Abstract
Purpose:
Human papillomavirus (HPV) vaccine series completion rates among females and males remain low in Florida (46.4% and 34.5%, respectively). Multiple stakeholders influence vaccination uptake, including health care providers (HCPs), public health professionals (PHPs), and members of professional organizations. We examined stakeholder efforts related to increasing vaccine uptake and education among parents/adolescents and HCPs.
Methods:
We conducted an environmental scan of stakeholder efforts and identified stakeholders using our professional networks and a snowball sampling approach. Stakeholders (n = 46) completed a survey about involvement in and barriers to vaccination promotion efforts. A subset (n = 12) of stakeholders participated in follow-up interviews further exploring vaccination efforts and barriers. Survey data were analyzed using descriptive statistics. Interview data were analyzed using deductive analysis and coded using constructs from the PRECEDE-PROCEED model.
Results:
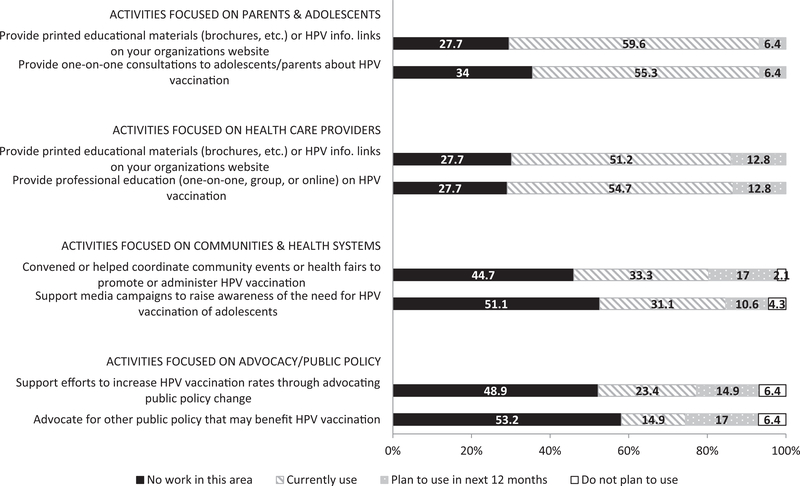
The majority of our survey sample was PHPs (50.0%) and HCPs (32.6%). Stakeholder efforts were focused on adolescent/parent/HCP education including providing: educational materials for HCPs (55.8%) and adolescents/parents (59.6%), one-on-one consultations for adolescents/parents (55.3%), and HCP education (54.7%). Lack of knowledge/understanding and education/information were barriers reported across almost all groups/areas. Office staff/HCP education and distribution of patient education materials were efforts described as important during qualitative interviews. Stakeholders also noted HCP discomfort when recommending HPV vaccine, parental perceptions that the vaccine is unnecessary, and a lack of education/understanding among parents and HCPs.
Conclusions:
Results suggest the need for parent/adolescent education, specifically targeting key areas we identified: importance and benefits of HPV vaccine, and education and skill building in vaccine communication for HCPs.
Keywords: Human papillomavirus, Vaccination, Cancer, Education, PRECEDE PROCEED model
1. Introduction
Despite evidence of effectiveness and recommendations for routine use [1], human papillomavirus (HPV) vaccination rates are low in both the US and Florida. Nationally, the most recent estimates from 2016 indicate that about 49.5% of females and 37.5% of males ages 13–17 completed the three-dose HPV vaccine series [2]. Coverage among Florida’s adolescents is similarly low, with 46.4% of females and 34.5% of males completing the series [2]. With the recent change to a two-dose series for younger adolescents, 2016 rates indicate a slight increase in completion rates both nationally and in Florida. However, without additional efforts to improve HPV vaccine coverage, many adolescents will be left vulnerable to HPV infection and related cancers.
To address suboptimal rates of HPV vaccination, the National Cancer Institute (NCI) provided a one-year supplement to 18 NCI-designated cancer centers in 2014–2015. The short-term goals were to conduct an environmental scan and develop/enhance linkages with existing coalitions and programs, with a focus on increasing HPV vaccination uptake in pediatric care settings.
Several stakeholder groups impact HPV vaccination uptake, such as health care providers (HCPs; e.g., physicians, nurses), parents [3], adolescents, professional and advocacy organizations, and department of health professionals [4]. Physicians, can facilitate vaccination uptake by providing: education for parents and adolescents about HPV [3], counterarguments to inaccurate information parents see in media [5,6], a strong recommendation and personal endorsement of the vaccine [7,8], yet, they often fail to do so [6,8–12].
Previous studies have examined barriers to HPV vaccination initiation and completion among providers and parents [6,8,9]; however, few have examined efforts related to increasing HPV vaccination rates, education, and understanding about HPV infection from the stakeholder perspective, specifically in Florida. This study is guided by portions of the PRECEDE-PROCEED model [13], which is used to assess and understand a community’s health needs and inform intervention development. PRECEDE offers a framework for assessing social, epidemiological, behavioral, environmental, educational, and ecological factors that contribute to the defined health problem (e.g., low vaccination rates). The PROCEED component involves testing and evaluating the health intervention that is developed [13]. Key components in this model that assisted in explaining current study findings consisted of: (1) predisposing factors (i.e., beliefs one has about vaccination), (2) enabling factors (i.e., facilitators influencing vaccination uptake) and (3) disabling factors (i.e., barriers hindering vaccination uptake and education). Specifically, we aimed to better understand efforts among community stakeholders (HCPs and community advocates) to increase HPV vaccination rates and educate those directly involved in vaccination decisions (HCPs and parents).
2. Methods
2.1. Utilization of PRECEDE-PROCEED
The PRECEDE-PROCEED model was utilized in multiple facets of our project. Prior to development of interview guides and assessment survey and data collection, the epidemiological assessment phase involved reviewing national and statewide adolescent immunization rates in order to better understand community needs. Our semi-structured interview guides for each stakeholder group and our assessment survey included items which assessed several PRECEDE constructs from the educational and ecological phase of the model such as predisposing, enabling, and reinforcing factors. Additionally, in our interview guides and assessment survey, we assessed administrative and policy issues related to vaccination.
We conducted our environmental scan August 2015-April 2016, where we assessed current vaccination efforts and barriers surrounding HPV vaccine series initiation and completion. Data collection consisted of an assessment survey followed by semi-structured phone interviews with a subgroup of participants.
2.2. Recruitment
We define stakeholders as individuals who influence HPV vaccine initiation and completion rates in Florida and included: HCPs, public health professionals (PHPs), professional organization members, and parents. We utilized multiple recruitment strategies, including snowball sampling, to obtain stakeholder participants from across the state that represented key stakeholder groups.
After obtaining IRB approval, recruitment began with attendees of a meeting at Moffitt Cancer Center (MCC) comprised of community-based advocacy organization members and health care organizations. We asked attendees to recommend additional individuals who may be interested in participating in our study. We then contacted those additional individuals via email and informed them we were interested in hearing more about their work surrounding HPV vaccination uptake. Additionally, we asked for recommendations for individuals who were engaging in similar work.
Additional stakeholders were recruited through a community advocacy event and a conference focused on HPV vaccination education and uptake. Individuals who attended either event were informed of the opportunity to complete our assessment survey. Participants were compensated with a $5 retail store gift card upon assessment survey completion.
2.3. Assessment survey
Stakeholders completed a 41-item survey adapted from a survey developed by the American Cancer Society’s National HPV Vaccination Roundtable that has been used previously to examine stakeholder activities focused on HPV vaccination [14]. Stakeholders were asked about their involvement in specific HPV vaccination efforts and perceived barriers to vaccination efforts in four specific groups/areas: (1) adolescents (ages 11–18) and their parents, (2) HCPs, (3) communities/health systems, and (4) advocacy/public policy (e.g., advocacy efforts throughout communities to improve public perception of vaccination, policies by payers/health care systems to cover vaccine associated costs). We chose the final items in our survey through careful review and discussion with our study team which included members with expertise in survey design, community engaged research, and HPV vaccination. Our ultimate project goal was to understand the activities stakeholders (DOH professionals, physicians, nurses, etc.) are engaged in to improve education and HPV vaccination rates in their respective counties. We aimed to select items that would best inform activities that could then be implemented into future multilevel interventions.
Items assessing stakeholder engagement in vaccination efforts focused on efforts related to education for: parents/adolescents, HCPs, communities/health systems, and public policy (e.g., do you provide printed educational materials or HPV informational links on your organizations website?). We asked stakeholders about additional efforts focused on activities related to HPV vaccine dissemination (e.g., do you provide free/reduced cost HPV vaccination?). Response options for these items included: have never engaged in this activity, plan to engage in this activity in the next 12 months, currently engaging in this activity, and do not plan to engage in this activity in the next 12 months.
Perceived barriers to HPV vaccination were assessed using items from previous studies of HCPs [15,16]. Stakeholders were asked about barriers to implementing HPV vaccination efforts they previously indicated. Barriers were assessed for each group/area (i.e., parents/adolescents, HCPs). HCPs were asked additional questions regarding specific administrative and logistical barriers, as well as provider-specific barriers. Stakeholders were asked to report the frequency of experiencing each barrier. Response options used qualitative descriptors coupled with quantitative anchors: never (0%), rarely (1–25%), sometimes (26–50%), often (51–75%), always (>75%).
Basic demographic information was collected such as county, organization, occupation, and the primary role in which they address vaccination. Finally, stakeholders were asked to indicate their willingness to participate in a follow-up phone interview with our study team. This allowed us to further explore personal and contextual factors regarding vaccination efforts and the barriers they have experienced [17].
2.4. Phone interviews
Stakeholder interview guides consisted of 11 open-ended questions and several probes. Interview guides for HCPs, professional organization members, and PHPs were adapted from an existing set of interview guides developed by Vanderbilt University. The interview guide for parents/community members was developed by our study team at MCC and questions were designed based on results from previous studies, [8] where HCPs reported common parental barriers, overall barriers to vaccination uptake and completion, and patient-level behaviors (i.e., how they recommend HPV vaccination, communication with patient/parent). The interviewers also referenced a summary of assessment survey responses specific to the interview participant, which helped facilitate discussion and served as a prompt for stakeholders in recalling their assessment survey responses. Interviews lasted 20–45 min, were audio recorded, transcribed verbatim, and verified by a study team member.
2.5. Quantitative analysis
Frequencies of vaccination efforts and barriers were calculated. We report only the activities stakeholders are currently engaging in and barriers they indicated experiencing ‘often’ (51–75% of the time) or ‘always’ (>75% of the time). Additionally, only those stakeholders who reported engaging in specific vaccination efforts and experienced specific barriers when engaging in these activities provided responses, therefore sample sizes differ across vaccination efforts and barriers.
2.6. Qualitative analysis
One of two study team members conducted the interviews (NRS & PL), while another team member took notes and operated the digital audio recorders (PL & BA). Interviews were analyzed using deductive content analysis [6,18] using MAXQDA v. 12. Transcripts were read independently by two team members (MLK & PL) and coded using a framework adapted from the PRECEDE-PROCEED model [13]. Team members met after coding every 3–4 transcripts to discuss emerging subcategories and areas of disagreement. Any areas of disagreement between coders were discussed to reach consensus.
3. Results
3.1. Sample
The survey sample was comprised of 47 stakeholders. The greatest proportion of stakeholders represented state (22.3%) or local health departments (20.6%). They reported various occupations, including PHPs (50%) and HCPs (32.6%). Participants represented several Florida counties, however the majority of participants represented Pasco County (11%) and Hillsborough County (9%). Responses were not mutually exclusive, such that stakeholders could select multiple organizations and occupations, if they acted in multiple roles.
The interview sample (n = 12) was comprised of a subset of stakeholder survey participants and represented various different occupations. The majority of interview participants were HCPs (41.6%) and PHPs (25%), while the remaining participants were either parents/advocates/volunteers (16.6%) or members of a community organization such as the American Cancer Society or the Women and Girls Cancer Alliance (16.6%). For a full survey and interview sample description, see Table 1.
Table 1.
Stakeholder survey and interview participant characteristics (n = 47).
| Stakeholder characteristics | Survey participants (n = 47) n (%) |
Interview participants (n = 12) n (%) |
|---|---|---|
| Occupation | ||
| Public health professionala | 23 (48.9) | 3 (25.0) |
| Health care providerb | 15 (31.9) | 5 (41.6) |
| Advocate/Volunteer/Parent | 4 (8.5) | 2 (16.6) |
| Member of a community organization | 3 (6.4) | 2 (16.6) |
| Student/Intern | 3 (6.4) | 0 (0.0) |
| Primary Role (in which stakeholders address HPV vaccination) | ||
| Public health professionala | 19 (40.4) | 3 (25.0) |
| Parent | 7 (14.9) | 2 (16.6) |
| Health care providerb | 9 (19.1) | 5 (41.6) |
| Leader of a professional organizationc | 3 (6.4) | 0 (0.0) |
| Member of a professional organizationc | 3 (6.4) | 0 (0.0) |
| Member of an advocacy/community organizationd | 3 (6.4) | 2 (16.6) |
| Other | 2 (4.3) | 0 (0.0) |
| County | ||
| Pasco | 5 (10.6) | – |
| Hillsborough | 4 (8.5) | – |
| Pinellas | 3 (6.4) | – |
| Leon | 2 (4.3) | – |
| Clay | 1 (2.1) | – |
| Palm Beach | 1 (2.1) | – |
| Miami-Dade | 1 (2.1) | – |
| Collier | 1 (2.1) | – |
| Orange | 1 (2.1) | – |
| Leon | 1 (2.1) | – |
| Gadsen | 1 (2.1) | – |
| Alachua | 1 (2.1) | – |
| Charlotte | 1 (2.1) | – |
| Lake | 1 (2.1) | – |
| Seminole | 1 (2.1) | – |
| Lee | 1 (2.1) | – |
County information was only provided by 26 stakeholders and was only assessed during survey.
Public health professionals include quality improvement, disease control program manager, and interventions specialist.
Health care providers include physicians and nurses.
Professional organizations include the American Academy of Pediatrics.
Advocacy/community organizations include the American Cancer Society and the Women and Girls Cancer Alliance.
3.2. Assessment survey: Current efforts and barriers to vaccination
3.2.1. Adolescents/parents
As shown in Fig. 1, the most frequent HPV vaccination efforts focused on adolescents and parents were educational activities of providing: one-on-one consultation to adolescents and their parents on HPV vaccination (55.3%) and printed educational materials or HPV informational links on their organizations’ websites (59.6%). Stakeholders most often indicated barriers such as: a lack of knowledge among families that the vaccine is a three-dose series (often/always: 31.9%) and a lack of education/understanding about HPV infection including its link to cancer (often/always: 44.7%). For a full description of additional common barriers indicated by all stakeholder groups, see Table 2.
Fig. 1.
Assessment survey results: Most common vaccination efforts among stakeholders (n = 47).
Table 2.
Most common perceived barriers among stakeholders (n = 47).
| Activities focused on | Often (51–75%) n (%) |
Always (>75%) n (%) |
|---|---|---|
| Parents & adolescents | ||
| Lack of knowledge among families that vaccine is a series of 3 shots | 13 (27.7) | 2 (4.3) |
| Lack of education/understanding about HPV and its link to cancer | 18 (38.3) | 3 (6.4) |
| Health care providers | ||
| Concerns about adding another vaccine to the vaccine schedule | 6 (12.8) | 0 (0.0) |
| Concerns about up-front cost of purchasing private stock HPV vaccine | 5 (10.6) | 1 (2.1) |
| Communities & health systems | ||
| Lack of education/understanding about HPV infection including its link to cancer | 5 (10.6) | 2 (4.3) |
| Lack of information about HPV vaccine | 6 (12.8) | 1 (2.1) |
| Lack of knowledge among families that vaccine is a series of 3 shots | 6 (12.8) | 1 (2.1) |
| Advocacy & public policy | ||
| Lack of information about HPV vaccine | 3 (6.4) | 1 (2.1) |
n values represent those who indicated engaging in the relevant HPV-related activities and experienced barriers related to these activities.
n values differ between and within each group.
3.2.2. Healthcare providers
Stakeholders reported primarily education-related efforts focused on HCPs included providing: HCP-targeted printed educational materials or HPV informational links on their organization’s website (51.2%) and professional education (e.g., one-on-one, group, online) on HPV vaccination (48.9%). Common barriers were logistical and administrative and included concerns about: adding another vaccine to the vaccine schedule (often: 12.8%) and up-front costs of purchasing private stock HPV vaccine (often/ always: 12.8%).
3.2.3. Communities/health systems
The majority of efforts focused on communities/health systems included: convening or coordinating events or health fairs to promote/administer HPV vaccine (33.3%) and supporting media campaigns to raise awareness of the need for HPV vaccination of adolescents (31.1%). The most frequently reported barriers included a lack of: education/understanding about HPV infection including its link to cancer (often/always: 14.9%), information about the HPV vaccine (often/always: 14.8%), and knowledge among families that the vaccine is a series of three shots (often/ always: 14.9%).
3.2.4. Advocacy/public policy
Common advocacy/public policy activities related to HPV vaccination included: supporting efforts to increase HPV vaccination rates through advocating public policy change (23.4%) and advocating for other public policy that may benefit HPV vaccination (14.9%). The most commonly reported barrier for this area was a lack of information about HPV vaccine (8.5%).
3.3. Qualitative findings
Main themes fell into three broad categories: enabling, disabling, and predisposing factors. Definitions of these categories as well as exemplar quotes can be found in Table 3. Within each of these three categories, different factors emerged for the different populations of interest including parent/adolescent, HCP, and communities/health systems. These different populations are included as sub-codes.
Table 3.
Qualitative themes and exemplar quotes (n = 12).
| Theme and definition | Stakeholder group | Exemplar quotes |
|---|---|---|
| Enabling Factors: | Parent/Adolescent | “Our MAs educate the parents prior to the patient walking into the room of every vaccine that we intend to do… And we use a bunch of industry-supplied tools for reminders like the little magnets.” (Int. #2) “[W]e educate them what these other vaccines are to make them aware how important they are. And once you do that education, you’re basically there, they want it.” (Int. #3) “I think I’d really to hear it [vaccine information] from the pediatrician as opposed to just having a brochure to read, although I do appreciate a good brochure.” (Int. #9) |
| Resources and policies that facilitate vaccination uptake and completion. | ||
| Provider | “So if there’s a way just to close system-specific CME offerings or CE offerings to systems… you can catch them you know at an all-staff meeting, or primary care specific updates or things like that where they already have it built into their schedule.” (Int. #1) “It’s my opinion that the entire staff needs to be educated, so that every single patient contact reinforces the routine of immunization and protocol.” (Int. #2) “We definitely have [conducted quality improvement initiatives]. We’ve looked at our rates. And we actually do okay.” (Int. #12) |
|
| Communities/Health Systems | “We built into our EMR orderable items for first dose and for reminders for second and third dose. We opened up our schedule six months out, so that second and third doses were scheduled at the time of the administration of first dose.” (Int. #2) “The other thing, I think this is what my thought I had earlier is that, legislatively, the states that you see that it’s required for school, they do better.” (Int. #3) “I think definitely a mass media campaign is a great place to start because that will at least get people talking about it.” (Int. #10) |
|
| Disabling Factors: | Parent/Adolescent | “I think it’s more that they’re thinking that their 11- and 12 year-olds are going to be having sex soon. You know, it’s that fear of, it’s too young, and I’m not ready to deal with this at that age, and why can’t they wait until later.” (Int. #3) “Sometimes, the kids can say I don’t want it and the parent will just follow. That’s kind of a common theme.” (Int. #6) “I also think that there’s a very, very limited understanding of why boys need to be vaccinated.” (Int. #9) |
| Policies, beliefs, and barriers in place that would discourage vaccine uptake and completion. | ||
| Provider | “…they go along with the parents, because the parents think that’s too much. So instead of them actually being the ones educating the parents on the safety of the vaccine, they go along with the parents.” (Int. #3) “I think some of the pediatricians are not educated themselves outside of the practice, that about the benefit, the incredible benefit of HPV vaccination.” (Int. #4) “I think time is not necessarily that there’s truly not enough time. I think it’s that it doesn’t seem to be a priority if they come in either for other health issues.” (Int. #5) “I think some of them focus more on the mandated as opposed to recommended [vaccines].” (Int. #7) |
|
| Communities/Health Systems | “[I]t’s those patients ages 18 to 26, either when they’re not covered by the Kids’ Shots program anymore, once they get their own jobs, they’re not on their parents’ insurance and have to self-pay for that vaccine on their own, that’s a barrier.” (Int. #1) “Leaders of that town are against vaccines.” (Int. #6) “The other barrier is actually because there’s a series of three. The continuance of it, it might be a little harder for the parent to make it there or, you know, setting up the appointments and this and the other stuff.” (Int. #8) “Well, one, it’s not required [for school]. And number two, because of the – because it was rolled out as a prevention around sexually transmitted disease, as opposed to against cancer prevention.” (Int. #11) |
|
| Predisposing Factors: | Parent/Adolescent | “I think that’s the majority when they say they don’t need that right now because they’re not (sexually) active.” (Int. #4) “And then, of course, then there’s also the anti-vaccine movement that has a social media presence and some celebrity endorsements that certainly doesn’t help either the public perception or provider responses.” (Int. #11) |
| Exogenous factors including health beliefs as well as demographic variables that influence the likelihood that a person will get vaccinated. | ||
| Provider | “So I think it’s both the provider perception or belief, their fear of engaging in that level of conversation with parents or what parents’ potential reaction is going to be.” (Int. #1) “You know, there are a few that think they know better than the ACIP, you know.” (Int. #2) “[I]t hasn’t been on many people’s radar necessarily as a top priority.” (Int. #5) |
|
| Communities/Health Systems | “Well, as an organization, I think it’s absolutely one of our national priorities. In fact, I just was listening to our National Cancer Control Director say HPV vaccination will be an organizational priority in 2016.” (Int.#5) “I mean, if they’re in there might as well get them and see if they have the shot, if they’re at the age and get it done.” (Int. #8) |
|
3.3.1. Enabling factors
Education was the most commonly mentioned enabling factor across all populations. Typically, participants mentioned printed materials to educate parents about HPV vaccination and the consequences of HPV infection would be most beneficial. Numerous stakeholders noted the importance of having educational opportunities for providers, with particular emphasis on raising provider awareness of current recommendation guidelines with the goal of increasing strong provider HPV vaccination recommendations. Several participants emphasized the need to educate all office staff, as they were identified as often being the first to discuss vaccinations with parents. During one interview, a physician participant indicated the medical assistants are the first in their office to educate parents about vaccines. Many of the participants noted electronic provider/office staff reminders were a beneficial systems-level factor for increasing vaccination uptake. At the community level, participants suggested a school entry requirement is a necessary enabling factor to increase HPV vaccination and many parents only get school-mandated vaccines.
3.3.2. Disabling factors
The primary systems-level barrier mentioned by stakeholders was a lack of integration between certain EHRs and immunization registries, leading to uncertainty about who still needs to get vaccinated. Several stakeholders also mentioned if the parents gave adolescents a voice in the vaccination decision, they usually declined due to a fear of needles or a desire not to have multiple injections at a single visit. Participants also noted many parents are resistant to vaccination due to the idea that their child may engage in sexual activity at an earlier age than what they deemed appropriate. Many providers also expressed concerns about damaging relationships with parents if they were perceived as “too pushy” in recommending the vaccine.
Several stakeholders identified lack of provider recommendation and poor communication as disabling factors. During one interview, a parent recalled taking their child to their HCP and indicated they were given a brief brochure about HPV vaccination by the HCP along with a brief oral description of what the vaccine prevents, but left the visit feeling like they still needed more information. Some stakeholders also indicated the lack of a mandate gives the perception among parents and providers that it is optional, which they believed led to weaker recommendations from providers and lower uptake among parents. Additional disabling factors mentioned included the time and out of pocket cost, particularly for older patients who no longer qualify for the Vaccines for Children (VFC) Program.
3.3.3. Predisposing factors
Stakeholders identified several predisposing factors that they believed influenced vaccine uptake. The biggest influence for parents/adolescents was the misinformation reported through the media or on social media. Many providers also noted some often feel the vaccine is unnecessary or felt vaccination was a low priority relative to other health concerns. Several providers also anticipated parental hesitancy to the vaccine, leading them to avoid the conversation about HPV vaccine to avert conflict. At the community/health systems level, many stakeholders mentioned a general anti-vaccine sentiment. Some also indicated that until recently, cervical cancer was not considered a “priority cancer site” and therefore HPV vaccination was not a focus of their cancer prevention efforts. For a full description of all sub-codes identified, see Table 3.
4. Discussion
HPV vaccination rates remain low in the US and Florida [19], thereby representing a missed opportunity to prevent several HPV-related cancers. Provider knowledge and attitudes (i.e., few perceived barriers to vaccination) can predict vaccination recommendation practices [20], which can positively impact HPV vaccination series initiation and completion rates [21]. Parents can also positively or negatively impact vaccine initiation and completion rates depending on their awareness about HPV infection [22] and their attitudes towards vaccination [23]. We aimed to understand what key stakeholders are doing in their respective counties to increase HPV vaccination rates.
Qualitative themes aligned with survey results and we were able to establish sub-codes that further elucidate the efforts in which stakeholders are engaging and the barriers they encounter in clinical practice and the community. Survey results revealed the majority of participants indicated several “enabling” factors, which were described in the survey as various educational activities for target groups (i.e., parents, adolescents). Stakeholder interview responses were partially categorized into components of the PRECEDE-PROCEED model (predisposing & enabling factors). They aligned with our survey results because the majority of our survey results were factors that could contribute to an increase in vaccination rates (the HPV-related activities stakeholders indicated engaging in). These were also mentioned during interviews and could be described as enabling factors or predisposing factors. Additionally, when completing our survey, stakeholders indicated barriers they encountered when implementing the HPV-related activities they engaged in. A theme that emerged from stakeholder interviews was “disabling factors,” which was used to describe these barriers stakeholders described.
Quantitative and qualitative results indicate that primary efforts or enabling factors to increase HPV vaccination uptake and completion consist of activities focused on parent/patient and HCP education. For parents/patients, stakeholders indicated engaging in activities such as providing one-on-one consultations about HPV vaccination for parents/patients and providing them with HPV educational materials. A high-quality physician recommendation for HPV vaccination is comprised of a strong, consistent, timely, and urgent recommendation. However, our interviews of HCPs and parents demonstrated there are inconsistencies in what is discussed during visits with HCPs and the quality of recommendation for HPV vaccination. These results partially support previous research, which indicates a lack of a high quality provider recommendation [7] and lack of parental [24,25] and provider [26] knowledge are common barriers to vaccination uptake.
Predisposing factors are beliefs that may facilitate or hinder vaccination uptake. Stakeholders indicated parents may turn to media sources to obtain medical information and advice. Research has shown parents initially hear about the vaccine from media reports, which could preemptively influence their perception of the vaccine prior to a discussion with their HCP [27]. While vaccine hesitancy among parents has been well-documented across multiple studies and can predict vaccination uptake/completion [22,25,28–31], stakeholders also felt HCPs may have preconceived notions about parental beliefs about HPV vaccination and may also experience discomfort or hesitation in having the discussion about vaccination. This hesitancy and discomfort could lead to the HCP omitting the conversation to avoid confrontation [32–34], Considering this, the HCPs’ discomfort in discussing the vaccine and a possible lack of effective communication training may play a much larger role in the conversation surrounding vaccination than previous research has accounted for. This is also consistent with the primary disabling factor uncovered in our study: provider discomfort discussing the vaccine with parents.
An additional critical disabling systems-related factor identified consisted of the lack of integration between certain EHR systems and the Florida SHOTS registry, which prevents providers from accurately identifying children due for vaccines. A common and relevant systems-related barrier previously identified is the lack of an effective EHR system to provide patient and provider reminders, thereby reducing missed clinical opportunities for series initiation and completion [35]. Ultimately, this prevents providers from maintaining a continuity of care and ensuring that patients who are newly established in their practice are up to date on recommended vaccines. Systems-focused interventions such as EMR-linked clinical decision support tools providing patient immunization history, provider and patient reminders and educational content have demonstrated effectiveness in increasing HPV vaccination rates [36].
While HCP education and the implementation of a comprehensive EHR system are independently effective ways to increase adolescent vaccination rates [37], the President’s Cancer Panel, as well as recent research demonstrate that multi-level interventions focused on education and reminder/recall systems are more effective than single-method interventions in increasing vaccine acceptance and vaccination rates [4,38]. Perceived lack of importance of the vaccine because it is not school-mandated was a unique barrier indicated by stakeholders in our study. To our knowledge, previous research has not directly assessed this as a potential barrier to vaccination uptake among Florida stakeholders. However, among providers and parents representing other states, previous research has assessed perceptions of a mandate and found that while some parents and providers are in support of it [39 40 41], there are still some who are opposed to an HPV vaccination mandate [41]. Rhode Island, Virginia, and Washington DC are the only states with a school mandate for the HPV vaccine. Yet initiation rates for Virginia are still below the national average of 60%, while Rhode Island and Washington DC rates are well above the national average with 88.9% and 79.2% of adolescents initiating the series, respectively [42]. This suggests that a school mandate for the HPV vaccine may be an effective policy-level facilitator for increasing adolescent vaccination rates. However, a mandate could cause pushback in states that adopt this policy. In previous research, among those who were opposed to a school mandate, their perceptions were driven by the belief that HPV is not transmitted casually and they doubted the safety and efficacy of the vaccine [41]. Similarly, previous research has found that parents are significantly more likely to indicate support of a vaccine mandate if they believe HPV vaccine is just as important or more important than other vaccines and believe in the effectiveness of the vaccine and its ability to prevent related cancers [43]. Additionally, in Rhode Island, where there is a mandate for school entry, 73% of girls and 68.7% of boys are up to date on their HPV vaccinations compared to 49.5% of girls and 37.5% of boys nationally [42]. Considering this, if other states did adopt a mandate, it should be accompanied by educational sessions for key stakeholders with a strong emphasis on vaccine safety, benefits, and risks of HPV infection.
One strength of our study is the examination of vaccination efforts and related barriers across multiple groups of stakeholders, all of whom possess varying levels of influence in vaccination decisions. Additionally, we believe that our focus on current activities related to increasing HPV vaccination education and uptake helped enhance recall among our stakeholder sample. To our knowledge, our study is among the first to explore stakeholder perspectives in Florida related to HPV vaccination efforts and barriers experienced when engaging in these efforts. Our study is also responsive to the National Institute of Health for HPV-focused environmental scans [44]. Through the implementation of a diverse stakeholder sample and the exploration of HPV-related activities and barriers existing at multiple levels, our environmental scan provides a multifaceted exploration of these key factors that can influence HPV vaccination. Thus, our scan adds to the growing literature focused on increasing HPV vaccination rates. This is beneficial for the development of future multi-level interventions, which could utilize findings and also engage stakeholders similar to those in our sample in intervention development and execution.
Our results should be considered in light of certain limitations. Due to recruitment methods, the participation rate for the survey portion of the study cannot be determined; however, our interview sample was comprised of about half (42.9%) of those survey participants who initially agreed to participate in an interview. With a small interview sample (n = 12), it was difficult to evaluate in-depth all of the HPV vaccination efforts survey participants indicated. However, every effort was made to obtain qualitative interviews from participants with diverse experiences. Our parent sample was comprised of individuals who were already in support of the vaccine and had some form of a personal connection to cancer and HPV infection and their responses may not be reflective of parents in the general population. Finally, our sample also did not include any individuals in public policy, whose opinions could have elucidated additional barriers. Overall, while our sample size for both the survey and interviews was relatively small and this could be perceived as a limitation, this limitation is minimized due to the fact that we were not aiming to examine the population directly affected by vaccination, but rather key stakeholders in the HPV vaccination process.
5. Conclusions
Stakeholders in Florida indicated engaging in various efforts related to increasing HPV vaccination uptake among adolescents, mainly education for physicians and parents/adolescents. However, since vaccination rates remain low and a lack of knowledge and effective provider recommendation are common barriers, future research could assess the effectiveness of HPV-related efforts we identified.
Additionally, our results suggest a need for provider communication training, which emphasizes parent/patient engagement in the discussion about vaccination, how to establish relationships, initiating the conversation about vaccination, conveying the importance of vaccination, and addressing the misconceptions associated with this vaccine.
Perhaps the most important and unique findings that our study uncovered consist of the lack of integration of a vaccination registry with EMR systems and the lack of perceived importance of the HPV vaccine due to the lack of a school mandate. These barriers further support the need for multi-level interventions that effectively address vaccination in a way that targets individuals with varying levels of importance in the decision about vaccination.
While our study utilized a statewide stakeholder sample, previous research assessing HPV vaccination barriers among samples of parents and physicians across the US has demonstrated that the barriers we uncovered are also nationwide barriers. Our environmental scan also uncovered barriers that previous research had not found, indicating that additional factors should be taken into consideration in order to develop effective multi-level interventions aiming to improve public perception/understanding of HPV vaccination, increase vaccination rates, and ultimately decrease HPV-related cancer incidence rates.
Funding sources and Acknowledgements
This project was approved by the institutional review board (protocol: #19784). This work was supported by a supplement from the National Cancer Institute (NCI) under grant number: 3P30CA076292–16S3. The efforts of Monica Kasting are supported by the National Cancer Institute of the National Institutes of Health (R25-CA090314). Dr. Kasting is additionally supported by the Center for Research in Infection and Cancer (K05-CA181320). The authors wish to thank Nazach Rodriguez for helping with this project by conducting a portion of our stakeholder interviews.
Abbreviations and acronyms:
- ACIP
advisory committee on immunization practices
- HPV
human papillomavirus
- VFC
vaccines for children program
- US
United States
- HCP
health care providers
- PHP
public health professional
- EMR
electronic medical record
- EHR
electronic health record
Footnotes
Conflicts of interest
Authors Lake, Kasting, Malo, Giuliano, and Vadaparampil have no conflicts of interest to declare related to the submitted work. The contents of this manuscript are solely the responsibility of the authors.
References
- [1].Markowitz LE, Dunne EF, Saraiya M, et al. Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2014;63(RR-05):1–30. [PubMed] [Google Scholar]
- [2].Walker T, Meyer SA. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years-United States, 2016. MMWR Morb Mort Weekly Report 2017;66(33):874–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Reiter PL, Stubbs B, Panozzo CA, Whitesell D, Brewer NT. HPV and HPV vaccine education intervention: effects on parents, healthcare staff, and school staff. Cancer Epidemiol Biomark Prev 2011;20(11):2354–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].National Cancer Institute. President’s Cancer Panel Annual Report 2012–2013-Accelerating HPV Vaccine Uptake: Urgency for action to prevent cancer. 2012; https://deainfo.nci.nih.gov/advisory/pcp/annualreports/hpv/index.htm.
- [5].Quinn GP, Murphy D, Malo TL, Christie J, Vadaparampil ST. A national survey about human papillomavirus vaccination: what we didn’t ask, but physicians wanted us to know. J Pediat Adolesc Gynecol 2012;25(4):254–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Kasting ML, Scherr CL, Ali K, Lake P, Malo TL, Johns T, Roetzheim RG, Quinn GP, Vadaparampil ST. Human papillomavirus vaccination training experience among family medicine residents and faculty. Family Med 2017;49(9):9. [PMC free article] [PubMed] [Google Scholar]
- [7].Gilkey MB, Malo TL, Shah PD, Hall ME, Brewer NT. Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomark Prev 2015;24(11):1673–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Vadaparampil ST, Malo TL, Sutton SK, et al. Missing the target for routine human papillomavirus vaccination: consistent and strong physician recommendations are lacking for 11–12 year old males. Cancer Epidemiol Prev Biomark 2016;cebp:1294.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Vadaparampil ST, Kahn JA, Salmon D, et al. Missed clinical opportunities: provider recommendations for HPV vaccination for 11–12 year old girls are limited. Vaccine 2011;29(47):8634–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Vadaparampil ST, Malo TL, Kahn JA, et al. Physicians’ human papillomavirus vaccine recommendations, 2009 and 2011. Am J Prev Med 2014;46(1):80–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sturm L, Donahue K, Kasting M, Kulkarni A, Brewer NT, Zimet GD. Original article: Pediatrician-parent conversations about human papillomavirus vaccination: an analysis of audio recordings. J Adolesc Health 2017;61:246–51. [DOI] [PubMed] [Google Scholar]
- [12].Perkins RB, Clark JA, Apte G, et al. Missed opportunities for HPV vaccination in adolescent girls: A qualitative study. Pediatrics 2014;134(3):e666–74. [DOI] [PubMed] [Google Scholar]
- [13].Green L, Kreuter M. The precede–proceed model. Health promotion planning: an educational Mountain View (CA): Mayfield Publishing Company;1999: 32–43. [Google Scholar]
- [14].Mroz S, Zhang X, Williams M, Conlon A, LoConte N. Working to increase vaccination for Human Papillomavirus: A survey of Wisconsin Stakeholders, 2015. Prev Chronic Dis 2017;14(85). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Vadaparampil ST, Staras SA, Malo TL, et al. Provider factors associated with disparities in human papillomavirus vaccination among low-income 9-to 17-year-old girls. Cancer 2013;119(3):621–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Scherr C, Augusto B, Ali K, Malo T, Vadaparampil S. Provider-reported acceptance and use of the Centers for Disease Control and Prevention messages and materials to support HPV vaccine recommendation for adolescent males. Vaccine 2016;34(35):4229–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Patton MQ. Qualitative evaluation and research methods. SAGE Publications, inc; 1990. [Google Scholar]
- [18].Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62 (1):107–15. [DOI] [PubMed] [Google Scholar]
- [19].Reagan-Steiner S National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2015. MMWR. Morb Mort Weekly Report 2016; 65. [DOI] [PubMed] [Google Scholar]
- [20].Kahn JA, Zimet GD, Bernstein DI, et al. Original article: Pediatricians’ intention to administer human papillomavirus vaccine: the role of practice characteristics, knowledge, and attitudes. J Adolesc Health 2005;37:502–10. [DOI] [PubMed] [Google Scholar]
- [21].Gerend MA, Shepherd MA, Lustria MLA, Shepherd JE. Predictors of provider recommendation for HPV vaccine among young adult men and women: findings from a cross-sectional survey. Sex Transm Infect 2016;92(2):104. [DOI] [PubMed] [Google Scholar]
- [22].Khurana S, Sipsma HL, Caskey RN. HPV vaccine acceptance among adolescent males and their parents in two suburban pediatric practices. Vaccine 2015;33 (13):1620–4. [DOI] [PubMed] [Google Scholar]
- [23].Hofman R, van Empelen P, Richardus JH, et al. Predictors of HPV vaccination uptake: a longitudinal study among parents. Health Educ Res 2014;29(1):83. [DOI] [PubMed] [Google Scholar]
- [24].Tiro JA, Meissner HI, Kobrin S. Chollette V. What Do Women in the U.S. Know about Human Papillomavirus and Cervical Cancer? Cancer Epidemiol Biomark Prev 2007;16(2):288–94. [DOI] [PubMed] [Google Scholar]
- [25].Allen JD, Othus MKD, Shelton RC, et al. Parental Decision Making about the HPV Vaccine. Cancer Epidemiol Biomark Prev 2010;19(9):2187–98. [DOI] [PubMed] [Google Scholar]
- [26].Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediat 2014;168(1):76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Etter DJZG Rickert VI. Human papillomavirus vaccine in adolescent women: A 2012 update. Curr Opin Obstet Gynecol 2012;24(5):6. [DOI] [PubMed] [Google Scholar]
- [28].McRee A-L, Gilkey MB, Dempsey AF. HPV vaccine hesitancy: Findings from a statewide survey of health care providers. J Pediat Health Care 2014;28 (6):541–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: A critical review. Soc Sci Med 2014;112:1–11. [DOI] [PubMed] [Google Scholar]
- [30].Staras SAS, Vadaparampil ST, Patel RP, Shenkman EA. Parent perceptions important for HPV vaccine initiation among low income adolescent girls. Vaccine 2014;32(46):6163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Thompson E, Rosen B, Vamos C, Kadono M, Daley E. Human papillomavirus vaccination: what are the reasons for nonvaccination among U.S. adolescents? J Adolesc Health 2017;61(3):6. [DOI] [PubMed] [Google Scholar]
- [32].McRee A, Gilkey M, Dempsey A. HPV Vaccine Hesitancy: Findings from a statewide survey of health care providers. J Pediatr Health Care. 2014;28(6):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Bynum SA, Staras SA, Malo TL, Giuliano AR, Shenkman E, Vadaparampil ST. Factors associated With Medicaid providers’ recommendation of the HPV vaccine to low-income adolescent girls. J Adolesc Health 2014;54(2):190–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].McCave E Influential factors in HPV vaccination uptake among providers in four states. J Commun Health 2010;35(6):8. [DOI] [PubMed] [Google Scholar]
- [35].Conroy K, Rosenthal SL, Zimet GD, et al. Human papillomavirus vaccine uptake, predictors of vaccination, and self-reported barriers to vaccination. J Women’s Health 2009;18(10):8. [DOI] [PubMed] [Google Scholar]
- [36].Mayne S, Karavite D, Grundmeier RW, et al. The implementation and acceptability of an HPV vaccination decision support system directed at both clinicians and families. AMIA Ann Symp Proc 2012:616–24. [PMC free article] [PubMed] [Google Scholar]
- [37].Perkins RB, Zisblatt L, Legler A, Trucks E, Hanchate A, Gorin SS. Effectiveness of a provider-focused intervention to improve HPV vaccination rates in boys and girls. Vaccine 2015;33(9):1223–9. [DOI] [PubMed] [Google Scholar]
- [38].Smulian EA, Mitchell KR, Stokley S. Interventions to increase HPV vaccination coverage: A systematic review. Hum Vaccin Immunother 2016;12 (6):1566–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Perkins RB, Pierre-Joseph N, Marquez C, Iloka S, Clark JA. Parents’ opinions of mandatory Human Papillomavirus (HPV) vaccination: does ethnicity matter? Womens Health Issues 2010;20(6):420–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Kahn JA, Cooper HP, Vadaparampil ST, et al. Human papillomavirus vaccine recommendations and agreement with mandated human papillomavirus vaccination for 11-to-12-year-old girls: a statewide survey of Texas physicians. Cancer Epidemiol Biomark Prev 2009;18(8):2325–32. [DOI] [PubMed] [Google Scholar]
- [41].Tissot AM, Zimet GD, Rosenthal SL, Bernstein D, Wetzel C, Kahn JA. Effective strategies for HPV vaccine delivery: The views of pediatricians. J Adolesc Health 2008;41(2):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Walker TY, Elam-Evans LD, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years – United States, 2016. MMWR Morb Mortal Wkly Rep 2017 2017;66(33):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Calo W, Gilkey M,sss Shah P, Moss J, Brewer N. Parents’ Support for School-Entry Requirements for Human Papillomavirsus Vaccination: A National Study. Cancer Epidemiol Biomark Prev 2016;25(9):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Wilburn A, Vanderpool R, Knight J Kentucky’s Human Papillomavirus Vaccination Project. Prev Chronic Dis: Environmental Scanning as a Public Health Tool; 2016. p. 13. [DOI] [PMC free article] [PubMed] [Google Scholar]