Abstract
Purpose:
Sagging eye syndrome (SES), horizontal and/or vertical strabismus caused by orbital connective tissue degeneration, was first defined 10 years ago. In this study, we investigated the causes of acquired binocular diplopia in adults presenting to single institution since the description of SES.
Design:
Retrospective observational case series.
Methods:
We reviewed medical records of all new patients over age 40 years who presented to the Stein Eye Institute with binocular diplopia between January 2015 and December 2018. We tabulated clinical causes of diplopia in patients grouped by age and gender. In patients with SES, we tabulated binocular alignment, types of treatment, and surgical outcomes.
Results:
There were 945 patients of mean age 66.5 years, of whom 514 (54.4%) were female. The most common cause of diplopia was SES (31.4%). The 297 patients with SES were older at 71.2 years (p<0.0001) and more predominantly female at 59.9% than other patients (52.0%, p=0.023). The relative proportion of SES patients among all diplopic patients increased with age from about 4.7% under age 50 years, to about 60.9% over age 90 years. Age-related distance esotropia was present in 35% of cases of SES. Cyclovertical strabismus was present in 65% of SES cases. Strabismus surgery was performed in 50.2% of cases of SES. Mean esotropia at distance decreased from 6.9±0.7Δ pre-operatively to 0.3±0.3Δ post-operatively. Pre-operative hypertropia decreased from 3.0±0.3Δ to 0.7±0.2Δ post-operatively. Surgery resolved diplopia in all cases.
Conclusion:
It is important to recognize that SES is a very common cause of adult binocular diplopia.
Introduction
Aging is a progressive risk factor for strabismus, with incidence increasing with age1. Reports of the causes of acquired diplopia in adults have emphasized cranial nerve palsies1–7, with most studies2–5 reporting trochlear or abducens palsy as the commonest cause of diplopia. Previous reports indicate that incidence of cranial neuropathies increases with age1, 5. However, diplopic elderly patients are often encountered in whom cranial neuropathies are implausible or have been ruled out.
Aging is also associated with a decrease in the range of ocular movements, particularly supraduction8. This phenomenon is caused by inferior displacement of the horizontal rectus extraocular muscle pulleys in the elderly as the pulley suspensions degenerate9. A decade ago, Rutar and Demer introduced the sagging eye syndrome (SES) as a form of strabismus caused by degeneration of the rectus pulley suspensions10. Magnetic resonance imaging (MRI) in SES demonstrates thinning of the lateral rectus-superior rectus band ligament, permitting inferior displacement of the lateral rectus pulley. When inferior displacements of lateral rectus muscle pulleys are similar in both eyes, SES presents as distance esotropia more than near; if inferior displacements differ in the two eyes, the presentation may include cyclovertical strabismus11. Clinical diagnosis of SES is based on motility patterns, and presence of age-related adnexal changes such as superior sulcus deformity, aponeurotic ptosis, and high lid crease. Since its initial description 10 years ago, SES has been increasingly recognized as a cause of acquired diplopia in adults.
Kawai et al.7 reported the causes of acquired diplopia in Japanese adults aged 60 years or older, based on review of 236 cases imaged with MRI. They considered three types of orbital pulley disorders: SES, heavy eye syndrome12, 13 and highly myopic strabismus14, 15. Kawai et al.7 reported that the most frequent cause of diplopia in these older in Japanese adults was orbital pulley disorder, causing 24.2% of cases. Except for Kawai et al., all other clinical studies of diplopia etiology were done before the recognition of the existence of SES. Therefore, we investigated the prevalence of SES in older adults who complained of acquired binocular diplopia in a population in the U.S.A.
Methods
Subjects.
We reviewed the medical records of new patients of age 40 years older who have presented at the Pediatric Ophthalmology and Strabismus Division of the Stein Eye Institute between January 2015 and December 2018 with the complaint of acquired binocular diplopia caused by strabismus. This study was approved by the Institutional Review Board of the David Geffen School of Medicine, University of California, Los Angeles, and followed the tenets of the Declaration of Helsinki.
Diagnostic criteria for Sagging Eye Syndrome.
We included two types of strabismus as SES: age-related distance esotropia (ARDE) with deviation angle greater at distance than near, or small angle cyclovertical strabismus with or without horizontal strabismus (CVS). ARDE was defined as symptomatic esotropia at distance, with orthophoria or asymptomatic esophoria of 10Δ or less at 33 cm near viewing distance. CVS was defined as a symptomatic vertical strabismus meeting the following criteria: 1) the hypotropic eye more excyclorotated than the hypertropic eye; 2) versions and/or Hess screen testing inconsistent with a classical superior oblique palsy (SOP) pattern such as significant under-depression in adduction and/or over-elevation in adduction; 3) difference in hypertropia with head tilting to the right and left shoulder 6Δ or less; and 4) absence of superior oblique muscle atrophy on MRI when available. Normal saccades were required, as were age-related external ocular adnexa findings such as superior sulcus deformity, aponeurotic ptosis, or high lid crease. We excluded other causes of strabismus such as thyroid ophthalmopathy, cranial nerve palsies, myasthenia gravis, childhood-onset strabismus, orbital trauma, and any types of restrictive strabismus, for example as resulting from scleral buckles, brachytherapy plaques, or glaucoma drainage devices.
Main Outcome Measures.
We recorded clinical factors including age, gender and cause of diplopia in all patients. We parsed patients into those with SES, versus those having other causes of diplopia (Others). Intergroup comparisons were performed for age and gender. In patients with SES, we recorded binocular alignment at distance (5m) and near (33cm) by the alternate prism cover test in primary position, as well as types of treatment received. We subdivided patient with SES into group with ARDE versus CVS using binocular alignment at first visit, and evaluated the surgical outcome of those who underwent strabismus surgery.
Statistical analyses.
Statistical analyses were performed using GraphPad Prism7 (GraphPad Software, Inc., La Jolla, CA, USA). Student’s t-test was used to compare age distributions and the chi-square test was used to compare gender differences. Paired t-testing was used to compare pre- and postoperative strabismus angles. The 0.05 level was considered statistically significant.
Results
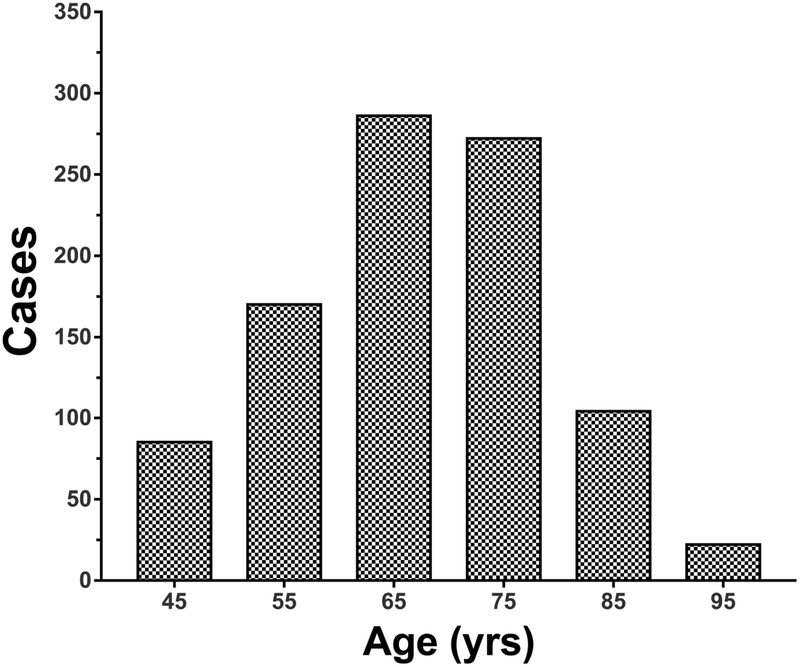
We identified a total of 945 patients over age 40 years newly presenting with diplopia caused by strabismus. Mean age at the initial visit was 66.5 ± 11.8 (Mean, SD) years. Most subjects were between 60 and 80 years of age (Fig. 1). There were 514 females (54.4%) and 431 males (45.6%).
Fig. 1:
Ages of patients presenting with acquired binocular diplopia.
Causes of Diplopia.
The most common cause of diplopia was SES, identified in 297 patients (31.4%). The second most common cause was trochlear palsy (10.3%) followed by thyroid eye disease (8.3%), mechanical strabismus due to implantation of devices such as scleral buckles, brachytherapy plaques, glaucoma drainage devices (7.2%), abducens palsy (6.9%), convergence insufficiency exotropia (5.1%), orbital fracture (3.3%), intermittent exotropia (2.5%), myasthenia gravis (2.1%), oculomotor palsy (1.9%), and decompensated esophoria (1.9%), childhood strabismus with surgery in child (1.7%), heavy eye syndrome (1.5%), sensory exotropia (1.4%), internuclear ophthalmoplegia (1.3%), decompensated exotropia (1.1%), childhood strabismus without surgery (1.0%), skew deviation (1.0%), consecutive exotropia (1.0%), consecutive hypertropia (0.8%), consecutive esotropia (0.8%), Duane’s syndrome (0.8%), nystagmus (0.8%), plus miscellaneous others (4.4%, Fig. 2).
Fig. 2:
Causes of diplopia. The most common cause of diplopia was sagging eye syndrome.
Age.
The average age of patients with SES was 71.2 ± 9.9 (SD) years, significantly older than the others group at 64.4 ±11.9 years (Fig. 3A: p< 0.0001). The relative proportion of SES among all patients increased with age (Fig. 3B). In patients aged 40–49 years, SES caused 4.7% of all diplopia, increasing to 19.3% in ages 50–59 years, 31.4% in ages 60–69 years, 41.8% in ages 70–79 years, 40.0% in ages 80–89 years, and 60.9% over age 90 years.
Fig. 3.
A: Age distribution of new patients presenting with acquired binocular diplopia. The average age of patient with sagging eye syndrome was 71 ± 10 (Mean ± SD) years. The average age of patients presenting with other causes of diplopia was 64±12 years (*** P< 0.0001). B. The proportion of diplopia due to sagging eye syndrome increases with age.
Gender.
There were 178 females (59.9%) and 119 males (40.1%) in SES group, representing a significantly greater female preponderance than the 337 females (52.0%) and 311 males (48.0%) in others group (p=0.023).
Strabismus Type in SES.
There were 104 (35.0%) patients with ARDE; these had 9.1 ± 0.6Δ (mean, SEM) mean esotropia at distance, but less than 1.6 ± 0.5Δ at near (Fig. 4). There were 193 (65.0%) patients with CVS; these had 3.9 ± 0.25Δ mean hypertropia and 3.8 ± 0.6Δ esotropia at distance, but there was no significant horizontal strabismus at near (Fig. 4). There was combined hypertropia and esotropia in 84 (28.2%) patients, and 109 patients (36.7%) had hypertropia alone.
Fig. 4:
Strabismus angle in two types of sagging eye syndrome. ARDE - age-related distance esotropia. CVS - cyclovertical strabismus with or without esotropia.
Treatment and Surgical Outcome in Sagging Eye Syndrome.
Patients who had small angle strabismus and wore spectacles for refractive necessity were offered the option of prism correction in lieu of strabismus surgery. Prism treatment was not a part of the diagnostic evaluation nor was its attempt required to establish eligibility for strabismus surgery. Prism spectacles were prescribed to 102 (34.3%) patients with SES (Fig. 5). However, patients to whom prism spectacles were prescribed often did not fill their prescriptions and instead opted for strabismus surgery without trying prismatic spectacles. Strabismus surgery was recommended as an alternative to prismatic spectacles in 178 (59.6%) patients with SES (Fig. 5); 149 (83.7%) of these underwent surgery. The combination of prismatic spectacles and strabismus surgery was generally not offered because surgeries were designed to be sufficient in themselves to alleviate diplopia.
Fig. 5:
Treatment of sagging eye syndrome.
Surgical approaches were individually chosen by the operating surgeons. In age-related distance esotropia, medial rectus recession was often chosen for surgical convenience since it is equally effective but more comfortably tolerated under topical anesthesia than lateral rectus resection27. Among the operated patients, 129 patients underwent one surgery, 16 patients had two surgeries, and 4 patients had three surgeries, giving a 13.4% re-operation rate. Esotropia was treated by medial rectus muscle recession in 56 patients, lateral rectus muscle resection or plication in 31 patients, combined medial and lateral rectus surgeries in 2 patients, equatorial lateral rectus myopexy in 2 patients and superior and lateral rectus myopexy in 1 patient. Vertical strabismus was treated by graded vertical rectus partial tenotomy (GVRT) in 64 patients and vertical rectus muscle recession/resection or plication in 24 patients. Some patients had both horizontal and vertical rectus surgery. Except for myopexy procedures, adjustable sutures were generally employed. Mean distance pre-operative esotropia was 6.9 ± 0.7Δ (mean, SEM), while mean hypertropia was 3.0 ± 0.3Δ. Mean distance post-operative esotropia and hypertropia at the latest follow up visit at 219 ± 256 (Mean, SD) days was 0.3 ± 0.3Δ and 0.7 ± 0.2Δ and, respectively. Surgery eventually resolved distance diplopia in all cases (Fig. 6). There were no post-operative adduction defects. Only one patient treated with bilateral medial rectus muscle recession developed post-operative convergence insufficiency requiring base-in prisms in her reading spectacles.
Fig. 6:
Strabismus angles before and after strabismus surgery for sagging eye syndrome. (*** P< 0.0001).
Discussion
To the authors’ knowledge, this is the first clinic-based prevalence study of causes of adult-onset diplopia to consider SES in the United States. Remarkably, SES was the commonest cause of diplopia, representing almost one third of all cases at 31%. The plausibility of SES as a cause of diplopia is supported by our finding that average age of patients with SES was significantly greater than for other causes of diplopia, and that the proportion of diplopia attributable to SES increases markedly with age. Similar to an earlier report, SES was more common in females than males11, and two-thirds of patients with SES had a vertical component of strabismus, either alone or with ARDE. Confirming and extending a prior report16, approximately 50% of SES patients were treated by strabismus surgery, which was successful with one operation in 87% of patients.
There are several epidemiological reports on strabismus in the elderly1–7. However, to our knowledge, only one from Japan that has heretofore considered SES as a cause of acquired diplopia7. Kawai et al.7 described orbital pulley disorders, including SES, heavy eye syndrome12, 13 and highly myopic strabismus14, 15, are the most common cause of acquired diplopia in Japanese persons over age 60 years, comprising about a quarter of all diplopia. This prevalence is lower than in the current study, representing a notable difference since the Japanese subjects were all over age 60 years, while our current study included subjects as young as age 40 years who have lower prevalence of SES. Martinez-Thompson et al.1 reviewed the causes of new-onset strabismus in adult patients over 19 years of age in Olmsted County, Minnesota during 20-year period from 1985 through 2004, an interval predating recognition of SES. Among the 753 cases of new onset adult strabismus in Olmstead County, the most common type of strabismus was paralytic (44.2%), followed by convergence insufficiency (15.7%), small-angle hypertropia (13.3%) and divergence insufficiency (10.6%). However, it is plausible that many cases of small-angle hypertropia and divergence insufficiency in the Olmsted study might have actually represented SES. Furthermore, some cases diagnosed as SOP might instead be SES, since the diagnosis was made using only the three-step test, which is now known to be only 70% sensitive and 50% specific17,18. Therefore, the Olmstead study is not inconsistent with the current one.
Many cases of SES presented with cyclovertical strabismus. The prevalence of CVS due to SES was 20.4% among all diplopic patients. Trochlear palsy was present in 10.3% of patients as the second most common cause of diplopia in our study. If we combine the groups with CVS due to SES, and the group with SOP, a vertical component of strabismus was present in about 30% of all diplopic adult patients. This is comparable to prevalence of vertical strabismus among the strabismic patients who were included in an epidemiological study of 1,214 Japanese community adult volunteers19. The prevalence of strabismus in the Japanese epidemiological study was 1.7%, of whom a third had vertical component. Therefore, it is important to recognize that SES can present not only as ARDE, but commonly also as CVS. It is highly possible that significant portion of the strabismus cases diagnosed as SOP in older epidemiological studies1–6 might actually have had SES.
The current study demonstrates that SES is more common in females, consistent with previous studies that showed female predominance in ARDE20, 21, 22. Our study showed 60% female predominance among patients with SES. Other studies have reported 69% to 85% of female predominance in ARDE, comparable to the current preponderance of 66%20, 21, 22. Female sex hormones such as progesterone and esotrogen are known to be important in maintaining collagen content by preventing the collagen degradation in women23,24. However, since levels of those hormones decrease after menopause,24 and the orbital pulley system is composed of collagen, elastin, and smooth muscle25, it would not be surprising for involutional changes in orbital connective tissues to be more common in females than males.
Various types of strabismus surgery can treat ARDE, including medial rectus weakening11, 16, 26, 27, lateral rectus tightening16, 26, 27, lateral rectus equatorial myopexy28, and superior and lateral rectus union myopexy13, 29. Chaudhuri and Demer recommend for ARDE that the target angle for correction by medial rectus muscle weakening be based upon twice the distance esotropia measured in the most affected horizontal gaze direction27. On the other hand, an increase in surgical dose is not required for lateral rectus plication/resection in ARDE27. Lateral rectus equatorial myopexy uses a permanent scleral suture to fixate the posterior lateral rectus belly into its correct anatomic position28. The muscle-to-muscle union of the superior and lateral rectus bellies was first described by Yokoyama to treat heavy eye syndrome13, but Morad et al. have used this procedure to treat ARDE, albeit with a 50% re-operation rate29. In the current study, initial surgery was medial rectus muscle weakening in 56 patients, lateral rectus muscle tightening in 31 patients, lateral rectus equatorial myopexy in 2 patients, and superior and lateral rectus myopexy in 1 patient. The overall re-operation rate was 13.4%. Given that the re-operation rate after superior and lateral rectus union myopexy in SES is high, conventional surgeries such as medial rectus recession (with augmented dosing)27 or lateral rectus tightening seem preferable for treating ARDE.
For the treatment of hypertropia in CVS, two procedures have been advocated: graded vertical rectus tenotomy (GVRT)16, 30, 31), and conventional vertical rectus muscle weakening or tightening16. GVRT, which corrects hypertropia up to 10Δ, is also less invasive than full tendon vertical rectus procedures16, 30. In the current study, patients with CVS averaged about 4Δ hypertropia, and 94% had hypertropia under 10Δ. Thus, GVRT was performed in 72% of CVS cases. It is fortunate that this minimally technique, which is preferably performed under topical anesthesia, is appropriate for the majority of patients with CVS.
There are few articles reporting surgical outcomes in SES32, 33, 16, 27. Outcomes of several different surgical approaches have been reported for ARDE: bilateral medial rectus recession32, 16, 27, bilateral lateral rectus resection or plication16, 27, and unilateral lateral rectus resection33. Every study has reported successful outcomes. Chaudhuri and Demer16 reported that SES recurred in 20% of patients following surgery after an average of 635 days. This follow-up period was longer than our mean follow-up of 219 days. Later recurrence therefore remains possible in the current patients.
In conclusion, SES is the most common cause of acquired diplopia in adults aged 40 years and older, representing about a third of all cases. While SES can be treated effectively by strabismus surgery, there may be later recurrences of diplopia.
Supplementary Material
ACKNOWLEDGEMENTS/DISCLOSURES
A. Funding/Support: Grants EY008313 and EY000331 from the US Public Health Service, National Eye Institute and an unrestricted grant from Research to Prevent Blindness to the Department of Ophthalmology. The sponsors or funding organizations had no role in the design or conduct of this research.
B. Financial Disclosures: Joseph L. Demer: National Eye Institute Grants EY008313 and EY029715, and an Unrestricted Grant to the UCLA Department of Ophthalmology from Research to Prevent Blindness. Stacy L. Pineles: National Eye Institute Grant R21EY029655. Soh Youn Suh: National Eye Institute Grant EY029715. The following authors have no financial disclosures: Toshiaki Goseki, Laura Robbins, Federico G. Velez.
C. Authorship: All authors attest that they meet the current ICMJE criteria for authorship.
D. Other Acknowledgments: None.
Funding/Support: This study was supported by grants to Joseph L. Demer from the U.S. Public Health Service (NEI grant EY008313), Washington, DC, and an unrestricted grant from Research to Prevent Blindness, New York, NY. The funding organization had no role in the design or conduct of this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meeting presentation: American Association for Pediatric Ophthalmology and Strabismus (AAPOS) Annual Meeting, March 30, 2019.
Conflict of Interest: No conflicting relationship exists for any author.
References
- 1.Martinez-Thompson JM, Diehl NN, Holmes JM, Mohney BG. Incidence, types, and lifetime risk of adult-onset strabismus. Ophthalmology 2014;121(4):877–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kobashi R, Ohtsuki H, Hasebe S. Clinical studies of ocular motility disturbances. Part 1. Ocular motility disturbances: causes and incidence. Jpn J Ophthalmol 1996;40(4):502–510. [PubMed] [Google Scholar]
- 3.Akagi T, Miyamoto K, Kashii S, Yoshimura N. Cause and prognosis of neurologically isolated third, fourth, or sixth cranial nerve dysfunction in cases of oculomotor palsy. Jpn J Ophthalmol 2008;52(1):32–35. [DOI] [PubMed] [Google Scholar]
- 4.Park UC, Kim SJ, Hwang JM, Yu YS. Clinical features and natural history of acquired third, fourth, and sixth cranial nerve palsy. Eye (Lond) 2008;22(5):691–696. [DOI] [PubMed] [Google Scholar]
- 5.Tamhankar MA, Biousse V, Ying GS, et al. Isolated third, fourth, and sixth cranial nerve palsies from presumed microvascular versus other causes: a prospective study. Ophthalmology 2013;120(11):2264–2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Sahn MF, Granet DB, Marvasti A, Roa A, Kinori M. Strabismus in Adults Older Than 60 Years. J Pediatr Ophthalmol Strabismus 2016;53(6):365–368. [DOI] [PubMed] [Google Scholar]
- 7.Kawai M, Goseki T, Ishikawa H, Hoshina M, Shoji N. Causes, background, and characteristics of binocular diplopia in the elderly. Jpn J Ophthalmol 2018;62(6):659–666. [DOI] [PubMed] [Google Scholar]
- 8.Clark RA, Isenberg SJ. The range of ocular movements decreases with aging. J AAPOS 2001;5(1):26–30. [DOI] [PubMed] [Google Scholar]
- 9.Clark RA, Demer JL. Effect of aging on human rectus extraocular muscle paths demonstrated by magnetic resonance imaging. Am J Ophthalmol 2002;134(6):872–878. [DOI] [PubMed] [Google Scholar]
- 10.Rutar T, Demer JL. “Heavy Eye” syndrome in the absence of high myopia: A connective tissue degeneration in elderly strabismic patients. J AAPOS 2009;13(1):36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaudhuri Z, Demer JL. Sagging eye syndrome: connective tissue involution as a cause of horizontal and vertical strabismus in older patients. JAMA Ophthalmol 2013;131(5):619–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tan RJ, Demer JL. Heavy eye syndrome versus sagging eye syndrome in high myopia. J AAPOS 2015;19(6):500–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yamaguchi M, Yokoyama T, Shiraki K. Surgical procedure for correcting globe dislocation in highly myopic strabismus. Am J Ophthalmol 2010;149(2):341–346 e342. [DOI] [PubMed] [Google Scholar]
- 14.Nakao Y, Kimura T. Prevalence and anatomic mechanism of highly myopic strabismus among Japanese with severe myopia. Jpn J Ophthalmol 2014;58(2):218–224. [DOI] [PubMed] [Google Scholar]
- 15.Kohmoto H, Inoue K, Wakakura M. Divergence insufficiency associated with high myopia. Clin Ophthalmol 2010;5):11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chaudhuri Z, Demer JL. Long-term Surgical Outcomes in the Sagging Eye Syndrome. Strabismus 2018;26(1):6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Demer JL, Kung J, Clark RA. Functional imaging of human extraocular muscles in head tilt dependent hypertropia. Invest Ophthalmol Vis Sci 2011;52(6):3023–3031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manchandia AM, Demer JL. Sensitivity of the three-step test in diagnosis of superior oblique palsy. J AAPOS 2014;18(6):567–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goseki T, Ishikawa H. The prevalence and types of strabismus, and average of stereopsis in Japanese adults. Jpn J Ophthalmol 2017;61(3):280–285. [DOI] [PubMed] [Google Scholar]
- 20.Ridley-Lane M, Lane E, Yeager LB, Brooks SE. Adult-onset chronic divergence insufficiency esotropia: clinical features and response to surgery. J AAPOS 2016;20(2):117–120. [DOI] [PubMed] [Google Scholar]
- 21.Mittelman D Age-related distance esotropia. J AAPOS 2006;10(3):212–213. [DOI] [PubMed] [Google Scholar]
- 22.Godts D, Mathysen DG. Distance esotropia in the elderly. Br J Ophthalmol 2013;97(11):1415–1419. [DOI] [PubMed] [Google Scholar]
- 23.Kanda N, Watanabe S. Regulatory roles of sex hormones in cutaneous biology and immunology. J Dermatol Sci 2005;38(1):1–7. [DOI] [PubMed] [Google Scholar]
- 24.Shah MG, Maibach HI. Estrogen and skin. An overview. Am J Clin Dermatol 2001;2(3):143–150. [DOI] [PubMed] [Google Scholar]
- 25.Kono R, Poukens V, Demer JL. Quantitative analysis of the structure of the human extraocular muscle pulley system. Invest Ophthalmol Vis Sci 2002;43(9):2923–2932. [PubMed] [Google Scholar]
- 26.Lim L, Rosenbaum AL, Demer JL. Saccadic velocity analysis in patients with divergence paralysis. J Pediatr Ophthalmol Strabismus 1995;32(2):76–81. [DOI] [PubMed] [Google Scholar]
- 27.Chaudhuri Z, Demer JL. Medial rectus recession is as effective as lateral rectus resection in divergence paralysis esotropia. Arch Ophthalmol 2012;130(10):1280–1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clark TY, Clark RA. Surgical correction of an inferiorly displaced lateral rectus with equatorial myopexy. J AAPOS 2016;20(5):446 e441–446 e443. [DOI] [PubMed] [Google Scholar]
- 29.Morad Y, Pras E, Nemet A. Superior and Lateral Rectus Myopexy for Acquired Adult Distance Esotropia: A “One Size Fits All” Surgery. Strabismus 2017;25(3):140–144. [DOI] [PubMed] [Google Scholar]
- 30.Chaudhuri Z, Demer JL. Graded vertical rectus tenotomy for small-angle cyclovertical strabismus in sagging eye syndrome. Br J Ophthalmol 2016;100(5):648–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brooks SE, Habib L. Graded Marginal Recession: A Surgical Technique to Correct Small Angle Vertical Deviations. J Pediatr Ophthalmol Strabismus 2016;53(2):85–89. [DOI] [PubMed] [Google Scholar]
- 32.Mittelman D Surgical management of adult onset age-related distance esotropia. J Pediatr Ophthalmol Strabismus 2011;48(4):214–216. [DOI] [PubMed] [Google Scholar]
- 33.Yadav S, Young J, Voas-Clarke C, Marsh IB, Durnian JM. Treatment of age-related distance esotropia with unilateral lateral rectus resection. J AAPOS 2014;18(5):446–448. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.