Abstract
Little is known about how adolescents receive depression follow-up care in primary care. The purpose of this study was to describe the rates of symptom assessment and depression treatment over time in a group of adolescents screening positive for moderate or severe depression in the primary care setting. Retrospective chart reviews were conducted to gather information related to symptom reassessments, antidepressant prescriptions, psychotherapy referrals, and treatment discontinuation. Descriptive statistics were calculated, and a qualitative content analysis was conducted to determine reasons for treatment discontinuation. Eighty records were reviewed (mean age=15.3; 73% female; 59% Black). Treatment was initiated for 83% (n=66) of patients, and 45% (n=30) of patients discontinued treatment during the review period for a variety of reasons. To improve adolescents’ adherence to depression treatment, providers should address factors that contribute to treatment discontinuation and use tools to manage depression follow-up care.
Keywords: Adolescent, depression, primary health care, psychotherapy, antidepressants
Introduction
Adolescent depression is a prevalent and serious problem in the United States. In 2017, an estimated 13.3% of US adolescents experienced a major depressive episode (Substance Abuse and Mental Health Services Administration [SAMHSA], 2018). Recent analysis of national data has also shown that rates of adolescent depression have risen significantly over the past ten years (Mojtabai, Olfson, & Han, 2016; Twenge, Joiner, Rogers, & Martin, 2018). Depression is also associated with significant sources of morbidity and mortality in adolescents, such as anxiety, substance abuse, and suicidal behavior (Thapar, Collishaw, Pine, & Thapar, 2012).
For the majority of adolescents, depression is treated by a provider in the primary care setting rather than by a mental health specialist (Anderson, Chen, Perrin, & Van Cleave, 2015; Olfson, Blanco, Wang, Laje, & Correll, 2014). Although pediatric primary care providers receive comprehensive training in a wide range of health conditions, formal training in the management of psychiatric disorders is necessarily limited in scope (Shahidullah et al., 2018), and pediatric primary care providers have expressed a lack of confidence in identifying and treating mental health disorders (Horwitz et al., 2015). The American Academy of Pediatrics (AAP) developed Guidelines for Adolescent Depression in Primary Care (GLAD-PC) to assist primary care providers in the delivery of research-supported depression screening, assessment, and treatment services for youth (Cheung et al., 2007; Cheung, Zuckerbrot, Jensen, Laraque, & Stein, 2018). For adolescents with moderate or severe depression (the population on which this study focuses), the AAP recommends that the primary care provider initiate one or more evidenced-based treatments for adolescent depression, such as psychotherapy or antidepressant medications (Lewandowski et al., 2013) at the time of the positive screening (Cheung et al., 2007; Cheung et al., 2018). The individual should be reassessed by the primary care provider within 6–8 weeks to determine if symptoms have improved or worsened (Cheung et al., 2007; Cheung et al., 2018).
Although guidelines exist for the management of depression care in primary care, many adolescents experiencing depression do not obtain the appropriate mental health treatment in this setting (SAMHSA, 2018; Merikangas et al., 2011). Many adolescents who are diagnosed with depression in primary care do not receive any form of mental health treatment. In a large sample of US youth, O’Connor and colleagues (2016) found that 21% of adolescents screening positive for moderate to severe depression in primary care did not receive any treatment for depression. Of those who did receive treatment in the primary care setting, many were prescribed antidepressants and/or referred to psychotherapy, consistent with best practice guidelines. O’Connor and colleagues (2016) observed that 29% of adolescents with depression were referred to psychotherapy alone, 19% were prescribed an antidepressant alone, and 16% received a combination of psychotherapy referral and antidepressant prescription.
Two studies have examined provider follow-up for depression among adolescents in primary care. Both studies found that the majority of adolescents receiving antidepressant prescriptions did not receive the recommended clinical follow-up (Cloutier et al., 2013; O’Connor et al., 2016). Cloutier and colleagues (2013) found that 80% of Canadian adolescents who were prescribed an antidepressant by a primary care provider did not receive adequate follow-up visits, as defined by having three follow-up visits during the first three months of treatment. Similarly, a study by O’Connor and colleagues (2016) found that 40% of US adolescents prescribed an antidepressant did not receive any follow-up care in the three months following the prescription of an antidepressant. Moreover, 68% of adolescents did not receive a reassessment of depressive symptoms in the three months following their initial depression diagnosis (O’Connor et al., 2016). While these studies have examined important aspects of adolescent depression treatment and follow-up, they have done so within a short time frame and therefore may have missed follow-up services that occurred several months following initial screening and diagnosis. Since many studies have demonstrated that adolescent depression is a complex disorder (Eapen & Crncec, 2012) and has a high potential to reoccur in the future (Thapar et al., 2012), it is important to consider how adolescent depression treatment evolves over longer periods of time.
To promote higher adherence to best practice management of adolescent depression in primary care, it is important not only to characterize current practice patterns but also to understand factors that lead to adherence and non-adherence to recommendations. Some factors that impact patients’ receipt of appropriate follow-up care may be outside the typical scope of the primary care provider. For instance, a review of adherence research found that side effects, difficulty getting prescriptions filled, cost, low social support, lack of accessibility, and negative attitudes towards treatment affected adherence to treatment across a range of physical and mental health conditions in adolescent and adult populations (Jin, Sklar, Oh, & Li, 2008). In a recent review focused on adolescents, poor social support and coerced treatment were associated with non-adherence to psychiatric treatment for adolescents experiencing a variety of mental health conditions (Timlin, Hakko, Heino, & Kyngäs, 2014). More research is needed to determine factors that impact adherence to mental health treatments among adolescents (Häge et al., 2016; Timlin et al., 2014). To our knowledge, no studies have examined reasons for non-adherence to treatment for adolescents being treated for depression in primary care. Since the majority of adolescents are treated for depression in primary care, it is important to explore patient, family, and provider factors that impact adherence to depression treatment.
The current study examined patterns of adolescent depression treatment in the primary care setting using retrospective chart review data. The purpose of this study was to examine the rates of depression symptom assessment, psychotherapy referral, antidepressant prescription, and treatment discontinuation over two years among a group of adolescents screening positive for moderate and severe depression in the primary care setting. The specific aims of the study were to:
Determine how many adolescents received treatment for depression;
Determine what percentage of adolescents received depression follow-up care according to AAP GLAD-PC recommendations;
Determine how many adolescents discontinued prescribed depression treatment over time; and
Explore the reasons why adolescents discontinued depression treatment.
Method
Study Design
This study consisted of descriptive, retrospective chart reviews for adolescent patients who screened positive for moderate or severe depression in two primary care clinics.
Participants and Setting
Participants were identified through a Computer Decision Support System (CDSS), called the Child Health Improvement through Computer Automation (CHICA) System, implemented by the research team in two primary care clinics. One component of the system is a Pre-Screener Form (PSF) which is administered to patients via tablet upon check-in to their well-child visits. The PSF consists of a 20-item tailored questionnaire, including screening items for depression, substance use, diet, and sexual behaviors, administered to adolescents between the ages of 12 and 20 at their well-child visits. Based on patients’ responses to these questions, a primary care provider worksheet is generated prioritizing the top six health needs of the patient with provider action prompts based on Bright Futures guidelines (Tanski, Garfunkel, Duncan, & Weitzman, 2010). A detailed description of the system has been described elsewhere (Anand, Biondich, Liu, Rosenman, & Downs, 2004; Anand, Carroll, Biondich, Dugan, & Downs, 2015; Aalsma et al., 2018; Carroll et al., 2013; Gilbert & Downs, 2015).
The primary care clinics where these visits took place were part of the local county hospital system in an urban, Midwest city. Primary care providers at these clinics were primarily trained in pediatrics with some being adolescent medicine board certified. The team received exempt Institutional Review Board approval to conduct this study from the local university.
The research team created and tested an adolescent depression module (Aalsma et al., 2018). Adolescents aged 12–20 were specifically screened for depression on the PSF using the Patient Health Questionnaire-2 (PHQ-2; Richardson et al., 2010a) with a reflex Patient Health Questionnaire-9 (PHQ-9; Richardson et al., 2010b). Patients were first asked the two items on the PHQ-2, which assess for anhedonia and depressed mood in the past two weeks. If patients answered either of these questions affirmatively, the PHQ-9 was automatically administered and scored. A score of 5–9 indicated mild depression; a score of 10–14 indicated moderate depression, and a score of >14 indicated severe depression (Kroenke, Spitzer, & Williams, 2001). It should be noted that Richardson and colleagues (2010b) recommend a PHQ-9 cut off greater than 10 for adolescent patients; however, the study team chose a lower cut off in order to identify more youth that may need follow-up for depression management in primary care. Primary care providers were given guidance on next steps according to AAP GLAD-PC guidelines based on the patient’s PHQ-9 score.
Adolescents were included in the sample for this study if they were aged 12–20 at their first positive depression screening with the CDSS and scored in the moderate or severe range on the PHQ-9 (score >9; Kroenke et al., 2001). The team chose to focus the chart reviews on these patients since the AAP recommends antidepressant medication and/or psychotherapy treatment for patients with moderate to severe depression (Cheung et al., 2007; Cheung et al., 2018). While the AAP recommends that primary care providers conduct a diagnostic interview after a positive self-report screening (Cheung et al., 2007; Cheung et al., 2018), individuals without a diagnosis of depression in their medical record were not excluded from the analysis to determine how all individuals screening positive for moderate or severe depressive symptoms received follow-up care over time. Individuals were excluded from analysis if they did not have a complete clinic visit record (n=3).
Chart Abstraction
Retrospective chart reviews were conducted on all patients with a PHQ-9 score greater than 9 from October 2014 to December 2016. All initial positive depression screens occurred in 2014 or 2015. Primary care provider notes for each primary care visit from 2014–2016 were reviewed, and data related to the variables in Table 1 were entered into a spreadsheet. The patients’ records were split and initially reviewed by three trained coders. Each primary care visit was entered into a separate row in the spreadsheet, and reviewers placed data into columns based on the variables in Table 1.
Table 1.
Variables Extracted from the Medical Record
| Variable Label | Description | Response Scale |
|---|---|---|
| Date of visit | Date of primary care visit | Date |
| PHQ-9 Score | PHQ-9 score at visit. Used to determine if and when individuals received symptom reassessments | Numeric score |
| Comorbid Diagnoses | Any diagnoses listed in the medical record, including depression diagnoses | Free response |
| Not Depressed/No Concerns | Visits in which the provider noted that the patient was no longer depressed | Yes/No |
| Started on SSRI | Visits in which the provider initiated SSRI | Yes/No |
| Maintain Dose | Visits in which the provider maintained the SSRI dose | Yes/No |
| Increase Dose | Visits in which the provider increased the SSRI dose | Yes/No |
| Decrease Dose | Visits in which the provider decreased the SSRI dose | Yes/No |
| SSRI Change | Visits in which the provider switched the patient to a different SSRI | Yes/No |
| SSRI Stop | Visits in which the provider noted the patient had discontinued use of the SSRI | Yes/No |
| Psychotherapy Referral | Visits in which the provider referred the patient to psychotherapy | Yes/No |
| Psychotherapy Not Interested | Visits in which the patient reported they were uninterested in psychotherapy | Yes/No |
| Psychotherapy Attending | Visits in which the provider noted that the patient was currently attending psychotherapy | Yes/No |
| Reasons for Stopping SSRI | Any reason noted in the chart related to the patient’s discontinuation of the SSRI | Free response |
| Reasons for Stopping Psychotherapy | Any reason noted in the chart related to the patient’s discontinuation of psychotherapy | Free response |
| Depression Not Mentioned | Any visits in which depression was not mentioned in the provider note | Yes/No |
Data Analysis
Two reviewers recoded a randomly selected 20% of patients’ charts to calculate interrater reliability. The pooled kappa was 0.71 indicating substantial agreement (Landis & Koch, 1977). Descriptive statistics were calculated using IBM SPSS Statistics 24 (2016) to address the first three aims. For aim three, the AAP GLAD-PC (Cheung et al., 2007) recommendations released in 2007 were used as the standard by which adherence to best practice guidelines was determined. GLAD-PC was updated by the AAP in 2018 (Cheung et al., 2018) with updated recommendations regarding primary care provider depression management training, integrated depression care, and universal depression screening (Cheung et al., 2018). However, since the medical record visits used for analysis took place prior to the release of these updated recommendations, the 2007 GLAD-PC recommendations were used to determine adherence to best practice guidelines. Additionally, guidelines related to ongoing management of depression in the primary care setting did not change substantially between the 2007 and 2018 publications (Cheung et al., 2007; Cheung et al., 2018).
To address aim four, qualitative descriptive content analysis methods were used to determine reasons for discontinuing selective serotonin reuptake inhibitor (SSRI) medications and psychotherapy among all patients. Primary care provider notes were reviewed for any information regarding reasons for SSRI or psychotherapy discontinuation. Conventional content analysis methods were used to derive categories from the textual data without having predefined categories, allowing the categories to emerge from the data (Hsieh & Shannon, 2005). Two individuals reviewed the qualitative data independently, placing similar reasons for discontinuation of SSRIs and psychotherapy into categories. The two reviewers then met to determine the final categories of reasons for SSRI and psychotherapy discontinuation based on consensus.
Results
Eighty youth met inclusion criteria. Patients were, on average, 15.25 years old (SD=2.3) at the first positive depression screening. Seventy-three percent (n=58) were female. The majority of the sample was Black (59%; n=47). The remainder of the sample was Hispanic (12.5%; n=10), White (10%; n=8), or of other/unknown race or ethnicity (19%; n=15). Individuals averaged 4.2 (SD=3.1) visits with a primary care provider over the two-year review period. The average number of primary care visits in which depression was addressed was 3.1 (SD=2.3). The average PHQ-9 score at the first positive screening was 14.4 (SD=3.6). Records indicated that 71.3% (n=57) of adolescents with a positive depression screening had a documented depression diagnosis during the review period. Primary care was provided by clinicians trained in pediatrics (33%; n=15), family medicine (24%; n=11), pediatric or family nursing practice (15%; n=7), adolescent medicine (11%; n=5), medicine-pediatrics (6.5%, n=3), internal medicine (4%; n=2), and other medical specialties (6.5%; n=3)
Rates of Depression Treatment
Rates of depression treatment according to depression diagnosis are presented in Table 2. A total of 83% (n=66) of records indicated that the patient received depression treatment during the review period. Ninety-eight percent (n=56) of those adolescents with diagnoses of depression received treatment for depression during the review period. Forty-three percent (n=10) of adolescents screening positive for moderate or severe depression but not receiving a diagnosis of depression received treatment for depression. The majority of participants received psychotherapy alone or a combination of psychotherapy and SSRI prescriptions. Eighteen percent (n=14) of patients did not receive any treatment for depression over the review period according to the medical record; the majority of these individuals did not have a documented diagnosis of depression.
Table 2.
Rates of Depression Treatment according to Depression Diagnosis over Two-Year Period
| Treatment type (N=80) | Depression Diagnosis (n=57) n (%) | No Depression Diagnosis (n=23) n (%) |
|---|---|---|
| Antidepressant prescription only | 4 (7%) | 0 (0%) |
| Psychotherapy referral only | 23 (40%) | 8 (35%) |
| Both psychotherapy referral and antidepressant prescription | 29 (51%) | 2 (8.5%) |
| No depression treatment | 1 (2%) | 13 (56.5%) |
Rates of Depression Treatment Follow-up according to GLAD-PC
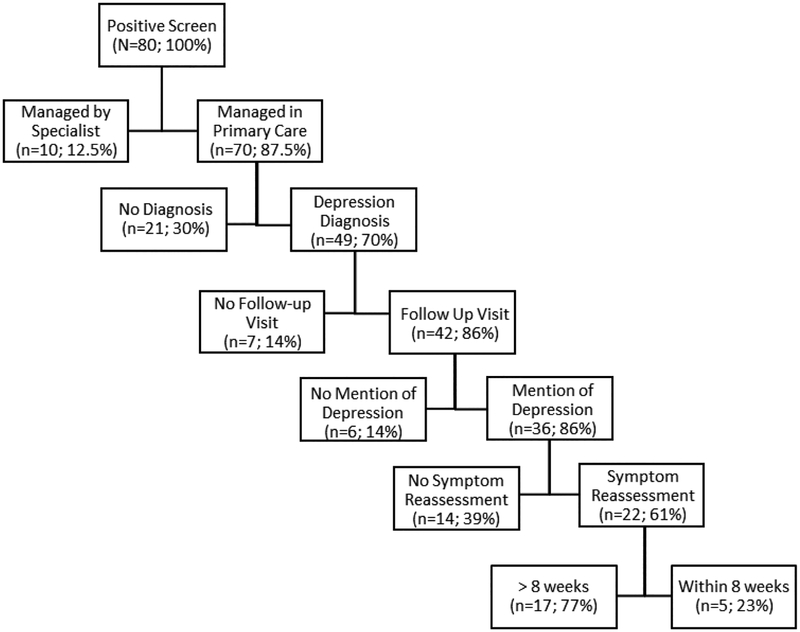
The rates of various depression follow-up actions are depicted in Figure 1. Out of the 80 patients, 12.5% (n=10) were referred to a mental health specialist for medication and psychotherapy management outside of primary care. Of those who were not referred to a mental health specialist (n=70), records indicated that 70% (n=49) received a diagnosis of depression. Of those with a diagnosis of depression, 14% of patients (n=7) did not have any follow-up visits with a primary care provider; these individuals were diagnosed with depression and never returned for a primary care visit within the hospital system. Records indicated that 86% of patients (n=42) with diagnoses of depression did have subsequent visits with a primary care provider. For 14% of patients (n=6) who had additional primary care visits, there was no mention of depression in the visit record; these individuals were diagnosed with depression and returned to the clinic for visits, but none of those visits addressed symptoms of depression. Eighty-six percent of patients (n=36) had subsequent follow-up visits in which concerns with depression were documented in the medical record. Sixty-one percent (n=22) with follow-up visits addressing depression had a documented symptom reassessment of depressive symptoms using the PHQ-9. The remaining 39% of patients (n=14) attending visits where depression was addressed did not have a documented symptom reassessment. Of those with symptom reassessments, five (23%) received them within the recommended period (6–8 weeks).
Figure 1. Rates of Depression Follow-Up Care.
Flow diagram depicting rates of depression follow-up care for adolescents according to American Academy of Pediatrics Guidelines for Adolescent Depression in Primary Care.
Rates of and Reasons for Treatment Discontinuation
Of the patients who received treatment for depression, 45% (n=30) discontinued their depression treatment during the review period. For 83% of patients (n=25) who discontinued treatment, primary care providers documented a reason for discontinuation of depression treatment. Of those prescribed an antidepressant, 69% (n=24) discontinued treatment, and of those referred to or already attending psychotherapy, medical records indicated that 24% (n=15) stopped attending psychotherapy. Four individuals discontinued antidepressant treatment and two individuals discontinued psychotherapy due to resolution of depressive symptoms, as noted in the medical record.
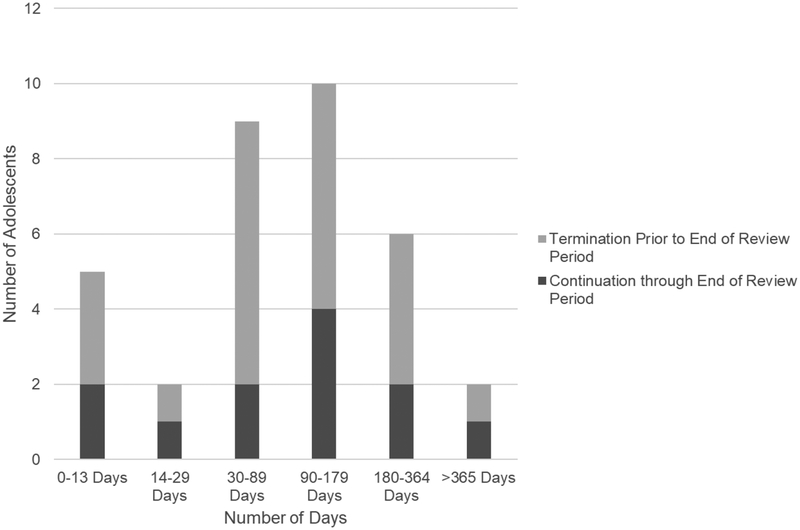
When records indicated that participants terminated treatment for any reason other than resolution of depressive symptoms, participants were considered to have prematurely discontinued depression treatment. For 17 patients, providers documented reasons for premature discontinuation of antidepressants, including negative side effects (n=5), prescription refill issues (n=4), inability to afford treatment (n=3), negative personal attitudes towards antidepressants (n=3), and family resistance to antidepressant treatment (n=3). For three patients, personal attitudes and family resistance to antidepressant treatment prevented patients from initiating antidepressant treatment after it had been prescribed to them. The majority of patients prescribed SSRIs also terminated use of SSRI medication prior to one year of use, in contrast to the recommendation by the AAP (See Figure 2; Cheung et al., 2007).
Figure 2. Duration of SSRI Treatment.
Chart depicting duration of medication use in days for the 27 patients who were prescribed SSRI medication that was managed by a primary care provider. Records indicated that seven patients started and stopped antidepressant medication two times during the review period. Data in this chart reflect instances of initial SSRI uptake for all patients (n=27) as well as second round SSRI uptake (n=7). SSRI = Selective Serotonin Reuptake Inhibitor
Providers documented reasons for premature discontinuation of psychotherapy for eight patients. Reasons for premature discontinuation of psychotherapy noted in the medical record included lack of therapist availability (n=4), family transitions (e.g. moving; n=3), disinterest in psychotherapy (n=3), and cost (n=1).
Discussion
Many adolescents who receive treatment for depression obtain it within the primary care setting, and while guidelines exist for the treatment of adolescent depression in this setting, this study demonstrated that the majority of adolescent patients may not receive depression follow-up care according to best practice guidelines, even within the context of a CDSS which supports adolescent depression screening and subsequent management.
The current study demonstrated that 83% of adolescents screening positive for moderate or severe depression received some form of depression treatment during the course of the two-year review period, and almost all adolescents (98%) with a diagnosis of depression received depression treatment during the review period. O’Connor and colleagues (2016) found that treatment was initiated for 79% of adolescents within the first three months of receiving a depression diagnosis, while Soria-Saucedo, Walter, Cabral, England, & Kazis (2016) found a lower rate of 58% of youth receiving necessary treatment for depression. The use of a CDSS to screen for depressive symptoms and prompt provider responses to depressive symptoms, as was the case in this study, may explain the higher rates of treatment initiation, since CDSS is well known to improve adherence to other screening and treatment protocols (Murphy, 2014). Over time, adolescents experiencing depression may have a progressively increasing likelihood of being connected to treatment, also potentially explaining the higher rates of treatment initiation in the current study.
The current study also examined the rates of adherence to AAP GLAD-PC depression management recommendations. Records indicated that, of those diagnosed with and treated for depression in the primary care setting, 86% of patients received some form of follow-up care related to their depression, and 10% received a documented symptom reassessment within the recommended 8-week period, consistent with AAP guidelines. O’Connor et al. (2016) found similar rates of depression follow-up care (81%) and higher rates of symptom reassessment within three months (32%). Even within the context of the CDSS that was used in the current study, symptom reassessment rates according to best practice guidelines were still low. Further development of CDSS to more precisely identify patients who should be scheduled at sooner intervals based on screening and diagnosis results, re-administer symptom checklists, and prompt primary care provider responses based on symptom reassessments may improve provider management of adolescent depression follow-up care and promote greater adherence to AAP GLAD-PC recommendations (Koposov et al., 2017).
This study is one of the first to examine the rates of discontinuation of depression treatment among adolescents in the primary care setting, with medical records indicating that 45% of patients prescribed to antidepressants or referred to psychotherapy discontinued their treatment. This is similar to what was found in a recent study by Cummings, Ji, Lally, and Druss (2019), in which 50% of Medicaid-enrolled youth diagnosed with depression did not receive minimally adequate treatment for depression (i.e. >3 psychotherapy visits and/or >144 days of antidepressant refills) in the 6 months following a diagnosis of depression. The rate of treatment discontinuation observed in our study is also similar to overall rates of depression treatment discontinuation noted among adult populations (40%; Fortuna, Alegria, & Gao, 2010; Mowbray, Campbell, Kim, & Scott, 2018). In particular, adolescents who were prescribed antidepressant medication had high rates of discontinuation. Provider notes revealed that the majority of these adolescents did not continue use of SSRIs for the recommended one-year period (Cheung et al., 2007). One reason that rates of psychotherapy discontinuation may have been lower is that adolescents receiving psychotherapy would have a more continual source of support to troubleshoot any issues with treatment, boost motivation, and encourage treatment engagement (Hamrin & Iennaco, 2017; Hamrin, Sinclair, & Gardner, 2017). If adolescents are prescribed medications without the support of a mental health professional, they may not have sufficient support to continue with treatment, especially if they have not received education about what to expect or how to troubleshoot problems with their medication. Beyond engaging adolescents in psychotherapy when they are prescribed an antidepressant medication, CDSS or other technology could be used to improve patient adherence to depression treatment protocols by messaging adolescents or caregivers within 1–2 weeks of starting a medication to conduct automated or highly structured assessments concerning side effects, problems with prescription refills, or other general questions or concerns.
Many of the reasons for discontinuation listed in the medical record were similar to those that have been observed across a range of health treatments, such as cost, lack of family support for treatment, issues with prescription refills, and medication side effects (Jin, Sklar, Oh, & Li, 2008). In the current study, adolescents’ personal attitudes towards psychotherapy and antidepressant medication also were common reasons for discontinuing treatment. To improve treatment engagement, primary care providers should assess barriers to engagement, such as patient and caregiver beliefs about depression treatments at the onset of treatment. If patients endorse negative attitudes towards treatment, providers can deliver psychoeducation regarding the causes of and treatments for depression (Li, Dorstyn, & Denson, 2014) or match patients’ beliefs about depression to corresponding treatments (Vittengl, Clark, Thase, & Jarrett, 2018). For example, psychotherapy may be a more appropriate treatment option for patients who do not endorse beliefs about the biological etiology of depression (Vittengl et al., 2018). It is also possible that discussing expectations about treatment and troubleshooting solutions to potential problems before they occur may promote adherence to prescribed depression treatments (Rush & Thase, 2018). Strategies such as shared decision aids (Simmons, Elmes, McKenzie, Trevena, & Hetrick, 2017) or brief motivational interviewing sessions delivered in the primary care setting (Hamrin & Iennaco, 2017) also may be helpful in boosting adolescents’ adherence to psychotropic medications for depression. The integration of behavioral health services into the primary care setting may also assist in addressing barriers to treatment engagement, such as lack of therapist availability (Richardson, McCarty, Radovic, & Suleiman, 2017).
This study was limited by the use of the medical record as a method for determining rates of depression treatment and follow-up. Individuals may have received care for depression that was outside of the health system network or not documented in the medical record. Additionally, reasons for the adolescent’s discontinuation of treatment may not have been noted in the medical record. The current study also only examined records associated with primary care visits; visit records for other providers, such as social workers and mental health specialists, were not included in the analysis and may have contained important information about depression management. It appeared that some of the adolescents included in the study obtained mental health treatment outside of the healthcare system; thus, to remain consistent, we decided to only examine primary care provider notes concerning depression follow-up care. During data abstraction, the healthcare system migrated to a new electronic health record platform, and during this process, three patient records were found to have missing appointment information. Other information may have been missing from patient records after the migration of which the team was unaware.
This study also has limited generalizability given the composition of the sample and data collection setting. First, the sample in this study was small, and the majority of patients were female and Black. Also, the majority of primary care providers involved in caring for participants were trained in pediatrics and may have received more specialized training in managing pediatric mental health concerns than other specialties such as family or internal medicine primary care providers. Additionally, all participants were identified by CDSS which was implemented in two primary care clinics. Research should be conducted to determine rates of depression follow-up care in larger, more representative samples.
Conclusions
Despite the small sample size, the findings of the current study suggest that many adolescents receiving treatment for depression in the primary care setting may not be receiving follow-up care for depression according to AAP guidelines and prematurely discontinuing depression treatment. While using a CDSS to screen adolescents for depressive symptoms may improve treatment initiation, ensuring that adolescents receive follow-up care for depression remains a challenge. Due to the complexity of depression and high possibility for recurrence in the future, strategies should be developed to improve rates of depression treatment follow-up and adherence to best practice guidelines within the primary care setting.
Acknowledgements:
The authors would like to thank our research assistants for their assistance in chart reviews including Lindsey Jones, Taylor Hunton, and Marilyn Pate.
Grant Support: The design, data collection, analysis, and interpretation of data of this study was supported by a grant from the Agency for Healthcare Research and Quality [R01HS022681]. Data analysis, interpretation, and the writing of the manuscript was supported by a grant from the National Institutes of Health [NINR T32NR007066].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: Dr. Downs is a co-founder of Digital Health Solutions, LLC, a company created to market the Computer Decision Support System software discussed in this paper. The remaining authors have no conflicts to report.
Submission Declaration: This article is original and not under consideration elsewhere. We presented preliminary findings of this project in the form of a poster presentation at the Society for Adolescent Health and Medicine Conference on March 16, 2018. The poster presentation abstract was published in SAHM’s Journal of Adolescent Health and can be found at the link below. Since this presentation, we have added more participants to the sample, revised our inclusion and exclusion criteria, completed interrater reliability analysis, and updated our results. https://www.jahonline.org/article/S1054-139X(17)30710-3/pdf
Clinical Trials Registry:
Consent: The team received exempt Institutional Review Board approval to conduct this study from Indiana University.
References
- Anderson LE, Chen ML, Perrin JM, & Van Cleave J (2015). Outpatient visits and medication prescribing for US children with mental health conditions. Pediatrics, 136(5), e1178–e1185. doi: 10.1542/peds.2015-0807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand V, Biondich PG, Liu GC, Rosenman M, & Downs SM (2004). Child health improvement through computer automation: The CHICA system. Studies in Health Technology and Informatics, 107(Pt 1), 187–191. doi: 10.3233/978-1-60750-949-3-187 [DOI] [PubMed] [Google Scholar]
- Anand V, Carroll AE, Biondich PG, Dugan TM, & Downs SM (2015). Pediatric decision support using adapted Arden Syntax. Artificial Intelligence in Medicine, 92, 15–23. doi: 10.1016/j.artmed.2015.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll AE, Bauer NS, Dugan TM, Anand V, Saha C, & Downs SM (2013). Use of a computerized decision aid for ADHD diagnosis: a randomized controlled trial. Pediatrics, 132(3), e623–e629. doi: 10.1542/peds.2013-0933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert AL, & Downs SM (2015). Medical legal partnership and health informatics impacting child health: Interprofessional innovations. Journal of Interprofessional Care, 29(6), 564–569. doi: 10.3109/13561820.2015.1029066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aalsma MC, Zerr AM, Etter DJ, Ouyang F, Gilbert AL, Williams RL, … Downs SM (2018). Physician intervention to positive depression screens among adolescents in primary care. Journal of Adolescent Health, 62(2), 212–218. doi: 10.1016/j.jadohealth.2017.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung AH, Zuckerbrot RA, Jensen PS, Ghalib K, Laraque D, & Stein RE (2007). Guidelines for adolescent depression in primary care (GLAD-PC): II. Treatment and ongoing management. Pediatrics, 120(5), e1313–e1326. doi: 10.1542/peds.2006-1395 [DOI] [PubMed] [Google Scholar]
- Cheung AH, Zuckerbrot RA, Jensen PS, Laraque D, & Stein REK (2018). Guidelines for adolescent depression in primary care (GLADPC): Part II. Treatment and ongoing management. Pediatrics, 141(3), e20174082. doi: 10.1542/peds.2017-4081. [DOI] [PubMed] [Google Scholar]
- Cloutier AM, Greenfield B, Lavoie A, Lynd LD, Tournier M, Brabant MJ, & Moride Y (2013). Effectiveness of risk communication interventions on the medical follow-up of youth treated with antidepressants. Psychiatry Research, 209(3), 471–478. doi: 10.1016/j.psychres.2012.12.029 [DOI] [PubMed] [Google Scholar]
- Cummings JR, Ji X, Lally C, & Druss BG (2019). Racial and ethnic differences in minimally adequate depression care among Medicaid-enrolled youth. Journal of the American Academy of Child & Adolescent Psychiatry, 58(1), 128–138. doi: 10.1016/j.jaac.2018.04.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eapen V, & Crncec R (2012). Strategies and challenges in the management of adolescent depression. Current Opinion in Psychiatry, 25(1), 7–13. doi: 10.1097/YCO.0b013e32834de3bd [DOI] [PubMed] [Google Scholar]
- Fortuna LR, Alegria M, & Gao S (2010). Retention in depression treatment among ethnic and racial minority groups in the United States. Depression and Anxiety, 27(5), 485–494. doi: 10.1002/da.20685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Häge A, Weymann L, Bliznak L, Märker V, Mechler K, & Dittmann RW (2016). Non-adherence to psychotropic medication among adolescents–a systematic review of the literature. Zeitschrift für Kinder-und Jugendpsychiatrie und Psychotherapie, 44, 69–78. doi: 10.1024/1422-4917/a000505 [DOI] [PubMed] [Google Scholar]
- Hamrin V, & Iennaco JD (2017). Evaluation of motivational interviewing to improve psychotropic medication adherence in adolescents. Journal of Child and Adolescent Psychopharmacology, 27(2), 148–159. doi: 10.1089/cap.2015.0187 [DOI] [PubMed] [Google Scholar]
- Hamrin V, Sinclair VG, & Gardner V (2017). Theoretical approaches to enhancing motivation for adherence to antidepressant medications. Archives of Psychiatric Nursing, 31(2), 223–30. doi: 10.1016/j.apnu.2016.09.004 [DOI] [PubMed] [Google Scholar]
- Horwitz SM, Storfer-Isser A, Kerker BD, Szilagyi M, Garner A, O’Connor KG, … & Stein RE (2015). Barriers to the identification and management of psychosocial problems: changes from 2004 to 2013. Academic Pediatrics, 15(6), 613–620. doi: 10.1016/j.acap.2015.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, & Shannon SE (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- IBM SPSS Statistics for Windows, Version 24.0 [computer program]. (2016). Armonk, NY: IBM Corp. [Google Scholar]
- Jin J, Sklar GE, Oh VMS, & Li SC (2008). Factors affecting therapeutic compliance: A review from the patient’s perspective. Therapeutics and Clinical Risk Management, 4(1), 269–286. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2503662/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koposov R, Fossum S, Frodl T, Nytrø Ø, Leventhal B, Sourander A, … Skokauskas N (2017). Clinical decision support systems in child and adolescent psychiatry: A systematic review. European Child & Adolescent Psychiatry, 26(11), 1309–1317. doi: 10.1007/s00787-017-0992-0 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ‐9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis JR, & Koch GG (1977). The measurement of observer agreement for categorical data. Biometrics, 33, 159–174. Retrieved from https://www.jstor.org/stable/2529310 [PubMed] [Google Scholar]
- Lewandowski RE, Acri MC, Hoagwood KE, Olfson M, Clarke G, Gardner W, … & Frank S (2013). Evidence for the management of adolescent depression. Pediatrics, 132(4), e996–e1009. doi: 10.1542/peds.2013-0600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Dorstyn DS, & Denson LA (2014). Psychosocial correlates of college students’ help-seeking intention: A meta-analysis. Professional Psychology: Research and Practice, 45(3), 163–170. doi: 10.1037/a0037118 [DOI] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swendsen J, Avenevoli S, Case B, … & Olfson M (2011). Service utilization for lifetime mental disorders in US adolescents: results of the National Comorbidity Survey–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 50(1), 32–45. doi: 10.1016/j.jaac.2010.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, & Han B (2016). National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics, 138(6), e20161878. doi: 10.1542/peds.2016-18783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowbray O, Campbell RD, Kim I, & Scott JA (2018). Quitting mental health services among racial and ethnic groups of Americans with depression. The Journal of Behavioral Health Services & Research, 45(2), 269–279. doi: 10.1007/s11414-017-9560-0 [DOI] [PubMed] [Google Scholar]
- Murphy EV (2014). Clinical decision support: Effectiveness in improving quality processes and clinical outcomes and factors that may influence success. The Yale Journal of Biology and Medicine, 87(2), 187–197. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4031792/ [PMC free article] [PubMed] [Google Scholar]
- O’Connor BC, Lewandowski RE, Rodriguez S, Tinoco A, Gardner W, Hoagwood K, & Scholle SH (2016). Usual care for adolescent depression from symptom identification through treatment Initiation. JAMA Pediatrics, 170(4), 373–380. doi: 10.1001/jamapediatrics.2015.4158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M, Blanco C, Wang S, Laje G, & Correll CU (2014). National trends in the mental health care of children, adolescents, and adults by office-based physicians. JAMA Psychiatry, 71(1), 81–90. doi: 10.1001/jamapsychiatry.2013.3074 [DOI] [PubMed] [Google Scholar]
- Richardson LP, McCarty CA, Radovic A, & Suleiman AB (2017). Research in the integration of behavioral health for adolescents and young adults in primary care settings: A systematic review. Journal of Adolescent Health, 60(3), 261–269. doi: 10.1016/j.jadohealth.2016.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson LP, McCauley E, Grossman DC, McCarty CA, Richards J, Russo JE, … & Katon W (2010b). Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics, 126(6), 1117–1123. doi: 10.1542/peds.2010-0852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson LP, Rockhill C, Russo JE, Grossman DC, Richards J, McCarty C, … & Katon W (2010a). Evaluation of the PHQ-2 as a brief screen for detecting major depression among adolescents. Pediatrics, 125(5), e1097–e1103. doi: 10.1542/peds.2009-2712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, & Thase ME (2018). Improving depression outcome by patient-centered medical management. American Journal of Psychiatry, 175(12), 1187–1198 doi: 10.1176/appi.ajp.2018.18040398 [DOI] [PubMed] [Google Scholar]
- Shahidullah JD, Kettlewell PW, Palejwala MH, Forman SG, Billups A, Anismatta SL, & Madsen B (2018). Behavioral health training in pediatric residency programs: A national survey of training directors. Journal of Development & Behavioral Pediatrics, 39(4), 292–302. doi: 10.1097/DBP.0000000000000548 [DOI] [PubMed] [Google Scholar]
- Simmons MB, Elmes A, McKenzie JE, Trevena L, & Hetrick SE (2017). Right choice, right time: Evaluation of an online decision aid for youth depression. Health Expectations, 20(4), 714–723. doi: 10.1111/hex.12510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soria-Saucedo R, Walter HJ, Cabral H, England MJ, & Kazis LE (2016). Receipt of evidence-based pharmacotherapy and psychotherapy among children and adolescents with new diagnoses of depression. Psychiatric Services, 67(3), 316–323. doi: 10.1176/appi.ps.201500090 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2018). Results from the 2017 National Survey on Drug Use and Health: Mental health detailed tables. Retrieved from https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDetailedTabs2017.htm#tab9-8B
- Tanski S, Garfunkel LC, Duncan PM, & Weitzman M (2010). Performing preventive services: A Bright Futures handbook. Elk Grove Village, IL: American Academy of Pediatrics. [Google Scholar]
- Thapar A, Collishaw S, Pine DS, & Thapar AK (2012). Depression in adolescence. Lancet, 379, 1056–1067. doi: 10.1016/S0140-6736(11)60871- [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timlin U, Hakko H, Heino R, & Kyngäs H (2014). A systematic narrative review of the literature: Adherence to pharmacological and nonpharmacological treatments among adolescents with mental disorders. Journal of Clinical Nursing, 23(23–24), 3321–3334. doi: 10.1111/jocn.12589 [DOI] [PubMed] [Google Scholar]
- Twenge JM, Joiner TE, Rogers ML, & Martin GN (2018). Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clinical Psychological Science, 6(1), 3–17. doi: 10.1177/2167702617723376 [DOI] [Google Scholar]
- Vittengl JR, Clark LA, Thase ME, & Jarrett RB (2018). Could treatment matching patients’ beliefs about depression mprove outcomes?. Behavior Therapy. doi: 10.1016/j.beth.2018.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]