Abstract
Background
Current trends in serum lipid levels among children are likely to be important predictors of future cardiovascular disease prevalence. However, no studies have examined trends in low-density lipoprotein cholesterol (LDL-C) levels in Japanese children.
Methods
We investigated trends in LDL-C levels from 2008 through 2017 and HDL-C levels from 2007 through 2017 in a population of 10- and 13-year-old children in Fukuroi City, Japan. We analyzed 17,838 children, accounting for 93.8% of all fifth and eighth graders in the entire city. Adverse lipid levels were defined as follows: 130 mg/dL or higher for LDL-C, and lower than 40 mg/dL for HDL-C. The Jonckheere-Terpstra and Cochran-Armitage tests were used to evaluate secular trends in mean serum lipid levels and prevalence of dyslipidemia, respectively.
Results
There were no significant trends in BMI during the study period. In children aged 10 years, serum levels of LDL-C and HDL-C showed significant positive associations with calendar year during the study period for both sexes. A significant increase in HDL-C levels was observed in girls aged 13 years. On the other hand, no significant trends were observed in the prevalence of high LDL-C or low HDL-C regardless of sex or age, while the prevalence of high non-HDL-C showed a significant increase in boys.
Conclusions
In the Fukuroi population, serum levels of LDL-C and HDL-C slightly increased in both boys and girls aged 10 years, and HDL-C levels slightly increased in girls aged 13 years, during the past decade.
Key words: child, cholesterol, epidemiology, lipoproteins
INTRODUCTION
Elevated low-density lipoprotein cholesterol (LDL-C) has been shown to be a major cause of coronary heart disease in epidemiological studies, as well as in animal and laboratory experiments.1 Carotid arterial wall atherosclerosis rapidly progresses during childhood in individuals with familial hypercholesterolemia, which is characterized by elevated LDL-C.2 It is widely acknowledged that children initially identified as having elevated levels of serum cholesterol tend to have elevated follow-up levels (in studies tracking childhood to adulthood).3–8 Adverse LDL-C levels in childhood persist over time, progressing to dyslipidemia in adulthood.8 A population-based, prospective cohort study conducted in Finland showed an association between adult carotid artery intima-media thickness (IMT) and childhood LDL-C levels.9 A cohort study of a semirural black and white community in Bogalusa, Louisiana, United States also demonstrated that childhood LDL-C levels predict carotid IMT in young adults.10 Moreover, intimal atherosclerotic lesions reportedly appeared in the aortas and coronary arteries of adolescent individuals who died of external causes and underwent autopsy.11 In Japan, a nationwide autopsy study of atherosclerosis in infants, children, and young adults found that atherosclerotic lesions undergo substantial developments in extent and prevalence between 10 and 39 years of age.12,13 Thus, the influence of risk factors in early life may contribute to the development of future cardiovascular disease.9 The Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents strongly recommends a universal lipid screening in 9- to 11-year-old children to prevent future cardiovascular disease.14 Current trends in childhood cholesterol levels might predict subsequent cardiovascular disease trends in adults.
In the United States, beneficial trends in serum lipid concentrations were reportedly observed among youths between 1988–1994 and 2007–2010, while adverse lipid profiles persisted.15 Adverse trends in serum lipid concentrations were also reported among Chinese children during a period from 2004 to 2014.16 In Japan, nationwide surveys on serum total cholesterol (T-C) were conducted in 1960, 1970, 1980, and 1990, revealing a yearly increase in T-C concentration among 10- to 19-year-old males and females.17 However, since T-C concentration reflects both levels of LDL-C and high-density lipoprotein cholesterol (HDL-C), which is known as good cholesterol,18 studies that directly evaluate secular trends in LDL-C and HDL-C levels among children are warranted. We recently reported that there were no significant trends in T-C, non-HDL-C, and HDL-C levels in a 10-year-old population in Iwata City, Shizuoka, Japan from 1993 to 2008.19 Since that study was conducted, there have been no reports on serum lipid trends in Japanese children. Moreover, no previous study has examined secular trends in LDL-C among Japanese schoolchildren. Accordingly, the present study aimed to provide the most up-to-date data regarding serum lipid levels in children and investigated secular trends in LDL-C levels from 2008 through 2017 and HDL-C levels from 2007 through 2017 in a 10- and 13-year-old population in Fukuroi City, Shizuoka, Japan.
METHODS
Study population
Fukuroi City, in Shizuoka Prefecture, Japan, is located at 135 degrees east longitude and 34 degrees north latitude, roughly 240 km away from Tokyo and 320 km from Osaka, and covers an area of 108 km2. Fukuroi City is adjacent to Iwata City, where the trends in serum T-C from 1993 to 200120 and HDL-C from 1993 to 200819 were previously reported. Fukuroi City had a population of 87,174 as of April 2016. Land use consisted of 17.2% residential, 36.2% agricultural, and 19.5% mountainous woodlands in 2011. Approximately 4% of the labor force is engaged in primary industries, while 40% and 53% are engaged in secondary and tertiary industries, respectively. Both commerce and industry in the city have developed proportionately with the development of transport lines, such as National Route 1, Tomei expressway, Tokaido Shinkansen Line, and Tokaido Main Line.
Fukuroi City has 12 municipal elementary schools, 4 municipal junior high schools, and no private schools. Almost all children living in the city are enrolled in municipal schools. There were 19,008 fifth and eighth grade children who attended municipal schools from 2007 through 2017. The Fukuroi Board of Education conducts health screening including anthropometry measurements and blood tests for all fifth and eighth graders during April through June every year. The source population of the present study comprised 19,008 children; of these, 17,838 who participated in health examinations from 2007 through 2017 were included in the analysis. The present study protocol was approved by the Ethics Committee of the Kindai University Faculty of Medicine. This study was conducted in accordance with the ethical principles of the Declaration of Helsinki.
Examinations
Anthropometric variables were measured in each school during April through June each year by Yogo teachers who have a Japan national health education license. Measurements were conducted in accordance with the Japanese School Health and Safety Act to ensure uniform quality control. Height was measured to an accuracy of 0.1 cm, and body weight to 0.1 kg.21 Body mass index (BMI; kg/m2) was calculated as body weight (kg) divided by height squared (m2). To determine overweight subjects, cut-offs of BMI based on an adult BMI of 25 kg/m2 were calculated using the standardized centile curves of BMI for Japanese children.22 Cut-offs for boys and girls aged 10 years were >20.04 kg/m2 and >20.97 kg/m2, respectively, and those for boys and girls aged 13 years were >23.26 kg/m2 and >23.89 kg/m2, respectively. Similarly, cut-offs of BMI based on an adult BMI of 18.5 kg/m2 were calculated to determine underweight subjects. Cut-offs for boys and girls aged 10 years were <14.57 kg/m2 and <14.39 kg/m2, respectively, and those for underweight boys and girls aged 13 years were <16.52 kg/m2 and <16.17 kg/m2, respectively.
Non-fasting blood samples were collected by nurses and medical technologists who were staff members of the Shizuokaken Yoboigakukyokai (the Shizuoka Prefecture Preventive Medicine Association, Shizuoka, Japan) in each school during April through June each year. LDL-C and HDL-C levels were measured using the direct method with commercial assays (Cholestest LDL and Cholestest N HDL, Sekisui Medical Co. Ltd., Tokyo, Japan, from 2007 through 2010; Determiner L LDL-C and MetaboLead HDL-C, Kyowa Medex Co. Ltd., Tokyo, Japan, from 2011 to 2017). Intra- and inter-laboratory coefficients of variation were less than 4% throughout the study period (2007–2017). Cut-offs for high LDL-C and low HDL-C were defined according to the 2011 Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents as follows: high LDL-C, ≥130 mg/dL; high non-HDL-C, ≥145 mg/dL; and low HDL-C, <40 mg/dL.14
Statistical analysis
Statistical analysis was performed with SAS software for Windows ver. 9.4 (SAS Institute Inc., Cary, NC, USA). The Jonckheere-Terpstra test was used to evaluate secular trends in anthropometric variables and levels of serum lipids during the study period. The explanatory variable was the calendar year of health examination. Dependent variables were individual measurements of height, body weight, BMI, LDL-C, non-HDL-C, HDL-C, T-C, and the ratio of LDL-C to HDL-C. In addition, the Cochran-Armitage test was used to evaluate secular trends in prevalence of overweight, underweight, high LDL-C, high non-HDL-C, and low HDL-C. Since differences in serum lipid levels are known to be associated with age and sex,23 sex- and age-specific evaluations were performed in each regression model. P < 0.05 was considered statistically significant.
RESULTS
Table 1 shows anthropometric variables over the period from 2007 through 2017. Although height and weight in girls aged 10 years showed significant increases, there were no significant trends in BMI in both boys and girls aged 10 and 13 years during the study period. No significant trends were observed in the prevalence of overweight in both boys and girls aged 10 and 13 years during the study period, while a significant decrease was observed in girls aged 10 years who were judged to be underweight (Table 2).
Table 1. Secular trends in anthropometric measurements.
| Number of children |
Height | Weight | BMI | Number of children |
Height | Weight | BMI | |||||||||||||
| Percentiles | Percentiles | |||||||||||||||||||
| 5th | 50th | 95th | 5th | 50th | 95th | 5th | 50th | 95th | 5th | 50th | 95th | 5th | 50th | 95th | 5th | 50th | 95th | |||
| Boys at age 10 | Girls at age 10 | |||||||||||||||||||
| 2007 | 387 | 128 | 138 | 149 | 25 | 32 | 45 | 14 | 17 | 23 | 400 | 127 | 138 | 150 | 24 | 32 | 44 | 14 | 16 | 21 |
| 2008 | 430 | 129 | 138 | 149 | 25 | 32 | 47 | 14 | 17 | 23 | 391 | 129 | 138 | 150 | 25 | 32 | 45 | 14 | 17 | 22 |
| 2009 | 452 | 129 | 138 | 149 | 25 | 32 | 47 | 14 | 17 | 23 | 380 | 129 | 139 | 150 | 25 | 32 | 46 | 14 | 17 | 22 |
| 2010 | 419 | 129 | 138 | 148 | 26 | 32 | 45 | 14 | 17 | 23 | 432 | 128 | 139 | 150 | 24 | 32 | 45 | 14 | 17 | 21 |
| 2011 | 461 | 129 | 138 | 146 | 26 | 31 | 47 | 14 | 17 | 23 | 395 | 128 | 139 | 150 | 25 | 32 | 46 | 14 | 17 | 22 |
| 2012 | 423 | 128 | 138 | 148 | 26 | 32 | 47 | 15 | 17 | 23 | 420 | 128 | 139 | 151 | 25 | 32 | 46 | 14 | 17 | 21 |
| 2013 | 434 | 127 | 138 | 148 | 25 | 32 | 50 | 14 | 17 | 23 | 410 | 129 | 139 | 150 | 25 | 32 | 46 | 14 | 17 | 22 |
| 2014 | 435 | 128 | 139 | 149 | 25 | 32 | 46 | 14 | 17 | 23 | 434 | 128 | 139 | 151 | 25 | 32 | 46 | 14 | 17 | 21 |
| 2015 | 442 | 130 | 138 | 148 | 26 | 32 | 48 | 15 | 17 | 23 | 420 | 128 | 139 | 150 | 25 | 32 | 44 | 14 | 17 | 21 |
| 2016 | 430 | 128 | 138 | 148 | 25 | 32 | 47 | 14 | 17 | 23 | 395 | 128 | 139 | 152 | 25 | 32 | 49 | 14 | 17 | 22 |
| 2017 | 502 | 128 | 138 | 149 | 25 | 33 | 49 | 14 | 17 | 24 | 412 | 129 | 140 | 152 | 25 | 33 | 47 | 14 | 17 | 22 |
| P for trend | 0.324 | 0.120 | 0.143 | 0.005 | 0.029 | 0.216 | ||||||||||||||
| Boys at age 13 | Girls at age 13 | |||||||||||||||||||
| 2007 | 395 | 145 | 160 | 171 | 35 | 47 | 70 | 16 | 18 | 26 | 373 | 145 | 155 | 163 | 37 | 46 | 60 | 16 | 19 | 24 |
| 2008 | 382 | 146 | 160 | 171 | 35 | 47 | 65 | 16 | 18 | 24 | 346 | 146 | 155 | 163 | 37 | 46 | 60 | 16 | 19 | 25 |
| 2009 | 389 | 145 | 159 | 170 | 35 | 47 | 66 | 16 | 19 | 25 | 360 | 146 | 154 | 162 | 37 | 46 | 58 | 16 | 19 | 24 |
| 2010 | 360 | 145 | 160 | 171 | 35 | 48 | 65 | 16 | 18 | 23 | 387 | 145 | 154 | 163 | 35 | 46 | 58 | 16 | 19 | 24 |
| 2011 | 406 | 146 | 159 | 171 | 35 | 47 | 63 | 16 | 18 | 23 | 372 | 145 | 153 | 163 | 37 | 46 | 59 | 16 | 19 | 24 |
| 2012 | 434 | 146 | 159 | 170 | 35 | 48 | 65 | 16 | 18 | 24 | 356 | 145 | 154 | 162 | 36 | 45 | 60 | 16 | 19 | 25 |
| 2013 | 388 | 147 | 159 | 170 | 36 | 47 | 62 | 16 | 19 | 24 | 404 | 146 | 154 | 162 | 36 | 45 | 58 | 16 | 19 | 23 |
| 2014 | 424 | 147 | 158 | 169 | 35 | 46 | 63 | 16 | 18 | 23 | 383 | 145 | 154 | 162 | 36 | 46 | 59 | 16 | 19 | 24 |
| 2015 | 378 | 145 | 159 | 171 | 35 | 47 | 63 | 16 | 18 | 23 | 395 | 145 | 154 | 163 | 36 | 46 | 59 | 16 | 19 | 24 |
| 2016 | 403 | 145 | 160 | 171 | 34 | 47 | 65 | 16 | 18 | 25 | 374 | 146 | 155 | 162 | 36 | 46 | 59 | 16 | 19 | 24 |
| 2017 | 409 | 146 | 160 | 172 | 35 | 47 | 66 | 16 | 18 | 25 | 416 | 145 | 154 | 163 | 36 | 46 | 60 | 16 | 19 | 25 |
| P for trend | 0.335 | 0.568 | 0.097 | 0.585 | 0.296 | 0.206 | ||||||||||||||
BMI, body mass index.
The Jonckheere-Terpstra test was used to evaluate secular trends, with calendar year as the explanatory variable and individual measurements as dependent variables.
Table 2. Secular trends in overweight and underweight children (numbers and proportions).
| Total | Overweight | Underweight | Total | Overweight | Underweight | |||||
| Boys at age 10 | Girls at age 10 | |||||||||
| 2007 | 387 | 52 | 13.4% | 25 | 6.5% | 400 | 27 | 6.8% | 32 | 8.0% |
| 2008 | 430 | 61 | 14.2% | 24 | 5.6% | 391 | 29 | 7.4% | 26 | 6.6% |
| 2009 | 452 | 56 | 12.4% | 32 | 7.1% | 380 | 29 | 7.6% | 35 | 9.2% |
| 2010 | 419 | 50 | 11.9% | 29 | 6.9% | 432 | 20 | 4.6% | 37 | 8.6% |
| 2011 | 461 | 52 | 11.3% | 45 | 9.8% | 395 | 30 | 7.6% | 20 | 5.1% |
| 2012 | 423 | 50 | 11.8% | 22 | 5.2% | 420 | 26 | 6.2% | 29 | 6.9% |
| 2013 | 434 | 67 | 15.4% | 31 | 7.1% | 410 | 29 | 7.1% | 33 | 8.0% |
| 2014 | 435 | 54 | 12.4% | 36 | 8.3% | 434 | 23 | 5.3% | 19 | 4.4% |
| 2015 | 442 | 59 | 13.3% | 26 | 5.9% | 420 | 25 | 6.0% | 23 | 5.5% |
| 2016 | 430 | 60 | 14.0% | 30 | 7.0% | 395 | 38 | 9.6% | 24 | 6.1% |
| 2017 | 502 | 81 | 16.1% | 36 | 7.2% | 412 | 29 | 7.0% | 27 | 6.6% |
| P for trend | 0.182 | 0.686 | 0.645 | 0.044 | ||||||
| Boys at age 13 | Girls at age 13 | |||||||||
| 2007 | 395 | 36 | 9.1% | 61 | 15.4% | 373 | 21 | 5.6% | 17 | 4.6% |
| 2008 | 382 | 26 | 6.8% | 55 | 14.4% | 346 | 24 | 6.9% | 24 | 6.9% |
| 2009 | 389 | 29 | 7.5% | 52 | 13.4% | 360 | 21 | 5.8% | 21 | 5.8% |
| 2010 | 360 | 18 | 5.0% | 49 | 13.6% | 387 | 20 | 5.2% | 27 | 7.0% |
| 2011 | 406 | 22 | 5.4% | 62 | 15.3% | 372 | 20 | 5.4% | 19 | 5.1% |
| 2012 | 434 | 28 | 6.5% | 46 | 10.6% | 356 | 24 | 6.7% | 24 | 6.7% |
| 2013 | 388 | 21 | 5.4% | 50 | 12.9% | 404 | 18 | 4.5% | 34 | 8.4% |
| 2014 | 424 | 22 | 5.2% | 72 | 17.0% | 383 | 22 | 5.7% | 21 | 5.5% |
| 2015 | 378 | 19 | 5.0% | 51 | 13.5% | 395 | 23 | 5.8% | 22 | 5.6% |
| 2016 | 403 | 34 | 8.4% | 75 | 18.6% | 374 | 22 | 5.9% | 28 | 7.5% |
| 2017 | 409 | 33 | 8.1% | 66 | 16.1% | 416 | 24 | 5.8% | 21 | 5.0% |
| P for trend | 0.682 | 0.165 | 0.815 | 0.780 | ||||||
Body mass index (BMI) cut-offs were used to determine overweight and underweight children;
overweight boys and girls: BMI (kg/m2) >20.04 and >20.97 at age 10 years, and >23.26 and >23.89 at age 13, respectively.
underweight boys and girls: BMI (kg/m2) <14.57 and <14.39 at aged 10 years, and <16.52 and <16.17 at age 13, respectively.
The Cochran-Armitage test was used to evaluate secular trends.
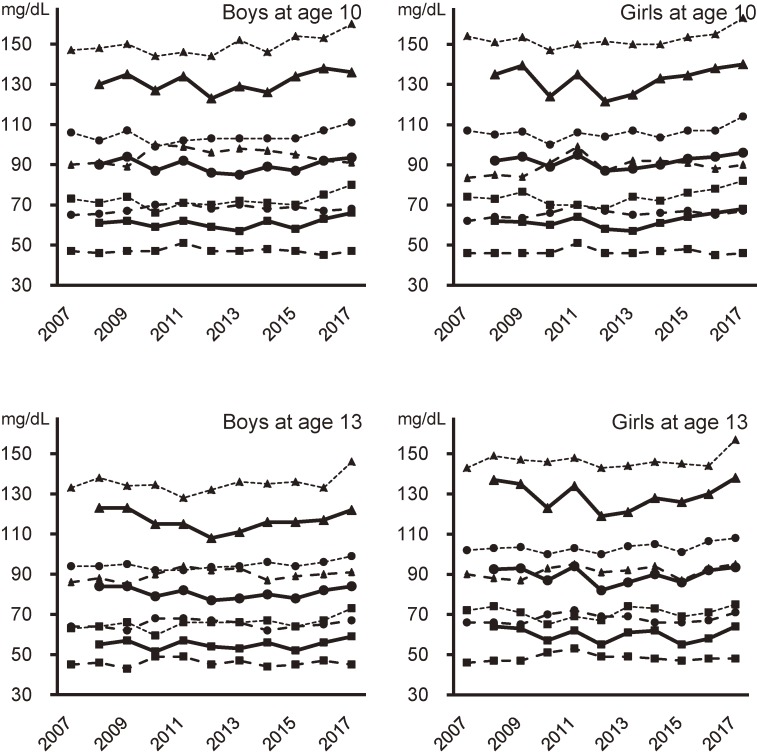
Figure 1 shows serum levels (95th, 50th, and 5th percentiles) of LDL-C, non-HDL-C, and HDL-C. LDL-C showed a significant positive association with calendar year in both boys and girls aged 10 years from 2008 through 2017. In addition, non-HDL-C showed a significant positive association with calendar year in both boys and girls aged 10 and 13 years from 2007 through 2017. Furthermore, HDL-C showed a significant positive association with calendar year in both boys and girls aged 10 years, and showed a significant increase in girls aged 13 years during the same period. T-C also showed a significant (P < 0.001) increase from 2007 through 2017, regardless of sex or age. The LDL-C to HDL-C ratio (LDL-C/HDL-C) showed no significant trends in both boys and girls aged 10 and 13 years from 2008 through 2017.
Figure 1. Secular trends in the percentiles of serum cholesterol levels. Triangles, 95th percentile; Circles, 50th percentile; Squares, 5th percentile; Solid lines, low-density lipoprotein cholesterol (LDL-C); Broken lines, high-density lipoprotein cholesterol (HDL-C); Dotted lines, non-high-density lipoprotein cholesterol (non-HDL-C). The Jonckheere-Terpstra test was used to evaluate secular trends, with calendar year as the explanatory variable and individual measurements as dependent variables. In children aged 10 years, significant increases were observed in LDL-C (P = 0.009 in boys, 0.014 in girls), HDL-C (P = 0.021 in boys, P < 0.001 in girls), and non-HDL-C (P < 0.001 in both sexes). In children aged 13 years, significant increases were observed in non-HDL-C in boys (P = 0.001) and girls (P < 0.001), and in HDL-C in girls (P = 0.017).
Table 3 shows the prevalence of adverse lipid levels from 2007 through 2017. No significant trends were observed during the study period in children with high LDL-C and those with low HDL-C, regardless of sex or age, while the prevalence of high non-HDL-C showed a significant increase in boys aged 10 and 13 years.
Table 3. Secular trends in children with dyslipidemia (numbers and proportions).
| Total | High LDL-C | High non-HDL-C | Low HDL-C | Total | High LDL-C | High non-HDL-C | Low HDL-C | |||||||
| Boys at age 10 | Girls at age 10 | |||||||||||||
| 2007 | 387 | 23 | 5.9% | 4 | 1.0% | 400 | 37 | 9.3% | 7 | 1.8% | ||||
| 2008 | 430 | 25 | 5.8% | 26 | 6.0% | 6 | 1.4% | 391 | 28 | 7.2% | 30 | 7.7% | 2 | 0.5% |
| 2009 | 452 | 33 | 7.3% | 35 | 7.7% | 2 | 0.4% | 380 | 37 | 9.7% | 34 | 8.9% | 4 | 1.1% |
| 2010 | 419 | 18 | 4.3% | 20 | 4.8% | 3 | 0.7% | 432 | 12 | 2.8% | 24 | 5.6% | 7 | 1.6% |
| 2011 | 461 | 34 | 7.4% | 29 | 6.3% | 3 | 0.7% | 395 | 29 | 7.3% | 32 | 8.1% | 0 | 0.0% |
| 2012 | 423 | 15 | 3.5% | 21 | 5.0% | 6 | 1.4% | 420 | 13 | 3.1% | 28 | 6.7% | 4 | 1.0% |
| 2013 | 434 | 18 | 4.1% | 34 | 7.8% | 5 | 1.2% | 410 | 13 | 3.2% | 29 | 7.1% | 4 | 1.0% |
| 2014 | 435 | 19 | 4.4% | 25 | 5.7% | 3 | 0.7% | 434 | 25 | 5.8% | 32 | 7.4% | 4 | 0.9% |
| 2015 | 442 | 30 | 6.8% | 36 | 8.1% | 6 | 1.4% | 420 | 32 | 7.6% | 37 | 8.8% | 2 | 0.5% |
| 2016 | 430 | 39 | 9.1% | 40 | 9.3% | 3 | 0.7% | 395 | 32 | 8.1% | 35 | 8.9% | 5 | 1.3% |
| 2017 | 502 | 40 | 8.0% | 60 | 12.0% | 4 | 0.8% | 412 | 37 | 9.0% | 54 | 13.1% | 4 | 1.0% |
| P for trend | 0.080 | <0.001 | 0.882 | 0.204 | 0.060 | 0.524 | ||||||||
| Boys at age 13 | Girls at age 13 | |||||||||||||
| 2007 | 395 | 8 | 2.0% | 8 | 2.0% | 373 | 16 | 4.3% | 2 | 0.5% | ||||
| 2008 | 382 | 11 | 2.9% | 13 | 3.4% | 6 | 1.6% | 346 | 24 | 6.9% | 22 | 6.4% | 3 | 0.9% |
| 2009 | 389 | 10 | 2.6% | 10 | 2.6% | 8 | 2.1% | 360 | 25 | 6.9% | 21 | 5.8% | 3 | 0.8% |
| 2010 | 360 | 3 | 0.8% | 8 | 2.2% | 0 | 0.0% | 387 | 13 | 3.4% | 21 | 5.4% | 1 | 0.3% |
| 2011 | 406 | 7 | 1.7% | 8 | 2.0% | 3 | 0.7% | 372 | 24 | 6.5% | 22 | 5.9% | 1 | 0.3% |
| 2012 | 434 | 5 | 1.2% | 10 | 2.3% | 8 | 1.8% | 356 | 9 | 2.5% | 14 | 3.9% | 1 | 0.3% |
| 2013 | 388 | 7 | 1.8% | 10 | 2.6% | 2 | 0.5% | 404 | 11 | 2.7% | 20 | 5.0% | 3 | 0.7% |
| 2014 | 424 | 10 | 2.4% | 12 | 2.8% | 7 | 1.7% | 383 | 16 | 4.2% | 21 | 5.5% | 2 | 0.5% |
| 2015 | 378 | 8 | 2.1% | 13 | 3.4% | 5 | 1.3% | 395 | 15 | 3.8% | 20 | 5.1% | 4 | 1.0% |
| 2016 | 403 | 10 | 2.5% | 13 | 3.2% | 3 | 0.7% | 374 | 19 | 5.1% | 17 | 4.5% | 2 | 0.5% |
| 2017 | 409 | 10 | 2.4% | 21 | 5.1% | 7 | 1.7% | 416 | 33 | 7.9% | 37 | 8.9% | 5 | 1.2% |
| P for trend | 0.723 | 0.027 | 0.449 | 0.842 | 0.243 | 0.359 | ||||||||
LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol.
2011 Expert Panel cut-offs (high LDL-C, ≥130 mg/dL; high non-HDL-C, ≥145 mg/dL; low HDL-C, <40 mg/dL) were used.
The Cochran-Armitage test was used to evaluate secular trends.
DISCUSSION
This is the first study to report secular trends of LDL-C in Japanese children. We found no remarkable changes in the prevalence of adverse LDL-C (≥130 mg/dL) or HDL-C (<40 mg/dL) in a population of school-aged children in Fukuroi City during the past decade, while the prevalence of high non-HDL-C increased. With regard to serum cholesterol levels, both HDL-C and LDL-C slightly increased in children aged 10 years for both sexes, and HDL-C slightly increased in girls aged 13 years.
The Circulatory Risk in Communities Study has reported that serum levels of LDL-C were positively associated with risk of coronary heart disease in a Japanese population.24 On the other hand, dyslipidemia, including high LDL-C, in adults often emerges during childhood,8 and the Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents strongly recommends cardiovascular health and risk reduction in children and adolescents.14 However, no previous study has examined secular trends in LDL-C among Japanese schoolchildren. In the present study, the Fukuroi population aged 10 years showed a yearly increase in serum LDL-C levels, with an accompanying increase in HDL-C levels. The present study also showed no significant trends in LDL-C/HDL-C in both boys and girls aged 10 and 13 years. The increase in HDL-C levels might have counteracted the effects of increased LDL-C levels in our study population. In addition, there were no remarkable trends in the prevalence of adverse lipid levels (ie, high LDL-C or low HDL-C). In Japan, nationwide surveys regarding serum T-C levels were conducted in 1960, 1970, 1980, and 1990, revealing a yearly increase in serum T-C levels among children and adolescents.17 More recently, our previous study found no significant trends in T-C, non-HDL-C, and HDL-C levels from 1993 to 2008 in a 10-year-old population in Iwata City (a city adjacent to Fukuroi City).19 The Japanese National Nutrition Survey reported that the total energy consumption per capita among 7- to 14-year-old children was 1,985 kcal/day in 2007 and 1,976 kcal/day in 2016, and that there were no remarkable differences in body height and weight among 13-year-old children between 2007 and 2016.25 Similar to these reports, the present study revealed no significant trends in BMI and the prevalence of overweight, while the prevalence of underweight showed a decrease in girls at age 10. To predict the prevalence of adult cardiovascular disease in the future, a continuous survey regarding blood lipids among children will be necessary.
With respect to serum LDL-C levels, both 10-year-old boys and girls showed significant increases during the study period; however, no significant trends were observed in 13-year-old children. These results suggest that there may be an age-related difference in trends of serum cholesterol. A possible explanation can be provided in terms of susceptibility, which is defined as a capacity characterized by biological factors that can modify the effect of a specific exposure.26 It is recognized that children are more susceptible to environmental exposure and have a greater potential for adverse health effects than adults.27,28 This may explain why environmental effects on serum lipids may be smaller during juvenile and adolescent periods compared to previous growth stages. Susceptibility may be one reason for the age-related difference in trends of serum cholesterol.
The present study has notable strengths. First, this study is the first to report trends in LDL-C in Japanese children. Childhood trends in serum lipids, which include not only T-C, HDL-C, and non-HDL but also LDL-C, provide additional information to predict subsequent cardiovascular disease trends in adults. Second, the source population of the present study comprised all children in Fukuroi City aged 10 and 13 years. Moreover, the analyzed population was 93.8% of the source population. Third, data were obtained from annual health examinations conducted during a consistent period (April to June) from 2007 through 2017. Reportedly, dynamic changes in serum lipids are observed during puberty, and serum lipid concentrations decrease with pubertal growth.23 If data of serum lipids were collected at the same age, this might have helped remove the effect of growth on serum lipid levels. However, since blood sampling was performed during the 3-month period in the present school screening, the effect of growth on the lipids levels could not be removed completely. In contrast, there are also some limitations worth noting. First, our data were obtained from only one city in Japan, so the data were not randomly selected from throughout Japan. Yet, according to a nationwide report of the School Health Examination Survey by the Ministry of Education, Culture, Sports, Science and Technology, Japan (conducted from April through June in 2016), at age 10, mean height was 139 cm in boys and 140 cm in girls, and mean body weight was 34 kg in both boys and girls.29 At age 13, mean height was 160 cm in boys and 155 cm in girls, and mean body weight was 49 kg in boys and 47 kg in girls.29 Thus, mean height and weight are similar between the Fukuroi population and the general population in Japan. If there are no remarkable differences in characteristics between the Fukuroi population and the overall Japanese population, trends of the Japanese population may be inferred from trends of the Fukuroi population. Second, many factors related to serum lipids, including physical activity and dietary habits, were not considered in the present study. Further investigation is warranted; in particular, a study involving several cities throughout Japan and a large-scale survey of lifestyle in children to examine future cardiovascular disease trends in Japanese adults would be useful.
In conclusion, we found no remarkable changes in the prevalence of adverse LDL-C levels from 2008 through 2017 and HDL-C levels from 2007 through 2017 in a population of school-aged children in Fukuroi City, while the prevalence of high non-HDL-C increased from 2007 through 2017. Among boys and girls aged 10 years, both serum levels of LDL-C and HDL-C slightly increased during the past decade. Serum HDL-C levels also slightly increased in girls aged 13 years during the same period.
ACKNOWLEDGEMENTS
The authors thank the Board of Education, teaching staff members of elementary and junior high schools, and staff members of the local health center in Fukuroi City for their support. This work was supported in part by a Grant-in-Aid for “Research on Health Promotion from Childhood” from Fukuroi, Japan.
Conflicts of interest: None declared.
REFERENCES
- 1.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–2497. 10.1001/jama.285.19.2486 [DOI] [PubMed] [Google Scholar]
- 2.Wiegman A, de Groot E, Hutten BA, et al. Arterial intima-media thickness in children heterozygous for familial hypercholesterolaemia. Lancet. 2004;363(9406):369–370. 10.1016/S0140-6736(04)15467-6 [DOI] [PubMed] [Google Scholar]
- 3.Freedman DS, Shear CL, Srinivasan SR, Webber LS, Berenson GS. Tracking of serum lipids and lipoproteins in children over an 8-year period: the Bogalusa Heart Study. Prev Med. 1985;14:203–216. 10.1016/0091-7435(85)90036-2 [DOI] [PubMed] [Google Scholar]
- 4.Porkka KV, Viikari JS, Akerblom HK. Tracking of serum HDL-cholesterol and other lipids in children and adolescents: the Cardiovascular Risk in Young Finns Study. Prev Med. 1991;20:713–724. 10.1016/0091-7435(91)90066-D [DOI] [PubMed] [Google Scholar]
- 5.Webber LS, Srinivasan SR, Wattigney WA, Berenson GS. Tracking of serum lipids and lipoproteins from childhood to adulthood. The Bogalusa Heart Study. Am J Epidemiol. 1991;133:884–899. 10.1093/oxfordjournals.aje.a115968 [DOI] [PubMed] [Google Scholar]
- 6.Porkka KV, Viikari JS, Taimela S, Dahl M, Akerblom HK. Tracking and predictiveness of serum lipid and lipoprotein measurements in childhood: a 12-year follow-up. The Cardiovascular Risk in Young Finns study. Am J Epidemiol. 1994;140:1096–1110. 10.1093/oxfordjournals.aje.a117210 [DOI] [PubMed] [Google Scholar]
- 7.Tan F, Okamoto M, Suyama A, Miyamoto T. Tracking of cardiovascular risk factors and a cohort study on hyperlipidemia in rural schoolchildren in Japan. J Epidemiol. 2000;10:255–261. 10.2188/jea.10.255 [DOI] [PubMed] [Google Scholar]
- 8.Nicklas TA, von Duvillard SP, Berenson GS. Tracking of serum lipids and lipoproteins from childhood to dyslipidemia in adults: the Bogalusa Heart Study. Int J Sports Med. 2002;23(Suppl 1):S39–S43. 10.1055/s-2002-28460 [DOI] [PubMed] [Google Scholar]
- 9.Raitakari OT, Juonala M, Kähönen M, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–2283. 10.1001/jama.290.17.2277 [DOI] [PubMed] [Google Scholar]
- 10.Li S, Chen W, Srinivasan SR, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA. 2003;290:2271–2276. 10.1001/jama.290.17.2271 [DOI] [PubMed] [Google Scholar]
- 11.Strong JP, Malcom GT, McMahan CA, et al. Prevalence and extent of atherosclerosis in adolescents and young adults: implications for prevention from the Pathobiological Determinants of Atherosclerosis in Youth Study. JAMA. 1999;281:727–735. 10.1001/jama.281.8.727 [DOI] [PubMed] [Google Scholar]
- 12.Tanaka K, Masuda J, Imamura T, et al. A nation-wide study of atherosclerosis in infants, children and young adults in Japan. Atherosclerosis. 1988;72:143–156. 10.1016/0021-9150(88)90075-5 [DOI] [PubMed] [Google Scholar]
- 13.Imakita M, Yutani C, Strong JP, et al. Second nation-wide study of atherosclerosis in infants, children and young adults in Japan. Atherosclerosis. 2001;155:487–497. 10.1016/S0021-9150(00)00595-5 [DOI] [PubMed] [Google Scholar]
- 14.Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute . Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: Summary report. Pediatrics. 2011;128(Suppl 5):S213–S256. 10.1542/peds.2009-2107C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kit BK, Carroll MD, Lacher DA, Sorlie PD, DeJesus JM, Ogden C. Trends in serum lipids among US youths aged 6 to 19 years, 1988–2010. JAMA. 2012;308:591–600. 10.1001/jama.2012.9136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ding W, Cheng H, Yan Y, et al. 10-Year Trends in serum lipid levels and dyslipidemia among children and adolescents from several schools in Beijing, China. J Epidemiol. 2016;26:637–645. 10.2188/jea.JE20140252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murata M. Secular trends in growth and changes in eating patterns of Japanese children. Am J Clin Nutr. 2000;72(5)(Suppl):1379S–1383S. 10.1093/ajcn/72.5.1379s [DOI] [PubMed] [Google Scholar]
- 18.Elshourbagy NA, Meyers HV, Abdel-Meguid SS. Cholesterol: the good, the bad, and the ugly - therapeutic targets for the treatment of dyslipidemia. Med Princ Pract. 2014;23:99–111. 10.1159/000356856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kouda K, Nakamura H, Nishio N, Fujita Y, Takeuchi H, Iki M. Trends in body mass index, blood pressure, and serum lipids in Japanese children: Iwata population-based annual screening (1993–2008). J Epidemiol. 2010;20:212–218. 10.2188/jea.JE20090079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kouda K, Nakamura H, Tokunaga R, Takeuchi H. Trends in levels of cholesterol in Japanese children from 1993 through 2001. J Epidemiol. 2004;14:78–82. 10.2188/jea.14.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Foster TA, Voors AW, Webber LS, Frerichs RR, Berenson GS. Anthropometric and maturation measurements of children, ages 5 to 14 years, in a biracial community—the Bogalusa Heart Study. Am J Clin Nutr. 1977;30:582–591. 10.1093/ajcn/30.4.582 [DOI] [PubMed] [Google Scholar]
- 22.Inokuchi M, Hasegawa T, Anzo M, Matsuo N. Standardized centile curves of body mass index for Japanese children and adolescents based on the 1978–1981 national survey data. Ann Hum Biol. 2006;33:444–453. 10.1080/03014460600802353 [DOI] [PubMed] [Google Scholar]
- 23.Kouda K, Nakamura H, Fan W, Takeuchi H. Negative relationships between growth in height and levels of cholesterol in puberty: a 3-year follow-up study. Int J Epidemiol. 2003;32:1105–1110. 10.1093/ije/dyg207 [DOI] [PubMed] [Google Scholar]
- 24.Imano H, Noda H, Kitamura A, et al. Low-density lipoprotein cholesterol and risk of coronary heart disease among Japanese men and women: the Circulatory Risk in Communities Study (CIRCS). Prev Med. 2011;52:381–386. 10.1016/j.ypmed.2011.02.019 [DOI] [PubMed] [Google Scholar]
- 25.Ministry of Health, Labour and Welfare of Japan. The National Health and Nutrition Survey in Japan. https://www.mhlw.go.jp/bunya/kenkou/kenkou_eiyou_chousa.html. Accessed 2018.10.02.
- 26.Hines RN, Sargent D, Autrup H, et al. Approaches for assessing risks to sensitive populations: lessons learned from evaluating risks in the pediatric population. Toxicol Sci. 2010;113:4–26. 10.1093/toxsci/kfp217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Selevan SG, Kimmel CA, Mendola P. Identifying critical windows of exposure for children’s health. Environ Health Perspect. 2000;108(Suppl 3):451–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Branum AM, Collman GW, Correa A, et al. ; National Children’s Study Interagency Coordinating Committee, Centers for Disease Control and Prevention; National Children’s Study Interagency Coordinating Committee, National Institute of Environmental Health Sciences; National Children’s Study Interagency Coordinating Committee, National Institute of Child Health and Human Development; National Children’s Study Interagency Coordinating Committee, U.S. Environmental Protection Agency . The National Children’s Study of environmental effects on child health and development. Environ Health Perspect. 2003;111:642–646. 10.1289/ehp.111-1241458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Statistics Bureau, Ministry of Internal Affairs and Communications. Japan Statistical Yearbook 2018. 2018. [Google Scholar]