1 month of abstinence were assessed with linear mixed modeling. In this analysis, the focus was on the group (Abstainers vs. Relapsers) x days abstinent interaction and the main effect for days abstinent (time). Main effects for days abstinent were followed-up with simple effects tests for Abstainers and Relapsers. Random intercepts were modeled for all participants. Average number of drinks/month over lifetime, age, years of education, frequency of comorbid psychiatric conditions, and ICV were employed as covariates in these analyses. Interactions, main and simple effects for all ROIs were considered statistically significant at p < .05.
Associations between regional brain volume changes and duration of post-treatment abstinence in Relapsers:
Associations between change in regional brain volumes and duration of abstinence after treatment in Relapsers were assessed for Relapsers via linear mixed modeling. The duration of post-treatment abstinence served as the dependent measure, with age, lifetime average drinks/month, ICV and ROI volume (e.g., left lateral OFC) as predictors. These exploratory associations were considered statistically significant at p < .05.
RESULTS
Group demographics and clinical measures
Controls were younger, had more education, and demonstrated lower BDI and STAI scores than Abstainers and Relapsers (all p < .05). Abstainers and Relapsers were equivalent on age, BDI and STAI scores, duration of abstinence at AP1 and AP2, cigarette consumption measures, and frequency of the following: anti-relapse/craving medication use, antidepressant use, cigarette smokers, history of substance use disorders and comorbid medical conditions. The most common medical conditions among the alcohol dependent group were hypertension (n = 28) and hepatitis C positivity (n = 15), and Abstainers and Relapsers were equivalent on the frequency of these conditions. Abstainers had a higher level of education, lower lifetime alcohol consumption and a lower frequency of psychiatric comorbidities than Relapsers (all p < .05). The three groups were equivalent on ICV and percent of male and Caucasian participants (See Table 1). .
Volume comparisons of Controls, Abstainers and Relapsers at AP1 (1 week of abstinence)
As seen in Table 2, Relapsers showed significantly smaller volumes than Controls in bilateral precentral gyrus, insula and total frontal cortex, as well as in multiple subregions of anterior cingulate (ACC), orbitofrontal (OFC), dorsal prefrontal (DPFC) cortical subregions (all p ≤ .026); the magnitude of these differences were moderate to strong. Abstainers had significantly smaller volumes than Controls in the left rostral ACC, right medial OFC, bilateral insula and left total frontal cortex, with correspondingly moderate effect sizes (all p ≤ .026). Relapsers exhibited smaller volumes than Abstainers in the left lateral OFC, right superior frontal gyrus, bilateral precentral gyri and bilateral total frontal cortex (all p ≤ .026), with moderate to strong effect sizes. Greater age was inversely related to volumes in all regions (p < .01) except bilateral ACC subregions and bilateral insula. In comparisons between Abstainers and Relapsers, average number of drinks/month over lifetime, years of education, and frequency of psychiatric comorbidities were not significant predictors of volume for any ROI.
Volume changes for Abstainers and Relapsers over AP1-AP2 Interval
Main effects for group (Abstainers vs. Relapsers) were observed for the left rostral ACC, left lateral OFC, right rostral middle frontal gyrus, bilateral precentral gyrus and bilateral total frontal cortex; in all these main effects, Abstainers had larger volumes than Relapsers across AP1-AP2 (see Fig. 2 for representative pattern for these regions). Main effects for days abstinent (time) were significant for all regions except the ACC subregions, right caudal middle frontal gyrus, and right precentral gyrus. Simple effects tests indicated that the main effects for days abstinent for the bilateral lateral OFC, bilateral rostral middle frontal gyrus, left precentral gyrus, and bilateral insula were driven by significant volume recovery in Relapsers. (see Fig. 3 for representative pattern for these regions). The main effects for days abstinent for the bilateral superior frontal gyrus was driven by statistically significant volume recovery in Abstainers. Relapsers volume change for the superior frontal gyrus over the AP1-AP2 interval was not significant, but they showed a similar percent change as Abstainers for this region. Greater age was inversely related to volume increases in all regions (p < .01) except bilateral ACC subregions and bilateral insula. Average number of drinks/month over lifetime, years of education, and frequency of psychiatric comorbidities were not significant predictors of volume change for any ROI (see Table 3).
Figure 2.
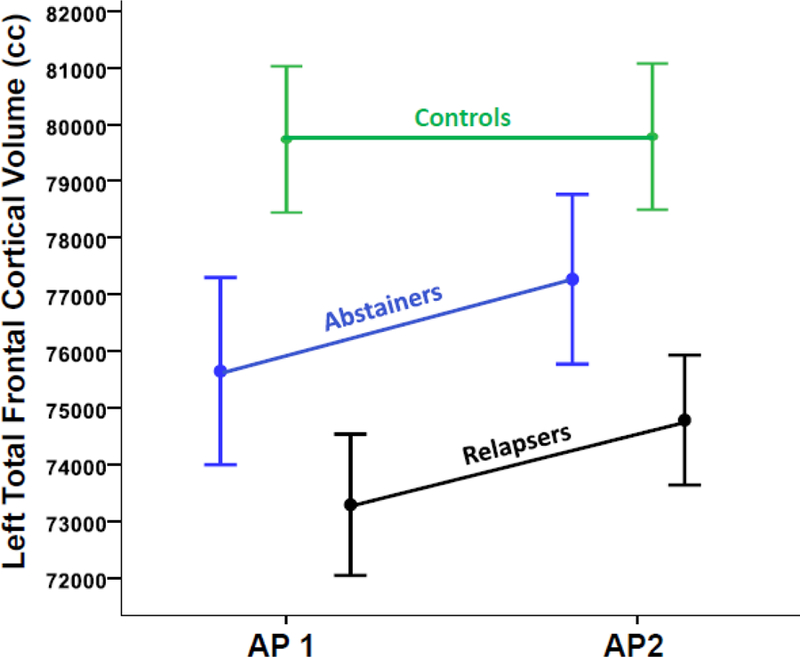
Group Changes in Left Total Frontal Volume Over AP1 and AP2. Note. Group means and error bars are offset for viewability.
Figure 3.
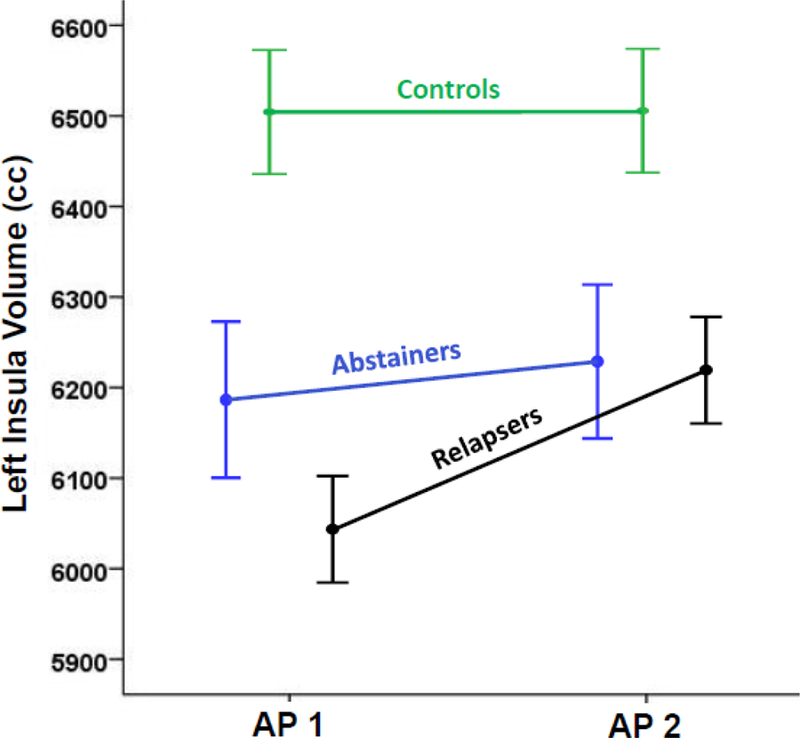
Group Changes in Left Insula Volume Over AP1 and AP2. Note. Group means and error bars are offset for viewability.
Table 3.
Longitudinal Volume Changes for Abstainers and Relapsers
| Region | Hemisphere and subregion | Main Effects | Simple Effects P-values | Volume Percent Change AP1 to AP2 | |||
|---|---|---|---|---|---|---|---|
| Group Main Effect | Days Abstinent (Time) Main Effect | ABS | REL | ABS | REL | ||
| Anterior Cingulate | Left Caudal | NS | NS | .10 | NS | 5.1 | 0.6 |
| Right Caudal | NS | NS | NS | .018 | 3.9 | 1.7 | |
| Left Rostral | F(1, 116) = 4.3, p = .041 | NS | NS | NS | 0.7 | 0.2 | |
| Right Rostral | .060 | NS | NS | NS | 4.5 | 1.5 | |
| Orbitofront al | Left Medial | NS | F(1, 63) = 6.8, p = .012 | .014 | .004 | 2.2 | 3.4 |
| Right Medial | NS | F(1, 63) = 5.5, p = .022 | .060 | NS | 1.7 | −0.3 | |
| Left Lateral | F(1, 116) = 4.8, p = .031 | F(1, 64) = 21.2, p < .001 | NS | <.001 | 0.0 | 0.9 | |
| Right Lateral | .065 | F(1, 64) = 10.7, p = .002 | .09 | .01 | 0.7 | 0.5 | |
| Dorsal Prefrontal | Left Caudal Middle Frontal | NS | F(1, 63) = 9.6, p = .003 | .041 | .013 | 0.8 | 1.8 |
| Right Caudal Middle Frontal | NS | NS | NS | NS | 1.5 | 2.2 | |
| Left Rostral Middle Frontal | .097 | F(1, 63) = 7.8, p = .007 | NS | .017 | 0.9 | 2.2 | |
| Right Rostral Middle Frontal | F(1, 115) = 5.9, p = .017 | F(1, 63) = 5.8, p = .019 | NS | .030 | 0.0 | 0.6 | |
| Left Superior Frontal | .058 | F(1, 64) = 4.4, p = .040 | .017 | NS | 1.2 | 1.0 | |
| Right Superior Frontal | F(1, 115) = 5.0, p = .027 | F(1, 64) = 4.9, p = .030 | .037 | NS | 1.2 | 1.1 | |
| Precentral | Left | F(1, 115) = 5.9, p = .017 | F(1, 64) = 7.0, p = .010 | NS | .10 | 0.1 | 0.8 |
| Right | F(1, 115) = 8.7, p = .004 | .070 | NS | NS | 0.0 | 0.6 | |
| Insula | Left | NS | F(1, 64) = 18.9, p < .001 | NS | <.001 | 0.6 | 2.4 |
| Right | NS | F(1, 64) = 4.9, p < .031 | NS | .057 | 0.2 | 1.7 | |
| Total Frontal Cortical | Left | F(1, 115) = 6.0, p = .015 | F(1, 64) = 13.6, p < .001 | .028 | .008 | 1.0 | 1.0 |
| Right | F(1, 115) = 6.8, p = .010 | F(1, 64) = 10.7, p = .002 | .049 | .014 | 0.6 | 0.7 | |
Note. Full statistics are provided for significant main effects (p < .05) and p-values only for statistical trends for main effects (i.e., p ≤.10); p-values are provided for simple effects. P-values > .10 for any test listed as not significant (NS);
ABS: Abstainers; REL: Relapsers.
Volume comparisons of Controls, Abstainers and Relapsers at AP2 (4 weeks of abstinence)
At approximately 4 weeks of abstinence, Relapsers continued to demonstrate significantly smaller volumes than Controls in the bilateral precentral gyrus, insula and total frontal cortex, left rostral and right caudal ACC, as well as in multiple subregions of the OFC and DPFC (all p ≤ .026); the magnitude of these differences were moderate to strong. Abstainers had significantly smaller volumes than Controls in the left rostral ACC, and bilateral insula (all p ≤ .026), with moderate effect sizes. Relapsers showed smaller volumes than Abstainers in the right caudal ACC, and bilateral superior frontal cortex, precentral gyrus and total frontal cortex (all p ≤ .026), with moderate sizes for these differences. Greater age was associated with smaller volumes in all regions (p < .01) except bilateral ACC subregions and bilateral insula. In comparisons between Abstainers and Relapsers, average number of drinks/month over lifetime, years of education, and frequency of psychiatric comorbidities were not significant predictors of volume for any ROI (see Table 4).
Table 4.
Assessment Point 2 Volumes for Abstainers and Relapsers
| Region | Hemisphere and Subregion | CON (n = 33) | ABS (n = 39) | REL (n = 65) | ES CON vs. ABS | ES CON vs. REL | ES ABS vs. REL |
|---|---|---|---|---|---|---|---|
| Anterior Cingulate | Left Caudal | 1923 (454) | 1845 (460) | 1833 (456) | 0.17 | 0.20 | 0.03 |
| Right Caudal | 2214 (408) | 2182(405) | 2017 (402)$, & | 0.08 | 0.49 | 0.41 | |
| Left Rostral | 2546 (349) | 2345 (358)# | 2224 (355)$ | 0.57 | 0.90 | 0.34 | |
| Right Rostral | 1841 (345) | 1864 (340) | 1752 (438) | 0.07 | 0.23 | 0.29 | |
| Orbitofrontal | Left Medial | 4540 (552) | 4449 (629) | 4438 (629) | 0.15 | 0.16 | 0.02 |
| Right Medial | 5093 (641) | 4757 (636) | 4607 (637)$ | 0.53 | 0.76 | 0.24 | |
| Left Lateral | 9746 (854) | 9456 (917) | 9075 (910)$ | 0.33 | 0.73 | 0.42 | |
| Right Lateral | 9881 (835) | 9632 (880) | 9316 (873)$ | 0.29 | 0.65 | 0.36 | |
| Dorsal Prefrontal | Left Caudal Middle Frontal | 6598 (1216) | 6140 (1069) | 6069 (1070) | 0.45 | 0.50 | 0.07 |
| Right Caudal Middle Frontal | 5967 (1050) | 5995 (1021) | 5655 (1147) | 0.03 | 0.29 | 0.31 | |
| Left Rostral Middle Frontal | 15382 (1964) | 14872 (1975) | 14194 (1977)$ | 0.26 | 0.60 | 0.34 | |
| Right Rostral Middle Frontal | 16386 (2071) | 15440 (1905) | 14628 (1906)$ | 0.48 | 0.92 | 0.43 | |
| Left Superior Frontal | 22238 (1899) | 21499 (2003) | 20453 (2004)$, & | 0.38 | 0.89 | 0.52 | |
| Right Superior Frontal | 21353 (1956) | 20948 (1993) | 19959 (1995)$, & | 0.21 | 0.70 | 0.50 | |
| Precentral | Left | 12489 (1183) | 12671 (1156) | 11893 (1225)$, & | 0.15 | 0.50 | 0.65 |
| Right | 12742 (1149) | 12865 (1230) | 11935 (1157)$, & | 0.06 | 0.68 | 0.78 | |
| Insula | Left | 6543 (458) | 6219 (473)# | 6206 (470)$ | 0.70 | 0.72 | 0.03 |
| Right | 6507 (455) | 6156 (470)# | 6149 (467)$ | 0.76 | 0.76 | 0.01 | |
| Total Frontal Cortical | Left | 80291 (5186) | 77420 (5286) | 74636 (5290)$, & | 0.55 | 1.07 | 0.53 |
| Right | 80259 (5516) | 77762 (5528) | 74550 (5532)$, & | 0.45 | 1.03 | 0.58 |
Note. Mean (SD); ABS: Abstainers; CON: Non-smoking Light Drinking Controls; ES: Effect size; REL: Relapsers;
CON > ABS, p < .026;
CON > REL, p < .026;
ABS > REL, p < .026.
Associations between regional brain volume changes and duration of post-treatment abstinence in Relapsers
Relapsers maintained sobriety for 137 ± 80 days after treatment. In Relapsers, increasing volumes over the AP1-AP2 interval in the following regions were positively related to longer duration of sobriety after treatment: left lateral OFC [β = .022, standard error of the estimate (SE) = .006; F(1, 103) = 12.3, p = .001], right lateral OFC [β = .023, SE = .007; F(1, 103) = 16.5, p < .001], right precentral gyrus [β = .012, SE = .004; F(1, 103) = 6.5, p = .012], left insula [β = .036, SE = .012; F(1, 103) = 9.3, p = .003], right insula [β = .035, SE = .012; F(1, 103) = 9.1, p = .003], left caudal middle frontal [β = .015, SE = .005; F(1, 103) = 7.3, p = .005], total left frontal [β = .023, SE = .012; F(1, 101) = 6.8, p = .010], and total right frontal [β = .020, SE = .010; F(1, 101) = 6.2, p = .015].
DISCUSSION
The primary findings from this predominately Caucasian, male, Veteran cohort were: 1) At approximately 1 week of sobriety (AP1), Relapsers exhibited smaller volumes than Controls in 15 of 20 ROIs, while Abstainers had smaller volumes than Controls in only 5 of 20 ROIs investigated. Relapsers showed smaller volumes than Abstainers in the left lateral OFC, right superior frontal gyrus, and bilateral precentral gyrus and total frontal cortex. 2) Over the AP1-AP2 interval, Abstainers demonstrated significant volume recovery in the left medial OFC, bilateral superior frontal gyri and total frontal cortex. Relapsers showed significant volume increases in the left medial OFC, left insula and bilateral lateral OFC, rostral middle frontal gyri and total frontal cortex. 3) At approximately 4 weeks of sobriety (AP2), Relapsers continued to demonstrate smaller volumes than Controls in the same 15 of 20 regions apparent at AP1. Abstainers continued to show smaller volumes than Controls only in the left rostral ACC and bilateral insula. Relapsers exhibited smaller volumes than Abstainers in the right caudal ACC, bilateral superior frontal gyri, and bilateral precentral gyri and total frontal cortex at AP2; importantly, these volume differences were not explained by demographic, clinical or alcohol consumption variables. 4) In Relapsers, greater volume increases in multiple frontal cortical subregions and the insula over the AP1-AP2 interval were related to longer duration of abstinence after treatment.
Although our longitudinal analyses did not reveal a significant group x days abstinent interaction for any ROI, Abstainers and Relapsers did exhibit a different pattern of recovery for most ROIs over the AP1-AP2 interval. Relapsers had significant volume increases in 10 ROIs, whereas Abstainers showed recovery in only 6 ROIs. The left medial OFC, left caudal middle frontal cortex and bilateral total frontal cortex were the only ROIs where both Abstainers and Relapsers showed significant volume increases over the AP1-AP2 interval. Despite the significant volume increases in Relapsers for multiple ROIs over the AP1-AP2 interval, at AP2, they continued to demonstrate significantly smaller volumes than Controls and Abstainers in the same ROIs as AP1. At AP2, Abstainers only continued to show smaller volumes than Controls in the left rostral ACC and bilateral insula. At both AP1 and AP2, in all ROIs where Abstainers had smaller volumes than Controls, Relapsers also demonstrated smaller volumes than Controls.
The structural integrity of components of circuits subserving fundamental aspects of executive functions, assignment of external and internal stimulus salience, and emotional/mood regulation (Seeley et al., 2007; Volkow & Baler, 2014; Williams, 2016), as assessed by volumetric voxel-wise and ROI analyses, has been repeatedly shown to relate to treatment outcome [see (Durazzo & Meyerhoff, 2017; D. Seo & Sinha, 2015) and references therein]. Correspondingly, dysfunction in executive skills, impulse control, and assignment of stimulus salience and mood disorders are associated with relapse in AUD (Bates, Buckman, & Nguyen, 2013; Durazzo & Meyerhoff, 2017; D. Seo & Sinha, 2014; S. Seo et al., 2015). Relapsers demonstrated significant volume deficits, throughout the initial month of sobriety, in multiple regions that are cortical nodes in the above circuits. Alternately, at both AP1 and AP2, Abstainers showed smaller volumes than Controls in only a few of these cortical nodes. The results from AP1 cross-sectional comparisons indicate that Relapsers entered treatment with markedly greater structural injury than Abstainers in multiple subregions of the ACC, OFC, DPFC as well as across the left and right total frontal cortex. The significant volume increases in 10 ROIs in Relapsers suggest adaptive plasticity in those regions, despite continuing to exhibit significant volume deficits at AP2. The exact processes and mechanisms contributing to the disparate cross-sectional and longitudinal volumetric results for Abstainers and Relapsers are unclear. The findings for Abstainers and Relapsers were not attributable to age, level of lifetime alcohol consumption, education, cigarette smokers, use of anti-craving medications or psychiatric comorbidities. However, the cross-sectional and longitudinal results for Abstainers and Relapsers may be related to potential differences in premorbid factors [e.g., polymorphisms in neurotrophic factors, genetic and/or other vulnerability for hazardous alcohol consumption (Mon et al., 2013; Tessner & Hill, 2010)], or comorbid factors (e.g., diet/nutrition, exercise, social environment, subclinical pulmonary, hepatic, cardiac, or cerebrovascular dysfunction) not specifically assessed in this report, and clearly warrant consideration in future studies.
The findings may have implications for rTMS and potentially other non-invasive neurostimulation methods. The safe and effective application of rTMS-induced brain stimulation necessitates consistent and accurate regulation of the magnitude of stimulation of the target tissue. To titrate the magnitude of stimulation for the individual, rTMS output is typically adjusted to an observable physiological measure of cortical activity, such as evoked motor response of the thumb following excitation of the contralateral primary motor cortex (George, 2007). For rTMS, the distance from the stimulation coil (placed adjacent to scalp) to the cortex influences the level of stimulation of the underlying tissue (Stokes et al., 2005). Adjustment of stimulation magnitude to the target site based on the distance of the coil from the primary motor cortex (precentral gyrus) to the target site are recommended for optimizing rTMS treatment (Stokes et al., 2007). The left dorsolateral prefrontal cortex was a common stimulation target of previous rTMS studies in AUD. At both AP1 and AP2, Relapsers and Abstainers showed disparate levels of volume loss of the left precentral gyrus and DPFC. Abstainers had numerically larger left precentral gyrus volumes at both AP1 and AP2, and averaged 4.6 percent smaller DPFC volume over the AP1-AP2 interval than Controls; Relapsers averaged 5.5 percent smaller left precentral gyrus volumes and 9.4 percent smaller DPFC volume than Controls over the AP1-AP2 interval. Considering the level of atrophy in Abstainers and Relapsers in the foregoing regions will influence length from the skull to the cortical surface, distance adjusted stimulation output for a dorsolateral anterior frontal target may have been required for proper calibration of rTMS output intensity in this sample.
In Relapsers, greater increases in the left caudal middle frontal gyrus, right precentral gyrus and bilateral insula, lateral OFC and total frontal cortex were related to longer duration of abstinence after treatment. Over the AP1-AP2 interval, Relapsers showed significant volume increases in most of these regions with the greatest increases in the bilateral insula. The lateral OFC is implicated in switching between habitual behavior and goal-directed behavior following evaluation consequences as well as reward identification and acquisition (Moorman, 2018; Rolls & Grabenhorst, 2008) and the collective components of the insula are key neural substrates involved in modulating drive and craving-related aspects of reward processing (Paulus, 2007). A variety of neurobiological abnormalities, reflecting adverse neuroplastic and functional changes of the insula, lateral OFC and dorsolateral prefrontal cortex, are related to the persistence of the relapse-remit cycle in AUD (Durazzo et al., 2011; Meyerhoff, Durazzo, & Ende, 2013; Paulus, 2007; Volkow, Wang, Tomasi, & Baler, 2013). It is noteworthy that Abstainers did not differ from Controls on any of the OFC, DPFC subregions or left and right total frontal cortex volumes at AP2. Therefore, promoting adaptive plasticity in components of the OFC, insula, dorsolateral prefrontal cortex, and/or the total frontal cortex during early recovery, potentially through rTMS, other neurostimulation techniques (Bellamoli et al., 2014; Dunlop et al., 2017; Fettes et al., 2017), and/or nutrition and exercise may decrease the risk of relapse in AUD.
This study has limitations that may affect the generalizability of the results. We observed no statistically significant interactions for longitudinal analyses comparing Abstainers and Relapsers over approximately 1 month of sobriety, despite simple effects tests demonstrating different levels of volume recovery for Abstainers and Relapsers in multiple regions. This may indicate we did not have sufficient power and/or within-group variance was too high to yield statistically significant interactions. There is no universally accepted definition of relapse in AUD (Witkiewitz & Marlatt, 2007); therefore, our operationalization of relapse - any alcohol consumption within 12 months of initial assessment - may not be congruent with criteria employed in other studies. Limitations also include the reliance on self-report and/or medical records for the determination of drinking status at post-treatment in most participants, and the inability to examine sex effects because of the small number of females. It is imperative to include comparable number of females in future research to investigate the potential influence of sex. Given both our previous volumetric work and focus on common cortical rTMS targets in AUD, we confined our analyses to frontal and insula volumes; however, it is possible that volume changes in other cortical or subcortical regions are also associated with relapse in this sample.
In conclusion, the persistent regional and total frontal GM volume deficits observed over 4 weeks from last alcohol use in future Relapsers, combined with the volumetric findings from previous cross-sectional studies, may define an neuroimaging endophenotype that differentiates those who respond more favorably to typical psychosocial and pharmacological interventions provided for AUD. Interventions that promote adaptive neuroplasticity during early recovery in the cortical regions investigated in this study may improve long-term outcomes in those seeking treatment for AUD.
ACKNOWLEDGMENT
This study was supported by National Institutes of Health (AA10788 to DJM and DA24136 to TCD) and Department of Veterans Affairs (RX002303 to TCD) with resources and use of facilities at the San Francisco VA Medical Center and the VA Palo Alto Health Care System. We thank Dr. Ellen Herbst, Ricky Chen and colleagues of the Veterans Administration Substance Abuse Day Hospital and Dr. David Pating and colleagues at the Kaiser Permanente Chemical Dependency Recovery Program in San Francisco for their valuable assistance in participant recruitment. We thank Drs. Stefan Gazdzinski and Anderson Mon for MRI data acquisition, Dr. Xiaowei Zou for longitudinal FreeSurfer data processing, and Mr. Thomas Schmidt for assistance with psychiatric assessments and cohort maintenance. We also wish to extend our gratitude to our participants, who made this research possible.
Funding: National Institutes of Health (AA10788 to Dieter J. Meyerhoff and DA24136 to Timothy C. Durazzo) and Department of Veterans Affairs (RX002303 to Timothy C. Durazzo) with resources and use of facilities at the San Francisco VA Medical Center and the VA Palo Alto Health Care System.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest: The Authors received funding from the National Institutes and Department of Veterans Affairs. The Authors have no conflicts of interest to report.
COMPLICANCE WITH ETHICAL STANDARDS
Ethical approval: All procedures performed in this study involving human participants were in accordance with the ethical standards of institutional review boards of the University of California San Francisco and the San Francisco VA Medical Center and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Written informed consent was obtained from all individual participants included in the study prior to involvement in any research-related procedures.
REFERENCES
- Bates ME, Buckman JF, & Nguyen TT (2013). A role for cognitive rehabilitation in increasing the effectiveness of treatment for alcohol use disorders. Neuropsychol Rev, 23(1), 27–47. doi: 10.1007/s11065-013-9228-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A, Wustenberg T, Genauck A, Wrase J, Schlagenhauf F, Smolka MN, … Heinz A (2012). Effect of brain structure, brain function, and brain connectivity on relapse in alcohol-dependent patients. Arch Gen Psychiatry, 69(8), 842–852. doi: 10.1001/archgenpsychiatry.2011.2026 [DOI] [PubMed] [Google Scholar]
- Bellamoli E, Manganotti P, Schwartz RP, Rimondo C, Gomma M, & Serpelloni G (2014). rTMS in the treatment of drug addiction: an update about human studies. Behav Neurol, 2014, 815215. doi: 10.1155/2014/815215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhler M, & Mann K (2011). Alcohol and the human brain: a systematic review of different neuroimaging methods. Alcohol Clin Exp Res, 35(10), 1771–1793. doi: 10.1111/j.1530-0277.2011.01540.x [DOI] [PubMed] [Google Scholar]
- Cardenas VA, Durazzo TC, Gazdzinski S, Mon A, Studholme C, & Meyerhoff DJ (2011). Brain Morphology at Entry into Treatment for Alcohol Dependence Is Related to Relapse Propensity. Biol Psychiatry, 70(6), 561–567. doi:S0006-3223(11)00377-5 [pii] 10.1016/j.biopsych.2011.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1977). Statistical power analysis for the behavioral sciences (rev. ed.) New York: Academic Press. [Google Scholar]
- Dunlop K, Hanlon CA, & Downar J (2017). Noninvasive brain stimulation treatments for addiction and major depression. Ann N Y Acad Sci, 1394(1), 31–54. doi: 10.1111/nyas.12985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durazzo TC, Gazdzinski S, Yeh PH, & Meyerhoff DJ (2008). Combined neuroimaging, neurocognitive and psychiatric factors to predict alcohol consumption following treatment for alcohol dependence. Alcohol and Alcoholism, 43(6), 683–691. doi:agn078 [pii] 10.1093/alcalc/agn078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durazzo TC, & Meyerhoff DJ (2017). Psychiatric, Demographic, and Brain Morphological Predictors of Relapse After Treatment for an Alcohol Use Disorder. Alcohol Clin Exp Res, 41(1), 107–116. doi: 10.1111/acer.13267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durazzo TC, Mon A, Gazdzinski S, & Meyerhoff DJ (2016). Regional brain volume changes in alcohol-dependent individuals during early abstinence: associations with relapse following treatment. Addict Biol doi: 10.1111/adb.12420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durazzo TC, Mon A, Gazdzinski S, Yeh PH, & Meyerhoff DJ (2015). Serial longitudinal magnetic resonance imaging data indicate non-linear regional gray matter volume recovery in abstinent alcohol-dependent individuals. Addict Biol, 20(5), 956–967. doi: 10.1111/adb.12180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durazzo TC, Mon A, Pennington D, Abe C, Gazdzinski S, & Meyerhoff DJ (2014). Interactive effects of chronic cigarette smoking and age on brain volumes in controls and alcohol-dependent individuals in early abstinence. Addict Biol, 19(1), 132–143. doi: 10.1111/j.1369-1600.2012.00492.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durazzo TC, Tosun D, Buckley S, Gazdzinski S, Mon A, Fryer SL, & Meyerhoff DJ (2011). Cortical thickness, surface area, and volume of the brain reward system in alcohol dependence: relationships to relapse and extended abstinence. Alcohol Clin Exp Res, 35(6), 1187–1200. doi: 10.1111/j.1530-0277.2011.01452.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fettes P, Schulze L, & Downar J (2017). Cortico-Striatal-Thalamic Loop Circuits of the Orbitofrontal Cortex: Promising Therapeutic Targets in Psychiatric Illness. Front Syst Neurosci, 11, 25. doi: 10.3389/fnsys.2017.00025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- George MS, Bohning DE, Lorberbaum JP, Nahas Z, Anderson B, Borckardt JJ, Molnar C, Kose S, Ricci R, Rostogi K (2007). Overview of transcranial magnetic stimulation: history mechanisms physics and safety. In George MS, Belmaker RH (Ed.), Transcranial magnetic stimulation in clinical psychiatry (pp. 1–38). Washington, DC; London, England: American Psychiatric Publishing, Inc. [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, … Hasin DS (2015). Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry, 72(8), 757–766. doi: 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens JR, Weisner C, Ray GT, Fireman B, & Walsh K (2005). Hazardous drinkers and drug users in HMO primary care: prevalence, medical conditions, and costs. Alcohol Clin Exp Res, 29(6), 989–998. [DOI] [PubMed] [Google Scholar]
- Meyerhoff DJ, Durazzo TC, & Ende G (2013). Chronic alcohol consumption, abstinence and relapse: brain proton magnetic resonance spectroscopy studies in animals and humans. Curr Top Behav Neurosci, 13, 511–540. doi: 10.1007/7854_2011_131 [DOI] [PubMed] [Google Scholar]
- Mon A, Durazzo TC, Gazdzinski S, Hutchison KE, Pennington D, & Meyerhoff DJ (2013). Brain-derived Neurotrophic Factor (BDNF) Genotype is Associated with Lobar Gray and White Matter Volume Recovery in Abstinent Alcohol Dependent Individuals. Genes Brain Behav, 12(1), 98–107. doi: 10.1111/j.1601-183X.2012.00854.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorman DE (2018). The role of the orbitofrontal cortex in alcohol use, abuse, and dependence. Prog Neuropsychopharmacol Biol Psychiatry, 87(Pt A), 85–107. doi: 10.1016/j.pnpbp.2018.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulus MP (2007). Neural basis of reward and craving--a homeostatic point of view. Dialogues Clin Neurosci, 9(4), 379–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennington DL, Durazzo TC, Schmidt T, Mon A, Abe C, & Meyerhoff DJ (2013). The Effects of Chronic Cigarette Smoking on Cognitive Recovery during Early Abstinence from Alcohol. Alc Clin Exp Research, 37(7), 1220–1227. doi: 10.1111/acer.12089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rando K, Hong KI, Bhagwagar Z, Li CS, Bergquist K, Guarnaccia J, & Sinha R (2011). Association of frontal and posterior cortical gray matter volume with time to alcohol relapse: a prospective study. Am J Psychiatry, 168(2), 183–192. doi:appi.ajp.2010.10020233 [pii] 10.1176/appi.ajp.2010.10020233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuter M, Schmansky NJ, Rosas HD, & Fischl B (2012). Within-subject template estimation for unbiased longitudinal image analysis. Neuroimage, 61(4), 1402–1418. doi: 10.1016/j.neuroimage.2012.02.084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolls ET, & Grabenhorst F (2008). The orbitofrontal cortex and beyond: from affect to decision-making. Prog Neurobiol, 86(3), 216–244. doi:S0301-0082(08)00098-1 [pii] 10.1016/j.pneurobio.2008.09.001 [DOI] [PubMed] [Google Scholar]
- Salling MC, & Martinez D (2016). Brain Stimulation in Addiction. Neuropsychopharmacology, 41(12), 2798–2809. doi: 10.1038/npp.2016.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankoh AJ, Huque MF, & Dubey SD. (1997). Some comments on frequently used multiple endpoint adjustment methods in clinical trials. Statistics in Medicine, 16(22). [DOI] [PubMed] [Google Scholar]
- Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, … Greicius MD (2007). Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci, 27(9), 2349–2356. doi: 10.1523/jneurosci.5587-06.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo D, & Sinha R (2014). The neurobiology of alcohol craving and relapse. Handb Clin Neurol, 125, 355–368. doi: 10.1016/b978-0-444-62619-6.00021-5 [DOI] [PubMed] [Google Scholar]
- Seo D, & Sinha R (2015). Neuroplasticity and Predictors of Alcohol Recovery. Alcohol Res, 37(1), 143–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo S, Mohr J, Beck A, Wustenberg T, Heinz A, & Obermayer K (2015). Predicting the future relapse of alcohol-dependent patients from structural and functional brain images. Addict Biol, 20(6), 1042–1055. doi: 10.1111/adb.12302 [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Riley DM, Schuller R, Pavan DS, Cancilla A, … Leo GI (1988). The reliability of alcohol abusers’ self-reports of drinking and life events that occurred in the distant past. J Stud Alcohol, 49(3), 225–232. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Maisto SA, & Cooper AM. (1985). Time-line follow-back assessment method. NIAAA treatment handbook series, 2, 85–1380. [Google Scholar]
- Stokes MG, Chambers CD, Gould IC, English T, McNaught E, McDonald O, & Mattingley JB (2007). Distance-adjusted motor threshold for transcranial magnetic stimulation. Clin Neurophysiol, 118(7), 1617–1625. doi: 10.1016/j.clinph.2007.04.004 [DOI] [PubMed] [Google Scholar]
- Stokes MG, Chambers CD, Gould IC, Henderson TR, Janko NE, Allen NB, & Mattingley JB (2005). Simple metric for scaling motor threshold based on scalp-cortex distance: application to studies using transcranial magnetic stimulation. J Neurophysiol, 94(6), 4520–4527. doi: 10.1152/jn.00067.2005 [DOI] [PubMed] [Google Scholar]
- Tessner KD, & Hill SY (2010). Neural circuitry associated with risk for alcohol use disorders. Neuropsychol Rev, 20(1), 1–20. doi: 10.1007/s11065-009-9111-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, & Baler RD (2014). Addiction science: Uncovering neurobiological complexity. Neuropharmacology, 76 Pt B, 235–249. doi: 10.1016/j.neuropharm.2013.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Tomasi D, & Baler RD (2013). Unbalanced neuronal circuits in addiction. Curr Opin Neurobiol, 23(4), 639–648. doi: 10.1016/j.conb.2013.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LM (2016). Precision psychiatry: a neural circuit taxonomy for depression and anxiety. Lancet Psychiatry, 3(5), 472–480. doi: 10.1016/s2215-0366(15)00579-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K (2011). Predictors of heavy drinking during and following treatment. Psychol Addict Behav, 25(3), 426–438. doi: 10.1037/a0022889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, & Marlatt GA (2007). Modeling the complexity of post-treatment drinking: it’s a rocky road to relapse. Clin Psychol Rev, 27(6), 724–738. doi:S0272-7358(07)00006-2 [pii] 10.1016/j.cpr.2007.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]


