Abstract
Objectives: Chiropractic care may have value in improving patient outcomes and decreasing opioid use, but little is known about the impetus for or process of incorporating these services into conventional medical settings. The purpose of this qualitative study was to describe organizational structures, care processes, and perceived value of chiropractic integration within U.S. private sector medical facilities.
Design: Multisite, comparative organizational case study.
Settings: Nine U.S. private sector medical facilities with on-site chiropractic care, including five hospitals and four clinics.
Participants: One hundred and thirty-five key facility stakeholders including doctors of chiropractic (DCs), non-DC clinicians, support staff, administrators, and patients.
Methods: Researchers conducted 2-day site visits to all settings. Qualitative data were collected from audio-recorded, semi-structured, role-specified, individual interviews; standardized organizational data tables; and archival document review. A three-member, interdisciplinary team conducted thematic content analysis of verbatim transcripts using an existing conceptual framework and emergent codes.
Results: These nine medical facilities had unique organizational structures and reasons for initiating chiropractic care in their settings. Across sites, DCs were sought to take an evidence-based approach to patient care, work collaboratively within a multidisciplinary team, engage in interprofessional case management, and adopt organizational mission and values. Chiropractic clinics were implemented within existing human resources, physical plant, information technology, and administrative support systems, and often expanded over time to address patient demand. DCs usually were co-located with medical providers and integrated into the collaborative management of patients with musculoskeletal and co-morbid conditions. Delivery of chiropractic services was perceived to have high value among patients, medical providers, and administration. Patient clinical outcomes, patient satisfaction, provider productivity, and cost offset were identified as markers of clinic success.
Conclusion: A diverse group of U.S. private sector medical facilities have implemented chiropractic clinics, and a wide variety of facility stakeholders report high satisfaction with the care provided.
Keywords: : integrative medicine, chiropractic, delivery of healthcare, interprofessional relations, organizational case studies, health services research
Introduction
Although not delivered on-site at most U.S. medical facilities, chiropractic care is a treatment approach with demonstrated safety and efficacy for managing pain and disability associated with musculoskeletal disorders.1–3 Components of multimodal chiropractic care (such as spinal manipulation, manual therapies, exercise, and patient education) are recommended as first-line treatments by current low back pain clinical practice guidelines.4 Of particular relevance to a current important national healthcare initiative, use of chiropractic services has been associated with decreased use of opioid medications in patients with spinal pain conditions.5–9
Over the past two decades, the large U.S. public healthcare delivery systems of the Department of Defense and Department of Veterans Affairs have increased delivery of chiropractic services.10–12 Previous work has demonstrated positive patient and provider perceptions, beneficial outcomes, and expanded use of services in these systems.13–17 Chiropractic services are also included in U.S. private medical settings ranging from large healthcare systems to smaller care delivery sites.18–20 However, there is no central coordination or assessment of these programs. Consequently, data are lacking on the optimal means of chiropractic service implementation in private medical facilities.
Improving the quality of chiropractic service delivery in private medical facilities supports the Triple Aim of optimizing the U.S. healthcare system in terms of patient experience, population health, and cost reduction.21 Previous studies on chiropractic care report high patient satisfaction22–24; improved health outcomes in patients with musculoskeletal pain1–3; and cost reduction in conservative management of spinal pain conditions.25,26 A better understanding of the existing models of chiropractic integration into private sector medical settings is a key precursor to overall quality improvement. Since healthcare systems are highly complex entities, and the inclusion of chiropractic services is subject to much variation, the objective of this study was to describe the delivery of chiropractic services in private sector healthcare facilities using a qualitative case study approach.
Materials and Methods
We conducted a comparative organizational case study27 of nine chiropractic clinics (Table 1) located in private sector medical facilities. For the purposes of this paper we use the terms “medical facilities” or “medical settings” to indicate conventional structures and processes that comprise the broad, long-established U.S. medical system, in which chiropractors previously had not been included at all, and currently have begun to be somewhat included. Starting with such facilities identified from a prior study,28 we used purposive sampling to select institutions with organizational diversity in facility type (e.g., hospital, ambulatory care), administrative structure, geographic location, and clinical focus (e.g., primary care, spine, integrative medicine). Some facilities had included doctors of chiropractic (DCs)—and in some instances complementary and integrative health providers such as acupuncturists or massage therapists—for over 10 years, whereas others had only recently started. We obtained written approval for each site's participation, first from the lead DC and then from a facility senior administrator. We conducted 2-day site visits at each facility during the period of October 2015 to June 2016. Site visit teams were composed of two to four researchers, with at least one investigator on each team having extensive experience conducting qualitative case studies. The Palmer College of Chiropractic Institutional Review Board (IRB Assurance No. X2015-6-2-G, approval date June 9, 2015) exempted the study under 45 CFR 46.101(b) due to its exclusive use of interview procedures and collection of existing documents. As a breach of confidentiality from a signed consent document was the primary risk to study participants, those interviewed provided verbal approval after reading an informational brochure and hearing a standardized informed consent script as approved by the IRB.
Table 1.
Private Sector Medical Facility Descriptions
| Facility type | Location | Business model | Associated practitioners in clinic or setting | Key affiliations and other attributes |
|---|---|---|---|---|
| Integrative primary care center | East Coast (urban) | Not-for-profit; Established by philanthropic grant; revenue from private insurance, Medicare, Medicaid, self-pay | Primary care physicians, nurse practitioner, clinical psychologist, naturopathic physician, acupuncturists, yoga specialist, chiropractor | Seeking accountable care organization and patient-centered medical home designations; weekly meeting for case management |
| Primary care clinic | Midwest (suburban) | Not-for-profit; revenue from private insurance, Medicare, Medicaid, and self-pay | Primary care physicians, endocrinologist, psychologists, podiatrist, rheumatologist, chiropractors | Affiliated with a regional health system |
| Spine center | East Coast (suburban) | Not-for-profit; revenue from private insurance, Medicare, Medicaid, and self-pay | Neurosurgeons, internist, orthopedist, physiatrists, physical therapists, physician assistant, chiropractors | Affiliated with a community hospital, regional health system, and state opioid reform task force; first community-based program in state to receive National Committee for Quality Assurance certification in Back Pain Recognition Program; engages in chiropractic clinical research |
| Ambulatory care center | East Coast (urban) | Not-for-profit; established by philanthropic grant; revenue from private insurance, Medicare, and self-pay | Internist, neurologist, psychiatrist, acupuncturist, occupational therapy, health coaching, physical therapist, massage therapists, yoga specialist, dietician, mindfulness instructor, chiropractors | Affiliated with a university, medical school, and a community hospital; engages in chiropractic clinical research and health science clinical education' twice monthly team meetings |
| Federally qualified health center | Midwest (suburban) | Not-for-profit; revenue from Medicare, Medicare, self-pay, and private insurance; sliding-scale fees available | Internists, obstetricians, pediatricians, nurse practitioners, physician assistants, dentists, pharmacists, chiropractors | Nine community-based clinics operating under Patient-Centered Medical Home designation; affiliated with a chiropractic college (student observations and internships; X-rays for clinic patients) |
| Cancer hospital network | South (suburban) | For-profit; revenue from private insurance, Medicare, Medicaid, and self-payment | Full-range of medical specialties focusing on cancer care; nursing, acupuncturists, naturopathic physicians, nutritionists, pain management, spiritual support, chiropractors | Affiliated with a national cancer hospital network, regional health science training programs; integrative approach blending cancer treatment with complementary therapies to address cancer side effects; involvement in cancer clinical trials |
| Sports medicine clinic | South (urban) | Not-for-profit; revenue from private insurance, Medicare, self-pay; noted some challenges initiating billing and reimbursement for chiropractic services | Orthopedists, primary care sports medicine physician, physician assistant, chiropractor | Affiliated with a university, medical school, and academic medical center; collegiate sports teams; medical residents rotate through clinic |
| Ambulatory care center | East Coast (suburban) | Not-for-profit; revenue from private insurance, Medicare, Medicaid, self-pay | Full range of medical specialties | Affiliated with a regional health system and serves as clinical site for a university-based medical school |
| Corporate health center | West Coast (urban) | For-profit on-site employee health clinic | Primary care physicians, dentists, optometrists, physical therapists, chiropractors, acupuncturist | Affiliated with a university, medical school, and academic medical center |
Data collection
Data collection included semi-structured interviews with facility stakeholders, a structured data table on background information completed by the lead DC, and review of archival material (e.g., policies, procedures, marketing/educational handouts). Interview guides were based on previous research by team members29,30 with content tailored to stakeholder role. Questions for administrative and clinical staff asked for detailed information about original context, clinic planning and implementation, clinic characteristics, care processes, program and financial impacts, and patient outcomes. Patient interviews focused on the experience of receiving chiropractic care within a medical setting. Interviews were audio recorded, with most conducted in person, although phone interviews were arranged for scheduling conflicts. Interview durations ranged from 10 to 15 min with patients (kept short to minimize participation burden), 45 min to 2 h with DCs, and 30 to 45 min for other stakeholders (senior leaders, other clinicians, clinic staff).
Data analysis
Audio recordings were transcribed verbatim. Quality control checks of transcription accuracy was performed on 10% of the interviews and deemed acceptable. An interdisciplinary team of three researchers (A.J.L., S.A.S., E.J.T.) conducted data management and coding using structured spreadsheet templates. Qualitative analysis used a directed content analysis approach31 following an extant conceptual model16 in which we identified thematic codes that were consistent with a priori concepts, along with emergent themes from transcript and document review. Analyses were organized in a systematic manner to facilitate site-by-site comparisons of key events in the clinic planning and implementation process, clinic structures, and outcomes.
Results
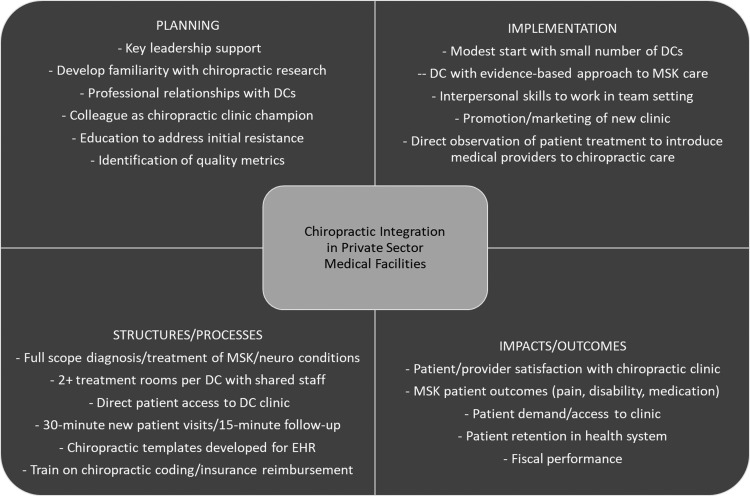
Table 1 depicts the medical facilities in our study including four primary or ambulatory care clinics, one multidisciplinary spine center, one specialty hospital, one corporate health clinic, one sports medicine clinic, and a community-based, federally qualified health center (FQHC). Primary facility affiliations included regional healthcare systems or hospital networks (n = 4) and university hospitals (n = 2). We completed 135 interviews (8–28 interviews/facility) with 46 non-DC clinicians (primarily medical doctors, but also doctors of osteopathy, nurse practitioners, physician assistants, psychologists, and acupuncturists), 25 DCs, 15 support staff, 23 administrators, and 26 patients. As summarized in Figure 1, our results provide a fundamental description of factors that may have bearing on the implementation of chiropractic clinics in medical settings. Results are described with respect to clinic planning, implementation, structures, processes, and outcomes/impacts.
FIG. 1.
Summary of key aspects of chiropractic integration into private sector medical settings. DCs, doctors of chiropractic; EHR, electronic health record.
Chiropractic clinic planning
Facilities varied in their impetus for starting a chiropractic clinic, but common themes included support from key leadership, familiarity with chiropractic research and practice, and professional relationships with given DCs. In some cases, the addition of chiropractic services was planned formally, organized within a group of new services (e.g., integrative medicine division), and coordinated across multiple stakeholders over an extended period. In others, chiropractic care was added to an existing service line and developed more organically. In all cases, the decision to introduce chiropractic services was seen as a presumptive positive step for the facility.
Chiropractic medicine is integral to the practice of medicine. It's not a set-aside. It's not a nice to have. It's not an alternative. It's an integral part of the way we should be practicing medicine. Our patients need it; and I think that any responsible hospital or community academic institution should have the service available to patients. (Associate Chief Medical Officer)
Some stakeholders reported initial cultural resistance to adding chiropractic, which was generally overcome through team meetings and mutual education emphasizing interprofessional communication and collaboration. Most sites identified continuous quality improvement processes introduced before clinic implementation that included metrics of patient outcomes and satisfaction, clinic access, and provider productivity.
Chiropractic clinic implementation
Regardless of facility catchment or physical plant size, sites initiated chiropractic services with one or, rarely, two full-time DCs. The first DCs hired often were identified by non-DC colleagues at the facility who “championed” the DC's inclusion on the team. The DC's clinical expertise was of paramount importance; however, stakeholders at all sites noted their organization was looking for additional elements when identifying the “right” chiropractor. These generally distilled into four themes: (1) an evidence-based approach to patient care; (2) appropriate interprofessional case management practices; (3) the interpersonal skills to work with a multidisciplinary team; and (4) the adoption of the organization's mission and values.
In our interviewing process, who the chiropractor is and whether they fit the culture is as important as their training. (CEO/physician)
Existing resources were adapted to provide clinic space and equipment, which expanded over time in most cases. Patient care schedules and appointment processes were based on existing clinical services, with input from the given DCs. Sites undertook varying degrees of promotion/marketing of the chiropractic clinic to the public, yet in several cases multiple stakeholders felt these efforts could have been more robust.
Facilities informed medical staff of this newly launched service in varying ways, ranging from formal department meetings and in-services to general announcements or ad hoc meetings. Direct observation of patient treatment was used sporadically across cases to introduce chiropractic care, which was viewed positively by clinicians who undertook this experience. Stakeholders reported interprofessional interaction during the course of patient care over time was the best facilitator for chiropractic integration.
Were all the physicians bought into chiropractic medicine from day one? No. It takes getting to know each other, getting to know how [DCs] practice … and when the referral transition begins, it's really a trust: “I trust you're going to take care of my patient, so I'm going to refer.” (Administrator)
Chiropractic clinic structures
Table 2 depicts the chiropractic clinics' structures. Staffing ranged from one to six DCs, with some DCs working as clinic administrators. Most shared medical assistants and clerical staff with other clinicians. Most DCs were salaried employees, although some were contractors or functioned under fee-for-service arrangements. The median reported annual salary for full-time DCs was $125,000 (range $75,000–$150,000).
Table 2.
Chiropractic Clinic Characteristics
| Year established | DC clinician staff | Support staff | Physical space | Patient access | Average weekly patient volume (scheduled visit duration) |
|---|---|---|---|---|---|
| 2014 | One full-time DC (salaried employee) | Two shared medical assistants and front office support staff | Two exam/treatment rooms | Provider referral; patient self-referral | Ten new patient visits (60 min); 50 follow-up visits (30 min) |
| 1996 | Two full-time and one part-time DCs (salaried employees) | One designated and one shared medical assistant, and shared front office support staff | Four exam/treatment rooms, with one designated for acupuncture cases | Provider referral; patient self-referral | Eighteen new patient visits (45 min); 215 follow-up visits (15 min) |
| 2006 | Six full-time DCs, two of whom also have administrative roles (salaried employees) | Office manager, medical assistants, and designated front office support staff | Five exam/treatment rooms; adjacent physical therapy suite with exercise equipment | Provider referral; patient self-referral | Ninety new patient visits (40 min); 300 follow-up visits (20 min) |
| 2008 | One full-time and one part-time DC (salaried employees) | Shared medical assistant and clinic coordinator as support staff | Three exam/treatment rooms | Provider referral; patient self-referral | Eight new patient visits (40 min); 65 follow-up visits (20 min) |
| 2011 | Two part-time DCs (fee-for-service contractors) | Shared medical assistants and clerical staff as support staff | Two exam/treatment rooms at each clinic | Provider referral | Six new patient visits (30–45 min); 37 follow-up visits (15–30 min) |
| 2012 | One full-time and one part-time DC, one of whom also has administrative role (salaried employees) | Shared administrative assistant as support staff | Three exam/treatment rooms shared with acupuncturists | In-patient: provider referral; out-patient: provider referral; patient self-referral | Fifteen new patient visits (30 min); 65 follow-up visits (15 min) |
| 2015 | One full-time DC (salaried employee) | Shared clinical coordinator and other support staff | Two to three exam/treatment rooms | Provider referral; patient self-referral | Fifteen new patient visits (30 min); 80 follow-up visits (15 min) |
| 2012 | Five full-time DCs, one of whom also has administrative role (salaried employees) | Multiple medical assistants, office manager, office coordinator, and insurance specialist | Two clinic locations; seven treatment rooms in larger clinic and two treatment rooms in smaller clinic | Provider referral; patient self-referral | Larger clinic:35 new patient visits (30–45 min); 375 follow-up visits (7.5–15 min); smaller clinic: 15 new patient visits (30–45 min); 65 follow-up visits (7.5–15 min) |
| 2008 | Two full-time DCs (salaried employees) | Shared clinical coordinator and other support staff | Two exam/treatment rooms | Provider referral; patient self-referral | Eight new patient visits (60 min); 90 follow-up visits (30 min) |
DC, Doctor of Chiropractic.
Treatment rooms often included the clinician's workstation and ranged in number from two rooms for single or dual-provider clinics to seven rooms shared by multiple DCs. Most DCs selected clinic equipment, although some reported compromising on preferred chiropractic tables to accommodate other clinicians (e.g., acupuncturists, massage therapists, or physical therapists) who shared treatment rooms. DCs considered most physical settings adequate, but several wished for more space to offer exercise therapy or educational programs.
All sites documented chiropractic care with virtually all patient care in electronic health record (EHR) systems. Most EHRs and/or the facility's information technology infrastructure provided electronic communication options, which the chiropractors and medical providers enjoyed as a support to interprofessional communication, real-time referral, patient scheduling, and coordinating care. However, billing and collection processes often were hindered by software incompatibility, clerical staff's unfamiliarity with chiropractic coding parameters, and/or insurance reimbursement processes that were more labor-intensive than for typical medical services.
Chiropractic clinic processes
Most sites allowed access to the chiropractic clinic from provider referral and patient direct access, although two settings (FQHC and specialty hospital) limited this to provider referral only. Most sites scheduled patients within a few days of the request, although some set appointments out 1–2 weeks due to the high demand for chiropractic services. An exception was a spine center that received a large proportion of its referrals through a hospital emergency department that triaged patients through a spine care pathway, which scheduled patients that day or within 24–48 h. New patient visits typically were scheduled for 30 min, with follow-up visits booked for 15 min. The efficiency of scheduling practices varied by site and, to some extent, hinged on whether clinical coordinators at the site scheduled patients or if this service was completed elsewhere. Some patients in a few facilities expressed frustration with scheduling delays due to the chiropractors' booked schedule or difficulties in using call-in centers or electronic self-scheduling mechanisms.
Virtually all DCs described their clinical practice as full scope diagnosis and management of musculoskeletal and neuromuscular conditions. While demographics varied, adults with spine and extremity pain or functional limitations comprised the typical patient. Most referring physicians gave a similar assessment.
If patients have a musculoskeletal diagnosis … I would like to think 100% of my patients that have that end up seeing a chiropractor. (Pain Medicine Physician)
Many DCs noted that clinicians and staff from within the healthcare system were on their patient rosters; some settings had added chiropractic care to the employee benefits package. Manual joint manipulation, mobilization, soft tissue therapies, exercise therapy, and patient education were the most common treatments offered.
Chiropractic clinic impacts/outcomes
Nearly all stakeholders had a very favorable perception of the chiropractic clinics. Among physicians, this was most commonly reported by those in primary care (internal medicine or family medicine), but also in neurology, physiatry (physical medicine and rehabilitation), pain medicine, oncology, occupational medicine, neurosurgery, orthopedic surgery, and other specialties:
My impression is [the chiropractors] provide really good medical care and in an integrated way and in a safe way. (Neurologist)
Many physicians reported that their positive opinion of the value of chiropractic care was shaped by various favorable experiences in coordinating patient care with the given DCs. Others who conveyed positive opinions about the chiropractic clinics included nurses, physician assistants, psychologists, and integrative therapy providers, such as acupuncturists and massage therapists.
They provide good care that's a necessary service for our patient population. (Nurse Manager)
Administrators overseeing the chiropractic clinics as well as senior facility leaders expressed favorable assessment of chiropractic clinic impact. In several facilities, the chiropractic clinic was identified as a standout among all clinical services in terms of patient access and patient satisfaction metrics.
[The chiropractors'] Ganey scores are off the chart … above the ninetieth [percentile] in all areas. Access to care, follow through, satisfaction with the office, satisfaction with patient care, satisfaction with testing, everything. (Administrative Executive Director)
Patients who used the chiropractic clinics reported high satisfaction with the quality of chiropractic care and with the fact that this care was coordinated with other providers in the system. Many patients stated they previously had not considered chiropractic care and only did so based on the high regard they had for the given facility, anticipating that a chiropractor at that facility would likely be highly competent.
I would not have been here without a referral, because I have never thought of chiropractic as something I wanted to try. [DC's] been thoroughly pleasant. She's been very complete. Getting my medical history and figuring out what was going on, I've been impressed with that. I've also been impressed with her ability to tie into the rest of the medical model … working in a team … that's tied into a wider medical care facility … I think is a good thing. (Patient)
All sites reported a trend of increased use over time, and most had expanded clinic staffing and space to accommodate rising patient volume. Despite increasing demand, some facilities have not increased the capacity (staffing/space) of the chiropractic clinic due to competing resource priorities. This has put pressure on patient access and care patterns, and revisions are being considered.
In fee-for-service sites, the variable (and considered low) reimbursement from third party payers for chiropractic services was reported to be a barrier to successful fiscal performance. In some instances, the chiropractic clinics were reported to be profit centers, in others they were neutral or loss leaders. In facilities in the process of adopting risk-based compensation models, the cost savings seen after including chiropractic services presented a stronger business case for clinic expansion. One facility identified a 50% decrease in unnecessary hospital admissions for low back pain cases and an overall savings of over $600,000 per year after implementing spine care pathways and chiropractic care.
Absolutely [chiropractic clinic is valued], especially now in the day and age that we live where we're looking to keep costs down, look[ing] for other alternatives besides prescription drugs and surgeries. I think it's definitely a good thing to have chiropractic integrated in with the hospital network. (Office Coordinator)
Discussion
This work presents a qualitative evaluation of chiropractic clinics at nine U.S. private sector medical facilities. Although inclusion of chiropractic services in medical facilities is a recent phenomenon, current clinical practice guidelines support increased use of interventions central to chiropractic care for common spinal conditions.4,32 Thus, chiropractic care likely will be implemented and/or expanded in such facilities.
The chiropractic profession has been described as at the “crossroads” between mainstream and integrative medicine.33 Although reasonable evidence supports the safety and effectiveness of multimodal chiropractic care, medical physician opinion of chiropractic practice is variable.34 Despite this, we found chiropractic services were used and valued by the physicians in our study sites. Certain facilities did experience some physician tensions regarding DC implementation—most notably in the early adoption phase—but these were overcome with communication, shared experiences, and relatively little effort in most cases. Study patients also were highly satisfied with chiropractic care, consistent with other published work.23,35 Some differences of opinion crossed patients, providers, and administrators regarding the optimal timing, frequency, and duration of chiropractic treatment plans, which is likely a reflection of the generally limited knowledge in the area of chiropractic dosage.36
Although our study facilities have not coordinated planning among themselves, it was striking to notice how similar the structures of chiropractic care were at each. All chiropractic clinics saw primarily musculoskeletal and neuromuscular conditions, with a wide range of associated comorbidities. Chiropractors were privileged for a full scope of diagnosis and management consistent with training and licensure, and treatment procedures invariably included manipulation and other manual therapies, patient education/active care, exercise, and lifestyle counseling. Depending on the specifics of a given patient case, collaboration between DCs and medical providers ranged from virtually no communication to ongoing in-person discussions. The DCs themselves also appeared strikingly similar in that they demonstrated and/or were perceived to have demonstrated exceptional clinical competence, an evidence-based practice approach, altruistic behavior, and collegial interpersonal traits. This cluster of characteristics has been associated with successful chiropractic integration in other settings.16
These healthcare facilities implemented chiropractic care under several different business models. While we did not collect quantitative data, it was reported that some chiropractic clinics were profitable, and others broke even or operated at a loss but were perceived to have secondary value, as has been noted in prior studies of conventional medical facilities seeking to establish and finance integrative medicine services.20,37,38 Cost savings by offsetting other healthcare services was reported to be a noteworthy accomplishment at one and a goal of another. Facilities will likely encounter differing incentives when implementing chiropractic services in fee-for-service versus value-based reimbursement models. Future work including formal healthcare economic analyses is needed to better understand the fiscal impacts of implementing chiropractic care in private medical facilities.
Since details of the actual population of chiropractic clinics within private sector medical facilities are unknown, our results are limited to the sample population. While we believe we captured a diverse representation of such clinics, further work is needed to assess this more fully. Using directed content analysis presents some inherent limitations since investigators approach the data with an informed theoretical construct, which can introduce bias. However, we feel this was minimized by our iterative approach to assessing emerging themes, and the participation of all four investigators to various degrees in the site visits, interviews, and data analysis.
Conclusions
We described the implementation of chiropractic services in a sample of nine U.S. private sector medical facilities. Chiropractic clinics were established within existing human resources, physical plant, information technology, and administrative support systems. Chiropractors were integrated in collaborative management of patients with musculoskeletal and co-morbid conditions. Chiropractic service delivery was perceived to have high value among patients, medical providers, and administration, with most facilities expanding their chiropractic workforce to meet increased demand. Patient clinical outcomes, patient satisfaction, provider productivity, and cost offset were identified as markers of clinic success.
Acknowledgments
The views expressed in this manuscript are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government. The authors thank Virginia Smith, MS, for her project coordination, and the lead DCs at each facility for their assistance in arranging the site visits. This study was funded by a grant from the NCMIC Foundation. Findings from this project were presented at the DC2017 Impact Spinal Health Conference, Washington, DC, in March 2017.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Bronfort G, Haas M, Evans R, et al. . Effectiveness of manual therapies: The UK evidence report. Chiropr Osteopat 2010;18:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clar C, Tsertsvadze A, Court R, et al. . Clinical effectiveness of manual therapy for the management of musculoskeletal and non-musculoskeletal conditions: Systematic review and update of UK evidence report. Chiropr Man Therap 2014;22:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bishop PB, Quon JA, Fisher CG, Dvorak MF. The Chiropractic Hospital-based Interventions Research Outcomes (CHIRO) study: A randomized controlled trial on the effectiveness of clinical practice guidelines in the medical and chiropractic management of patients with acute mechanical low back pain. Spine J 2010;10:1055–1064 [DOI] [PubMed] [Google Scholar]
- 4.Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians. Ann Intern Med 2017;166:514–530 [DOI] [PubMed] [Google Scholar]
- 5.Weeks WB, Goertz CM. Cross-sectional analysis of per capita supply of doctors of chiropractic and opioid use in younger Medicare beneficiaries. J Manipulative Physiol Ther 2016;39:263–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vogt MT, Kwoh CK, Cope DK, et al. . Analgesic usage for low back pain: Impact on health care costs and service use. Spine 2005;30:1075–1081 [DOI] [PubMed] [Google Scholar]
- 7.Rhee Y, Taitel MS, Walker DR, Lau DT. Narcotic drug use among patients with lower back pain in employer health plans: A retrospective analysis of risk factors and health care services. Clin Ther 2007;29(Suppl):2603–2612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Franklin GM, Rahman EA, Turner JA, et al. . Opioid use for chronic low back pain: A prospective, population-based study among injured workers in Washington state, 2002–2005. Clin J Pain 2009;25:743–751 [DOI] [PubMed] [Google Scholar]
- 9.Whedon JM, Toler AWJ, Goehl JM, Kazal LA. Association between utilization of chiropractic services for treatment of low-back pain and use of prescription opioids. J Altern Complement Med 2018; 24:552–556 [DOI] [PubMed] [Google Scholar]
- 10.Herman PM, Sorbero ME, Sims-Columbia AC. Complementary and alternative medicine services in the military health system. J Altern Complement Med 2017;23:837–843 [DOI] [PubMed] [Google Scholar]
- 11.Lisi AJ, Goertz C, Lawrence DJ, Satyanarayana P. Characteristics of Veterans Health Administration chiropractors and chiropractic clinics. J Rehabil Res Dev 2009;46:997–1002 [DOI] [PubMed] [Google Scholar]
- 12.Dunn AS, Green BN, Gilford S. An analysis of the integration of chiropractic services within the United States military and veterans' health care systems. J Manipulative Physiol Ther 2009;32:749–757 [DOI] [PubMed] [Google Scholar]
- 13.Goertz CM, Long CR, Hondras MA, et al. . Adding chiropractic manipulative therapy to standard medical care for patients with acute low back pain: Results of a pragmatic randomized comparative effectiveness study. Spine 2013;38:627–634 [DOI] [PubMed] [Google Scholar]
- 14.Lisi AJ, Brandt CA. Trends in the use and characteristics of chiropractic services in the Department of Veterans Affairs. J Manipulative Physiol Ther 2016;39:381–386 [DOI] [PubMed] [Google Scholar]
- 15.Williams VF, Clark LL, McNellis MG. Use of complementary health approaches at military treatment facilities, active component, U.S. Armed Forces, 2010–2015. MSMR 2016;23:9–22 [PubMed] [Google Scholar]
- 16.Lisi AJ, Khorsan R, Smith MM, Mittman BS. Variations in the implementation and characteristics of chiropractic services in VA. Med Care 2014;52(Suppl 5):S97–S104 [DOI] [PubMed] [Google Scholar]
- 17.Fletcher CE, Mitchinson AR, Trumble E, et al. . Providers' and administrators' perceptions of complementary and integrative health practices across the Veterans Health Administration. J Altern Complement Med 2016;23:26–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Branson RA. Hospital-based chiropractic integration within a large private hospital system in Minnesota: A 10-year example. J Manipulative Physiol Ther 2009;32:740–748 [DOI] [PubMed] [Google Scholar]
- 19.Carucci M, Lisi A. CAM services provided at select integrative medicine centers: What do their websites tell us? Topics Integr Health Care 2010;1:1..1004. [Google Scholar]
- 20.Davis MA, McDevitt L, Alin K. Establishing a chiropractic service in a rural primary health care facility. J Altern Complement Med 2007;13:697–702 [DOI] [PubMed] [Google Scholar]
- 21.Berwick DM, Nolan TW, Whittington J. The triple aim: Care, health, and cost. Health Affairs 2008;27:759–769 [DOI] [PubMed] [Google Scholar]
- 22.Carey TS, Garrett J, Jackman A, et al. . The outcomes and costs of care for acute low back pain among patients seen by primary care practitioners, chiropractors, and orthopedic surgeons. The North Carolina Back Pain Project. N Engl J Med 1995;333:913–917 [DOI] [PubMed] [Google Scholar]
- 23.Goertz CM, Salsbury SA, Long CR, et al. . Patient-centered professional practice models for managing low back pain in older adults: A pilot randomized controlled trial. BMC Geriatr 2017;17:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hertzman-Miller RP, Morgenstern H, Hurwitz EL, et al. . Comparing the satisfaction of low back pain patients randomized to receive medical or chiropractic care: Results from the UCLA low-back pain study. Am J Public Health 2002;92:1628–1633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kosloff TM, Elton D, Shulman SA, et al. . Conservative spine care: Opportunities to improve the quality and value of care. Popul Health Manag 2013;16:390–396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin BI, Gerkovich MM, Deyo RA, et al. . The association of complementary and alternative medicine use and health care expenditures for back and neck problems. Med Care 2012;50:1029–1036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yin RK. Case Study Research and Applications: Design and Methods. 6th ed. Thousand Oaks, CA: SAGE Publications, 2018 [Google Scholar]
- 28.Salsbury SA, Goertz CM, Twist EJ, Lisi AJ. Integration of doctors of chiropractic into private sector health care facilities in the United States: A descriptive survey. J Manipulative Physiol Ther 2018;41:149–155 [DOI] [PubMed] [Google Scholar]
- 29.Christianson JB, Finch MD, Choate CG, Findlay B. Consumer-focused strategies of innovative hospitals: The role of complementary therapies. Explore (NY) 2007;3:158–160 [DOI] [PubMed] [Google Scholar]
- 30.Khorsan R, Cohen AB, Lisi AJ, et al. . Mixed-methods research in a complex multisite VA health services study: Variations in the implementation and characteristics of chiropractic services in VA. Evid Based Complement Alternat Med 2013;2013:701280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–1288 [DOI] [PubMed] [Google Scholar]
- 32.Côté P, Wong JJ, Sutton D, et al. . Management of neck pain and associated disorders: A clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur Spine J 2016;25:2000–2022 [DOI] [PubMed] [Google Scholar]
- 33.Meeker WC, Haldeman S. Chiropractic: A profession at the crossroads of mainstream and alternative medicine. Ann Intern Med 2002;136:216–227 [DOI] [PubMed] [Google Scholar]
- 34.Busse JW, Jacobs C, Ngo T, et al. . Attitudes toward chiropractic: A survey of North American orthopedic surgeons. Spine 2009;34:2818–2825 [DOI] [PubMed] [Google Scholar]
- 35.Weeks WB, Goertz CM, Meeker WC, Marchiori DM. Public perceptions of doctors of chiropractic: Results of a national survey and examination of variation according to respondents' likelihood to use chiropractic, experience with chiropractic, and chiropractic supply in local health care markets. J Manipulative Physiol Ther 2015;38:533–544 [DOI] [PubMed] [Google Scholar]
- 36.Haas M, Vavrek D, Peterson D, et al. . Dose-response and efficacy of spinal manipulation for care of chronic low back pain: A randomized controlled trial. Spine J 2014;14:1106–1116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hunter J, Corcoran K, Phelps K, Leeder S. The challenges of establishing an integrative medicine primary care clinic in Sydney, Australia. J Altern Complement Med 2012;18:1008–1013 [DOI] [PubMed] [Google Scholar]
- 38.Dusek JA, Griffin KH, Finch MD, et al. . Cost savings from reducing pain through the delivery of integrative medicine program to hospitalized patients. J Altern Complement Med 2018;24:557–563 [DOI] [PMC free article] [PubMed] [Google Scholar]