Abstract
This article provides an analysis of the skills that health professionals and patients employ in reaching diagnosis and decision-making in telemedicine consultations. As governmental priorities continue to emphasize patient involvement in the management of their disease, there is an increasing need to accurately capture the provider–patient interactions in clinical encounters. Drawing on conversation analysis of 10 video-mediated consultations in 3 National Health Service settings in England, this study examines the interaction between patients, General Practitioner (GPs), nurses, and consultants during diagnosis and decision-making, with the aim to identify the range of skills that participants use in the process and capture the interprofessional communication and patient involvement in the diagnosis and decision-making phases of telemedicine consultations. The analysis shows that teleconsultations enhance collaborative working among professionals and enable GPs and nurses to develop their skills and actively participate in diagnosis and decision-making by contributing primary care–specific knowledge to the consultation. However, interprofessional interaction may result in limited patient involvement in decision-making. The findings of this study can be used to inform training programs in telemedicine that focus on the development of effective skills for professionals and the provision of information to patients.
Keywords: telemedicine, conversation analysis, eHealth, decision-making, patient-centered care
Diagnosis and Decision-Making in Telemedicine
Governments and care providers around the world are seeking to introduce telemedicine to address the rising demand for health-care and system capacity constraints (1). Despite the growing political support, telemedicine systems have failed to normalize (ie, become part of everyday practice) due to doubts about their efficacy, cost-effectiveness, and user acceptance (2,3). Technological competence, cost-effectiveness, and acceptability are central to the successful implementation of telemedicine services. However, equally essential is the ability to communicate effectively in this new medium (4). Telemedicine is potentially an ideal environment in which shared decision-making can take place, as it allows clinicians and the patient to collectively communicate about the patient’s care. Patients involved in shared decision-making have better health outcomes (5,6) and telemedicine offers the opportunity to make this possible.
The aim of this study is to capture the range of skills that health professionals and patients use in reaching diagnosis and decision-making in telemedicine consultations. The analysis also focuses on the interprofessional communication during the diagnosis and decision-making phases in video-mediated telemedicine as well as the patient involvement in reaching a diagnostic conclusion and deciding on the preferred course of management. Understanding the effect of telemedicine on the provider–patient relationship and how this affects the process and outcome of the consultation is especially important in view of the marked changes in the technical and interpersonal contexts within which communication takes place (6,7).
For more than a decade, research has been predominantly focusing on assessing telemedicine with regard to its technological attributes (8 –11), cost, quality, and access (12 –14) as well as patient and physician satisfaction (15 –18). However, little is known about the experiences and skills that participants employ in telemedicine encounters and further research is needed to analyze social interaction within an environment that is characterized by organizational, spatial, and technological novelties (19 –22). As Whitten et al (23) put it, “we know a good deal about bandwidths and resolutions, but little about the human dimensions that make practice possible” (p. 112).
Real-time videoconferencing (here forth referred as teleconsultations) represents a unique opportunity for cross-boundary collaboration and shared decision-making. It provides hospital specialists with the information to evaluate patients’ symptoms and concerns. It also enables consultants to communicate with GPs and/or nurses to reach a diagnosis and decide on a management plan and, perhaps most significantly, offers the opportunity to involve patients in decision-making. Patient-centered models of care focusing on patient autonomy, informed consent, and empowerment have gained a high level of policy support (24,25). Patients also declare their support for patient-centered decision-making in health care (26). As it has become a priority worldwide to continue to emphasize the inclusion of patients in diagnosis and decision-making, there is a pressing need for research that accurately and in detail captures and discusses the contribution of all participants in clinician–patient encounters.
Professionals and patients have competencies and use sets of knowledge that are relevant to the medical consultation. Shared decision-making is a model of the physician–patient relationship in which both parties have an equal role in determining the course of action. Clinicians and patients consider the available screening, treatment, or management options and based on the benefits and harms of each option make decisions about the best course of treatment (27).
Shared decision-making policies are becoming prominent due to the recognition that higher levels of patient involvement result in better quality of care, increased patient and medical staff satisfaction, and improved patient self-esteem (5). For patients, “shared decision-making means a willingness to engage in the decision making process and take responsibility for disclosing preferences, asking questions, weighing and evaluating treatment alternatives and formulating a treatment preference” (p.830) (28). However, previous work in the opening (22) and physical examination (29) phases in teleconsultations has shown that hospital specialists and primary care professionals draw on the skills acquired from their experience with face-to-face (FTF) encounters and determine the structure of the consultation, which in turn results in patients having limited scope to get involved in and contribute to the encounter.
The practice of telemedicine today is based on skills that professionals bring to it from their experience with FTF consultations. However, communication in FTF and telemedicine consultations differs significantly, partly due to the presence of a number of health-care professionals from diverse levels of care in the consultation and partly because of the presence of new technology (22). To optimize the use of telemedicine, new normative standards of behavior and interpersonal communication need to be developed to support important functions of the medical consultation, such as history taking, physical examination, diagnosis, and decision-making (30). There is a long list of arguments in the literature whether the available video link technologies facilitate or hinder communication between distant sites (31,32), and several researchers have called for more and rigorous studies examining the effect of telemedicine on patient–provider communication, relations, and outcomes (22,29,32).
We argue that further research is needed to understand telemedicine interaction as an accomplishment of social actors within an environment that is characterized by organizational, spatial, and technological novelties. Previous analyses of interaction in the opening (22) and physical examination (29) phases of teleconsultations have shown that those factors affect the way in which participants perform and perceive their roles. This study captures the skills that health professionals and patients use in the diagnosis and decision-making phases of telemedicine consultations with the aim to shed light on the effect of telemedicine on the patient–provider communication and inform policy makers about the resources and training required for all participants to develop and use communication skills that facilitate shared decision-making.
Methods
Miller (7) argues that qualitative analysis of the actual behavior of participants in teleconsultations can lead to a better understanding of the relationship between telemedicine and interpersonal communication. In this article, we present findings based on conversation analysis (CA). Conversation analysis is an ethnomethodological method that provides researchers with the opportunity to get an in-depth view of the skills that social actors use and rely on during social interactions (33). It involves the study of recorded talk and has been widely used in medical research to study doctor–patient interactions in FTF consultations (for a review, see the study by Atkinson and Heritage [34], Maynard and Heritage [35], and Silverman [36]) as well as to provide the frame for practical guidance to health-care professionals from different specialties (37 –40). In the context of telemedicine, CA helps to capture and understand communication as it happens, in situ, rather than as reported in retrospective satisfaction surveys with patients and clinicians.
Conversation analysis was used in this study to describe the procedures by which parties produce their own behavior and respond to the behavior of others in the diagnosis and decision-making phases in teleconsultations. The analysis yielded findings in 2 broad areas:
The range of skills that participants employ in the diagnosis and decision-making phases in video-mediated consultations.
The interprofessional communication and patient involvement during diagnosis and decision-making.
Ten (5 telecardiology and 5 televascular) randomly selected video-mediated consultations were recorded, transcribed (using the system developed by Jefferson, see the study by Atkinson and Heritage [34]), and analyzed. Research was conducted in 3 National Health Service (NHS) settings in England. A primary care clinic in the South East of England was the main telemedicine provider. From there, patients, GPs, nurses, and in some cases a relative accompanying the patient were able to communicate with specialists in 2 district hospitals: a cardiology specialist in hospital A and a vascular surgeon in hospital B. The communication between the participants was facilitated through a video -link that was set between the specialist’s office and the primary care clinic. Patients who were over 80 years of age, did not speak English as a first language, or their physicians specifically requested not to take part in the study were excluded. Ethics approval was provided by the Oxford A Research Ethics Committee (ref: 05/Q1604/15), and informed consent was obtained from all participants.
Findings
Decision-Making in Telemedicine Consultations
The nurse as evaluator and treatment facilitator
In order to overcome the fact that the specialist cannot directly assess the patient’s symptoms, active collaboration is established between the professionals during physical examination through telemedicine. Extract 1 (Figure 1) reveals the extent to which the nurse is involved not just in physical examination but also in reaching a diagnosis.
Figure 1.
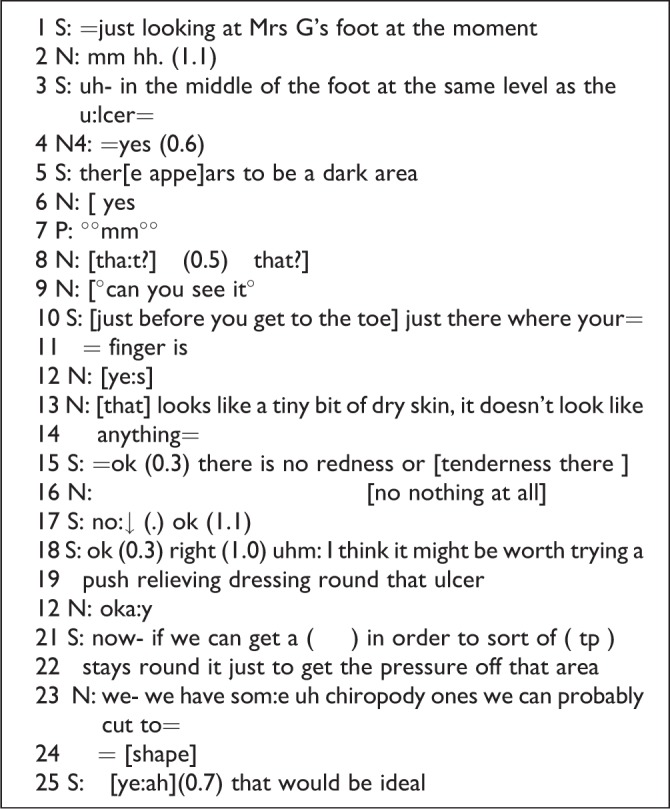
Televascular extract.
In extract 1 (Figure 1), the specialist requires the nurse to contribute to the diagnosis by assessing what the specialist perceives on her monitor as a dark area on the patient’s foot in line 5. Following the sequences 6 to 12 during which the 2 nurses and the specialist try to coordinate their efforts to locate the area on the patient’s foot which the specialist perceived as a dark area, the first nurse makes an assessment in line 13: “[that] looks like a tiny bit of dry skin, it doesn’t look like anything” which is confirmed in line 16: “[no nothing at all].” The nurse’s utterances are not descriptive remarks that allow the specialist to reach a diagnosis based on her own competencies but highly evaluative contributions as they involve an assessment of symptoms based on the nurse’s competences. Such evaluative contributions determine the plan of treatment that the specialist proposes immediately after, in lines 18 and 19: “ok (0.3) right (1.0) uhm: I think it might be worth trying a push relieving dressing round that ulcer.” Apart from the active role the nurse acquires during the assessment of symptoms, she also makes a contribution by proposing a specific type of pressure relieving dressing in lines 23 and 24: “we have som: e uh chiropody ones we can probably cut to [shape],” which also finds the specialist agreeing: “[ye: ah] (0.7) that would be ideal.”
There are instances in telemedicine consultations where the nurse makes significant contributions to the treatment decision by offering knowledge that is specific to primary care and the range of resources that are available for treating the patient locally. In extract 2 (Figure 2), the nurse volunteers such knowledge and makes an essential contribution at a point where the patient and the specialist were experiencing a discrepancy while discussing possible treatment plans.
Figure 2.
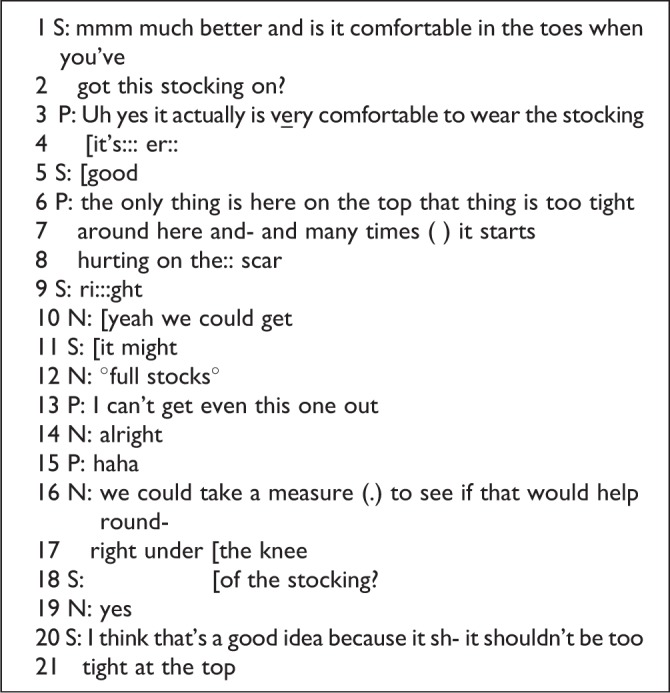
Televascular extract.
In extract 2 (Figure 2), the patient expresses satisfaction with the pressure relieving stocking that she has been prescribed and is currently using but she claims that wearing the stocking is somewhat uncomfortable at the top of the leg. The specialist receives this remark with a prolonged acknowledgment token in line 9: “ri::: ght” before the nurse interjects with a suggestion in lines 10: [yeah we could get] and 12. Although this is not a suggestion with a high medical value or risk, the nurse’s contribution is based on competencies that are specific to the primary care setting.
In extracts 1 and 2 (Figures 1 and 2), the nurse plays an important role in contributing to a diagnosis and deciding a plan of treatment in 2 distinct ways. In extract 1 (Figure 1), the nurse makes evaluations of symptoms and shapes the final diagnosis, whereas in extract 2 (Figure 2), the nurse contributes to the treatment plan with knowledge specific to primary care.
Consultant–nurse interaction and patient participation
Generally, in telemedicine consultations, the nurses are well involved in physical examination, diagnosis, and decision-making. At times, interprofessional interaction during decision-making or suggestion of treatment was the most active communication channel.
Extract 3 (Figure 3) is an example of “treatment negotiation” between the specialist and the nurse while the patient assumes the role of over hearer.
Figure 3.
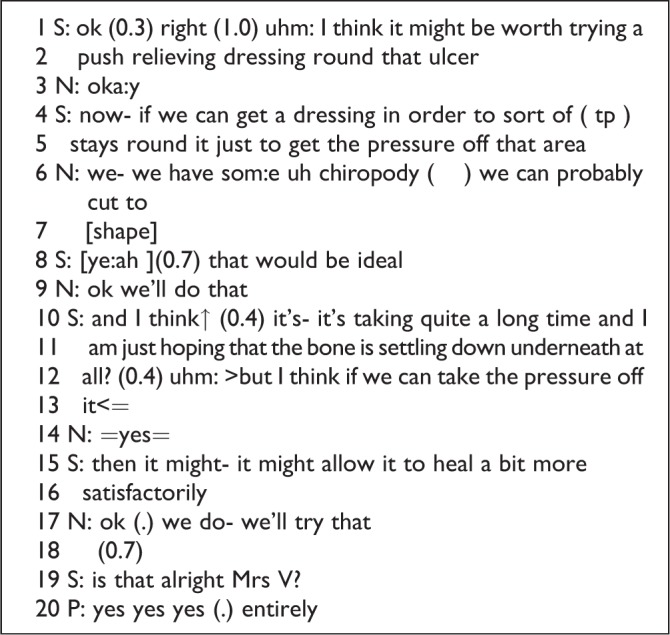
Televascular extract.
The consultant’s initial suggestion in lines 1 and 2 is not directly addressed to the patient and is received by the nurse who responds in line 3, an action which possibly establishes her as the recipient of all further communication with regard to the treatment plan. The consultant’s utterance in line 8 is a direct answer to the nurse’s suggestion which validates the interprofessional channel as the main channel of interaction. Finally, in line 18, the specialist explicitly involves the patient in the decision-making: “Is that alright Mrs V?”
The GP as informer and mediator
Interprofessional communication is even prominent when the professional at the primary care end is a GP. The GP often interjects to provide information based on his/her own set of knowledge which is specific to primary care. This set of knowledge consists of information with regard to medication, previous tests taken at the primary care, and information on the medical history and life circumstances of each patient that the specialist may not have available. Because general practitioners are in close contact with the patients, possibly know them for years, they are also more informed about the patients’ personal circumstances than consultants might be. In extract 4 (Figure 4), the GP and the specialist engage in information exchange that would assist with decision-making.
Figure 4.
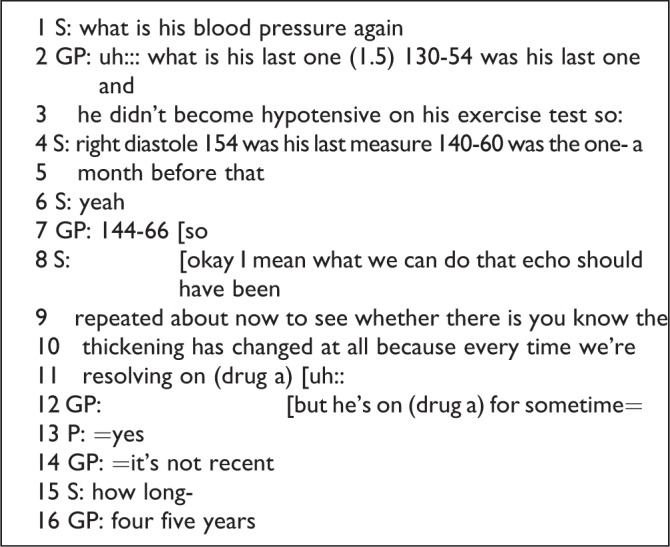
Telecardiology extract.
In extract 4 (Figure 4), the GP offers specific information regarding the patient’s medical history by referring to the electronic notes available to primary care. Whereas in extract 3 (Figure 3) there was a relative exclusion of the patient from decision-making, here the interprofessional and medically oriented talk from line 1 to line 12 excludes the patient completely from the preliminary stages of decision-making. The interjection of the patient in line 13: “yes” may be seen as an attempt of the patient to be involved in that process.
On other occasions, the GP acts as a mediator between the specialist and the patient. When acting as a mediator, the GP may assist the patient in overcoming technical problems which may occur in communication through the video -link as well as explain to the patient any activities relevant to the telemedical setting or emphasize certain points s/he thinks the specialist should take particular notice of such as various inconsistencies and paradoxically appearing symptoms. In extract (Figure 5), the GP explains to the patient the type of activities the specialist is engaging with.
Figure 5.

Telecardiology extract.
Having not been able to have a full view of the consultant, the patient finds it difficult to follow the interaction cues and keep up with the sequencing as the specialist does not look at the camera while he is trying to study the patient’s history. The noise of paper shuffling in line 1 is indicative of the engagement of the specialist with another activity, which the GP comes to explain in lower than the surrounding speech voice in line 4: “°°he is having your stuff up there he’s looking through°°.”
Consultant–GP interaction and patient participation
The GP is involved in the consultation by acting according to 2 distinct roles which have been identified in the previous sections. The 2 roles involve the GP as an informer, who provides medically and nonmedically oriented information to the specialist, and a mediator, who interjects to facilitate interaction between the patient and the consultant. By acting these 2 roles, the GP establishes himself as a main interactant in the encounter. Nevertheless, as it happens when the specialist and the patient interact with the nurse present, the GP and the specialist may engage in interprofessional talk that excludes the patient from important parts of the consultation.
In GP-led consultations, patient disengagement occurs as a result of 2 types of talk: clarifying queries and formulations. Clarifying queries can occur at any stage of the consultation. In the diagnosis and decision-making phase of the consultation, they are employed to enquire, summarize, or illustrate what has been discussed so far or express a query. By using this device, participants attempt to coordinate both their understanding and subsequent action. Extract (Figure 6) is an example of a clarifying query that attempts to facilitate common understanding of further action.
Figure 6.
Face-to-face (FTF) vascular extract.
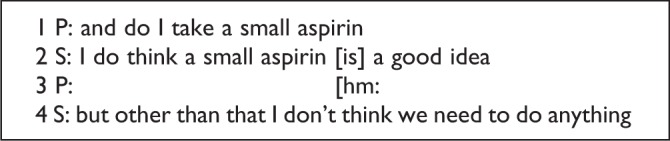
In extract 6, the patient enquires about whether she should be taking a small aspirin for her problem with clots in her veins. In line 2, the specialist agrees: “I do think a small aspirin [is]a good idea” and following the patient’s acceptance: “hm:” in line 3, she establishes that other than the small aspirin no other action is needed.
The same activity can also be accomplished by the use of formulation. Whereas clarifying queries are grammatically and semantically interrogative, formulations are not. Garfinkel and Sacks (41) have identified formulation as a phenomenon which occurs regularly in institutional talk where participants organize conversational tasks.
to describe that conversation, to explain it, or characterize it, or explicate, or translate, or summarize, or furnish the gist of it, or take note of its accordance with rules, or remark on its departure from rules. That is to say, a member may use some part of the conversation as an occasion to formulate the conversation…(41, p. 350).
In doctor–patient communication, formulations may facilitate mutuality in decision-making, as according to this model, decisions should be based on explicit agreement between the patient and the doctor about treatment options, management plans, or further tests. Central to the negotiation process are mutual understanding and confirmation of actions, without which any agreement lacks in dependability and may affect concordance.
The analysis of consultations, FTF, and telemedicine has revealed that formulating is undertaken by all participants, nurses, consultants, GPs, patients, and people accompanying patients. Extract 7 (Figure 7) is an example of formulation by the patient in a telecardiology consultation and is presented here as an indication of the device in telemedicine consultations:
Figure 7.
Telecardiology extract.
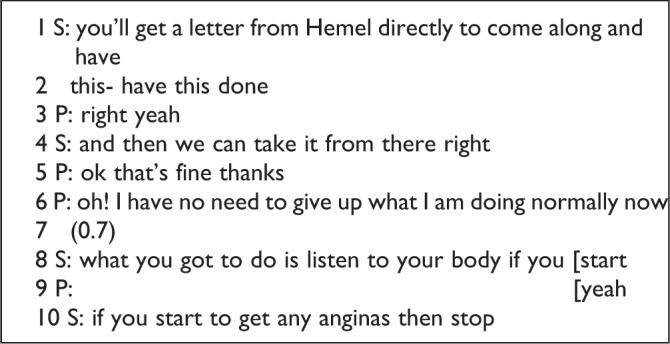
In extract 7 (Figure 7), the specialist explains further actions in lines 1 and 2. In lines 3 and 5, the patient accepts the plan of action before producing a formulation utterance in line 6. This formulation allows the patient to refer to whatever he feels it has not been mentioned in relation to the management plan and a common understanding has not been achieved.
Whereas formulations and clarifying queries do not follow a norm and all participants use both devices, in telemedicine, consultations are often used by the GP to orchestrate the activities and summarize, explain, characterize, and clear up misunderstandings. Extract (Figure 8) exemplifies the effect.
Figure 8.
Televascular extract.
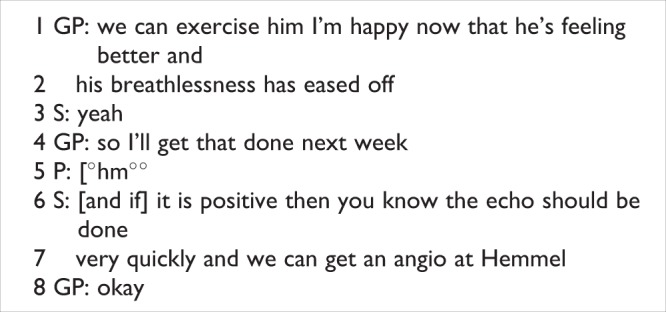
In lines 1 to 3, the GP and the specialist agree that now that the patient’s breathlessness has eased off they are able to do an exercise test on him. Up to this point, the patient is not involved at this planning of further action. In line 4, the GP produces an action formulation: “so I’ll get that done next week” to make the plan known to all participants. Perceiving himself as a possible recipient of the formulation, the patient produces a timid “°hm°°” in lower than the surrounding sound voice in line 5. At the same time, the specialist also perceives himself as the possible recipient and in lines 6 and 7 starts commenting in overlapping speech with the patient about actions they could take after the exercise test: “and if it is positive then you know the echo should be done very quickly and we can get an angio at Hemmel.” The GP agrees in line 8: “okay.”
In extract 9 (Figure 9), the interaction between the professionals has a clear educational character. Although the GP takes part in the decision-making process, he is not directly affecting decision-making. Following the initial formulation or query, the GP places himself into a learner’s position allowing the specialist to make decisions. Nevertheless formulations, clarifying queries, and what they achieve in telemedicine consultations, when the professionals engage in extensive interprofessional talk, have corollaries for patient involvement in decision-making.
Figure 9.
Telecardiology extract.
Formulations and clarifying queries exemplify the tendency of the consultants to perceive GPs’ interjections as attachments when the consultation has progressed, as formulations are followed by extensive interprofessional talk. The initiation of these devices by the GP establishes him or her as the rightful recipient of subsequent turns in interaction. There are instances where interprofessional communication breaks and the patient is involved in decision-making. Nevertheless the propensity of the 2 professionals to engage in interprofessional talk allows the patient to be involved at a minimal level. Extract 9 (Figure 9) exemplifies the profound effect that GP clarifying queries and formulations may have an interaction between the participants and the establishment of the interprofessional channel of interaction as the main channel of interaction during decision-making.
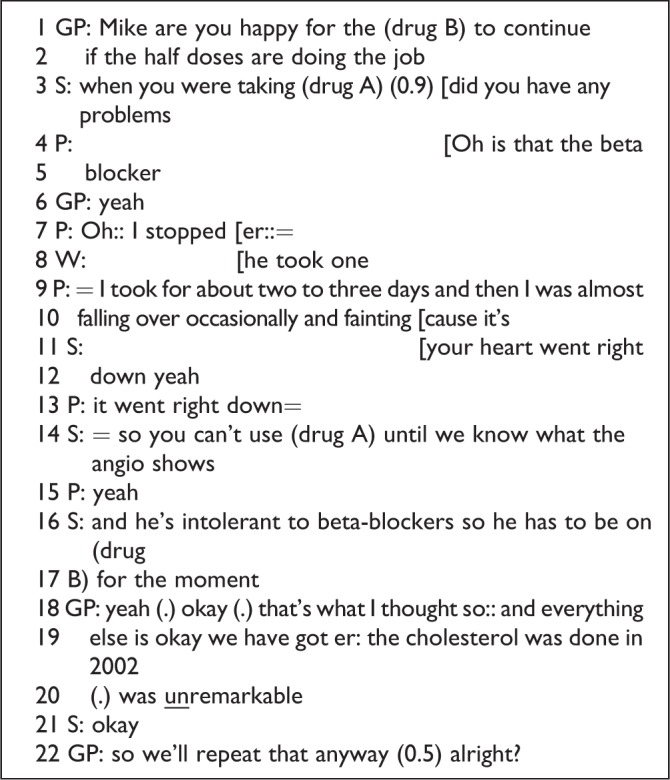
In lines 1 and 2 of extract 9 (Figure 9), the GP produces a clarifying query to address medication: “Mike are you happy for the (drug B) to continue if the half doses are doing the job.” The specialist involves the patient in the discussion in line 3: “When you were taking (drug A) (0.9) did you have any problems.” However, the consultant’s request for more information involves the patient only intermittently before the professionals return to an interprofessional mode to address the GP’s clarifying query. Although from lines 3 to 15 the patient participates in the discussion, his participation serves the purposes of information gathering, as when the specialist collects enough information to make a decision he switches back to addressing the GP in line 16 and 17 by referring to the patient as “he” and make him exogenous to the rest of the discussion and decision-making: “and he’s intolerant to beta-blockers so he has to be on (drug B) for the moment.” Finally, following the GP’s summarizing formulation in lines 18 to 20: “yeah (.) okay (.) that’s what I thought so:: and everything else is okay we have got er: the cholesterol was done in 2002 (.) was unremarkable,” the specialist and the GP decide on the plan of action.
Extract 9 (Figure 9) exemplifies this ability of the participants to readily switch between consultative and interprofessional talk. The impediment to communication and to what is considered mutuality in decision-making arrives from the local organization of turn taking. For example, the patient-consultant-patient sequence of lines 13-14-15 shifts into consultant-GP-specialist sequence initiated in lines 16-18-21 when the specialist refers to the patient as “he.” Nonetheless, it is this shift which makes the patient uninvolved in decision-making.
Discussion and Conclusions
It is very rare for health-care professionals from primary care and tertiary care to verbally communicate during the examination and decision-making phases while the patient is present. Communication typically takes place through letters to inform each other about the progress of patients and/or request for consultation appointments. Telemedicine achieves a convergence of health-care sectors and brings professionals from the 2 pathways in direct contact. Telemedicine allows professionals to exchange important information with regard to the history of the patient and previous tests and to consider the patients’ concerns under a shared model of care for diagnosis and treatment. During telemedicine encounters, primary care nurses (involved during physical examination as well as in diagnosis and decision-making phases) and GPs have a unique opportunity to take part in a consultation and develop their skills. Patients may require support in the use of telemedicine to maximize their contribution to the consultation and ensure that their voice is heard among a group of clinicians, a situation which can often be disempowering to the lone patient. On the whole, there is lack of holistic support and training for all actors involved in the use of telemedicine and training should not only focus on the technical aspects of using telemedicine equipment but also on the process of communication and shared decision-making within this environment.
Under the shared system of care, nurses also contribute to examination, diagnosis, and decision-making by offering knowledge specific to the primary care. For example, proposing a made-to-measure pressure relief stocking to meet the patient’s requirements and alleviate any discomfort for the patient, see discussion of extract 2 (Figure 2); although not a highly specialized management plan, it is perhaps one that the specialist would not have considered as a possible plan because of lack of specific knowledge or because such an approach falls outside the boundaries of her responsibilities.
Under the shared system of care that telemedicine makes available, the patient may be under the care of a number of professionals. Although telemedicine may be a shared care environment that is characterized by collaborative interaction between all participants, there is a risk that interprofessional interaction might exclude the patient from important aspects of the consultation. The analysis of telemedicine consultations revealed that because the nurse and the specialist or the GP and the specialist engage in extensive interprofessional talk, the patient assumes the role of over hearer of the consultation. In televascular consultations, where the nurse is present, interprofessional talk is established because of the extensive involvement of the nurse in physical examination and therefore extensive interaction between the nurse and the specialist during that phase. Subsequently, the interprofessional channel remains, by default, active during negotiation of treatment as well. In telecardiology consultations, where the GP is present, interprofessional talk is initiated by means of formulations produced by the GP. GPs’ formulations are used as summarizing or closure devices of local topics or the consultation as a whole (42).
In contrast to the fears that real-time telemedicine constitutes a type of communication which impedes interaction between the participants because of the intrinsic affordances of video-mediated communication (43,44) and physical proximity and camera angle (45), participants show great ability in switching between modes of interaction. Nonetheless, it is this switching which makes the patient uninvolved in decision-making. For example, in extract 8, the participants showed great skill in switching between consultative and interprofessional talk, and as a result, the patient did not actively participate in the decision-making process.
Limitations and Future Research
Although the results provide some useful insights for those engaged in telemedicine consultations, the sample for the study was small and, therefore, the generalizability of findings to other telemedicine settings requires careful assessment. Also, the sample was entirely drawn from NHS settings in the United Kingdom. Participant interactional strategies, organizational settings, and care pathways are particular to the United Kingdom and, therefore, identified outcomes may not apply to health-care systems of other countries. Further research may be needed to illuminate the strategies of participants in the opening phases of telemedicine consultations in other countries.
Future research studies, given the findings of the present study about the importance of introducing a third person in telemedicine, could usefully control for this in a comparative study of telemedicine and FTF consultations involving 2 health-care professionals and a patient, if such events could be found occurring naturally.
Author Biographies
Yannis Pappas is the director of the Research Centre for Health Service Organisation and Delivery and Reader in the University of Bedfordshire. His interests are in eHealth, applied health services research and optimisation of care delivery.
Jitka Vseteckova is a senior lecturer in Health and Social Care with the Open University. Her research focuses on health policy and planning, education and improvement of care and the development of evidence base in health and social care.
Nikolas Mastellos is a research fellow in eHealth and Health Services Research with Imperial College London. His research focuses on the application of digital health technologies in clinical research and practice and the design and conduct of clinical trials.
Geva Greenfield is a research fellow at Imperial College London. His interests are in integrated care, patient safety, prevention of long-term conditions, adherence to clinical practice guidelines, adherence to medications, and second opinion consultations.
Gurch Randhawa is a professor of Diversity in Public Health and Director of the Institute for Health Research at the University of Bedfordshire. He is also the director of the Organ Donor and Transplant Research Centre and Fellow with the Faculty of Public Health in the UK.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Barlow J, Bayer S, Curry R. Implementing complex innovations in fluid multi-stakeholder environments: experiences of ‘telecare’. Technovation. 2006;26:396–406. [Google Scholar]
- 2. May C, Harrison R, MacFarlane A, Mair F, Wallace P. Why do telemedicine systems fail to normalise as stable models of service delivery? J Telemed Telecare. 2003;9:S25–6. [DOI] [PubMed] [Google Scholar]
- 3. Broens THF, Huis in’t Veld MA, Vollenbroek-Hutten MMR, Hermens HJ, van Halteren AT, Nieuwenhuis LJM. Determinants of successful telemedicine implementations: a literature study. J Telemed Telecare. 2007;13:303–9. [DOI] [PubMed] [Google Scholar]
- 4. Miller EA. The technical and interpersonal aspects of telemedicine: effects on doctor-patient communication. J Telemed Telecare. 2003;9:1–7. [DOI] [PubMed] [Google Scholar]
- 5. Crawford M, Rutter D, Manley C, Weaver T, Bhui K, Fulop N, et al. Systematic review of involving patients in the planning and development of health care. BMJ. 2002;325:1263–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Street RL, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ Couns. 2009;74:295–301. [DOI] [PubMed] [Google Scholar]
- 7. Miller EA. Telemedicine and doctor-patient communication: an analytical survey of the literature. J Telemed Telecare. 2001;7:1–17. [DOI] [PubMed] [Google Scholar]
- 8. Buzug MT, Handels H, Holz D. Telemedicine: Medicine and Communication. New York, NY: Plenum Publishers; 2000. [Google Scholar]
- 9. Darkins AW, Cary AM. Telemedicine and Telehealth: Principles, Policies, Performance and Pitfalls. London: Free Association Books; 2000. [Google Scholar]
- 10. Ferrer-Roca O, Sosa-Iudicissa M. Technology and Informatics: Handbook of Telemedicine. Oxford: IOS Press; 1998. [Google Scholar]
- 11. Bashshur R, Shannon G, Krupinski E, Grigsby J. The taxonomy of telemedicine. Telemed J E Health. 2011;17:484–94. [DOI] [PubMed] [Google Scholar]
- 12. Johnston B, Wheeler L, Deuser J. Outcomes of the Kaiser Permanente tele-home health research project. Arch Family Med. 2000;9:40–5. [DOI] [PubMed] [Google Scholar]
- 13. Roine R, Ohinmaa A, Hailey D. Assessing telemedicine: a systematic review of the literature. CMAJ. 2001;165:765–71. [PMC free article] [PubMed] [Google Scholar]
- 14. Whitten P, Mair F, Haycox A, May C, Williams T, Hellmich S. Systematic review of cost effectiveness studies in telemedicine interventions. BMJ. 2002;324:1434–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Agha Z, Schapira RM, Laud PW, McNutt G, Roter DL. Patient satisfaction with physician–patient communication during telemedicine. Telemed J E Health. 2009;15:830–9. [DOI] [PubMed] [Google Scholar]
- 16. Dick PT, Filler R, Ravan A. Participant satisfaction and comfort with multi-disciplinary pediatric telemedicine consultations. J Pediatr Surg. 1999;34:137–41. [DOI] [PubMed] [Google Scholar]
- 17. Harrison R, Clayton W, Wallace P. Virtual outreach: a telemedicine pilot study using a cluster randomised control design. J Telemed Telecare. 1999;5:126–30. [DOI] [PubMed] [Google Scholar]
- 18. Wakefield DS, Kienzle MG, Zollo SA, Kash J, Band Uden-Holman J. Healthcare providers’ perceptions of telemedicine services. J Telemed Telecare. 1997;3:59–65. [DOI] [PubMed] [Google Scholar]
- 19. Finch T, May C, Mair F, Mort M, Gask L. Integrating service development with evaluation in telehealthcare: an ethnographic study. BMJ. 2003;327:1205–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hibbert D, Mair FS, May CR, Boland A, O’Connor J, Capewell S, et al. Health professionals’ responses to the introduction of a home telehealth service. J Telemed Telecare. 2004;10:226–30. [DOI] [PubMed] [Google Scholar]
- 21. Mair FS, Goldstein P, May C, Angus R, Shiels C, Hibbert D, et al. Patient and provider perspectives on home telecare: preliminary results from a randomized controlled trial. J Telemed Telecare. 2005;11:95–7. [DOI] [PubMed] [Google Scholar]
- 22. Pappas Y, Seale C. The opening phase of telemedicine consultations: an analysis of interaction. Soc Sci Med. 2009;68:1229–37. [DOI] [PubMed] [Google Scholar]
- 23. Whitten P, Sypher BD, Patterson JD. Transcending the technology of telemedicine: a case study in North Carolina. J Health Commun. 2000;12:109–35. [DOI] [PubMed] [Google Scholar]
- 24. Stewart M, Brown J. Patient-centredness in medicine In: Edwards A, Elwyn G. (eds). Evidence-Based Patient Choice. London: Oxford University Press; 2001. [Google Scholar]
- 25. Harris M, Greaves F, Patterson S, Jones J, Pappas Y, Majeed A, et al. The North West London Integrated Care Pilot—innovative strategies to improve care coordination for the elderly and people with diabetes. J Ambul Care Manage. 2012;35:216–25. [DOI] [PubMed] [Google Scholar]
- 26. Greenfield G, Ignatowicz AM, Belsi A, Pappas Y, Car J, Majeed A, et al. Wake up, wake up! It’s me! It’s my life! Patient narratives on person-centeredness in the integrated care context: a qualitative study. BMC Health Serv Res. 2014;14:619–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Elwyn G, Laitner S, Coulter A, Walker E, Watson P, Thomson R. Implementing shared decision making in the NHS. BMJ. 2010;341:971–5. [DOI] [PubMed] [Google Scholar]
- 28. Stevenson FA, Barry CA, Britten N, Barber N, Bradley CP. Doctor-patient communication about drugs: the evidence for shared decision making. Soc Sci Med. 2000;50:829–40. [DOI] [PubMed] [Google Scholar]
- 29. Pappas Y, Seale C. The physical examination in telecardiology and televascular consultations: a study using conversation analysis. Soc Sci Med. 2010;81:113–8. [DOI] [PubMed] [Google Scholar]
- 30. Loane M, Wootton R. A review of guidelines and standards for telemedicine. J Telemed Telecare. 2002;8:63–71. [DOI] [PubMed] [Google Scholar]
- 31. Aas IHM. A qualitative study of the organizational consequences of telemedicine. J Telemed Telecare. 2001;7:18–26. [DOI] [PubMed] [Google Scholar]
- 32. Miller EA. The continuing need to investigate the nature and content of teleconsultation communication using interaction analysis techniques. J Telemed Telecare. 2011;17:55–64. [DOI] [PubMed] [Google Scholar]
- 33. Ten Have P. Methodological issues in conversation analysis; 1990. Retrieved February 27, 2018, from: http://www.ai.univparis8.fr/corpus/papers/tenHave/mica.htm.
- 34. Atkinson JM, Heritage J. Structures of Social Action: Studies in Conversation Analysis. Cambridge: Cambridge UP; 1984. [Google Scholar]
- 35. Maynard DW, Heritage J. Conversation analysis: doctor–patient interaction and medical communication. Med Educ. 2005;39:428–35. [DOI] [PubMed] [Google Scholar]
- 36. Silverman D. Interpreting Qualitative Data: Methods for Analysing Talk, Text and Interaction. London: Sage Publications; 2001. [Google Scholar]
- 37. Mangione-Smith R, Stivers T, Elliott M, McDonald L, Heritage J. Online commentary during the physical examination: a communication tool for avoiding inappropriate antibiotic prescribing? Soc Sci Med. 2003;56:313–20. [DOI] [PubMed] [Google Scholar]
- 38. McCabe R, Heath C, Burns T, Priebe S. Engagement of patients with psychosis in the consultation: conversation analytic study. BMJ. 2002;325:1148–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Seale C, Chaplin R, Lelliott P, Quirk A. Antipsychotic medication, sedation and mental clouding: an observational study of psychiatric consultations. Soc Sci Med. 2007;65:698–711. [DOI] [PubMed] [Google Scholar]
- 40. Tapsell L, Brenninger V, Barnard J. Applying conversation analysis to foster accurate reporting in the diet history interview. J Am Diet Assoc. 2000;100:818–24. [DOI] [PubMed] [Google Scholar]
- 41. Garfinkel H, Sacks H. On formal structures of practical actions 1970. In: McKinney JD, Tiryakian EA. (eds). Theoretical Sociology. New York: Appleton-Century-Crofts, Republished in H. Garfinkel, ed; 1986:337–366. Ethnomethodological Studies of Work London: Routledge & Kegan Paul; 157–189. Heritage, John; 2016. [Google Scholar]
- 42. Gafaranga J, Britten N. Formulations in general practice consultations. Text & Talk. 2004;24:147–70. [Google Scholar]
- 43. Olson J, Olson G, Meader D. Face-to-face group work compared to remote group work with and without video In: Finn KE, Sellen AJ, Wilbur SB. (eds). Video-Mediated Communication. Mahwah: Lawrence Erlbaum Associates; 1997. [Google Scholar]
- 44. Bowers J, Pycock J, O’Brien J. Talk and embodiment in collaborative virtual environments. In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems: Common Ground Vancouver, Canada; 1996:58–65. [Google Scholar]
- 45. Boudourides M. Social impacts of reach media: from video-mediated communication to virtual collaborative environments. 2000. Paper presented at: I Reunion de Informatica y Etica Internet: Autopista de la informacion o comercio electronico, December 19-20, 2000; San Sebastian, Spain: Facultad de Informatika, Universidad del Paıs Vasco. [Google Scholar]


