Abstract
Introduction
The United States has been actively involved in major armed conflicts over the last 15 years. As a result, a significant proportion of active duty service personnel and returning veterans have endured combat, putting them at risk for developing post-traumatic stress disorder (PTSD), a disabling disorder that may occur after exposure to a traumatic event. Current therapies often require long-term, time-intensive and costly commitment from the patient and have variable degrees of success. There remains an ongoing need for better therapies, including complementary medicine approaches that can effectively reduce PTSD symptoms. While anecdotal evidence suggests that routine practice of Brazilian Jiu Jitsu (BJJ) can reduce symptoms of PTSD, there have been no formal studies to address this.
Materials and Methods
This study was approved by the University of South Florida Institutional Review Board (#PRO00019430). Male US active duty service members and veterans from the Tampa area participated in a 5-month (40 sessions) BJJ training program. Before beginning and again midway through and upon completion of training the participants completed several validated self-report measures that addressed symptoms of PTSD and other co-morbid conditions. Effect size and 95% confidence intervals were determined using a within-person single-group pretest–posttest design.
Results
Study participants demonstrated clinically meaningful improvements in their PTSD symptoms as well as decreased symptoms of major depressive disorder, generalized anxiety and decreased alcohol use; effect sizes varied from 0.80 to 1.85.
Conclusions
The results from this first-of-kind pilot study suggest that including BJJ as a complementary treatment to standard therapy for PTSD may be of value. It will be necessary to validate these promising results with a larger subject cohort and a more rigorous experimental design before routinely recommending this complementary therapy.
Keywords: post traumatic stress disorder, complementary medicine, Brazilian Jiu Jitsu, alcohol use, PCL5
INTRODUCTION
Post-traumatic stress disorder (PTSD) is a disabling condition that may occur after exposure to a traumatic event, and evokes a combination of intrusion and avoidance symptoms, negative alterations in cognition and mood, and alterations in arousal and reactivity.1 There is high comorbidity (>80%2) between PTSD and other health-related conditions including major depressive disorder (MDD), generalized anxiety disorder (GAD), and substance misuse or dependence.3,4 The United States has been involved in major armed conflicts for the better part of the last 15 years, putting a significant proportion of returning personnel at risk for developing PTSD. Prevalence estimates vary dramatically depending on sampling methodology and operational definition of PTSD, but a meta-analysis suggested prevalence was between 5% and 13% depending on combat exposure.5 Current guidelines for treating PTSD recommend trauma-focused psychological interventions that are designed to minimize the intrusion, avoidance, and hyper-arousal symptoms by some combination of re-experiencing and working through trauma-related memories.6 The most frequent of these include Prolonged Exposure (PE) therapy, Cognitive Processing Therapy (CPT), and Eye Movement Desensitization and Reprocessing (EMDR). These are generally time-intensive therapies and complete restoration of mental health is not a guarantee. Further, not all sufferers seek help with conventional treatments because of the stigma of mental health disorders. Together, these issues have led to the development and/or consideration of complementary and alternative medicine strategies to potentially manage PTSD.
One such adjunct is Brazilian Jiu Jitsu (BJJ), a martial art and self-defense system that focuses on grappling and ground fighting. There are numerous anecdotal reports espousing the purported effectiveness of BJJ, but no systematic studies have been performed. Studies of other martial arts such as Judo, Tai Chi, and Qigong suggest that these practices enhance mood state, reduce fatigue and promote psychological well-being.7–10 Within the context of females with military sexual trauma, self-defense training has been associated with significant reductions in behavioral avoidance, PTSD hyper arousal, and depression, with significant increases in interpersonal activity, and self-defense self-efficacy.11 The authors of this latter study argued that the self-defense curriculum provided an enhanced exposure therapy experience and therefore may be a valuable complementary tool to standard PTSD treatment. For these reasons, we undertook this small study to investigate proof-of-concept for the potential therapeutic efficacy of BJJ in reducing PTSD symptoms, as well as symptoms of related comorbidities.
METHODS
Participants
Armed service personnel and veterans from the greater Tampa area participated in this study. All study participants provided written informed consent prior to screening. The inclusion criteria for participation were: (i) Male, ages 18 years or older; (ii) US service member or veteran with prior combat-related deployment(s); (iii) current evidence of significant symptoms of PTSD as determined by the PTSD Checklist (PCL-5) and Psychiatric Diagnostic Screening Questionnaire (PDSQ) and a clinical interview; (iv) no suicidal/homicidal ideation or intent, and no evidence of psychotic behavior or being in psychological crisis; and (v) the ability to read and speak English. An official diagnosis of PTSD was not required for enrollment nor was time since onset determined. The exclusion criteria were: (i) previous training in BJJ during the past 6 months; (ii) major psychiatric disorder uncontrolled and likely to interfere with participation in the BJJ program (as determined by clinician assessment); (iii) current substance abuse dependence treatment anticipated to interfere with program participation; (iv) brain injury prohibiting speech, writing, and purposeful actions or positive screen for TBI expected to impact participation in the BJJ program. Contraindications to physical activity were also assessed using the Physical Activity Readiness Questionnaire (PAR-Q12). Based on these criteria, 29 male US active duty service members and veterans, from 22 to 60 years of age (average 34.5 ± 13.1 years), were screened for participation in this study, 23 were enrolled, but only 9 (39.1%) completed the full 5-month (40 session) BJJ training program. Reasons for withdrawal included deployment, relocation, work issues, transportation issues, and unspecified. In all cases, participant dropout occurred prior to the study midpoint. General demographic characteristics, military history and scores on the PCL-5 and PDSQ PTSD subscale of all enrolled subjects are presented in Supplementary Tables 1–3.
Procedure
This was a prospective cohort study with the objective of estimating the effect size of BJJ training in reducing mental health symptoms among US service members or veterans with current symptoms of combat-related PTSD. After recruitment and screening, psychological health status of study participants was assessed using a battery of validated self-report measures pre-, mid- and post-intervention. Participants were compensated with a $25 gift card each time they completed the self-report questionnaires (maximum $75). The intervention was training in BJJ twice weekly (70 minute classes) for 5 months (40 sessions). The length of intervention was determined based on previous studies examining the effect of Tai Chi on psychological well-being.7,9,10 The BJJ training regimen was administered at an appropriate training level by a qualified BJJ instructor at Tampa Jiu Jitsu, LLC and included the following components: standing and ground self-defense moves, concepts of positive Jiu Jitsu behavior, safe interaction with other students, appropriate conflict resolution, and a positive Jiu Jitsu lifestyle. The first ten classes served as a trial period to identify any participants who may have insufficient ability to obey all safety protocols put in place, obey instructor commands, self-calm with verbal cues from the instructor, and not make threatening or dangerous comments to other students or oneself. The study was approved by the University of South Florida Institutional Review Board (#PRO00019430).
Measures
The primary outcome measures for this study included the PCL-5 and PDSQ. The PCL-5 Checklist is a self-administered scale that identifies key symptoms of PTSD; it has been validated against the Clinician Administered PTSD Scale for DSM-513 and is considered reliable in the assessment of PTSD. The PDSQ provides a global assessment of psychopathology14,15 and subscale scores measuring symptoms of 13 psychological disorders, including (but not limited to) PTSD, major depressive disorder (MDD), generalized anxiety disorder (GAD), and alcohol abuse/dependence (AAD).
The secondary outcome measures included the Brief Symptom Inventory (BSI);16 the Post-traumatic Growth Inventory Short-Form (PTGI);17 the Centers for Epidemiological Studies Depression Scale (CES-D);18,19 Pittsburgh Sleep Quality Index (PSQI);20 Alcohol Use Disorder Identification Test (AUDIT)21,22 and Pain Outcomes Questionnaire (POC).23 Instruments were chosen for evaluation of multiple symptoms known to be associated with PTSD. These outcome measures were obtained prior to intervention, at the midpoint of BJJ training and then again at completion of training.
Data Analysis
Demographics, military history, and clinical history variables are presented as means and standard deviations for continuous variables, or percentages for categorical variables. To determine if there were meaningful differences between the subjects who withdrew versus completed the study, we performed analysis of variance (ANOVA) for continuous variables and Chi-square tests for categorical variables (Supplementary Tables 1–3). Subsequent analyses were only performed on subjects who completed the study. This included calculation of Cohen’s measure of effect size (d) and 95% confidence intervals (CI) using the within-person single-group pretest–posttest design as described previously.24 This method provides an uncontrolled comparison of symptomatology before and after enrollment in the BJJ program. Similarly, mean symptom scores on measures of PTSD and related comorbidities were evaluated by use of paired t-tests and repeated measures mixed models. This included assessment of symptom changes from pre-intervention to the mid-point, pre-intervention to end of the training program, mid-intervention to end of the training program, and assessment of linear trend over all three time assessments. For consistency, all effect sizes that represent an improvement on the measure of interest (Table I) are reported with positive numbers. All measures used were evaluated for internal consistency reliability using Cronbach’s α.
TABLE I.
Effect Size of BJJ Training on Psychological Outcome Measures (n = 9)
| Outcome Measure | Effect Pre to Mid | Effect Pre to Post | Effect Mid to Post | p-Trend† | |||
|---|---|---|---|---|---|---|---|
| d | CI | d | CI | d | CI | ||
| PCL-5 (PTSD) | 1.03* | 0.14, 1.92 | 1.49** | 0.46, 2.53 | 0.23 | −0.37, 0.84 | 0.002 |
| PDSQ Subscales: | |||||||
| Total score | 1.58** | 0.61, 2.55 | 1.85*** | 0.77, 2.94 | 0.46 | −0.08, 0.99 | 0.0009 |
| PTSD | 1.69** | 0.63, 2.75 | 1.57** | 0.57, 2.57 | 0.0 | −0.70, 0.70 | 0.0008 |
| Major depressive disorder | 1.04* | 0.28, 1.81 | 1.30** | 0.47, 2.12 | 0.10 | −0.14. 0.34 | 0.009 |
| Alcohol abuse/dependence | 1.17** | 0.54, 1.79 | 0.90* | 0.01, 1.79 | 0.21 | −0.54, 0.95 | 0.005 |
| Generalized anxiety disorder | 1.21* | 0.35, 2.06 | 0.90* | 0.14, 1.67 | 0.03 | −1.02, 1.07 | 0.004 |
| AUDIT | 0.24 | −0.30, 0.77 | 0.76 | −0.09, 1.62 | 0.71 | 0.18, 1.24 | 0.03 |
d: Effect size; positive values reflect symptom improvement. CI: 95% confidence interval. PDSQ: Psychiatric Diagnostic Screening Questionnaire. AUDIT: Alcohol Use Disorder Identification Test scale. *Paired t-tests: p < 0.05; **p < 0.01; ***p < 0.001. †Based on repeated measures mixed model. One of the nine subjects had missing data on some measures at one outcome assessment interval.
RESULTS
Primary Outcome Measures
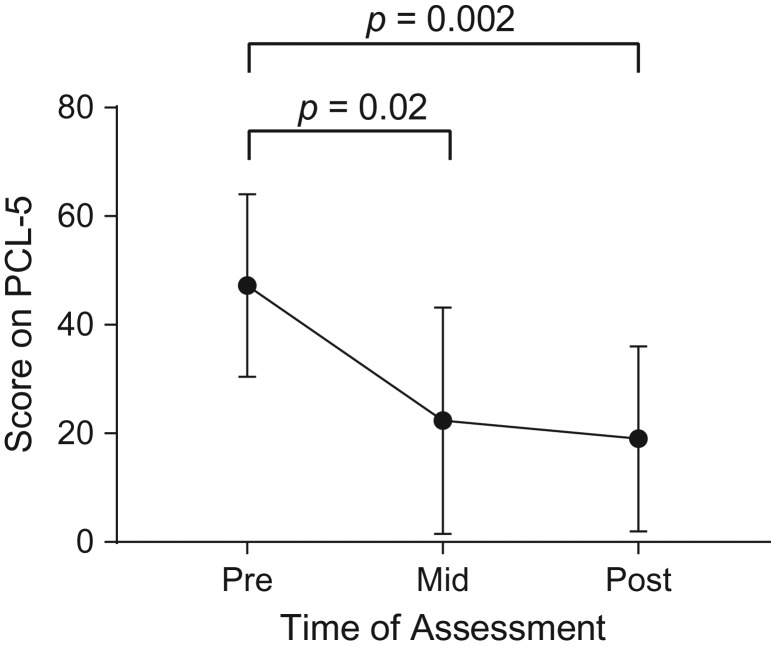
Over the course of 5 months (40 sessions) of BJJ training, scores on the PCL-5 (PTSD checklist) decreased significantly from a baseline of 47.2 ± 16.8 to 25.1 ± 20.4 after 2.5 months (p = 0.02), and 19.0 ± 17.0 (p = 0.002) after 5 months (Table I, Fig. 1). The effect size on the PCL-5 from pre-intervention to post-intervention was large (d = 1.49, CI [0.46, 2.53]). Internal consistency, as determined by Cronbach’s α, was high (0.968). Similar results were obtained on the PDSQ PTSD subscale (d = 1.57, CI [0.57, 2.57]; Cronbach’s α = 0.890) (Table I, Fig. 2B).
FIGURE 1.
Plot of mean scores on the PCL-5 (PTSD Checklist) pre-intervention, mid-intervention, and post-intervention. The filled circles represent the mean scores; vertical lines represent plus and minus one standard deviation.
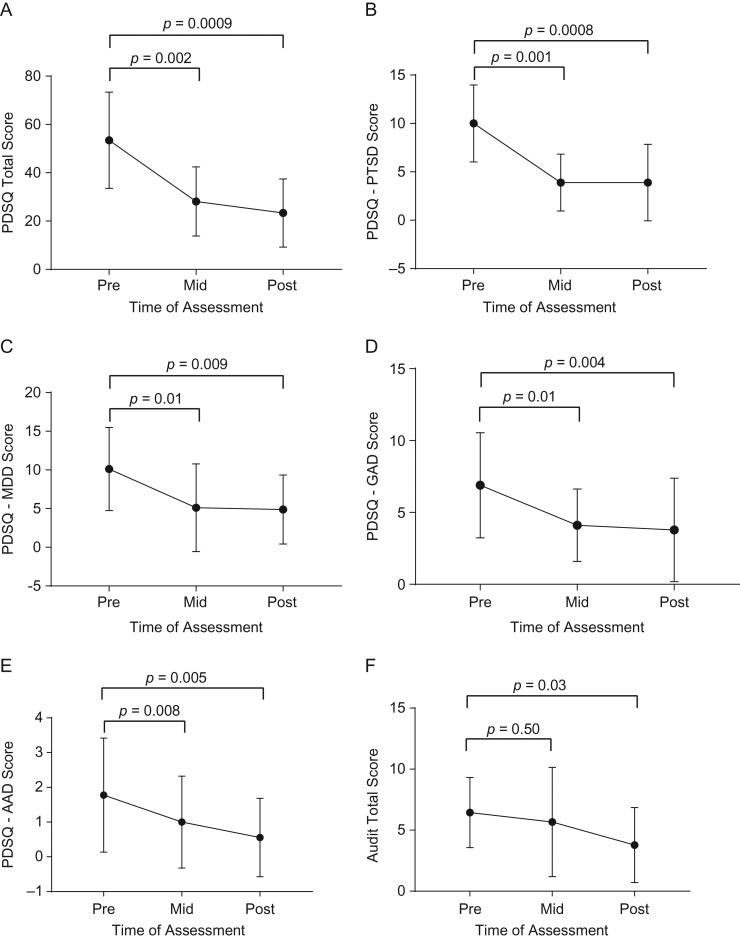
FIGURE 2.
Plot of mean total and subscale scores from the Psychiatric Diagnostic Screening Questionnaire (2A, Total; 2B, PTSD; 2C, MDD; and 2D, GAD; 2E, AAD; and 2F, Audit) pre-intervention, mid-intervention, and post-intervention. The filled circles represent the mean scores; vertical lines represent plus and minus one standard deviation. PDSQ: Psychiatric Diagnostic Screening Questionnaire. PTSD: post-traumatic stress disorder. MDD: major depressive disorder. GAD: generalized anxiety disorder. AAD: alcohol abuse disorder. AUDIT: alcohol use disorder identification test.
Secondary Outcome Measures.
In addition to measures of PTSD, we also examined other measures of mental health. The total score on the PDSQ is a measure of global psychopathology (Cronbach’s α = 0.965). Mean scores on this instrument decreased from 53.4 ± 19.9 prior to BJJ training to 28.1 ± 14.3 at the mid-point assessment and to 23.3 ± 14.1 by the end of the study (Table I, Fig. 2A). The effect sizes at 2.5 months (d = 1.58, CI [0.61, 2.55]) and 5 months (d = 1.85, CI [0.77, 2.94]) were both very large. In addition to global psychopathology score, subjects scored better at 5 months on PDSQ subscales that measured MDD (d = 1.30, CI [0.47, 2.12], p = 0.009, Cronbach’s α = 0.869; Table I, Fig. 2C); GAD (d = 0.90, CI [0.14, 1.67], p = 0.004, Cronbach’s α = 0.831; Table I, Fig. 2D); and AAD d = 0.90 (CI [0.01, 1.79], p = 0.005, Cronbach’s α = 0.635; Table I, Fig. 2E). Consistent with the results on the AAD subscale, mean scores at baseline, 2.5 months, and 5 months on the AUDIT scale were 6.4 ± 2.9, 5.7 ± 4.5, and 3.8 ± 3.1, respectively. This resulted in a pre- to post-intervention effect size of d = 0.76 (CI [−0.09, 1.63], Cronbach’s α = 0.768, p = 0.03) (Table I, Fig. 2f). The complete results obtained on all scales are presented in Supplementary Tables 4 and 5.
DISCUSSION
The goal of this study was to estimate the effect size of BJJ training on reduction of PTSD symptoms and symptoms of related comorbidities in a population of retired or active duty service personnel who had been combat-deployed. We observed significant improvements in symptomology on scales that specifically assessed PTSD symptoms, as well as measures of major depression, generalized anxiety disorder, and alcohol use.
One potential explanation for the observed benefits of BJJ training may be the physical exercise component of training. However, in a systematic review of the literature on exercise as a treatment for PTSD in non-veterans, results appeared promising, but not definitive.25 In the 35 years covered by this review, only 13 studies met the inclusion criteria for analysis, but none of these studies was a randomized controlled trial. Similar conclusions have been reached by other authors.26,27
Another potential explanation is that BJJ can be viewed as a problem solving opportunity for the practitioner that may instill a resilience that translates to life outside the gym. It has been suggested that a self-defense curriculum may provide an enhanced exposure therapy-like experience.11 Allowing veterans to repeatedly practice problem solving and successfully resolve difficult, uncomfortable struggles may promote re-learning how to be effective in adverse circumstances. Perception of being capable of contribution to the resolution of a traumatic event may lead to fewer symptoms of PTSD.28
Social withdrawal is an avoidance strategy that is associated with development of PTSD.29 A potential benefit of BJJ is that it forces its practitioners to engage in social interaction; the only way to practice and learn is to have training partners to grapple with. In addition to social interaction, the training paradigm in this study could also provide a degree of social support, since the participants were interacting with others who shared similar life experiences. It remains to be determined whether the participants would have experienced similar reductions in PTSD symptomology if they trained with others who had not served in the armed forces.30
In summary, veterans in this study had clinically significant improvements in symptoms of PTSD as determined using the PCL-5 and the PTSD subscale of the PDSQ self-report questionnaires. Meaningful reductions in PTSD comorbidities including depression, generalized anxiety, and alcohol use were also reported. The magnitude of the effect sizes suggests that routine practice of BJJ may be a beneficial complementary approach for the treatment of PTSD. However, given the limitations of the current small number of subjects and high percentage of subjects who did not complete the full 5-month program, these results should clearly be interpreted with caution. Going forward, it is imperative to conduct more rigorous testing to determine if these effects endure in a larger sample of veterans and/or armed services personnel of both genders. Moreover, future studies would benefit greatly from the use of an experimental design (e.g., randomized controlled trial). In this realm, the extent to which the practice of BJJ might impart similar benefits as compared to those achieved with traditional PTSD therapies or even other complementary or alternative medicine approaches could be formally evaluated.
Supplementary Material
FUNDING
State of Florida Department of Education.
CONFLICTS OF INTEREST
RD and RWD own Tampa Jiu Jitsu, where the BJJ training was offered. They participated in BJJ instruction, but had no role in study design, data collection, data analysis, or manuscript preparation
PREVIOUS PRESENTATIONS
The work contained in this paper was presented in poster form at the American Society for Neural Therapy and Repair annual meeting, April 2016 and at the Society for Neuroscience annual meeting, November 2016.
REFERENCES
- 1. American Psychiatric Association : Diagnostic and Statistical Manual of Mental Disorders, 5th ed Washington, DC, 2013. [Google Scholar]
- 2. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE: Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005; 62(6): 593–602. [DOI] [PubMed] [Google Scholar]
- 3. Kang B, Xu H, McConnell ES: Neurocognitive and psychiatric comorbidities of posttraumatic stress disorder among older veterans: a systematic review. Int J Geriatr Psychiatry 2019; 34(4): 522–38. 10.1002/gps.5055. [DOI] [PubMed] [Google Scholar]
- 4. Walter KH, Levine JA, Highfill-McRoy RM, Navarro M, Thomsen CJ: Prevalence of posttraumatic stress disorder and psychological comorbidities among U.S. active duty service members, 2006–2013. J Trauma Stress 2018; 31(6): 837–44. [DOI] [PubMed] [Google Scholar]
- 5. Kok BC, Herrell RK, Thomas JL, Hoge CW: Posttraumatic stress disorder associated with combat service in Iraq or Afghanistan: reconciling prevalence differences between studies. J Nerv Ment Dis 2012; 200(5): 444–50. [DOI] [PubMed] [Google Scholar]
- 6. The Management of Posttraumatic Stress Disorder Work Group VA/DOD Clinical Practice guideline for the management of posttraumatic stress disorder and acute stress disorder, version 3.0. Department of Veterans Affairs and Department of Defense. Washington, DC, 2017. [Google Scholar]
- 7. Liu X, Clark J, Siskind D, et al. : A systematic review and meta-analysis of the effects of Qigong and Tai Chi for depressive symptoms. Complement Ther Med 2015; 23(4): 516–34. [DOI] [PubMed] [Google Scholar]
- 8. Papacosta E, Gleeson M, Nassis GP: Salivary hormones, IgA, and performance during intense training and tapering in judo athletes. J Strength Cond Res 2013; 27(9): 2569–80. [DOI] [PubMed] [Google Scholar]
- 9. Wang C, Bannuru R, Ramel J, Kupelnick B, Scott T, Schmid CH: Tai Chi on psychological well-being: systematic review and meta-analysis. BMC Complement Altern Med 2010; 10: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wang F, Lee EK, Wu T, et al. : The effects of tai chi on depression, anxiety, and psychological well-being: a systematic review and meta-analysis. Int J Behav Med 2014; 21(4): 605–17. [DOI] [PubMed] [Google Scholar]
- 11. David WS, Simpson TL, Cotton AJ: Taking charge: a pilot curriculum of self-defense and personal safety training for female veterans with PTSD because of military sexual trauma. J Interpers Violence 2006; 21(4): 555–65. [DOI] [PubMed] [Google Scholar]
- 12. Chisholm DM, Collis ML, Kulak LL, Davenport W, Gruber N: Physical activity readiness. B C Med J 1975; 17: 375–8. [Google Scholar]
- 13. Bovin MJ, Marx BP, Weathers FW, et al. : Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition (PCL-5) in veterans. Psychol Assess 2016; 28(11): 1379–91. [DOI] [PubMed] [Google Scholar]
- 14. Zimmerman M, Chelminski I: A scale to screen for DSM-IV Axis I disorders in psychiatric out-patients: performance of the Psychiatric Diagnostic Screening Questionnaire. Psychol Med 2006; 36(11): 1601–11. [DOI] [PubMed] [Google Scholar]
- 15. Zimmerman M, Mattia JI: A self-report scale to help make psychiatric diagnoses: the Psychiatric Diagnostic Screening Questionnaire. Arch Gen Psychiatry 2001; 58(8): 787–94. [DOI] [PubMed] [Google Scholar]
- 16. Derogatis LR: BSI Brief Symptom Inventory: Administration, Scoring, and Procedure Manual, 4th ed., Minneapolis, MN, National Computer Systems, 1993. [Google Scholar]
- 17. Tedeschi RG, Calhoun LG: The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress 1996; 9(3): 455–71. [DOI] [PubMed] [Google Scholar]
- 18. Ensel WM: Measuring Depression: The CES-D Scale. NY, New York, Academic Press, 1986. [Google Scholar]
- 19. Radloff LS: The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401. [Google Scholar]
- 20. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ: The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28(2): 193–213. [DOI] [PubMed] [Google Scholar]
- 21. Davis TM, Bush KR, Kivlahan DR, Dobie DJ, Bradley KA: Screening for substance abuse and psychiatric disorders among women patients in a VA Health Care System. Psychiatr Serv 2003; 54(2): 214–8. [DOI] [PubMed] [Google Scholar]
- 22. Maust DT, Mavandadi S, Klaus J, Oslin DW: Missed opportunities: fewer service referrals after positive alcohol misuse screens in VA primary care. Psychiatr Serv 2011; 62(3): 310–2. [DOI] [PubMed] [Google Scholar]
- 23. Clark ME, Gironda RJ, Young RW: Development and validation of the Pain Outcomes Questionnaire-VA. J Rehabil Res Dev 2003; 40(5): 381–95. [DOI] [PubMed] [Google Scholar]
- 24. Morris SB, DeShon RP: Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol Methods 2002; 7(1): 105–25. [DOI] [PubMed] [Google Scholar]
- 25. Whitworth JW, Ciccolo JT: Exercise and post-traumatic stress disorder in military veterans: a systematic review. Mil Med 2016; 181(9): 953–60. [DOI] [PubMed] [Google Scholar]
- 26. Oppizzi LM, Umberger R: The effect of physical activity on PTSD. Issues Ment Health Nurs 2018; 39(2): 179–87. [DOI] [PubMed] [Google Scholar]
- 27. Rosenbaum S, Vancampfort D, Steel Z, Newby J, Ward PB, Stubbs B: Physical activity in the treatment of Post-traumatic stress disorder: a systematic review and meta-analysis. Psychiatry Res 2015; 230(2): 130–6. [DOI] [PubMed] [Google Scholar]
- 28. Saccinto E, Valles L, Hilterman E, Roiha M, Pietrantoni L, Perez-Testor C: Perceived self-efficacy during an emergency situation reduces posttraumatic stress symptoms. Span J Psychol 2013; 16: E56. [DOI] [PubMed] [Google Scholar]
- 29. Thompson NJ, Fiorillo D, Rothbaum BO, Ressler KJ, Michopoulos V: Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. J Affect Disord 2018; 225: 153–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jain S, McLean C, Adler EP, Rosen CS: Peer support and outcome for veterans with posttraumatic stress disorder (PTSD) in a residential rehabilitation program. Community Ment Health J 2016; 52(8): 1089–92. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.