Abstract
Purpose: This study examined whether older age moderates the association between gender-affirming medical treatment and quality of life (QOL) among transgender individuals.
Methods: Transgender men and women from the National Transgender Discrimination Survey who had either recently or never undergone medical treatment were included (n = 2420). A moderation analysis was utilized.
Results: As predicted, participants who initiated medical treatment had higher QOL than those who did not. Age moderated this association. The QOL difference was greater for older than for younger transgender individuals.
Conclusion: Among all transgender men and women, gender-affirming medical treatment can be especially beneficial for elders.
Keywords: aging, gender-affirming medical treatment, quality of life, transgender
Introduction
Most research suggests that gender-affirming medical treatments (i.e., hormonal and/or surgical), which align transgender individuals' outward physical appearance with their internal gender identity, tend to lead to higher quality of life (QOL).1,2 However, transgender elders may experience ageism when seeking treatment, as medical insurance plans place arbitrary limits on coverage for transgender elders.3 Some health care providers discourage transgender elders from undergoing these treatments.3 To address these biases, it could be helpful to know whether gender-affirming medical treatments differentially impact transgender elders' QOL.
The current quantitative study builds on earlier qualitative studies with transgender elders who have accessed gender-affirming medical treatments at later life, which found that undergoing medical treatments alleviated transgender elders' stress from having a gender expression that was incongruent with their birth sex.4,5 These studies, however, did not include a comparison sample of younger individuals, or transgender elders who did not undergo gender-affirming medical treatments. Research has found that QOL tends to improve among older cisgender people6 and transgender people.7–9 Thus, research is needed to compare the QOL of both younger and older transgender individuals who have undergone gender-affirming medical treatment with those within the same age group who have not undergone such treatment to examine the independent association of these treatments and QOL.
Transgender elders may experience greater QOL from initiating gender-affirming medical treatment than younger transgender individuals for several reasons. First, transgender elders may have developed coping capacities10 from navigating gender-related minority stress11,12 and age-related stigma.13 The exposure to dual forms of stigma and coping skills developed as a result could enhance their ability to navigate the gender-affirmation process successfully. Second, transgender elders are likely to have experienced more years of stigma than younger individuals, which may enhance the cathartic impact of gender-affirming medical treatment and result in greater improvement in QOL, relative to younger adults.4,8,14 Third, older individuals, who may internalize negative age stereotypes which characterize old age as a time of loss of control15 may particularly appreciate an opportunity to exercise control over their bodies, compared with younger individuals.
Based on these premises, we examined whether gender-affirming medical treatment differentially impacts the QOL of older and younger transgender individuals. We hypothesize that:
-
(1)
Both younger and older transgender individuals who have undergone recent gender-affirming medical treatment will have better QOL compared with their transgender counterparts who have not undergone the treatment.
-
(2)
Age will moderate this association, such that the QOL difference between individuals who underwent a recent gender-affirming medical treatment and those with no treatment will be greater for older than for younger transgender individuals.
Methods
This study analyzed data from the National Transgender Discrimination Survey, designed and fielded by the National Center for Transgender Equality and the National Gay and Lesbian Task Force. Detailed study methodologies can be found elsewhere.16 The original survey was approved by the Institutional Review Board (IRB) of Pennsylvania State University. Completion of the survey indicated consent.16 The current study was deemed to be exempt from IRB review by the Human Subjects Committee of Yale University, because the dataset is public and de-identified.
Participants
We included participants who (1) identified as transgender women or transgender men16 and (2) received their first gender-affirming medical treatment within the past 2 years or had not received any gender-affirming medical treatment. As gender nonbinary individuals may have different needs for treatment and risks for poor mental health outcomes compared with binary transgender individuals,17 consistent with previous research assessing QOL following gender-affirming medical treatment,1,2 we focused on transgender individuals with a binary gender identity. A total of 597 participants with missing data on the key variables of age and QOL were excluded.
Measures
Independent variable
Recent gender-affirming medical treatment. We focused on initial gender-affirming medical procedures that occurred within the past 2 years to increase our confidence that any age differences in the relationship between treatment and QOL were due to age rather than the time that had passed since treatment. Participants estimated the age in years that they “first got any kind of transgender-related medical treatment.”16 Age at first treatment was subtracted from participants' current age. If the difference was 2 years or less, participants were given a score of 1. Those who responded “not applicable” to the question asking for their age of first gender-affirming treatment were coded as 0. A total of 32% of the sample had recently undergone their first gender-affirming medical treatment.
Moderator
Age
Participants ranged in age from 18 to 98 (M = 33.8, standard deviation = 12.93 years). Consistent with operationalization for older age in previous studies,15 age was dichotomized as younger (ages 18–59 years) versus older (60 years old or older) for the interaction analysis.
Outcome
Quality of life
QOL was assessed with the question, “Because I am transgender/gender non-conforming, life in general is”: “much improved,” “somewhat improved,” “the same,” “somewhat worse,” “much worse,” and “in some ways better, in some ways worse.”16 The option of “much improved” was given the highest QOL score of 4. The option “Somewhat improved” was given a score of 3. The option of “in some ways better, in some ways worse” was combined with “the same” option to indicate a midlevel indicator of QOL, with a score of 2. The option “somewhat worse” was given a score of 1. The option of “much worse” was given the lowest score of 0. QOL was selected as the outcome variable, as it has been used as an indicator of psychological well-being among transgender individuals following gender-affirming medical treatment.1,2 The focus of our outcome measure on transgender-specific aspects of QOL is a strength in that it likely serves as a proxy for transgender identity development, which has been found to relate significantly to improved well-being in transgender individuals.9
Covariates
The following covariates were included based on their documented relationship to QOL in diverse samples7,18–20: gender identity (i.e., transgender men and transgender women); income (i.e., <$10K, $10K–$19,999, $20K–$49,999; $50K–$99,999, and $100K+); race/ethnicity (i.e., White, Hispanic/Latino/a, Black/African American, and other [American Indian or Alaska Native; Asian or Pacific Islander, Arab or Middle Eastern, or Multiracial or Mixed Race]); education (i.e., no high school degree, high school degree, some college, college degree, and graduate degree); relationship status (i.e., partnered [partnered, civil union, or married] and not partnered [single, divorced, separated, or widowed]); employment status (i.e., employed and unemployed); and health insurance status (i.e., insured and uninsured).
Analysis plan
Statistical analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC). Univariate and bivariate statistics (chi-square) examined participant characteristics overall and by receipt of gender-affirming medical treatment. Pearson's correlation, variance inflation factor, and tolerance between regression variables were utilized to examine multicollinearity. No multicollinearity was found.
To examine our first hypothesis, we conducted ordinal logistic regressions analyses within each age group (ages 18–59 and 60 years old or older), with QOL as the outcome, controlling for all covariates. To confirm the documented associations of age and gender-affirming medical treatment with QOL, QOL scores were first separately regressed on age and gender-affirming medical treatment status, while controlling for all covariates. To examine our second hypothesis, we treated the dichotomized age group as the moderator, gender-affirming medical treatment as the predictor, and QOL as the outcome, adjusting for all covariates in an ordinal logistic regression model.21 We then used a figure to graphically depict the relationship among gender-affirming medical treatment, age, and QOL. For all models, the level of significance was set at p < 0.05.
Results
Our sample consisted of 2420 individuals, with 1442 (59.59%) transgender men and 978 (40.41%) transgender women. The majority (82.69%) identified their race/ethnicity as White, 6.36% identified as Black or African American, 6.82% identified as Hispanic or Latino/a, and 7.02% identified as other. Table 1 shows the associations between all study variables and gender-affirming medical treatment. Income levels (p = 0.004), education (p < 0.0001), and QOL (p < 0.0001) were significantly different across treatment status.
Table 1.
Factors Associated with Undergoing Recent Initial Gender-Affirming Medical Treatment
| No treatment at all, n (%) | Underwent recent initial gender-affirming medical treatment, n (%) | pa | |
|---|---|---|---|
| Age | 0.60 | ||
| 18–59 Years old | 1579 (67.83) | 749 (32.17) | |
| 60 Years old or older | 60 (65.22) | 32 (34.78) | |
| Gender identity | 0.94 | ||
| Transgender man | 780 (54.09) | 662 (45.91) | |
| Transgender woman | 532 (54.40) | 446 (45.60) | |
| Income | 0.004 | ||
| <$10K | 255 (64.56) | 140 (35.44) | |
| $10K–$19,999 | 179 (62.59) | 107 (37.41) | |
| $20K–$49,999 | 438 (64.41) | 242 (35.59) | |
| $50K–$99,999 | 433 (69.39) | 191 (30.61) | |
| $100K+ | 252 (74.34) | 87 (25.66) | |
| Race/ethnicityb | 0.33 | ||
| White | 1391 (69.52) | 610 (30.48) | |
| Black | 106 (68.83) | 48 (31.17) | |
| Hispanic/Latino/a | 101 (61.21) | 64 (38.79) | |
| Otherc | 114 (67.06) | 56 (32.94) | |
| Education | <0.0001 | ||
| No high school degree | 111 (81.62) | 25 (18.38) | |
| High school degree | 186 (74.70) | 63 (25.30) | |
| Some college | 656 (67.01) | 323 (32.99) | |
| College degree | 395 (64.86) | 214 (35.14) | |
| Graduate degree | 272 (63.85) | 154 (36.15) | |
| Employment status | 0.71 | ||
| Employed | 1102 (68.02) | 518 (31.98) | |
| Unemployed | 186 (66.91) | 92 (33.09) | |
| Relationship status | 0.08 | ||
| Not partnered | 799 (65.98) | 412 (34.02) | |
| Partnered | 831 (69.37) | 367 (30.63) | |
| Health insurance status | 0.44 | ||
| Insured | 1258 (66.95) | 621 (33.05) | |
| Uninsured | 305 (68.85) | 138 (31.15) | |
| Quality of life | <0.0001 | ||
| Much worse | 85 (71.43) | 34 (28.57) | |
| Somewhat worse | 238 (77.78) | 68 (22.22) | |
| The same | 856 (74.96) | 286 (25.04) | |
| Somewhat improved | 255 (67.11) | 125 (32.89) | |
| Much improved | 190 (41.85) | 264 (58.15) |
Bold values indicate statistical significance at a level of <0.05. Data are missing for some covariates.
p-values obtained from chi-square tests.
Participants could choose more than one option for race/ethnicity.
Other includes American Indian or Alaska Native, Asian or Pacific Islander, Arab or Middle Eastern, or Multiracial or Mixed Race.
In support of the first hypothesis, we found that undergoing gender-affirming medical treatment was associated with higher QOL scores among both age groups, after adjusting for covariates: (adjusted odds ratio [aOR] = 2.39; 95% confidence interval [CI] = 1.93–2.95; p < 0.0001 among younger participants and aOR = 8.84; 95% CI = 1.43–51.92; p = 0.02 among older participants).
As shown in Table 2, increasing age (aOR = 1.03; 95% CI = 1.02–1.04; p < 0.0001) and undergoing recent gender-affirming medical treatment (aOR = 2.45; 95% CI = 1.99–3.02; p < 0.0001) were both significantly associated with increased odds of higher QOL scores among all participants (Table 2, models 1 and 2). Gender identity was significantly associated with higher QOL scores in all 3 models, suggesting that transgender women may have higher QOL than transgender men.
Table 2.
Covariate-Adjusted Multivariable Regression Models Demonstrating the Association Between the Quality-of-Life Outcome and Age (Model 1), Recent Gender-Affirming Medical Treatment (Model 2), and the Interaction Between Age and Recent Gender-Affirming Medical Treatment (Model 3)
| Outcome: quality-of-life scores | ||||||
|---|---|---|---|---|---|---|
| Predictors | Model 1 | p | Model 2 | p | Model 3 | p |
| aOR (95% CI) | aOR (95% CI) | B (SE) | ||||
| Interaction | ||||||
| Age group and recent treatment | — | — | — | — | 1.66 (0.69) | 0.03 |
| Age (continuous) | 1.03 (1.02–1.04) | <0.0001 | — | — | — | — |
| 18–59 Years old | — | — | — | — | 1 | |
| 60 Years old or older | — | — | — | — | 1.47 (0.42) | 0.13 |
| Recent treatment | ||||||
| No | — | — | 1 | 1 | ||
| Yes | — | — | 2.45 (1.99–3.02) | <0.0001 | 0.58 (0.10) | <0.0001 |
| Covariates | ||||||
| Gender identity | ||||||
| Transgender man | 1 | 1 | 1 | |||
| Transgender woman | 1.69 (1.35–2.11) | <0.0001 | 1.04 (1.10–1.69) | 0.01 | 0.31 (0.11) | 0.01 |
| Income | ||||||
| <$10K | 1 | 1 | ||||
| $10K–$19,999 | 1.03 (0.66–1.39) | 0.81 | 1.04 (0.74–1.46) | 0.83 | 0.07 (0.17) | 0.81 |
| $20K–$49,999 | 0.86 (0.63–1.17) | 0.33 | 0.86 (0.65–1.15) | 0.31 | −0.05 (0.15) | 0.29 |
| $50K–$99,999 | 0.77 (0.55–1.07) | 0.12 | 0.83 (0.61–1.12) | 0.22 | −0.09 (0.16) | 0.15 |
| $100K+ | 1.07 (0.81–1.12) | 0.47 | 1.06 (0.82–1.32) | 0.64 | 0.16 (0.19) | 0.58 |
| Race | ||||||
| White | 1 | 1 | 1 | |||
| Black | 1.01 (0.66–1.54) | 0.97 | 1.03 (0.68–1.46) | 0.98 | 0.02 (0.20) | 0.88 |
| Hispanic/Latino/a | 1.13 (0.79–1.63) | 0.50 | 1.13 (0.81–1.59) | 0.47 | 0.11 (0.17) | 0.44 |
| Other | 0.85 (0.61–1.19) | 0.35 | 0.98 (0.72–1.34) | 0.86 | −0.02 (0.16) | 0.65 |
| Education | ||||||
| No high school degree | 1 | 1 | 1 | |||
| High school degree | 0.72 (0.39–1.36) | 0.31 | 0.83 (0.47–1.46) | 0.52 | −0.22 (0.29) | 0.41 |
| Some college | 0.97 (0.55–1.71) | 0.92 | 0.96 (0.58–1.59) | 0.87 | −0.12 (0.26) | 0.66 |
| College degree | 1.18 (0.66–2.09) | 0.58 | 1.09 (0.65–1.82) | 0.75 | 0.07 (0.26) | 0.96 |
| Graduate degree | 0.91 (0.51–1.67) | 0.78 | 0.97 (0.57–1.64) | 0.90 | −0.02 (0.27) | 0.72 |
| Employment status | ||||||
| Employed | 1 | 1 | 1 | |||
| Unemployed | 0.49 (0.36–0.65) | <0.0001 | 0.48 (0.37–0.62) | <0.0001 | −0.74 (0.14) | <0.0001 |
| Relationship status | ||||||
| Not partnered | 1 | 1 | 1 | |||
| Partnered | 1.11 (0.91–1.34) | 0.31 | 1.16 (0.97–1.39) | 0.16 | 0.19 (0.09) | 0.11 |
| Health insurance status | ||||||
| Uninsured | 1 | 1 | 1 | |||
| Insured | 1.15 (0.90–1.47) | 0.25 | 1.19 (0.9–1.49) | 0.14 | 0.17 (0.12) | 0.18 |
Bold values indicate statistical significance at a level of <0.05.
aOR, adjusted odds ratio; CI, confidence interval; SE, standard error.
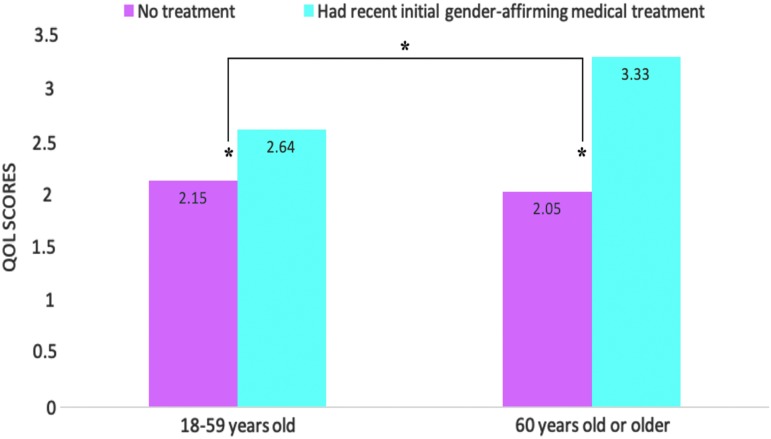
In support of the second hypothesis, the interaction between age and gender-affirming medical treatment status was positively associated with QOL, after adjusting for all covariates (β = 1.66, p = 0.03) (Table 2, model 3). As shown in Figure 1, older participants reported higher QOL scores after undergoing gender-affirming medical treatment relative to younger participants. The difference in QOL between those who had recent initial gender-affirming medical treatment and those who did not was on average 2.61 times higher among the older than the younger participants (μ = 3.33 vs. 2.05 among older participants and μ = 2.64 vs. 2.15 among younger participants, controlling for all covariates).
FIG. 1.
Difference in QOL for transgender individuals who had recent initial gender-affirming medical treatment and those who had no treatment at all. Means are adjusted for all covariates (gender identity, income, race/ethnicity, education, employment status, relationship status, and health insurance status). The bar which connects the two age groups shows the significant interaction of age group and medical treatment, after adjusting for covariates. *p < 0.05. Among transgender individuals who were 18–59 years old, those who had no treatment had an average QOL score of 2.15, and those who had recent initial gender-affirming medical treatment had an average QOL score of 2.64. Among transgender individuals who were 60 years old or older, those who had no treatment had an average QOL score of 2.05, and those who had recent initial gender-affirming medical treatment had an average QOL score of 3.33. QOL, quality of life.
Discussion
This is the first empirical study, to our knowledge, to demonstrate that transgender elders report higher QOL after undergoing gender-affirming medical treatment compared with their same-aged transgender peers who did not undergo the treatment and younger transgender individuals who underwent the treatment. We also found that transgender elders, regardless of whether they had recent gender-affirming medical treatment, tended to have significantly higher QOL than younger transgender individuals.
The higher QOL observed among transgender elders following the initiation of gender-affirming medical treatment may partially be due to their generally lower expectations for treatment opportunities. Alternatively, transgender elders, mindful of their limited time remaining in life, may seek to maximize positive aspects of the gender-affirming medical treatments, relative to their younger counterparts.22 Although transgender elders were found to have greater QOL following gender-affirming medical treatment than their younger counterparts, our findings support previous research suggesting that use of medical treatments was associated with greater QOL independent of age.1,2 This underscores the importance of ensuring access to gender-affirming medical treatment for transgender individuals who need it, regardless of age.23,24
The finding of higher QOL among older participants aligns with studies that have found that, in general, older adults tend to have higher QOL than younger adults8 and that transgender elders have more robust psychological resilience than younger transgender individuals.9 It is possible that the ability to manage transgender-related stigma (e.g., internalized trans-negativity)9 can strengthen transgender elders' capacity to embrace other potentially stigmatizing identities (e.g., older age).10,13 This pattern may also result from the synergistic nature of resisting negative stereotypes about both transgender identity and older age, which can be internalized over the lifespan.25 Transgender elders may have been more likely to question normative thinking, which may have allowed them to resist internalizing negative age stereotypes across their lifespan and to affirm positive age stereotypes giving them a QOL advantage relative to younger individuals.15,25
Limitations
The present study used a cross-sectional study design, thus, causal interpretations cannot be made. Future research should explore QOL among gender diverse people of all ages. It would also be helpful to examine the impact of treatment on different domains of QOL (e.g., mental and physical) with validated measures.
Future directions
Future longitudinal research should attempt to discern period and cohort effects when examining whether different types of gender-affirming medical treatment differentially impact other indicators for mental health (e.g., depression). Longitudinal studies could also examine the temporal ordering of variables and patterns of stress-related growth among transgender elders. Finally, future interventions should encourage younger individuals to learn from transgender elders to successfully navigate a society which stigmatizes individuals based on their age and gender identities.3,14,25
Conclusion
Our study indicates that transgender elders demonstrated higher QOL following recent gender-affirming medical treatment than did younger transgender individuals. Not all transgender individuals desire gender-affirming medical treatments. However, structural interventions should make these treatments more available to those who pursue them, regardless of age, to optimize the mental wellbeing of transgender individuals.
Acknowledgments
The authors thank the National Transgender Discrimination Survey investigators and participants. This research was supported by a National Institute on Minority Health and Health Disparities grant (1F31MD011203-0) to J.M.W.H. and a National Institute on Aging grant (U01AG032284) to B.R.L.
Disclaimer
This study utilized data from the National Transgender Discrimination Survey, designed and fielded by the National Center for Transgender Equality and the National Gay and Lesbian Task Force. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. White Hughto JM, Reisner SL: A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals. Transgend Health 2016;1:21–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lindqvist EK, Sigurjonsson H, Möllermark C, et al. : Quality of life improves early after gender reassignment surgery in transgender women. Eur J Plast Surg 2017;40:223–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Auldridge A, Tamar-Mattis A, Kennedy S, et al. : Improving the lives of transgender older adults: recommendations for policy and practice. Services and Advocacy for GLBT Elders and National Center for Transgender Equality; 2012. Available at https://transequality.org/sites/default/files/docs/resources/TransAgingPolicyReportFull.pdf Accessed October30, 2018 [Google Scholar]
- 4. Fabbre VD: Agency and social forces in the life course: The case of gender transitions in later life. J Gerontol B Psychol Sci Soc Sci 2017;72:479–487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fabbre VD: Gender transitions in later life: The significance of time in queer aging. J Gerontol Soc Work 2014;57:161–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bowling A, Iliffe S: Psychological approach to successful ageing predicts future quality of life in older adults. Health Qual Life Outcomes 2011;9:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fredriksen-Goldsen KI, Kim HJ, Shiu C, et al. : Successful aging among LGBT older adults: Physical and mental health-related quality of life by age group. Gerontologist 2015;55:154–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nuttbrock L, Hwahng S, Bockting W, et al. : Psychiatric impact of gender-related abuse across the life course of male-to-female transgender persons. J Sex Res 2010;47:12–23 [DOI] [PubMed] [Google Scholar]
- 9. Jackman KB, Dolezal C, Bockting WO: Generational differences in internalized transnegativity and psychological distress among feminine spectrum transgender people. LGBT Health 2018;5:54–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Friend RA: Older lesbian and gay people: A theory of successful aging. J Homosex 1990;20:99–118 [DOI] [PubMed] [Google Scholar]
- 11. Meyer IH: Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol Bull 2003;129:674–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hendricks ML, Testa RJ: A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the Minority Stress Model. Profess Psychol Res Pract 2012;43:460–467 [Google Scholar]
- 13. Fredriksen-Goldsen KI, Cook-Daniels L, Kim HJ, et al. : Physical and mental health of transgender older adults: An at-risk and underserved population. Gerontologist 2014;54:488–500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. White Hughto JM, Reisner SL, Pachankis JE: Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med 2015;147:222–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Levy BR, Pilver C, Chung PH, Slade MD: Subliminal strengthening: Improving older individuals' physical function over time with an implicit-age-stereotype intervention. Psychol Sci 2014;25:2127–2135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Grant JM, Mottet LA, Tanis J, et al. : Injustice at Every Turn: A Report of the National Transgender Discrimination Survey. 2011. Washington, DC, National Center for Transgender Equality and National Gay and Lesbian Task Force [Google Scholar]
- 17. Harrison J, Grant J, Herman JL: A gender not listed here: Genderqueers, gender rebels, and otherwise in the National Transgender Discrimination Survey. LGBTQ Public Policy J 2012;2:13–24 [Google Scholar]
- 18. Skarupski KA, de Leon CF, Bienias JL, et al. : Black-White differences in health-related quality of life among older adults. Qual Life Res 2007;16:287–296 [DOI] [PubMed] [Google Scholar]
- 19. Zaninotto P, Falaschetti E, Sacker A: Age trajectories of quality of life among older adults: Results from the English Longitudinal Study of Ageing. Qual Life Res 2009;18:1301–1309 [DOI] [PubMed] [Google Scholar]
- 20. Motmans J, Meier P, Ponnet K, T'Sjoen G: Female and male transgender quality of life: Socioeconomic and medical differences. J Sex Med 2012;9:743–750 [DOI] [PubMed] [Google Scholar]
- 21. Baron RM, Kenny DA: The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–1182 [DOI] [PubMed] [Google Scholar]
- 22. Luong G, Charles ST, Fingerman KL: Better with age: Social relationships across adulthood. J Soc Pers Relat 2011;28:9–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Leinung M, Urizar MF, Patel N, Sood SC: Endocrine treatment of transsexual persons: Extensive personal experience. Endocr Pract 2013;19:644–650 [DOI] [PubMed] [Google Scholar]
- 24. Coleman E, Bockting W, Botzer M, et al. : Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend 2012;13:165–232 [Google Scholar]
- 25. Levy B: Stereotype embodiment: A psychosocial approach to aging. Curr Dir Psychol Sci 2009;18:332–336 [DOI] [PMC free article] [PubMed] [Google Scholar]