Abstract
We assessed district-level geospatial trends in precision weighted prevalence and absolute wealth disparity in stunting, underweight, wasting, low birthweight, and anemia among children under five in India. The largest wealth disparities were found for anthropometric failures and substantial variation existed across states. We identified statistically significant (p < 0.001) geospatial patterns in district-wide wealth disparities for all outcomes, which differed from geospatial patterns for the overall prevalence. We characterized each district as either a “Disparity”, “Pitfall”, “Intensity”, or “Prosperity” area based on its overall burden and wealth disparity, as well as discuss the importance of considering both measures for geographically-targeted public health interventions to improve health equity.
Keywords: India, Districts, Geospatial, Child undernutrition, Wealth disparity
Highlights
-
•
District-wide prevalence and wealth disparity in child malnutrition were assessed.
-
•
The largest wealth disparities were found for anthropometric failures.
-
•
Distinct geospatial distribution of wealth disparity was found for different outcomes.
-
•
The correlation between mean prevalence and wealth disparity was moderate to strong for all outcomes, except anemia.
-
•
Both measures are needed for geographically targeted public health interventions to improve health equity.
1. Introduction
Globally, an estimated 230 million children below five years old are chronically malnourished, and more than half of under-five deaths in children are attributable to malnutrition (Van de Poel, Hosseinpoor, Jehu-Appiah, Vega, & Speybroeck, 2007). Numerous studies have consistently found that childhood malnutrition is associated with significantly increased risk of morbidity and mortality in the short-term as well as reduced work capacity and economic productivity in later life (Victora et al., 2008). In particular, India is at the forefront in its battle against child malnutrition. Although there has been a progressive decline in child malnutrition as shown from successive waves of the National Family Health Surveys (NFHS), the decline has been rather slow and malnutrition still continues to be highly prevalent, and improvements have not been equally distributed across the population (International Institute for Population Sciences (IIPS) and ICF, 2017).
The linkage between socioeconomic environments at macro- and micro-levels with child malnutrition has been well-studied. In India, there have been increases in economic inequality at the national level, within and between states, and within and between rural and urban areas (Chalasani & Rutstein, 2014; Deaton & Drèze, 2002; Sen & Himanshu, 2004). While macroeconomic growth is often seen as a major policy instrument in improving child health outcomes, a study by Subramanyam et al. found inconsistent association between changes in state per capita income and childhood malnutrition in India, suggesting the need for more focus at the micro-level instead of the state or national level (Subramanyam, Kawachi, Berkman, & Subramanian, 2011). Chalasani and Rutstein proposed that India's structural adjustment program in the early 1990s resulted in a retreat of state economic supervision which led to micro-level household wealth being a more important determinant of improvement in nutritional status and child survival (Chalasani & Rutstein, 2014).
Indeed, prior studies have consistently reported significant household-level socioeconomic inequality in malnutrition indicators, such as stunting, that has either persisted or increased in middle and low-income countries (Barros et al., 2018). The poorest sector shoulders a disproportionate burden of child malnutrition in India (Mazumdar, 2010). In India (Corsi, Mejía-Guevara, & Subramanian, 2016) and across South Asia (Kim, Mejía-Guevara, Corsi, Aguayo, & Subramanian, 2017), past and present socioeconomic conditions were found to be the strongest predictors of child undernutrition out of a comprehensive set of other known risk factors including those related to environmental and household practices. Household wealth directly affects one's ability to consistently secure food and access proper sanitation and health services, thereby increasing the risk of poor nutrition outcomes in children (Renzaho et al., 2019). Thus, it is important to monitor child malnutrition indicators across different levels of household wealth.
At the same time, existing literature on social determinants of child malnutrition have predominantly focused on nation-wide average associations (Corsi et al., 2016; Kanjilal, Mazumdar, Mukherjee, & Rahman, 2010; Prakash & Kumar, 2013; Subramanian, Ackerson, Davey Smith, & John, 2009; Subramanyam et al., 2011). Yet, national average estimates mask the inequalities amongst districts and socioeconomic classes. For a country as large as India, it is important to continue monitoring the geographical differences in undernutrition (Menon, Headey, Avula, & Nguyen, 2018). In India, districts represent the lowest administrative unit at which infrastructural, developmental, and other services are planned by the elected district councils and where demographic data are consistently provided. In addition, monitoring district-level child undernutrition is particularly important in the context of the Government of India's new initiative POSHAN Abhiyaan, or the National Nutrition Mission (NNM), initiated in 2018. The program aims to annually reduce the levels of stunting, anemia, and low birthweight by 2%, 3%, and 2% respectively in a tri-phase district-based manner (Aggarwal & Kakkar, 2019). Studying undernutrition through a district-level lens is essential for a geographically granular examination of India, which is a country that has tremendous spatial variation in nutrition. While the NFHS-4 does provide estimates of stunting and underweight stratified by wealth quintile, it does not do so for other nutritional outcomes such as anemia nor does it disaggregate them for each of India's 640 districts.
In this paper, we provide precision weighted estimates of the prevalence of five child malnutrition indicators – stunting, underweight, wasting, low birthweight, and anemia – for each of the 640 districts in India by wealth quintiles. Stunting and wasting are proxy indicators for distinct nutritional problems (i.e., chronic vs acute malnutrition) and are useful in assessing overall nutritional health and informing policy decisions and public health programming (Black et al., 2008). Birthweight is also an important marker of child malnutrition at birth and is one of the strongest risk factors associated with child mortality (McCormick, 1985). The most common form of anemia is iron deficiency anemia (IDA), especially in a nutrition deficit context (Anand, Rahi, Sharma, & Ingle, 2014). We comprehensively assess the distribution of burden of child malnutrition and their wealth disparity within and across districts via our precision weighted estimates. Further, we use maps and descriptive analyses to understand geospatial distribution of wealth disparity in child malnutrition in India.
2. Methods
2.1. Data source
The 2015–2016 National Family Health Survey (NFHS-4) is available to be downloaded at https://www.dhsprogram.com/Data/. Unlike previous iterations, the NFHS-4 enables district-level estimations of various population health and nutrition measures for all India, including seven union territories (IIPS and ICF, 2017). In the NFHS-4, stratified two-stage sampling was employed such that villages in rural areas and census enumeration blocks in urban areas were first selected as primary sampling units (PSUs) with a probability proportional to population size. Within selected rural and urban PSUs, households were randomly selected using systematic sampling with probability proportional to segment size (IIPS and ICF, 2017). From these households, data on children born within the past five years were collected.
2.2. Study population
In the NFHS-4, there were 247,743 children aged less than five years alive at the time of survey. Of them 22,741 children (9.2%) were missing anthropometry measures, leaving 225,002 children for the analysis of anthropometric failure outcomes. About a quarter of the children were missing birth weight (N = 60,561, 24.4%), leaving 187,182 children for the analysis of low birth weight. Birth weight data were taken from either written card record (53.2%) or mother's recall (46.8%). Blood hemoglobin measure was available for a total of 209,496 children.
2.3. Outcomes
Five child malnutrition indicators – stunting, underweight, wasting, low birthweight, and anemia – were considered in our analysis as binary outcomes. In the NFHS-4, height was measured as standing height for children older than 2 years and recumbent length for children younger than 2 years (IIPS, 2017). Weight for children older than 2 years was measured standing on a digital weight scale while for children younger than 2 years, they were handed to an examiner standing on the scale tared at zero (IIPS, 2017). Hemoglobin concentration was measured using the HemoCue method in the NFHS-4 (Kalaivani & Ramachandran, 2018). Stunting, an indicator of cumulative malnutrition, was defined as a child's height-for-age z-score more than 2 standard deviations (SDs) below the median of the World Health Organization (WHO) child growth reference standards (WHO, 2006). Wasting, an indicator of acute malnutrition, was defined to be when a child's weight-for-age z-score was 2 SDs below the median. Underweight is a composite indicator of both stunting and wasting, and was defined as weight-for-age z-score < 2 SD. A child was classified as having low birth weight if the birth weight was less than 2500 g. Anemia in children 6–59 months of age at sea level was defined by a blood hemoglobin concentration lower than 11 g/dL.
2.4. Household wealth
In the NFHS-4, the wealth index for a given household was calculated by aggregating its ownership of consumer goods, such as television, bicycle or car, and housing characteristics, such as construction material and type of water access (IIPS and ICF, 2017). Based on these assets, a score was derived for each household using principal component analysis. National wealth quintiles were created by dividing the distribution of household wealth index into five equally sized categories (Rutstein & Johnson, 2004).
2.5. Statistical analysis
Our final analytic sample followed a three-level hierarchical data structure with child i (level-1) nested within district j (level-2) and state k (level-3). We conducted two sets of multilevel logistic regression models for each of our binary outcome Y. First, we ran a null model to calculate the precision weighted probability of outcome Y in each district j:
Multilevel modeling in general provides a technically robust and efficient framework to account for the complex survey design and produces precision weighted estimates for predictions at higher level entities (Bell, Fairbrother, & Jones, 2019; Jones & Bullen, 1994; Subramanian, Delgado, Jadue, Vega, & Kawachi, 2003). In this case, precision weighted district means pool information and borrow strength from other districts that share the same state membership, hence resulting in more reliable estimates. Given (the median log odds of Y across all India), (the state-specific residual representing a differential from the national median and each state k), and (the district-specific residual representing a differential from the state median and each district j), the probability of Y for each district can be calculated as: exp()/(1 + exp()).
Second, we extended the above model to allow the relationship between household wealth quintile and outcome Y to vary across districts. This was done by incorporating random slopes for wealth quintiles (= poorest wealth quintile, …, = richest wealth quintile) at the district level:
In this model, the poorest wealth effect in district j consists of fixed average wealth effect across all districts () and a differential wealth effect that is specific to each district (). Having used separate coding, the probability of Y in district j for the poorest wealth quintile can be calculated as: exp()/(1 + exp()). A similar calculation was done for district-specific probability for other wealth quintiles. This analytical approach produces more stable and accurate predictions in the context of imbalanced data structure (i.e., some districts have very few observations in the highest or the lowest wealth quintile) and where the predictor variable does not vary as much within the unit of interest (i.e., wealth quintile does not vary as much within districts compared to across districts) (Rubin, 1980).
Given these estimates, we conducted the following descriptive and geospatial analyses. First, we computed district-wide summary statistics for wealth disparity in each outcome by taking the absolute percentage point difference between the highest and lowest wealth quintiles. We defined wealth disparity in absolute terms as opposed to relative terms (e.g. ratio) to indicate how large a proportion of the poorest wealth group is affected by greater exposures to diverse risk factors of child undernutrition. The relative difference can be computed from data provided in Supplementary. The distributions of district-wide wealth disparity in malnutrition outcomes, for all India and by each state, were presented in boxplots. Second, we mapped district-averaged prevalence and wealth disparity in each outcome using quintile classification. This method allowed identification of geographical hotspots of districts at the extremes of the spectrum. We used blue shades to indicate low prevalence or wealth disparity and red to indicate the opposite. The correlation between district prevalence and wealth disparity was also assessed for all outcomes.
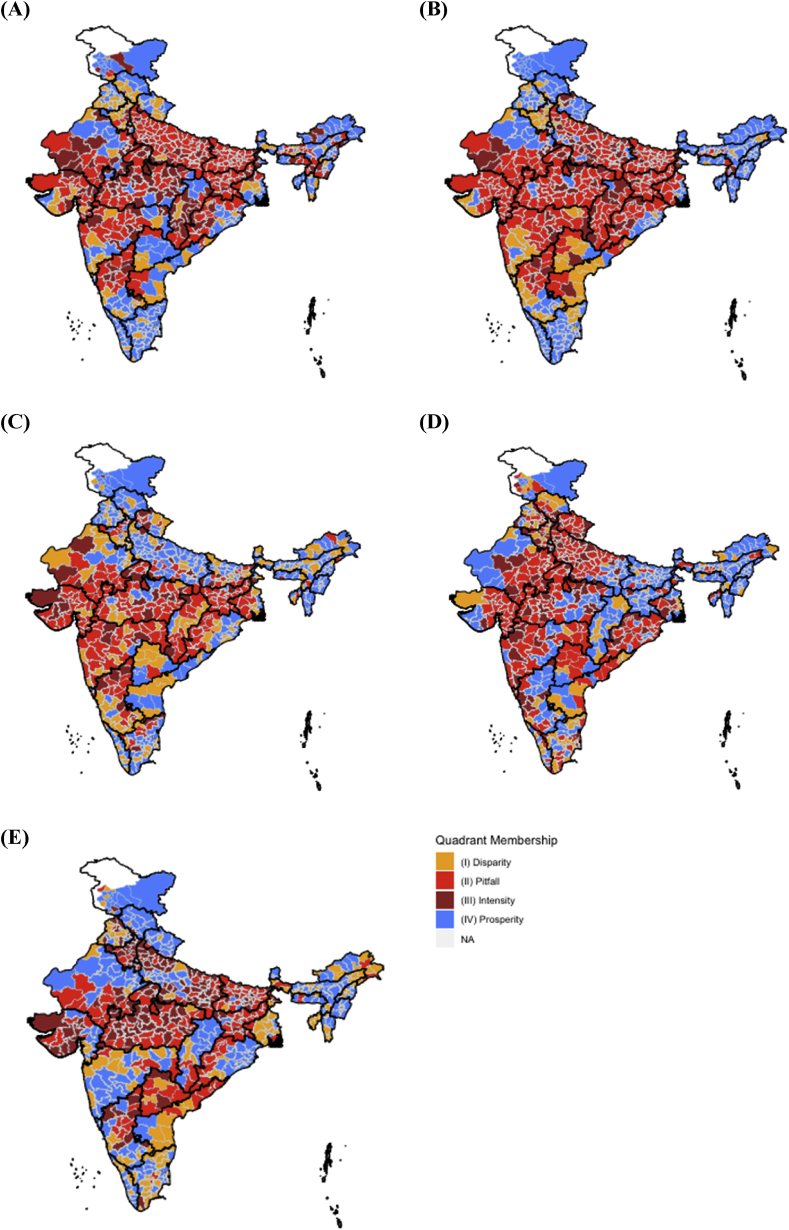
Third, we adopted a “quadrant analysis” method from Mazumdar except we used overall averages as quadrant demarcations instead of medians (Mazumdar, 2010). We did so because when visualizing the district-level prevalences and wealth disparities in a scatter plot, it was difficult to discern the patterns of how districts fared relative to each other without the assistance of guidelines. Thus, the average prevalence as well as the average wealth disparity act as thresholds, with values above characterized as “high” and those below characterized as “low”. The “Disparity” quadrant was characterized by low prevalence and high wealth disparity. This is a concerning quadrant regarding inequality because this means that even in well performing districts, there can be gross inegalitarian malnutrition outcomes. The “Pitfall” quadrant was characterized by high prevalence and high wealth disparity. The “Intensity” quadrant was defined by high prevalence and low wealth disparity, usually corresponding to poorer districts. The “Prosperity” quadrant was characterized by low prevalence and low wealth disparity. The distribution of these four quadrants were visualized in maps.
Lastly, we computed a Moran's I Index, which is an autocorrelation coefficient that tests how likely geospatial clusters could have appeared by chance for wealth disparity. We defined a geospatial cluster, or neighborhood, as a set of contiguous districts that share boundaries with other districts. Not all neighborhoods were of the same size. After defining neighborhoods, we computed the average wealth disparity of each neighborhood cluster (wealthrangelag). We performed a Monte Carlo test where wealthrangelag values were randomly assigned to spatial polygons in our dataset, and for each permutation, a Moran's I value was computed as:
where is the number of polygons (districts in this case), is wealthrange, is average wealthrange, is a matrix of spatial weights, and is the sum of all . We then compared our observed Moran's I to the sampling distribution of bootstrapped Moran's I where the null hypothesis was that wealthrangelag is randomly distributed across the polygons. Lastly, we performed Local Indicator Spatial Association (LISA) cluster map analysis with a Bonferroni-adjusted level of significance to control for Type I error (Anselin, L., 1995) in order to identify statistically significant clusters of high burden and low burden districts for each undernutrition indicator.
Multilevel modeling was performed in the MLwiN 3.0 software program via Monte Carlo Markov Chain (MCMC) methods using Gibbs sampler with the default prior distributions of IGLS estimations as starting values, a burn-in of 500 cycles, and monitoring of 5000 iterations of chains (Browne, 2019; Charlton, Rasbash, Browne, Healy and Cameron, 2019). All descriptive analyses and geospatial analysis were performed using R 3.5.3.
3. Results
3.1. District-wide wealth disparities in child malnutrition: A national view
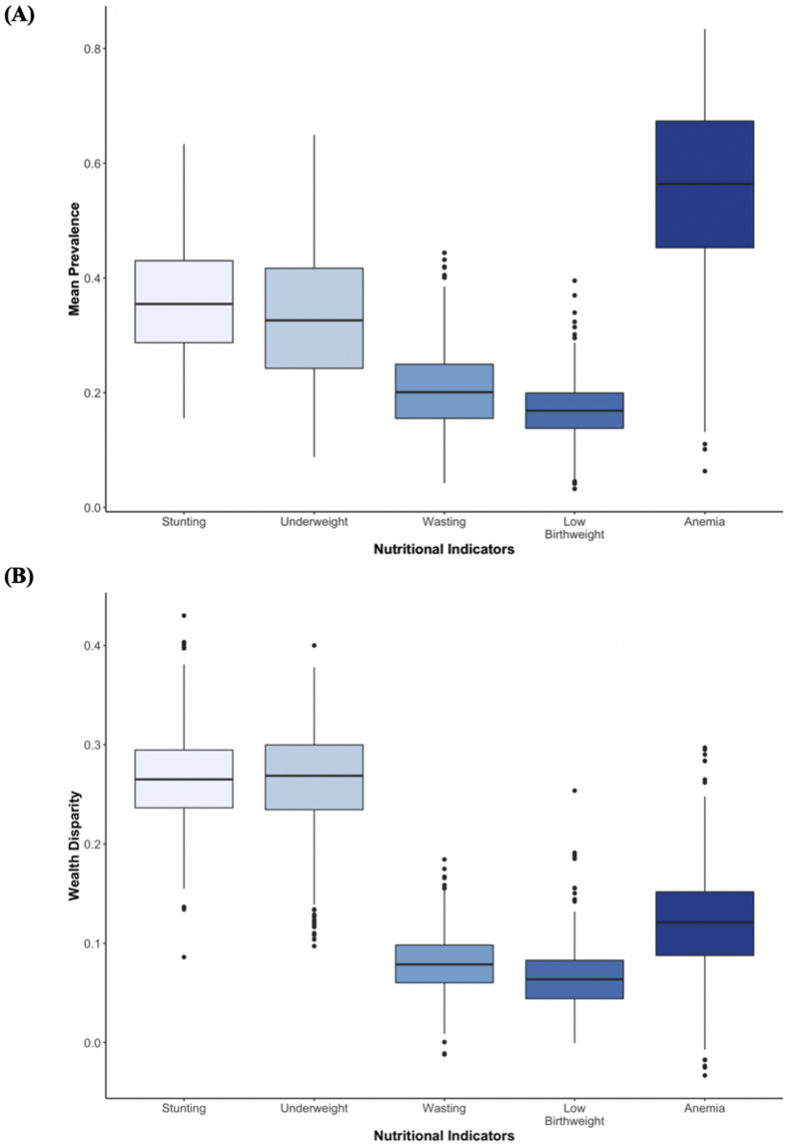
Fig. 1 shows boxplots of prevalence and wealth disparity, calculated as the absolute percentage point difference between the top and bottom wealth quintiles, of all the districts in India. Anemia was the most highly prevalent malnutrition outcome in India (54.6%), followed by stunting (34.7%), underweight (31.4%), wasting (20.0%), and low birth weight (16.9%) (Fig. 1A). When considering the average district-wide wealth disparity, the largest inequalities was found for stunting, with an absolute difference of 26.8% between the top and bottom wealth quintiles and for underweight, with a difference of 26.2% (Fig. 1B). The next highest wealth disparities were anemia and wasting, with differences of 12% and 8.1% respectively. The smallest disparity in predicted prevalence was for low birthweight with a 6.6% difference. Further summary statistics at the national level for each malnutrition outcome are provided in Table S1.
Fig. 1.
Boxplots summarizing the distributions of (A) prevalence and (B) wealth disparity (the absolute percentage point difference between the highest and lowest wealth quintiles) in district-wide child stunting, underweight, wasting, low birth weight, and anemia across 640 districts in India.
3.2. Variation in district-wide wealth disparities in child malnutrition across states
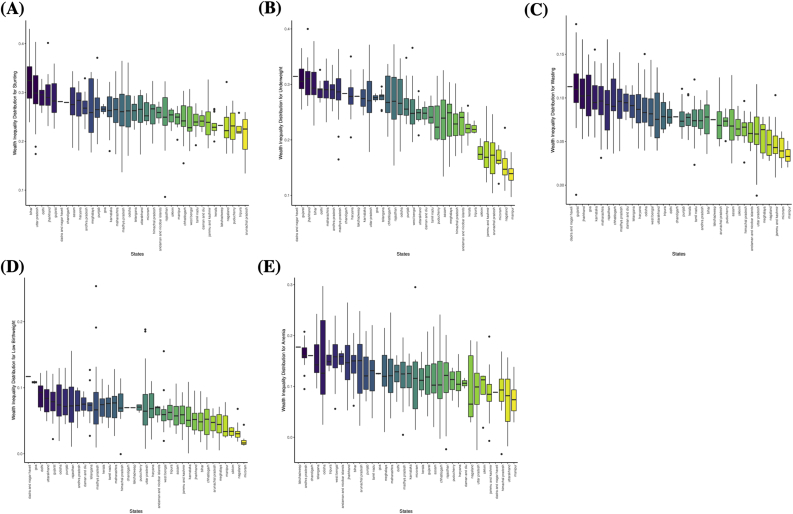
The district-wide prevalence of child malnutrition, overall and for the lowest and highest wealth quintiles, are presented in Table S2. Fig. 2 shows boxplots of district-level wealth disparity across states. As shown in Fig. 2A, the variation in wealth disparity in stunting existed across all states but to a different extent, with Bihar, Uttar Pradesh, and Delhi having the highest disparity while Puducherry, Tripura, and Arunachal Pradesh had the lowest. For stunting, the top three districts with the highest wealth disparity were Aurangabad in Bihar; Balrampur in Uttar Pradesh; and Pashchimi Singhbhum in Jharkhand with a 43%, 40% and 40% difference respectively. Across states, Gujarat, Jharkhand, and Bihar had the worst disparities in underweight while Mizoram, Nagaland, and Manipur had the least (Fig. 2B). For underweight, the top three districts with the highest wealth disparity were Bokaro in Jharkhand; Aurangabad in Bihar; and Udaipur in Rajasthan with a 40%, 38%, and 37% difference respectively. For wasting, Gujarat, Jharkhand, and Goa had the worst disparities while Jammu and Kashmir, Mizoram, and Manipur had the least (Fig. 2C). Panchmahal in Gujarat; Tapi in Gujarat; and Pratapgarh in Rajasthan had the largest wealth disparity in wasting, with a 18%, 17%, and 17% difference respectively. Delhi, Uttarakhand, and Gujarat had the worst disparities in low birthweight while Sikkim, Nagaland, and Mizoram had the least (Fig. 2D). For low birthweight, Mandsaur and Jhabua districts were outliers with wealth disparity of 25% and 19% differences which were far above the median in Madhya Pradesh. The distribution of wealth inequality across states for anemia is shown in Fig. 2E with Andra Pradesh, Telangana, and Odisha having the highest disparities while Himachal Pradesh, Uttarakhand, and Manipur had the lowest. The top three districts with the highest wealth inequality in anemia were Sundargarh in Odisha; Lunglei in Mizoram; and Nabarangapur in Odisha with a 30%, 30%, and 29% difference respectively. Overall, Bihar, Delhi, Gujarat, and Jharkhand ranked among the states with the highest wealth disparity in anthropometric failures. For anemia, the three worst-performing states in terms of wealth inequality were completely different than for the other anthropometrically oriented malnutrition outcomes.
Fig. 2.
Boxplots summarizing the distributions of within-state district-wide wealth disparity (the absolute percentage point difference between the highest and lowest wealth quintiles) in (A) stunting, (B) underweight, (C) wasting, (D) low birthweight, and (E) anemia.
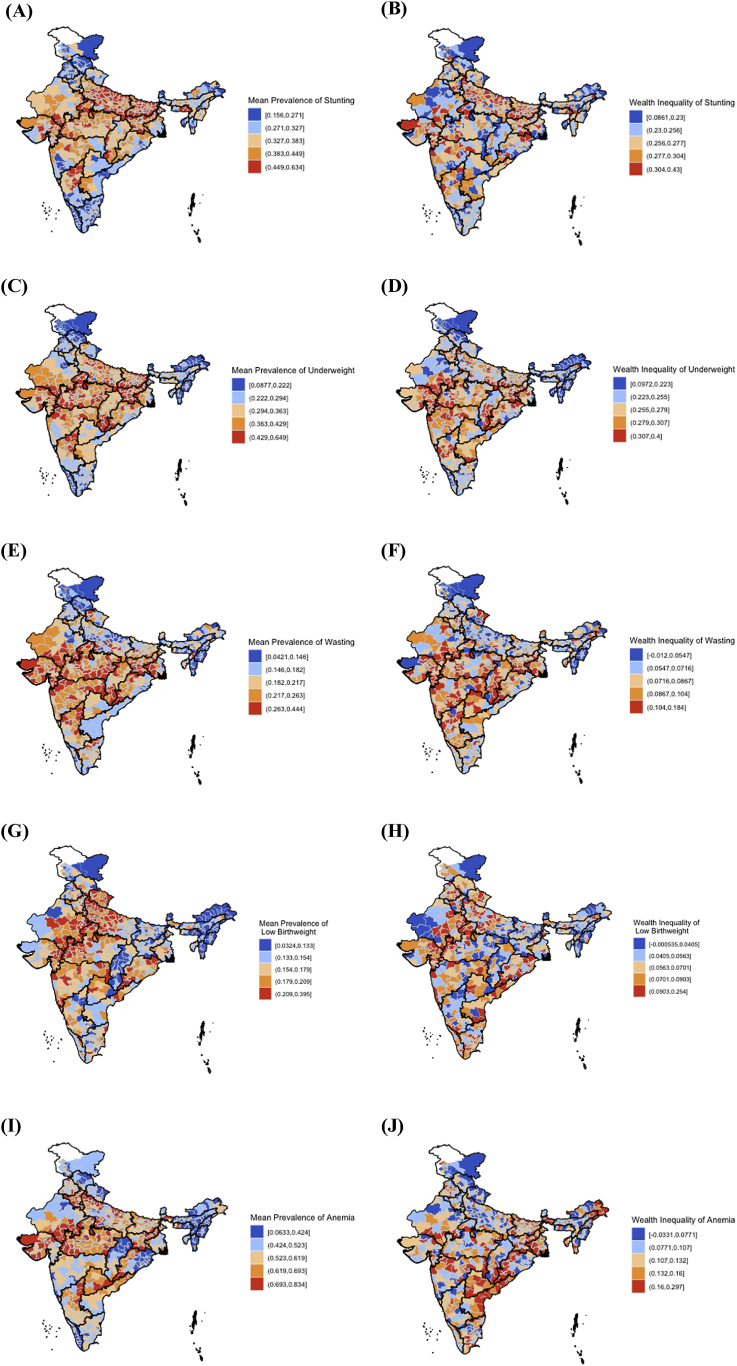
3.3. Geospatial patterning of district-wide wealth disparities in child malnutrition
Fig. 3 displays choropleth maps of district prevalence and wealth disparity of all five malnutrition indicators. The geospatial patterning of wealth disparity in malnutrition outcomes differed from those for the overall prevalence in malnutrition (Fig. 3). The worst inequality for stunting was primarily concentrated in the districts of north-central India. On the other hand, high inequality for underweight and wasting was more concentrated in central India. Inequality for low birthweight seems to be diffused across all India in small pockets of neighboring districts while for anemia, there was a region of high inequality districts concentrated in the southeast. In order to statistically test the likelihood of the geospatial distribution of wealth disparity we observed for each of the malnutrition outcomes, we calculated global Moran's I indices. They were highly statistically significant for all five malnutrition outcomes (p < 0.001), suggesting that the districts that were binned in the worst wealth disparity category were genuinely the worst-performing relative to their neighbors (Table S3). Further, significant Moran's I indices suggest that any clusters of districts that were similarly binned (e.g. districts all coded red) were genuinely correlated. To this end, we present LISA cluster maps (Fig. S2) that show significant clusters of high- and low-burden districts. Even with a fairly conservative Bonferroni Type I error control, the clustering patterns observed in Fig. 3 are supported by the LISA maps, in particular, the high wealth disparity burden of stunting in north-central India and anemia in southeast India (coded red).
Fig. 3.
Choropleth maps of district-wide overall burden and wealth disparity in child malnutrition indicators: (A) prevalence in stunting (B) wealth disparity in stunting (C) prevalence in underweight (D) wealth disparity in underweight (E) prevalence in wasting (F) wealth disparity in wasting (G) prevalence in low birthweight (H) wealth disparity in low birthweight (I) prevalence in anemia (J) wealth disparity in anemia.
3.4. Categorizing districts by overall burden and wealth disparity in child malnutrition
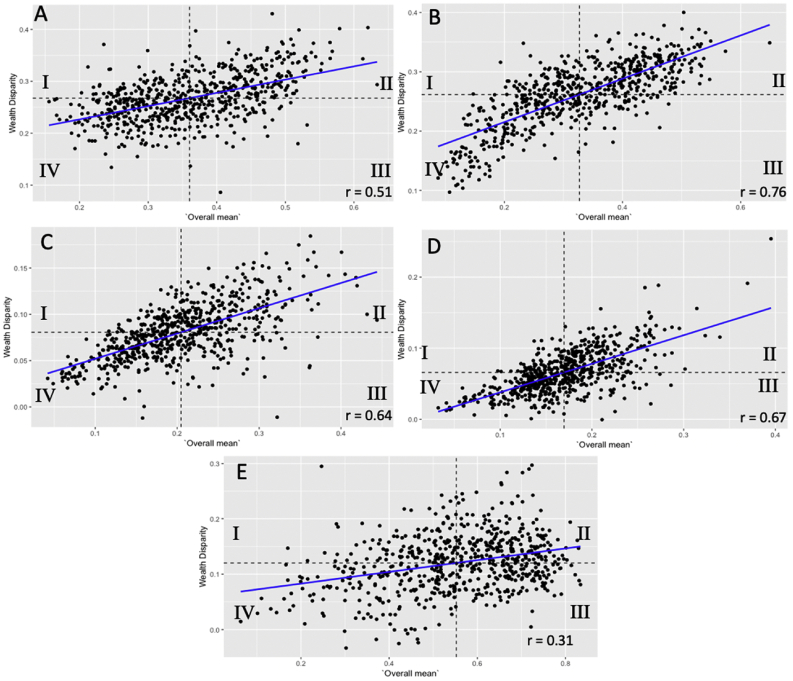
Fig. 4 shows scatterplots of all the districts divided into quadrants based on average prevalence and wealth disparity. All the malnutrition outcomes, except for anemia, had a moderate to strong correlation (0.5–0.8) between prevalence and the average wealth disparity across districts (Fig. 4). That is, a higher prevalence in four malnutrition indicators was associated with higher wealth-based disparities in prevalence. From the quadrant delineations, we can see general patterns of how some quadrants have bigger memberships than others; for instance, in underweight, there were more districts falling within quadrants II and IV. More clearly, however, we can use these demarcations and present geospatial maps of the quadrants (I: “Disparity”, II: “Pitfall”, III: “Intensity”, IV: “Prosperity”) by which each district is categorized for each of the five malnutrition indicators (Fig. 5). For stunting, the “Disparity”, “Pitfall”, and “Intensity” districts were localized to the north and center of India, with certain states such as Uttar Pradesh, Bihar, and Jharkhand being composed primarily of “Pitfall” and “Intensity” districts (Fig. 5A). States containing both “Prosperity” and “Disparity” districts reveal heterogeneity in the burden of malnutrition by overall prevalence and wealth disparity within states, such as Chandigarh, Himachal Pradesh, Uttarakhand, and Telangana for stunting. For underweight, the geospatial distribution of “Pitfall” and “Intensity” districts was very similar to that for stunting in northern India (Fig. 5B). However, unlike for stunting, where there were clusters of “Prosperity” districts in central India, particularly in Chhattisgarh, Telangana, Andhra Pradesh, Madhya Pradesh, and Maharashtra there was a bevy of “Disparity” states for underweight. Similarly, “Disparity” districts for wasting were also localized in Maharashtra and Telangana (Fig. 5C). However, the distribution differed in northern India where notably, Uttar Pradesh, Bihar, and the northern part of Madhya Pradesh was by majority comprised of “Prosperity” districts for wasting. For low birthweight, “Prosperity” districts were clustered in the east as well as along the western border of Rajasthan (Fig. 5D). The cluster of “Pitfall” and “Intensity” districts for low birthweight was centralized around the intersection of Uttar Pradesh, Rajasthan, and Madhya Pradesh borders. For anemia, the northernmost states of Jammu and Kashmir, Himachal Pradesh, and Uttarakhand; the northern part of Rajasthan, as well as a belt of central Indian states contained primarily of “Prosperity” districts (Fig. 5E). The “Disparity” districts for anemia were clustered in the northern part of Maharashtra as well as in most of West Bengal, Tamil Nadu and Andhra Pradesh. Most of northern India still performed poorly with regards to the anemia indicator as Madhya Pradesh, parts of Maharashtra, Uttar Pradesh, Bihar and Jharkhand were composed of “Pitfall” and “Intensity” districts.
Fig. 4.
Scatterplots of overall prevalence against wealth disparity for (A) stunting (B) underweight (C) wasting (D) low birthweight and (E) anemia, including the correlation coefficient. Horizontal and vertical lines are drawn at the averages of overall prevalence and wealth discrepancy to establish four quadrants. (I) Disparity quadrant refers to districts that fall below the mean prevalence but have high wealth disparity. (II) Pitfall quadrant refers to districts that have high prevalence and high wealth disparity. (III) Intensity quadrant refers to districts that have high prevalence but low wealth disparity. (IV) Prosperity quadrant refers to districts that have low prevalence and low wealth disparity.
Fig. 5.
Maps of 640 districts color coded by quadrant membership for (a) stunting (b) underweight (c) wasting (d) low birthweight and (e) anemia.
(I) Disparity quadrant refers to districts that fall below the mean prevalence but have high wealth disparity. (II) Pitfall quadrant refers to districts that have high prevalence and high wealth disparity. (III) Intensity quadrant refers to districts that have high prevalence but low wealth disparity. (IV) Prosperity quadrant refers to districts that have low prevalence and low wealth disparity. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
3.5. The poorest of the poor districts
Lastly, we provide geospatial maps focusing on the worst two wealth quintiles to see how the poorest populations in districts fare compared to each other (Fig. S1). Stunting and low birthweight had similar geospatial distributions in that poorer populations fare worse in northern India compared to eastern and southern parts of India. On the other hand, underweight was a dramatically widespread issue amongst the poorest sectors, spanning most of India except for the northern and eastern states. Wasting was felt most acutely in central and western India. Anemia was highly prevalent across the poorest of the poor in Rajasthan, Gujarat, Madhya Pradesh and Telangana.
4. Discussion
Although India has made measurable strides in reducing child malnutrition prevalence in the past decade, not all districts may have benefitted to the same extent. In this paper, we identified the largest district-wide wealth disparity for stunting and underweight, followed by anemia and wasting, and the least disparity for low birthweight. Wealth disparity also varied differently across states, with districts of worst disparity significantly concentrated in north-central India for stunting, central India for underweight and wasting, and the southeast for anemia. The correlation between district-wide prevalence and wealth disparity was moderate to strong for all child malnutrition indicators except for anemia. We characterized each district as one of four labels: “Disparity”, “Pitfall”, “Intensity”, or “Prosperity” based on its prevalence and wealth inequality, and mapped the geospatial distribution for each, thereby emphasizing the importance of considering both measures for targeting unique granular district-based health needs. Lastly, we found that among the poorest populations, anthropometric failures were highly prevalent across most of India, while low birthweight and anemia had distinct profiles that were more concentrated in central districts.
Our finding on the geographically widespread nature of wealth disparity in underweight and wasting aligns with previous studies that have noted significant wealth disparities affecting children of the lowest wealth quintiles (Gupta, Thakur, & Kumar, 2008; Kumar, Kumari, & Singh, 2015; Pathak & Mohanty, 2010). These studies have postulated that lack of access to quality maternal health services, detrimental environmental conditions which lead to higher susceptibility to infectious diseases, and low affordability to purchase the quality foods explain the high prevalence of underweight and stunting across urban India. The higher concentration of wasting in central India may be partially explained by acute illnesses and abrupt environmental changes specific to central India that lead to short-term nutritional disorder (Deaton & Drèze, 2002; Panter-Brick, 1997).
While the correlation between prevalence and wealth disparity was moderate to strong for stunting, underweight, wasting and low birthweight, it was low for anemia. Despite numerous programs and interventions to improve child anemia, the overall prevalence remains high due to inadequate allocation and distribution of resources, absence of nutrition education, and absence of adequate supervision (Anand et al., 2014). The high overall prevalence and relatively lower wealth disparity suggests the need for more universal interventions since the majority of the population seems to be faring poorly. Anand et al. suggest that a lifecycle approach needs to be implemented more aggressively across India, with nutritional and health related interventions targeting adolescent girls may continue throughout motherhood and first birth (Anand et al., 2014).
At the same time, even for malnutrition indicators that had moderate to high correlation between prevalence and wealth disparity, our geospatial maps of the districts by four quadrants (“Disparity”, “Pitfall”, “Intensity”, and “Prosperity”) suggested that across-district correlation may mask substantial intra-district variability. For instance, for wasting, Gujarat was binned as a high-performing district in terms of low average prevalence, but in respect to wealth disparity, it was among the worst. Thus, categorizing districts using such four-label approach recognizes the discordance between prevalence and wealth disparity profiles and has the potential to aid intervention development for equitable improvements. Districts with low prevalence but high inequality (eg. “Disparity” districts) likely require targeted measures and programs that differ from districts with high overall prevalence but low inequality (eg.“Intensity” districts), and hence both measures should be concurrently monitored.
Compared to prior studies that have focused on average prevalence of selected malnutrition indicators (Corsi et al., 2016; Menon et al., 2018; Subramanian et al., 2009) and based on older NFHS data (Prakash & Kumar, 2013; Subramanyam et al., 2011), we applied a precision-weighted algorithm to estimate district-wide prevalence and wealth disparity of a comprehensive set of policy relevant child malnutrition indicators using the latest NFHS-4 data. Our study is geographically granular in that it focuses on inter-district variation and allows for pronounced geospatial patterns of undernutrition through a wealth disparity-based perspective. Furthermore, by using both the average prevalence and wealth disparity, we identify specific health profiles of each district which would be overlooked in state- or national-level analyses. Our analysis, therefore, provides timely evidence for policymakers to tackle various undernutrition challenges in India, in a targeted and specific manner.
We also acknowledge a few data-related limitations. While focusing on the district level allows for analysis of granular differences in prevalence and wealth disparity in child malnutrition, a substantial variation within any given district can be expected. Our methodological approaches can be applied to examine geospatial variation in diverse population health and development indicators at geographic units lower than districts in future studies. Second, it should be noted that while anthropometry and hemoglobin measures were objectively taken in the NFHS-4, almost half of the data on low birthweight were self-reported by mothers and hence is prone to recall bias. Lastly, our precision weighted prevalence estimates and district-wide wealth disparity in child malnutrition indicators are crude in the sense that we did not adjust for other important demographic and socioeconomic characteristics that may drive higher burden in specific districts. However, our estimates form important evidence base to inform policy and interventions to target areas with the highest overall burden and the worst wealth disparity in child nutritional status.
5. Conclusion
We assessed the substantial burden of child malnutrition across all districts in India by examining geospatial variation in the overall prevalence in conjunction with wealth disparity. The relatively larger wealth disparity in underweight, wasting, and stunting suggests that efforts to reduce child anthropometric failures can benefit from targeting the poorer segments of the population. Further investigation of intra-district variation is warranted to design district-specific interventions that can improve equity in child nutritional outcomes. For instance, “Intensity” districts where prevalence is high may focus on reducing overall nutritional deficiencies through a concentrated wave of feeding programs. Although the government of India has initiated several nutritional policies and programs to address nutritional deficiencies, they stem from various departments and are thus asynchronous and uncoordinated. Coordinated cross-sectoral support from higher-level government and development partners is needed to ensure high coverage and continuous monitoring for a successful intervention especially in “Intensity” districts. On the other hand, addressing child undernutrition in the “Disparity” districts likely requires a different approach. Given that the poorer households are disproportionately shouldering the undernutrition burden in these districts, one proposal posited by several other studies is to provide social cash interventions to incentivize greater use of health services and improved nutritional outcomes among children.
6. Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author statement
Lathan Liou: Formal analysis, Writing – Original Draft, Writing - Review & Editing, Visualization.
Rockli Kim: Conceptualization, Methodology, Formal analysis, Investigation, Writing – Review & Editing, Supervision.
S.V. Subramanian: Conceptualization, Methodology, Writing – Review & Editing, Supervision.
Ethics statement
The study was reviewed by Harvard T.H. Chan School of Public Health Institutional Review Board and was considered exempt from full review because the study was based on an anonymous public use data set with no identifiable information on the study participants.
Financial disclosure statement
The authors have no financial relationships relevant to this article to disclose.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article to disclose.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2019.100524.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Aggarwal P., Kakkar R. National nutrition strategy: The needed timely modification to make integrated child development scheme more effective. Indian Journal of Pediatrics. 2019:1–5. doi: 10.1007/s12098-019-02869-9. [DOI] [PubMed] [Google Scholar]
- Anand T., Rahi M., Sharma P., Ingle G.K. Issues in prevention of iron deficiency anemia in India. Nutrition Burbank Los Angeles County California. 2014;30:764–770. doi: 10.1016/j.nut.2013.11.022. [DOI] [PubMed] [Google Scholar]
- Anselin L. Local indicators of spatial association—LISA. Geographical Analysis. 1995;27:93–115. [Google Scholar]
- Barros A.J., Victora C.G., França G.V., da Silva I.C.M., Amouzou A., Krasevec J. Socioeconomic inequalities persist despite declining stunting prevalence in low- and middle-income countries. Journal of Nutrition. 2018;148:254–258. doi: 10.1093/jn/nxx050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell A., Fairbrother M., Jones K. Fixed and random effects models: Making an informed choice. Quality and Quantity. 2019;53:1051–1074. [Google Scholar]
- Black R.E., Allen L.H., Bhutta Z.A., Caulfield L.E., de Onis M., Ezzati M. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet London, England. 2008;371:243–260. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- Browne W.J. Centre for Multilevel Modelling, University of Bristol; 2019. MCMC Estimation in MLwiN v3.03. [Google Scholar]
- Chalasani S., Rutstein S. Household wealth and child health in India. Population Studies. 2014;68:15–41. doi: 10.1080/00324728.2013.795601. [DOI] [PubMed] [Google Scholar]
- Charlton C., Rasbash J., Browne W.J., Healy M., Cameron B. Centre for Multilevel Modelling, University of Bristol; 2019. MLwiN version 3.04. [Google Scholar]
- Corsi D.J., Mejía-Guevara I., Subramanian S.V. Risk factors for chronic undernutrition among children in India: Estimating relative importance, population attributable risk and fractions. Social Science & Medicine. 2016;157:165–185. doi: 10.1016/j.socscimed.2015.11.014. [DOI] [PubMed] [Google Scholar]
- Deaton A., Drèze J. Poverty and inequality in India: A Re-examination. 2002. [DOI]
- Gupta M., Thakur J.S., Kumar R. Reproductive and child health inequities in Chandigarh union territory of India. Journal of Urban Health Bulletin of the New York Academy of Medicine. 2008;85:291–299. doi: 10.1007/s11524-007-9250-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IIPS . International Institute for Population Sciences (IIPS); Mumbai: 2017. National family health survey (NFHS-4), 2015-16: India. [Google Scholar]
- Jones K., Bullen N. Contextual models of urban house prices: A comparison of fixed- and random-coefficient models developed by expansion. Economic Geography. 1994;70:252–272. [Google Scholar]
- Kalaivani K., Ramachandran P. Time trends in prevalence of anaemia in pregnancy. Indian Journal of Medical Research. 2018;147:268–277. doi: 10.4103/ijmr.IJMR_1730_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanjilal B., Mazumdar P.G., Mukherjee M., Rahman M.H. Nutritional status of children in India: Household socio-economic condition as the contextual determinant. International Journal for Equity in Health. 2010;9 doi: 10.1186/1475-9276-9-19. 19–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim R., Mejía-Guevara I., Corsi D.J., Aguayo V.M., Subramanian S.V. Relative importance of 13 correlates of child stunting in South Asia: Insights from nationally representative data from Afghanistan, Bangladesh, India, Nepal, and Pakistan. Social Science & Medicine. 2017;187:144–154. doi: 10.1016/j.socscimed.2017.06.017. [DOI] [PubMed] [Google Scholar]
- Kumar A., Kumari D., Singh A. Increasing socioeconomic inequality in childhood undernutrition in urban India: Trends between 1992-93, 1998-99 and 2005-06. Health Policy and Planning. 2015;30:1003–1016. doi: 10.1093/heapol/czu104. [DOI] [PubMed] [Google Scholar]
- Mazumdar S. Determinants of inequality in child malnutrition in India. Asian Population Studies. 2010;6:307–333. [Google Scholar]
- McCormick M.C. The contribution of low birth weight to infant mortality and childhood morbidity. New England Journal of Medicine. 1985;312:82–90. doi: 10.1056/NEJM198501103120204. [DOI] [PubMed] [Google Scholar]
- Menon P., Headey D., Avula R., Nguyen P.H. Understanding the geographical burden of stunting in India: A regression-decomposition analysis of district-level data from 2015–16. Maternal and Child Nutrition. 2018;14 doi: 10.1111/mcn.12620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panter-Brick C. Seasonal growth patterns in rural Nepali children. Annals of Human Biology. 1997;24:1–18. doi: 10.1080/03014469700004732. [DOI] [PubMed] [Google Scholar]
- Pathak P.K., Mohanty S.K. Does the safe-motherhood programme reach the poor IN Uttar Pradesh, India? Asian Population Studies. 2010;6:173–191. [Google Scholar]
- Prakash R., Kumar A. Urban poverty and utilization of maternal and child health care services in India. Journal of Biosocial Science. 2013;45:433–449. doi: 10.1017/S0021932012000831. [DOI] [PubMed] [Google Scholar]
- Renzaho A.M.N., Chen W., Rijal S., Dahal P., Chikazaza I.R., Dhakal T. The impact of unconditional child cash grant on child malnutrition and its immediate and underlying causes in five districts of the Karnali Zone, Nepal - a trend analysis. Archives of Public Health Archives Belges de Sante Publique. 2019;77 doi: 10.1186/s13690-019-0352-2. 24–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin D.B. Using empirical Bayes techniques in the law school validity studies. Journal of the American Statistical Association. 1980;75:801–816. [Google Scholar]
- Rutstein S.O., Johnson K. ORC Macro; Calverton, Maryland, USA: 2004. The DHS wealth index, DHS Comparative Reports No. 6. [Google Scholar]
- Sen A., Himanshu H. Poverty and inequality in India: II: Widening disparities during the 1990s. 2004. [DOI]
- Subramanian S.V., Ackerson L.K., Davey Smith G., John N.A. Association of maternal height with child mortality, anthropometric failure, and anemia in India. Journal of the American Medical Association. 2009;301:1691–1701. doi: 10.1001/jama.2009.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian S.V., Delgado I., Jadue L., Vega J., Kawachi I. Income inequality and health: Multilevel analysis of Chilean communities. Journal of Epidemiology & Community Health. 2003;57:844–848. doi: 10.1136/jech.57.11.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanyam M.A., Kawachi I., Berkman L.F., Subramanian S.V. Is economic growth associated with reduction in child undernutrition in India? PLoS Medicine. 2011;8 doi: 10.1371/journal.pmed.1000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Poel E., Hosseinpoor A.R., Jehu-Appiah C., Vega J., Speybroeck N. Malnutrition and the disproportional burden on the poor: The case of Ghana. International Journal for Equity in Health. 2007;6 doi: 10.1186/1475-9276-6-21. 21–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora C.G., Adair L., Fall C., Hallal P.C., Martorell R., Richter L. Maternal and child undernutrition: Consequences for adult health and human capital. The Lancet. 2008;371:340–357. doi: 10.1016/S0140-6736(07)61692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2006. WHO child growth standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.