Abstract
Background
Tibial plateau fractures are complex and may result in sub-optimal results despite a timely and excellent reduction. An important cause for this may be the inability to detect and correct sagittal malalignment consequent to a reversal of the posterior tibial slope. We describe here the surgical steps to restore posterior tibial slope in a series of our patients with tibial condyle fractures involving the posterior column fragment using a fixed-angle locking plate.
Methods
This was a prospective cohort study of 4 cases who had sustained closed, bicondylar tibial plateau fractures (AO/OTA 41-C3) involving the posterior column fragment and reversed sagittal slope. All patients were operated in a prone position through a posterior approach. The fixation was done with a fixed angle locking plate.
Results
The average time taken for fracture union was 12 (range 10–15) weeks. The posterior tibial slope was restored in all the four patients (mean posterior proximal tibial angle = 8.5°, mean medial proximal tibial angle = 88°). There were no procedure-related complications. All patients attained excellent Knee Society Score at one year follow up (mean score = 93).
Conclusion
A posterior approach in the prone position gives direct access to the fracture apex which eases the fracture reduction and fixation to correct the sagittal malalignment in tibial condyle fractures involving the posterior column fragment. We propose this approach as an critical surgical technique which helps in improved outcomes of tibial condylar fractures.
Keywords: Tibial plateau fracture, Posterior column fracture, Coronal plane fracture, Tibial slope, Sagittal alignment
1. Introduction
Tibial condyle fractures are known for their complex management. Complex bicondylar fractures with separation of the articular portion from its metaphysis or diaphysis and alteration in the slope of the tibial articular surface (Schatzker type VI) constitute nearly one-fifth (20%) of the tibial plateau fractures and are the most challenging fracture patterns [1]. These fractures are commonly a result of very high energy trauma and present with significant soft tissue injuries. The focus of initial management is soft tissue care and limb survival. The next challenge is to restore articular congruency and articular alignment. Anatomically, posterior tibial slope plays a vital role in the normal knee function and its stability [2,3]. It is also crucial for normal-weight transfer, range of motion at the knee, and sagittal plane stability [4]. Alteration in the posterior tibial slope may affect tibial scissoring forces, anterior tibial translation, and the force on the anterior cruciate ligament. Therefore, an altered or reversed posterior tibial slope may lead to poor outcome in tibial condylar fractures despite a sound articular reduction and a sound union of the fracture [5,6].
Looking at the burden of this problem at our center, we developed a strategic, feasible, and patient-tailored surgical approach to correct the posterior tibial slope. We prospectively applied this strategy in four patients, who had sustained complex bicondylar fractures of the proximal tibia with reversal of the standard posterior sagittal slope and had intact posterior cortical hinge for correction. The improved outcomes in our patients point towards the utility of this simple and feasible approach, especially in the over-burdened trauma centers in the developing countries and pave the way for more extensive clinical studies.
2. Materials and methods
Our center is a tertiary-level referral center catering to the vast majority of trauma patients from all of Northern and Central India. The annual burden of fractures in our trauma center is nearly 3200 patients with 600 knee injuries, including 80–100 closed tibial plateau fractures. In the Year 2015, from January to December, we identified 14 patients, who had reversed tibial slope. Of these, four patients had an intact posterior cortical hinge amenable to indirect reduction by our technique. These patients were selected as cases for the current study and were prospectively followed-up for outcome assessment. The study was approved by the Institutional ethics committee and the departmental review board. A written and informed consent was sought before enrolment for the study.
All clinical demographics, radiological, and surgical details were recorded in a pre-structured proforma. All four patients had sustained closed, bicondylar, tibial plateau fractures(AO/OTA 41-C3) with a reversed sagittal slope of the posterior column fragment and, an intact posterior cortical hinge and anterior commination. All cases underwent the initial management in the emergency room as per the institutional protocol for triage and damage control, followed by a definitive treatment in the form of open reduction and internal fixation between 7 and 42 days of the injury.
Pre-operative evaluation: All patients underwent plain radiograph, and computed tomography (CT) scans as part of the pre-surgical evaluation. CT helps in identifying the fracture plane with detailed three-dimensional orientation and planning fracture-specific and fragment-specific management. Involvement of the posterior column was identified, and the posterior proximal tibial angle was measured. The fractures were classified according to Schatzker, AO/OTA, and the three-classification systems and subsequent surgical plans were made.
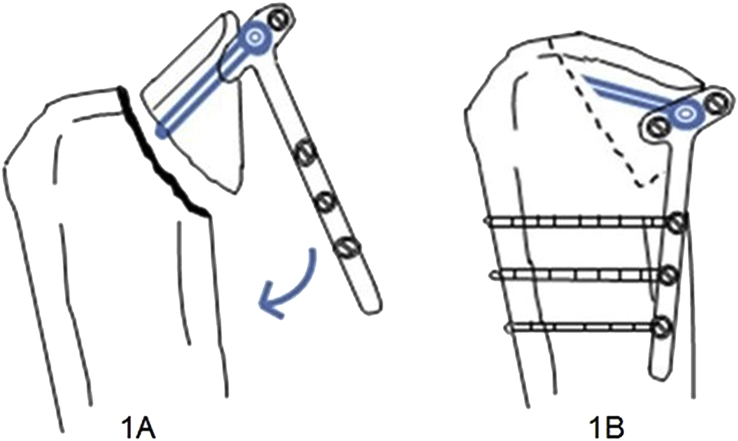
Surgical technique: Under general anesthesia, the patients were placed in a prone position. The fracture was accessed via a posterior approach as described in detail by Chouhan et al. [7]. The posterior column fragment was identified and manipulated to check the mobility and reducibility using a K-wire as a joystick (Fig. 1A). Subsequently, the articular fragment was fixed with locking screws inserted, through the horizontal limb of a fixed angle T-plate, parallel to the articular surface. The long arm of the plate was brought down to the posterior tibial diaphysis with the posterior fracture apex as a fulcrum and subsequently fixed with cortical screws (Fig. 1B). This maneuver disimpacted the anterior cortex and restored the normal posterior sagittal slope of the fragment. Any associated anterior rim fragment also fell into place with the correction of the articular slope. A lateral/medial column locking plate was applied to provide coronal stability to the construct with the patient in the same position with different incisions except in case-2.
Fig. 1.
(A) Schematic diagram of posterior column articular fragment fixed with locking screws through the horizontal limb of a fixed angle T-plate, parallel to the articular surface. (B) The long limb of the plate brought down to the posterior tibial diaphysis with the posterior fracture apex as fulcrum and fixed with cortical screws.
Parameters used to assess adequate fixation include articular reduction with <2 mm of articular step, coronal alignment with medial proximal tibial angle (MPTA) of 87 ± 5°, and condylar width within 5mm of the healthy side. Sagittal plane alignment, which is essential for the stability of the knee joint, should ideally be 9 ± 5° [3]. The concomitant ligament injury and meniscus problems were addressed according to the standard treatment protocols of the Department. Postoperatively, dressings were changed on day 2 and 4; an active range of motion (0–30°) was started as soon as the patients were out of pain. Progressively increasing range of motion exercises were introduced gradually in congruence with the patient's tolerance. Patients were allowed to move out of the bed with crutches with subsidence of pain. They have advised an initial non-weight bearing movement till six weeks and then, partial weight bearing for the next six weeks.
Follow-up: All patients were followed up for a minimum of 6 months for fracture healing and any loss of reduction. The functional outcome was assessed using the Knee Society Scoring system (KSS). Coronal plane alignment of the tibial articular surface was measured by the medial proximal tibial angle (MPTA) and sagittal alignment by the posterior proximal tibial angle (PPTA). All the measurements were done at the time of presentation and after healing of the fracture.
3. Results
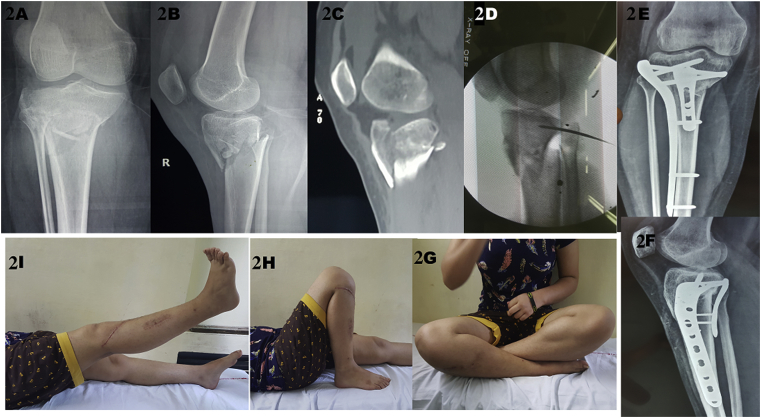
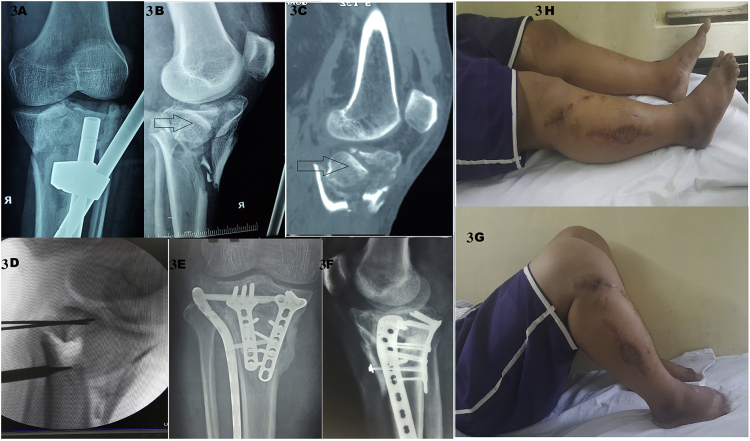
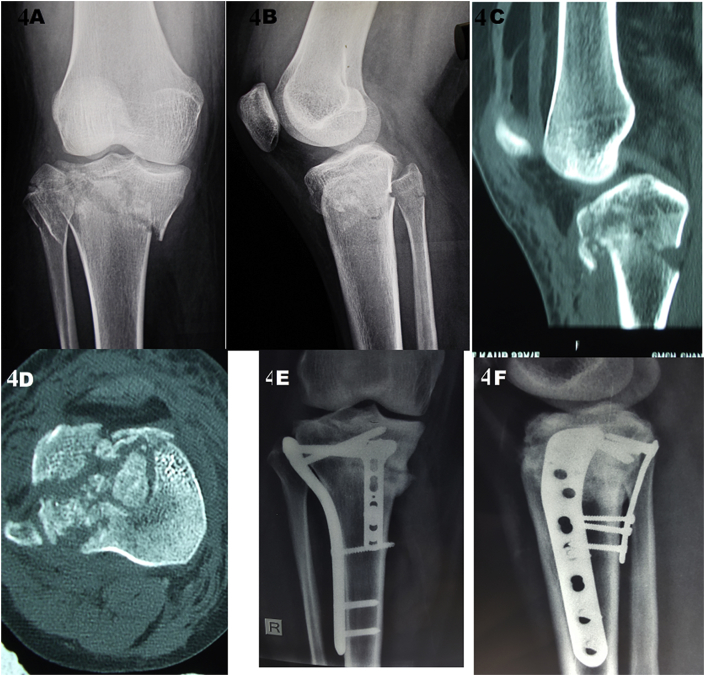
The baseline clinical and surgical data has been summarized in Table 1. Pre and post-operative radiographic features of the fractures in the four patients are depicted in Fig. 2, Fig. 3, Fig. 4, Fig. 5. All four patients showed radiological union at an average of 12 weeks (10–15 weeks) post-surgery (Table 2). The ‘restored’ posterior tibial slope (mean PPTA = 8.5°, mean MPTA = 88°) was maintained till final follow up. The mean knee flexion was 133°. Articular malreduction (>2mm step-off) was noted in one patient (case 2). There were no approach-related complications recorded in this series. All patients attained excellent KSS (mean score = 93) at one year of follow-up. All patients were able to sit cross-legged, squat, and carry out their daily activities without any pain or symptoms of instability in their knees.
Table 1.
Clinical summary of all four cases.
| Case no. | Age | Gender | Mode of injury | Condition of limb at initial presentation | Initial management | Final management and Duration of Surgery |
|---|---|---|---|---|---|---|
| 1 | 22 | F | RSA | Mild swelling no compartment syndrome | Distal tibial skeletal traction | Definitive fixation on 7th day, duration of surgery was 65 min. |
| 2 | 43 | M | RSA | Compartment syndrome | Fasciotomy and spanning external fixator | Fasciotomy wound closure on medial side and lateral side split skin grafting at 18 days final fixation done in 2 stage. At 6 weeks posterolateral and posteromedial fragment stabilized with fragment specific angle stable plate in prone position using posterior midline approach, 5 day later anterolateral plating done, duration of surgery was 105 min and 45 min in second surgery. |
| 3 | 24 | F | RSA | Mild swelling no compartment syndrome | Distal tibial skeletal traction | Definitive fixation on 7th day and duration of time was 75 min. |
| 4 | 35 | M | RSA | Grossly swollen limb with knee subluxation without compartment syndrome | Close reduction and spanning external fixator | Definitive fixation on 10th day and duration of surgery was 80 min. |
| Mean Surgery Time | 92.5 min. | |||||
M – Male, F – Female, RSA – Road side accident.
Fig. 2.
Case 1 - (A, B, C) Pre-operative AP and lateral radiographs and sagittal cut of CT scan showing the reversal of sagittal slope of the coronal split posterolateral fragment. (D). Fluoroscopic image of the patient showing correction of the posterior tibial slope using a K-wire as a joystick. (E, F). Restoration of posterior sagittal slope with posterior locking plate fixation (solid arrow) and lateral fixed angle plate fixation (dotted arrow). (G, H, I). Clinical outcome of the operated knee.
Fig. 3.
Case 2 - (A, B, C). Radiograph and CT scan showing complex tibial plateau fracture with spanning external fixator; Arrow showing the reversed sagittal slope of the coronal split posterolateral fragment. (D). K-wire is used to check the reducibility. (E, F). Two locking T-plates are applied to the posterolateral and posteromedial fragments; shown by arrows. Delayed definitive fixation has led to suboptimal correction. (G, H). Clinical outcome and the healed fasciotomy wound.
Fig. 4.
Case 3 - (A, B). Plain radiographs showing complex bicondylar fracture with reversed tibial slop. (C, D). Sagittal and axial CT scan images showing a large posteromedial fragment. (E, F). Posteromedial locking plate and lateral column plate with restored posterior slope.
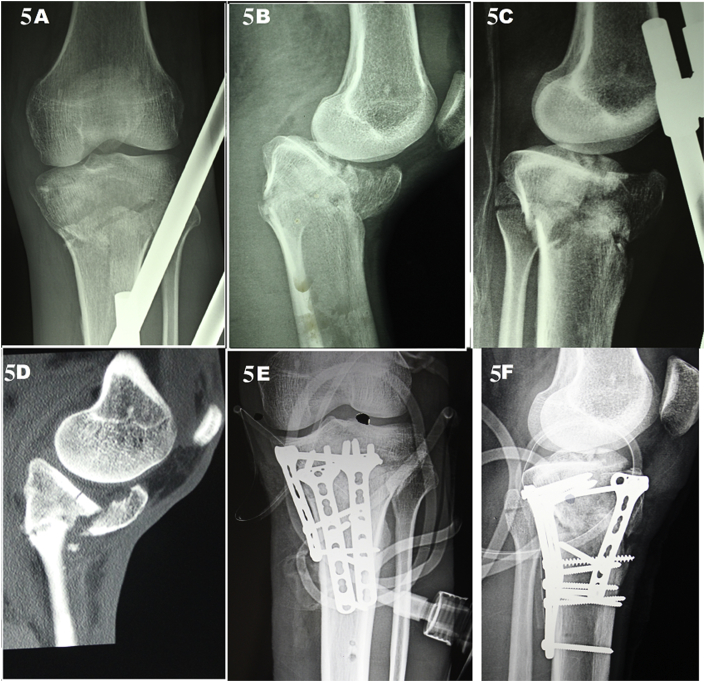
Fig. 5.
Case 4 (A) Plain radiograph anteroposterior view showing complex bicondylar fracture. (B, C) Lateral radiograph before and after spanning external fixator – showing reversed tibial slop and anterior comminution. (D) Sagittal cut of CT scan showing the reversed tibial slope. (E, F). Post-operative radiograph showing well fixed fracture with corrected slop.
Table 2.
Radiological and functional outcome.
| Case | Time for bony union (weeks) | MPTA | PPTA | Knee range of motion | KSS |
|---|---|---|---|---|---|
| 1 | 13 | 89° | 11° | 0–135° | 95 |
| 2 | 15 | 91° | 4° | 0–125° | 85 |
| 3 | 11 | 85° | 10° | 0–140° | 100 |
| 4 | 10 | 87° | 9° | 0–130° | 90 |
| Mean | 12 | 88° | 8.5° | 133° | 93 |
MPTA: medial proximal tibial angle, PPTA: posterior proximal tibial angle, KSS: knee society score.
4. Discussion
Despite the widely discussed importance of maintenance of tibial slope during the management of ligament injuries, limited work is available on the optimal alignment in the sagittal plane while correcting proximal tibial plateau fractures. Our paper highlights that a fracture-specific surgical exposure and fixation of the posterior column as a priority while managing tibial plateau fractures with reversal of the tibial slope, leads to improved functional outcomes. Our technique is simple, feasible, and applicable even in the busy trauma centers with limited expertise.
Erdil et al. evaluated the effect of the posterior tibial slope after fracture healing on the anteroposterior knee laxity, functional outcomes, and patient satisfaction in 126 patients of proximal tibial fracture treated at their institute [8]. The authors found a statistically significant anteroposterior laxity on the treated side as compared to the healthy side with no significant differences in the posterior tibial slope. They concluded that sagittal alignment is reasonably vital for stability and should not be ignored [8]. While looking at functional outcomes after dual plating for bicondylar tibial plateau fractures, Bareiet al. elaborated that these patients demonstrate substantial residual functional dysfunction after treatment compared with the general population. The poor outcome was postulated to be due to the absence of satisfactory sagittal plane alignment in as high as one-third (32%) of the patients [2,9].
The current management of proximal tibia fractures relies on understanding the complexity of the fracture, which has been revolutionized by the computed tomography-based three-column classification [10,11]. The CT based classifications improved the understanding of the fracture morphology and allowed a more strategic approach and fracture-specific management [12,13]. Posterior approach and prone positioning ease the correction of the sagittal plane malalignment of the posterior articular fragment. A direct posterior reduction and biological disimpaction of the anterior cortex helps restores the normal tibial slope without any need of bone grafting in most cases. Additionally, the posterior midline gastrocnemius raphe split approach for complex proximal tibial fractures significantly reduces the local wound complications. It is important to note that a conventional fixation with a lateral fixed-angle plate may not provide enough stability to the construct, and may even lead to loss of reduction [14]. Loss of reduction is especially noted in cases with coronal plane fracture of the posterior part of the tibial condyle, because the screws may not cross a large part of the posterior fragment when inserted through the lateral plate [13,15,16]. The application of a plate on the posterior aspect is more fracture specific and ensures a more secure fixation of fractures involving the posterior column [10,11]. Sagittal plane alignment of the articular fragment is essential for good functional outcomes, as excessive posterior slope or reversal of the slope will cause flexion or recurvatum deformities of the knee respectively [3,17].
Firoozabadi et al. proposed the concept of AO/OTA 41C3.3 reverse slope extension fracture in 25 fractures of 23 patients with a reversal of tibial slope as ‘hyperextension-varus injuries’ [18]. These fracture patterns are unique, as they specifically lead to crushing or comminution of the anterior cortex and tension failure of the posterior cortex. They proposed a method to correct the tibial slope which involves reduction from the compressive side that is inevitably comminuted that can make anatomical reduction more challenging with the conventional dual surgical approach with the correction of slope by anterior to posteriorly directed K-wires (joystick), blunt elevators or lamina spreaders aiming for the indirect reduction of the posterior intact cortex [18]. They suggested fixation of this injury complex by buttress plating with a locking implant, supplemented by a more posteriorly placed lateral plate to control the translation [18]. However, the loss of sagittal plane correction in follow-up limits the effectiveness of the study technique employed.
Furthermore, local wound complications occurred in 38% of patients requiring repeat interventions. As a possible solution to several of these problems, our posterior midline approach for fixation in the prone position allows a direct exposure and simple, quick maneuvering of the fracture fragment without the need of bulky spreader and excessive soft tissue retraction which could reduce the risk of local complications. It also allows a direct reduction of the intact posterior tension fracture, and indirect, but more biological disimpaction of the comminuted anterior cortex, thereby reducing the need of bone grafting. Our surgical technique can also be applied in cases with a coronal split of the tibial condyle where exposure and reduction of the posterior fragment may not be possible from the anterior side as seen in case 1 and 2.
We understand that our prospective series has a small number of patients, but we plan to extend this unique strategy in hyperextension type of the posterior condylar fractures as well to improve the functional outcomes. The importance of this technique lies in its feasibility and the ease of patient-specific modifications for optimal functional outcomes. Although case 2 in our series had a malreduction of the anterolateral fragment, probably attributable to the delay of 6 weeks in definitive intervention and an initial compartment syndrome with soft tissue problems, yet the excellent function recovery with KSS of 85 at a follow-up of 8 months was encouraging. The decreased range of movement secondary to low thigh-calf ratio bilaterally in this patient probably led to lower scores.
In conclusion, we propose a fracture-specific, simple, and feasible surgical technique to correct the sagittal plane malalignment of the posterior articular fragment. A direct posterior reduction and biological disimpaction of the anterior cortex restores the standard tibial slope. Fixation of the posterior column first in the management of tibial plateau fractures with reversal of tibial slope improves the clinical and functional outcomes. The use of posterior midline gastrocnemius raphe-split approach also helps in minimizing the local wound complications for complex proximal tibia fractures.
Funding
None.
Declaration of competing interest
None.
Acknowledgment
None.
References
- 1.Schatzker J., McBroom R., Bruce D. The tibial plateau fracture. The Toronto experience 1968--1975. Clin. Orthop. Relat. Res. 1979;(138):94–104. [PubMed] [Google Scholar]
- 2.Streubel P.N., Glasgow D., Wong A., Barei D.P., Ricci W.M., Gardner M.J. Sagittal plane deformity in bicondylar tibial plateau fractures. J Orthop Trauma. 2011;25(9):560–565. doi: 10.1097/BOT.0b013e318200971d. [DOI] [PubMed] [Google Scholar]
- 3.Barei D.P., Nork S.E., Mills W.J., Henley M.B., Benirschke S.K. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma. 2004;18(10):649–657. doi: 10.1097/00005131-200411000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Shelburne K.B., Kim H.-J., Sterett W.I., Pandy M.G. Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res: Off. Publ. Orthop. Res. Soc. 2011;29(2):223–231. doi: 10.1002/jor.21242. [DOI] [PubMed] [Google Scholar]
- 5.Brandon M.L., Haynes P.T., Bonamo J.R., Flynn M.I., Barrett G.R., Sherman M.F. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency Arthroscopy. J. Arthrosc. Relat. Surg.: Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 2006;22(8):894–899. doi: 10.1016/j.arthro.2006.04.098. [DOI] [PubMed] [Google Scholar]
- 6.Senişik S., Ozgürbüz C., Ergün M., Yüksel O., Taskiran E., Işlegen C. Posterior tibial slope as a risk factor for anterior cruciate ligament rupture in soccer players. J Sport Sci Med. 2011;10(4):763–767. [PMC free article] [PubMed] [Google Scholar]
- 7.Chouhan D.K., Dhillon M.S., Puneeth k, Ponnusamy V., Kanaujia R., Prakash M. Gastrocnemius raphe split approach for complex proximal tibia fractures – applicability and advantages. https://www.injuryjournal.com/article/S0020-1383(18)30513-8/fulltext [DOI] [PubMed]
- 8.Erdil M., Yildiz F., Kuyucu E., Sayar Ş., Polat G., Ceylan H.H. The effect of sagittal plane deformities after tibial plateau fractures to functions and instability of knee joint. Acta Chir Orthop Traumatol Cech. 2016;83(1):43–46. [PubMed] [Google Scholar]
- 9.Barei D.P., Nork S.E., Mills W.J., Coles C.P., Henley M.B., Benirschke S.K. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J. Bone Jt. Surg. Am. 2006;88(8):1713–1721. doi: 10.2106/JBJS.E.00907. [DOI] [PubMed] [Google Scholar]
- 10.Luo C.-F., Sun H., Zhang B., Zeng B.-F. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24(11):683–692. doi: 10.1097/BOT.0b013e3181d436f3. [DOI] [PubMed] [Google Scholar]
- 11.Zhu Y., Yang G., Luo C.-F., Smith W.R., Hu C.-F., Gao H. Computed tomography-based Three-Column Classification in tibial plateau fractures: introduction of its utility and assessment of its reproducibility. J. Trauma Acute Care Surg. 2012;73(3):731–737. doi: 10.1097/TA.0b013e31825c17e7. [DOI] [PubMed] [Google Scholar]
- 12.Krause M., Preiss A., Müller G., Madert J., Fehske K., Neumann M.V. Intra-articular tibial plateau fracture characteristics according to the “Ten segment classification”. Injury. 2016;47(11):2551–2557. doi: 10.1016/j.injury.2016.09.014. [DOI] [PubMed] [Google Scholar]
- 13.Adams J.D., Della Rocca G.J. Management of posterior articular depression in tibial plateau fractures. J Knee Surg. 2016;29(1):28–33. doi: 10.1055/s-0035-1566737. [DOI] [PubMed] [Google Scholar]
- 14.Weaver M.J., Harris M.B., Strom A.C., Smith R.M., Lhowe D., Zurakowski D. Fracture pattern and fixation type related to loss of reduction in bicondylar tibial plateau fractures. Injury. 2012;43(6):864–869. doi: 10.1016/j.injury.2011.10.035. [DOI] [PubMed] [Google Scholar]
- 15.Weil Y.A., Gardner M.J., Boraiah S., Helfet D.L., Lorich D.G. Posteromedial supine approach for reduction and fixation of medial and bicondylar tibial plateau fractures. J Orthop Trauma. 2008;22(5):357–362. doi: 10.1097/BOT.0b013e318168c72e. [DOI] [PubMed] [Google Scholar]
- 16.Barei D.P., O'Mara T.J., Taitsman L.A., Dunbar R.P., Nork S.E. Frequency and fracture morphology of the posteromedial fragment in bicondylar tibial plateau fracture patterns. J Orthop Trauma. 2008;22(3):176–182. doi: 10.1097/BOT.0b013e318169ef08. [DOI] [PubMed] [Google Scholar]
- 17.Cole P.A., Zlowodzki M., Kregor P.J. Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma. 2004;18(8):528–535. doi: 10.1097/00005131-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Firoozabadi R., Schneidkraut J., Beingessner D., Dunbar R., Barei D. Hyperextension varus bicondylar tibial plateau fracture pattern: diagnosis and treatment strategies. J Orthop Trauma. 2016;30(5):e152–157. doi: 10.1097/BOT.0000000000000510. [DOI] [PubMed] [Google Scholar]