Abstract
The purpose of the present study was to compare the results of open subpectoral biceps tenodesis and arthroscopic proximal biceps tenodesis for treating long head of biceps (LHB) lesions. From January 2015 to June 2016, a total of 259 patients underwent LHB tenodesis surgery. Among them, 117 patients (60 females and 57 males) who met the inclusion and exclusion criteria were enrolled into the present study and were randomly divided into two groups, including an open subpectoral tenodesis group (OSPBT; n=62) and an arthroscopic proximal tenodesis group (ASPBT; n=55). All patients were followed up for at least 12 months. The demographic characteristics of each patient were recorded in detail. Moreover, clinical examinations of LHB lesions, such as shoulder range of motion (ROM), Visual Analog Scale (VAS) scores (0, no pain, to 10, most severe pain), American Shoulder and Elbow Surgeons (ASES) scores, and Constant-Murley shoulder outcome scores, were investigated prior to surgery, as well as 3, 6 and 12 months after surgery. Postoperative complications were also comprehensively investigated. There were no significant differences in sex, body mass index, dominant shoulder, duration of pain, injury type and operation time between the groups. The mean length of hospital stay in the ASPBT group was significantly lower than that of the OSPBT group (5.4±1.8 days vs. 9.3±2.9 days; P<0.05). The clinical outcomes, including shoulder ROMs, VAS scores, ASES scores and Constant-Murley shoulder outcome scores, were significantly improved after either OSPBT or ASPBT treatment. Specifically, the VAS score, incidence of postoperative stiffness and bicipital groove tenderness in the OSPBT group were significantly lower than those in the ASPBT group at 3 months post-surgery (P<0.05). Additionally, there were no significant difference in the improvement of other clinical outcomes and postoperative complications between the two groups. ASPBT and OSPBT were both effective and safe techniques for treating LHB lesions. However, tenderness of the bicipital groove was more common in the early stages of recovery post-surgery in the ASPBT group, which may be related to tendinitis of the LHB in the bicipital groove.
Keywords: long head of bicep, open subpectoral tenodesis, arthroscopic proximal tenodesis
Introduction
Lesions of the long head of the biceps (LHB) tendon have been widely considered to be a notable trigger for anterior shoulder pain (1). Patients with mild symptoms of tendinopathy or partial LHB tears (<50% of tendon width), non-surgical treatments, such as rest, physical therapy, non-steroidal anti-inflammatory drug treatment and intra-articular injection of corticosteroids, can be effective; however, for most cases, including partial-thickness LHB tears, LHB instability/subluxation, associated rotator cuff tears, biceps pulley lesions and superior labrum anterior-posterior (SLAP) lesions, surgical intervention is still the preferred method of treatment (2–4). Biceps tenotomy and tenodesis have become two of the most commonly performed surgical procedures for lesions of the LHB tendons (5). Although tenotomy is a relatively simple and reproducible procedure which can significantly relieve shoulder pain without postoperative rehabilitation, it is only indicated for patients aged over 60 years, who are not involved in heavy labor and high-demand activities (6). Moreover, tenotomy has a higher incidence of cosmetic deformity (Popeye sign) than that of tenodesis (43 vs. 8%) (7). Therefore, tenodesis is currently the preferred technique for treating LHB lesions as it provides a better recovery of physical activity, fewer cosmetic deformities and more closely aligns with normal anatomy, despite a longer postoperative rehabilitation time and higher technical demand (8).
Numerous techniques have been applied with LHB tenodesis, including arthroscopic techniques and minimally open or open surgeries (9). Moreover, tenodesis sites can be positioned in the suprapectoral location just proximal to the pectoralis major tendon, the subpectoral location, or other positions such as the conjoint tendon or soft tissue sites (10). Although comparably preferable clinical outcomes have been reported in various studies investigating both open subpectoral biceps tenodesis (OSPBT) and arthroscopic suprapectoral biceps tenodesis (ASPBT), the results are still controversial and there is limited information regarding postoperative complications, such as re-tears, implant failure, nerve and vascular injuries, bicipital groove tenderness, deformities, and postoperative infection and stiffness (11,12).
The present study retrospectively investigated 117 cases who underwent LHB tenodesis. OSPBT and ASPBT were compared, including pre-/post-surgery shoulder range of motion (ROM), visual analog scale (VAS) scores, American Shoulder and Elbow Surgeons (ASES) scores, Constant-Murley shoulder outcome scores and postoperative complications. The purpose of the present study was to identify the differences in clinical outcomes and related complications between OSPBT and ASPBT.
Materials and methods
Study design and patients
This retrospective, single-center study was performed based on a protocol approved by the institutional review board at The First Affiliated Hospital of Anhui Medical University (Hefei, China), and was in accordance with the Good Clinical Practice guidelines (13) and the principles of the Declaration of Helsinki. Medical records of adult patients who had received LHB tenodesis surgeries at the Department of Orthopedics, The First Affiliated Hospital of Anhui Medical University between January 2015 and June 2016 were reviewed (n=259). The inclusion criteria were as follows: The diagnosis of SLAP tears; complete or partial tearing of the LHB; biceps lesions (tenosynovitis); and LHB instability/subluxation or associated rotator cuff tears (small- or medium-sized). Additionally, the inclusion criteria also included the presence of LHB lesion symptoms and signs, such as anterior shoulder pain, bicipital groove tenderness and positive results from the Speeds, Yergason's and O'Brien's tests; conservative treatments for at least 3 months; complete clinical evaluations and MRI scans; and followed up for more than 12 months. The exclusion criteria were as follows: Patients <18 years old; glenoid labrum lesions; glenohumeral instability; preoperative ROM deficit due to frozen shoulder or glenohumeral arthritis; contralateral shoulder injury or surgery; shoulder arthroplasty; massive rotator cuff tear; and neuromuscular disorder-related shoulder pain.
Grouping and treatments
A total of 117 patients (60 women and 57 men) who met the inclusion and exclusion criteria were enrolled in this study and randomly divided into two groups, the OSPBT group (n=62) and the ASPBT group (n=55). All tenodesis procedures (OSPBT and ASPBT) were performed by the same group of experienced orthopedic surgeons at The First Affiliated Hospital of Anhui Medical University. The choice of surgical technique was determined by surgeon preference.
Surgical technique and rehabilitation
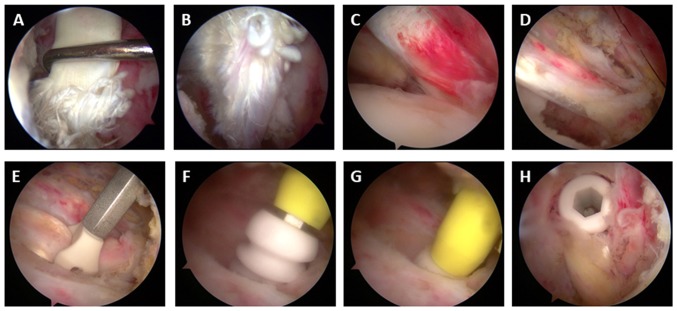
OSPBT was performed using the surgical technique described by Mazzocca et al (14). After positioning the upper arm in the external rotation position, the inferior margin of the pectoralis major was palpated and a 2–3 cm incision was made near the inferior margin of the pectoralis major in the axillary region. A Hohmann retractor was placed under the pectoralis major and a Chandler retractor was placed over the medial side of the humerus to enlarge the operative visual field. Subsequently, the LHB was isolated and extracted from the glenohumeral joint and LHB sheath by using a right-angle clamp (Fig. 1). The end of the LHB (3–4 cm) was removed and the terminal 3 cm of the tendon was stitched using a no. 2 high-strength suture. An appropriately sized interference screw implant (7 mm interference bio-screw; Arthrex GmbH) was used to affix the tendon into the reamed tenodesis site.
Figure 1.
A representative image of the isolation and extraction of long head of biceps tendon in the open subpectoral tenodesis procedure.
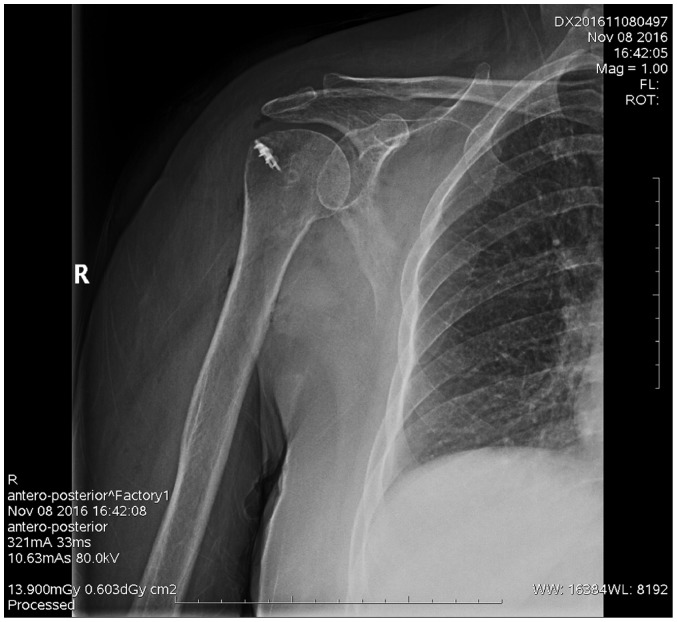
ASPBT was performed according to previously reported surgical techniques (15,16). After positioning the upper arm in the external rotation position, a probe was used to locate the major tubercle and medial side of the intertubercular groove. The arthroscope was repositioned into the lateral portal and the biceps tendon was identified in the sheath within the intertubercular groove. As shown in Fig. 2, coblation was then used to release the biceps tendon from the sheath and an appropriate position for tenodesis was localized proximal to the pectoralis major tendon. Subsequently, a portal was established at this location and a guide wire was placed. A 7.5 mm reamer was drilled in the center of intertubercular groove to the appropriate depth. A polydioxanone suture was used to stabilize the proximal tendon and the Swivelock screw (Arthrex GmbH) was then used to affix the tendon into the reamed tenodesis site. A postoperative X-ray examination was performed to identify the position (Fig. 3).
Figure 2.
Surgical procedures during the arthroscopic suprapectoral biceps tenodesis. (A) Identifying and (B) releasing the biceps tendon from its sheath, and (C) locating and (D) identifying the appropriate position for tenodesis. (E) Positioning, (F) drilling, (G) stabilizing and (H) affixing the tendon.
Figure 3.
A representative post-operative X-ray examination from the arthroscopic suprapectoral biceps tenodesis group.
Both treatment groups received the same postoperative rehabilitation program. In general, only passive exercises were performed in the first 6 weeks. Thereafter, active-assisted ROM and active exercises were permitted for the subsequent 6 weeks. From the 13th week, patients could begin biceps strengthening exercises. Specifically, for patients with rotator cuff tears and LHB lesions, the wounded shoulder was fixed with an abduction brace for 4 weeks and only passive exercises of elbow joints could be performed for the first 2 of these 4 weeks. Thereafter, passive exercises of the shoulder joints were allowed. For patients without rotator cuff tears, the wounded shoulder was fixed with an abduction brace for 2 weeks and only passive exercises of the shoulder and elbow joints were performed during the first 6 weeks.
Demographic characteristics and clinical examinations
The demographics of each patient were recorded in detail, including the age, sex, body mass index (BMI), smoking history, dominant shoulder, duration of pain, injury types, operation time and hospital stay. Moreover, clinical examinations of LHB lesions such as shoulder ROM, VAS scores (0, no pain, to 10, most severe pain), ASES scores and Constant-Murley shoulder outcome scores (Constant scores) were investigated preoperatively, as well as at 3, 6 and 12 months post-surgery. All patients received at least 12 months follow-up care after hospital discharge and the patients were advised to attend the associated outpatient clinic to complete these clinical assessments during this period. A total of 12 months following the surgery, the patients were contacted for follow-up using a telephone enquiry investigating abnormal signs of pain, instability or deformity, as had been mutually agreed. All patients were invited to the associated outpatient clinic if any abnormal signs appeared. Comprehensive evaluations and imaging examinations were performed to clarify the injury types and degrees. Furthermore, postoperative complications, including re-tears, implant failure, nerve and vascular injuries, bicipital groove tenderness, deformities (Popeye sign), postoperative infection and stiffness were comprehensively investigated.
Statistical analysis
Statistical analysis was performed using SPSS software (version 19.0; IBM Corp.). The results are presented as the mean ± SD. Student's t-test and one/two-way ANOVAs were applied for continuous data, with Bonferroni post-hoc tests. χ2 tests were applied for the categorical data. P<0.05 was considered to indicate a statistically significant difference.
Results
Demographic characteristics
A total of 117 adult patients (60 women and 57 men) with LHB lesions who met the inclusion and exclusion criteria were enrolled in the present study and divided into two groups, the OSPBT group (n=62) and the ASPBT group (n=55). The mean age of all 117 patients was 56.51±8.79 years (range, 32–78 years) and there were no significant differences in the mean ages between the OSPBT group (57.36±8.81 years old) and the ASPBT group (55.05±8.74 years old) (P>0.05). As shown in Table I, there were no significant differences in gender, BMI, dominant shoulder, duration of pain, injury type and operation time between the two groups. The mean number of days of hospital stay in the ASPBT group was significantly lower than that in the OSPBT group (5.4±1.8 vs. 9.3±2.9 days; P<0.05). All patients had completed at least 12 months of follow-up and the mean lengths of follow-up treatment in the OSPBT group and the ASPBT group were 20.11±7.10 and 20.51±7.47 months, respectively. A total of 34 patients abandoned the follow-up study after 12 months, including 18 patients from the OSPBT group and 16 patients from the ASPBT group.
Table I.
Demographic characteristics of patients in the OSPBT group and the ASPBT group.
| Variable | OSPBT (n=62) | ASPBT (n=55) | P-value |
|---|---|---|---|
| Age, years | 57.36±8.81 | 55.05±8.74 | 0.64 |
| Female, n (%) | 33 (53.2%) | 29 (52.7%) | 0.85 |
| BMI, kg/m2 | 28.38±2.69 | 28.77±2.41 | 0.39 |
| Smoking, n (%) | 9 (14.5%) | 7 (12.7%) | 0.72 |
| Dominant shoulder | |||
| Right, n (%) | 38 (61.3%) | 34 (61.8%) | 0.81 |
| Duration of pain, months | 16.16±7.77 | 15.74±7.79 | 0.65 |
| Injury types, n (%) | |||
| SLAP tear | 30 (48.4%) | 20 (36.4%) | 0.14 |
| Biceps tear | 37 (59.7%) | 32 (58.2%) | 0.74 |
| Tenosynovitis | 9 (14.5%) | 5 (9.1%) | 0.21 |
| LHB subluxation | 18 (29.0%) | 15 (27.3%) | 0.53 |
| Rotator cuff tear | 55 (88.7%) | 46 (83.6%) | 0.48 |
| Small-sized | 26 (41.9%) | 21 (38.2%) | 0.51 |
| Medium-sized | 29 (46.8%) | 25 (45.5%) | 0.24 |
| Operation time, h | 2.63±0.63 | 3.12±0.75 | 0.09 |
| Hospital stay, days | 9.3±2.9 | 5.4±1.8 | 0.03 |
| Follow-up, months | 20.11±7.10 | 20.51±7.47 | 0.78 |
Data are presented as the mean ± SD or n (%), and P<0.05 was considered to indicate a statistically significant difference when comparing the OSPBT group with the ASPBT group. ASPBT, arthroscopic suprapectoral biceps tenodesis; BMI, body mass index; OSPBT, open subpectoral biceps tenodesis; SLAP, superior labrum anterior-posterior.
Clinical examinations
The clinical examinations, including VAS scores, Constant scores and ASES scores were taken preoperatively, as well as 3, 6 and 12 months post-surgery. VAS scores (0, no pain, to 10, most severe pain) were applied for evaluating shoulder pain. As shown in Table II, the VAS scores in both groups at 3, 6 and 12 months post-surgery were significantly lower than the VAS scores of both groups preoperatively (P<0.05). At 3 months post-surgery, the VAS score in OSPBT group (2.41±0.76) was significantly lower than that in the ASPBT group (3.59±1.02; P<0.05). Moreover, there were no significant differences in the VAS scores between the OSPBT group and the ASPBT group preoperatively, at 6 or 12 months post-surgery (P>0.05). The average Constant scores and ASES scores between the two groups are also presented in Table II. The Constant scores and ASES scores of both groups at 3, 6 and 12 months post-surgery were significantly higher than the respective scores preoperatively in both groups (P<0.05). However, there were no significant differences observed in the Constant scores and ASES scores between the OSPBT group and the ASPBT group at any stage of the study (P>0.05).
Table II.
Clinical examinations of patients in the OSPBT group and the ASPBT group.
| Variable | OSPBT | ASPBT |
|---|---|---|
| VAS score | ||
| Preoperative | 5.02±1.05 | 4.92±1.51 |
| 3 months postoperatively | 2.41±0.76a,b | 3.59±1.02a |
| 6 months postoperatively | 1.64±0.81a | 1.77±0.81a |
| 12 months postoperatively | 0.95±0.65a | 1.18±1.36a |
| Constant score | ||
| Preoperative | 53.75±7.19 | 52.08±10.54 |
| 3 months postoperatively | 63.25±7.01a | 60.61±6.39a |
| 6 months postoperatively | 81.16±6.32a | 78.64±5.14a |
| 12 months postoperatively | 90.71±4.29a | 90.38±3.14a |
| ASES score | ||
| Preoperative | 52.89±8.16 | 49.51±11.05 |
| 3 months postoperatively | 68.39±3.98a | 64.84±4.07a |
| 6 months postoperatively | 80.52±5.93a | 78.36±5.53a |
| 12 months postoperatively | 89.05±4.02a | 88.51±3.42a |
Data presented as the mean ± SD or n (%), and P<0.05 was considered to indicate a statistically significant difference.
P<0.05 vs. respective preoperative score
P<0.05 vs. ASPBT. ASES, American Shoulder and Elbow Surgeons; ASPBT, arthroscopic suprapectoral biceps tenodesis; Constant score, Constant-Murley shoulder outcome scores; OSPBT, open subpectoral biceps tenodesis; VAS, visual analog scale.
ROM
The active ROMs, including forward elevation, abduction and external rotation, were evaluated preoperatively and at 12 months post-surgery. As shown in Fig. 4, the postoperative active ROMs were significantly higher than the preoperative active ROMs in both groups (P<0.05). However, there were no significant differences in the preoperative or postoperative active ROMs between the two groups (P>0.05).
Figure 4.
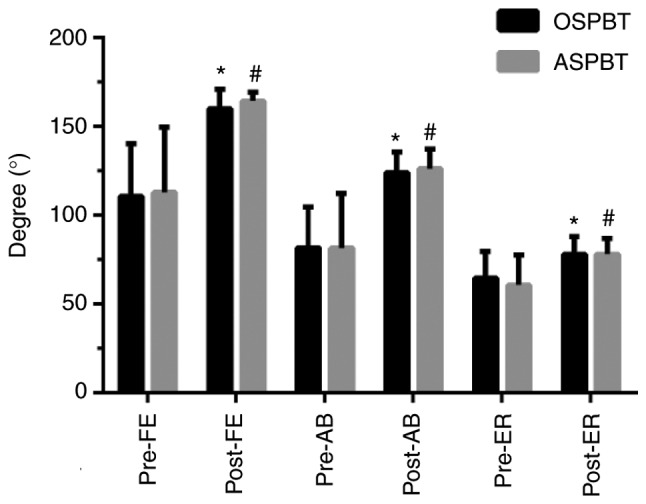
Degrees of active range of motion in the OSPBT and the ASPBT groups. Data are presented as the mean ± SD or n (%), and P<0.05 was considered to indicate a statistically significant difference. *P<0.05 vs. respective OSPBT preoperative score; #P<0.05 vs. respective ASPBT preoperative score. Pre-FE, preoperative forward elevation; post-FE, postoperative forward elevation; pre-AB, preoperative abduction; post-AB, postoperative abduction; pre-ER, preoperative external rotation; post-ER, Postoperative external rotation; ASPBT, arthroscopic suprapectoral biceps tenodesis; OSPBT, open subpectoral biceps tenodesis.
Postoperative complications
The postoperative complications, including re-tears, deformities (Popeye sign), implant failure, neurovascular injury, postoperative infection, stiffness and bicipital groove tenderness, were comprehensively investigated. As shown in Table III, there were no incidences of re-tears, deformities (Popeye sign), implant failure, neurovascular injury or postoperative infection. Moreover, the incidence of postoperative stiffness in the OSPBT group (3, 5.5%) was significantly lower than that in the ASPBT group (11, 17.7%; P<0.05). Furthermore, the incidences of bicipital groove tenderness in both two groups at 3, 6 and 12 months post-surgery were significantly lower than the incidences of bicipital groove tenderness in both groups on discharge day (P<0.05). At 3 months post-surgery, the incidence of bicipital groove tenderness in OSPBT group (10, 16.1%) was significantly lower than that in ASPBT group (23, 41.8%; P<0.05). Similarly, at 6 months post-surgery, the incidence of bicipital groove tenderness in the OSPBT group (4, 6.4%) was significantly lower than that in the ASPBT group (12, 21.8%; P<0.05). However, there was no significant difference in the incidences of bicipital groove tenderness between the OSPBT group and the ASPBT group at 12 months post-surgery (P>0.05).
Table III.
Postoperative complications of patients in the OSPBT group and the ASPBT group.
| Variable | OSPBT (%) | ASPBT(%) |
|---|---|---|
| Re-tears, n (%) | 0 (0) | 0 (0) |
| Popeye sign, n (%) | 0 (0) | 0 (0) |
| Implant failure, n (%) | 0 (0) | 0 (0) |
| Neurovascular injury, n (%) | 0 (0) | 0 (0) |
| Postoperative infection, n (%) | 0 (0) | 0 (0) |
| Stiffness, n (%) | 3 (5.5)b | 11 (17.7) |
| Bicipital groove tenderness, n (%) | ||
| Discharge day | 39 (62.9) | 37 (67.3) |
| 3 months postoperatively | 10 (16.1)a,b | 23 (41.8)a |
| 6 months postoperatively | 4 (6.4)a,b | 12 (21.8)a |
| 12 months postoperatively | 0 (0)a | 3 (5.4)a |
Data are presented as the mean ± SD or n (%), and P<0.05 was considered to indicate a statistically significant difference.
P<0.05 vs. respective group on discharge day
P<0.05 vs. ASPBT. ASPBT, arthroscopic suprapectoral biceps tenodesis; OSPBT, open subpectoral biceps tenodesis.
Discussion
In recent years, various techniques regarding LHB tenodesis have been reported, and among them, bony interference fixation tenodesis (BIFT) is the most widely used technique, exhibiting good clinical outcomes and a low rate of surgical complications (9,17). Furthermore, soft tissue fixation (STT) is associated with excellent performance, without producing subscapular lesions or Popeye's deformity (18). Hwang et al (19) suggested that arthroscopic BIFT at the distal bicipital groove produced a greater improvement in the elbow flexion strength index and a lower failure rate than STT. Chiang et al (20) investigated the biomechanical characteristics of suture anchor and interference screw fixation in subpectoral tenodesis, and reported that both of the techniques led to an equivalent ultimate failure load and stiffness. However, the interference screw fixation technique was associated with significantly less displacement in response to cyclic and failure loading.
In regards to the safety of tenodesis, brachial plexopathy (21), musculocutaneous nerve injury and lateral antebrachial cutaneous nerve injury (22,23) have been reported after OSPBT. Ma et al (24) reported a case of direct musculocutaneous nerve injury in subpectoral tenodesis, whereby the nerve was wrapped around the LHB in the revision surgery. Sethi et al (25) assessed the risk for neurological injury of open suprapectoral and subpectoral biceps tenodesis in cadavers, and suggested that penetration of the posterior humeral cortex at the suprapectoral location results in a high risk of damaging the axillary nerve due to its proximity, and should be avoided. Subpectoral bicortical button fixation drilled uniformly perpendicular to the axis of the humerus is performed in a safe location with respect to the axillary nerve. In this present study, it was found that the incidences of postoperative complications, such as re-tears, deformities (Popeye sign), implant failure, neurovascular injury and postoperative infection, were nil. Therefore, both suprapectoral and subpectoral tenodesis were deemed safe.
The results showed that the clinical outcomes, including shoulder ROMs, VAS scores, ASES scores and Constant scores, were significantly improved after OSPBT or ASPBT. Moreover, there were no significant differences in the improvement of clinical outcomes between the two groups. However, Gilmer et al (26) suggested that only 17% length of LHB tendon can be observed in ASPBT, and only 32% length of LHB can be observed in ASPBT even when the tendon is pulled into the joint with an arthroscopic grasper. This indicated that OSPBT may be the optimal method of tenodesis for the complete removal of all hidden biceps lesions and for the revision of failed postoperative LHB lesions (27). Kolz et al (28) compared the mechanical properties between OSPBT and ASPBT, and indicated that LHB in the suprapectoral region tended to have higher tensile strength than in the subpectoral region, and LHB tenodesis in the suprapectoral region could withstand higher failure loads and become more arthroscopically accessible. Furthermore, this present study found that the incidences of postoperative stiffness and bicipital groove tenderness in the ASPBT group were significantly higher than those in the OSPBT group. It was also reported that the VAS score in the OSPBT group was significantly lower than that in the ASPBT group at 3 months post-surgery. Similarly, Yi et al (29) suggested that VAS scores and tenderness at the bicipital groove were significantly decreased in the OSPBT group at the early stage post-surgery. However, there were no significant differences in ASES and Constant scores in this present study. This indicated that the early results of VAS score (within 3 months post-surgery) and bicipital groove tenderness (within 6 months post-surgery) for subpectoral tenodesis was related to the removal of the biceps tendinitis.
There were several limitations with this study, including: An insufficient number of enrolled patients; the absence of extended follow-up research; a lack of MRI data from enrolled patients preoperatively and postoperatively, especially MRI changes during the follow-up; and the study was not a prospective, randomized controlled trial.
In conclusion, the clinical outcomes, including shoulder ROMs, VAS scores, ASES scores and Constant scores, were significantly improved after OSPBT or ASPBT. Specifically, the VAS score, and the incidences of postoperative stiffness and bicipital groove tenderness in the OSPBT group were significantly lower than those in the ASPBT group at 3 months post-surgery. Moreover, there were no significant differences in the improvement of other clinical outcomes and postoperative complications between the two groups.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to statutory provisions regarding data and privacy protection but are available from the corresponding author on reasonable request.
Authors' contributions
JT, BX and RG were involved in the conception and design of the study; the collection, assembly, analysis and interpretation of the data; and in drafting of the article. They also provided statistical expertise and contributed to the final approval of the article, provision of study materials, technical and logistical support as well as critical revision of the article for important intellectual content. All authors contributed equally to this article.
Ethics approval and consent to participate
This study was approved by the ethics committee of The First Affiliated Hospital of Anhui Medical University (protocol no. PJ2014-10-04). Participants provided their written informed consent to participate in this study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Nair R, Kahlenberg CA, Patel RM, Knesek M, Terry MA. All-arthroscopic suprapectoral biceps tenodesis. Arthrosc Tech. 2015;4:e855–e861. doi: 10.1016/j.eats.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Werner BC, Brockmeier SF, Gwathmey FW. Trends in long head biceps tenodesis. Am J Sports Med. 2015;43:570–578. doi: 10.1177/0363546514560155. [DOI] [PubMed] [Google Scholar]
- 3.Levy DM, Meyer ZI, Campbell KA, Bach BR., Jr Subpectoral biceps tenodesis. Am J Orthop (Belle Mead NJ) 2016;45:68–74. [PubMed] [Google Scholar]
- 4.AlQahtani SM, Bicknell RT. Outcomes following long head of biceps tendon tenodesis. Curr Rev Musculoskelet Med. 2016;9:378–387. doi: 10.1007/s12178-016-9362-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel KV, Bravman J, Vidal A, Chrisman A, McCarty E. Biceps tenotomy versus tenodesis. Clin Sports Med. 2016;35:93–111. doi: 10.1016/j.csm.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Koh KH, Ahn JH, Kim SM, Yoo JC. Treatment of biceps tendon lesions in the setting of rotator cuff tears: Prospective cohort study of tenotomy versus tenodesis. Am J Sports Med. 2010;38:1584–1590. doi: 10.1177/0363546510364053. [DOI] [PubMed] [Google Scholar]
- 7.Slenker NR, Lawson K, Ciccotti MG, Dodson CC, Cohen SB. Biceps tenotomy versus tenodesis: Clinical outcomes. Arthroscopy. 2012;28:576–582. doi: 10.1016/j.arthro.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 8.Werner BC, Evans CL, Holzgrefe RE, Tuman JM, Hart JM, Carson EW, Diduch DR, Miller MD, Brockmeier SF. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: A comparison of minimum 2-year clinical outcomes. Am J Sports Med. 2014;42:2583–2590. doi: 10.1177/0363546514547226. [DOI] [PubMed] [Google Scholar]
- 9.Abraham VT, Tan BH, Kumar VP. Systematic review of biceps tenodesis: Arthroscopic versus open. Arthroscopy. 2016;32:365–371. doi: 10.1016/j.arthro.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 10.Werner BC, Lyons ML, Evans CL, Griffin JW, Hart JM, Miller MD, Brockmeier SF. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: A comparison of restoration of length-tension and mechanical strength between techniques. Arthroscopy. 2015;31:620–627. doi: 10.1016/j.arthro.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 11.Chung SW, Huong CB, Kim SH, Oh JH. Shoulder stiffness after rotator cuff repair: Risk factors and influence on outcome. Arthroscopy. 2013;29:290–300. doi: 10.1016/j.arthro.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 12.Johannsen AM, Macalena JA, Carson EW, Tompkins M. Anatomic and radiographic comparison of arthroscopic suprapectoral and open subpectoral biceps tenodesis sites. Am J Sports Med. 2013;41:2919–2924. doi: 10.1177/0363546513503812. [DOI] [PubMed] [Google Scholar]
- 13.Grimes DA, Hubacher D, Nanda K, Schulz KF, Moher D, Altman DG. The good clinical practice guideline: A bronze standard for clinical research. Lancet. 2005;366:172–174. doi: 10.1016/S0140-6736(05)66875-4. [DOI] [PubMed] [Google Scholar]
- 14.Mazzocca AD, Rios CG, Romeo AA, Arciero RA. Subpectoral biceps tenodesis with interference screw fixation. Arthroscopy. 2005;21:896. doi: 10.1016/j.arthro.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 15.David TS, Schildhorn JC. Arthroscopic suprapectoral tenodesis of the long head biceps: Reproducing an anatomic length-tension relationship. Arthrosc Tech. 2012;1:e127–e132. doi: 10.1016/j.eats.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lutton DM, Gruson KI, Harrison AK, Gladstone JN, Flatow EL. Where to tenodese the biceps: Proximal or distal? Clin Orthop Relat Res. 2011;469:1050–1055. doi: 10.1007/s11999-010-1691-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tahal DS, Katthagen JC, Vap AR, Horan MP, Millett PJ. Subpectoral biceps tenodesis for tenosynovitis of the long head of the biceps in active patients younger than 45 years old. Arthroscopy. 2017;33:1124–1130. doi: 10.1016/j.arthro.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 18.Baggio M, Martinelli F, Netto MB, Martins RO, da Cunha RC, Stipp WN. Evaluation of the results from arthroscopic tenodesis of the long head of the biceps brachii on the tendon of the subscapularis muscle. Rev Bras Ortop. 2016;51:157–162. doi: 10.1016/j.rbo.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hwang JT, Yang CJ, Noh KC, Yoo YS, Hyun YS, Lee YB, Liu X. Which is better for arthroscopic tenodesis of the long head of the biceps: Soft tissue or bony interference fixation? Arthroscopy. 2016;32:560–567. doi: 10.1016/j.arthro.2015.10.024. [DOI] [PubMed] [Google Scholar]
- 20.Chiang FL, Hong CK, Chang CH, Lin CL, Jou IM, Su WR. Biomechanical comparison of all-suture anchor fixation and interference screw technique for subpectoral biceps tenodesis. Arthroscopy. 2016;32:1247–1252. doi: 10.1016/j.arthro.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 21.Gombera MM, Kahlenberg CA, Nair R, Saltzman MD, Terry MA. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med. 2015;43:1077–1083. doi: 10.1177/0363546515570024. [DOI] [PubMed] [Google Scholar]
- 22.Rhee PC, Spinner RJ, Bishop AT, Shin AY. Iatrogenic brachial plexus injuries associated with open subpectoral biceps tenodesis: A report of 4 cases. Am J Sports Med. 2013;41:2048–2053. doi: 10.1177/0363546513495646. [DOI] [PubMed] [Google Scholar]
- 23.McCormick F, Nwachukwu BU, Solomon D, Dewing C, Golijanin P, Gross DJ, Provencher MT. The efficacy of biceps tenodesis in the treatment of failed superior labral anterior posterior repairs. Am J Sports Med. 2014;42:820–825. doi: 10.1177/0363546513520122. [DOI] [PubMed] [Google Scholar]
- 24.Ma H, Van Heest A, Glisson C, Patel S. Musculocutaneous nerve entrapment: An unusual complication after biceps tenodesis. Am J Sports Med. 2009;37:2467–2469. doi: 10.1177/0363546509337406. [DOI] [PubMed] [Google Scholar]
- 25.Sethi PM, Vadasdi K, Greene RT, Vitale MA, Duong M, Miller SR. Safety of open suprapectoral and subpectoral biceps tenodesis: An anatomic assessment of risk for neurologic injury. J Shoulder Elbow Surg. 2015;24:138–142. doi: 10.1016/j.jse.2014.06.038. [DOI] [PubMed] [Google Scholar]
- 26.Gilmer BB, DeMers AM, Guerrero D, Reid JB, III, Lubowitz JH, Guttmann D. Arthroscopic versus open comparison of long head of biceps tendon visualization and pathology in patients requiring tenodesis. Arthroscopy. 2015;31:29–34. doi: 10.1016/j.arthro.2014.07.025. [DOI] [PubMed] [Google Scholar]
- 27.Euler SA, Horan MP, Ellman MB, Greenspoon JA, Millett PJ. Chronic rupture of the long head of the biceps tendon: Comparison of 2-year results following primary versus revision open subpectoral biceps tenodesis. Arch Orthop Trauma Surg. 2016;136:657–663. doi: 10.1007/s00402-015-2393-5. [DOI] [PubMed] [Google Scholar]
- 28.Kolz CW, Suter T, Henninger HB. Regional mechanical properties of the long head of the biceps tendon. Clin Biomech (Bristol, Avon) 2015;30:940–945. doi: 10.1016/j.clinbiomech.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 29.Yi Y, Lee JM, Kwon SH, Kim JW. Arthroscopic proximal versus open subpectoral biceps tenodesis with arthroscopy repair of small- or medium-sized rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2016;24:3772–3778. doi: 10.1007/s00167-015-3641-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to statutory provisions regarding data and privacy protection but are available from the corresponding author on reasonable request.