Abstract
Background:
Pilomyxoid astrocytoma (PMA) is a variant of pilocytic astrocytomas but exhibits more aggressive behavior. Further, it is more prevalent in the hypothalamic/chiasmatic regions and is only rarely encountered in the thoracic spine.
Case Description:
A 9-year-old male presented with severe spastic paraparesis (motor/sensory) attributed to a thoracic cord PMA and scoliosis. The magnetic resonance (MR) showed an intraaxial ill-defined expansile lesion with heterogeneous enhancement extending from the cervicothoracic junction to conus medullaris. A multilevel decompressive laminectomy was performed with restricted tumor debulking; an expansile duraplasty was also effected. Two years later, the patient has moderately improved and has not shown any symptom progression.
Conclusion:
We recommend the early performance of a thoracic MR in children with idiopathic scoliosis presenting with the onset of a significant spastic paraparesis.
Keywords: Magnetic resonance imaging, Pilomyxoid astrocytoma, Radiotherapy, Scoliosis, Spinal cord, Thoracic

BACKGROUND
Intramedullary pilomyxoid astrocytoma (PMA) is a variant of pilocytic astrocytoma (PA).[2,5,6] That is categorized as the WHO Grade 2.[6] However, PMA is more aggressive than PA and is usually located within the spinal cord of younger patients.[9] The treatment options for PMA include surgical resection which is often limited to debulking (e.g., extent restricted to minimize neurological deficit) followed by radiotherapy with or without chemotherapy.[5,10] Here, we are presenting a 9-year-old with a thoracic PMA and scoliosis who successfully underwent laminectomy with partial tumor debulking/resection plus duraplasty and exhibited an adequate 2-year postoperative neurological outcome.
CASE PRESENTATION
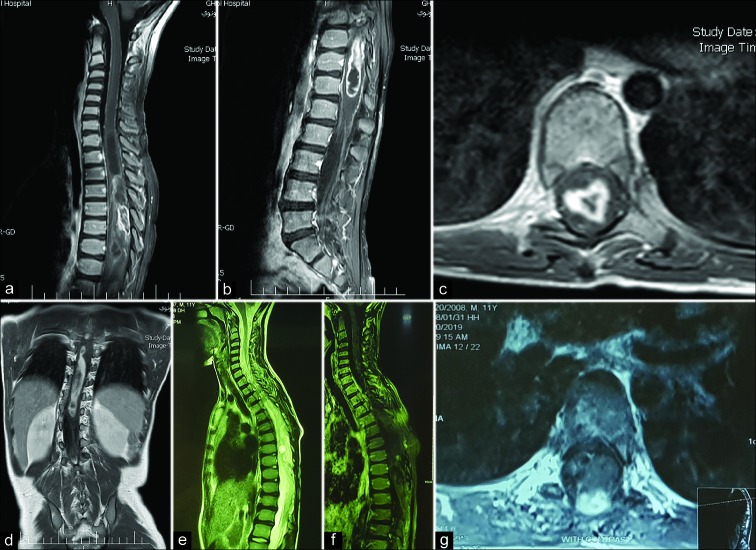
A 9-year-old male with spinal scoliosis recently diagnosed/brace (e.g., 1 month’s duration) presented with a severe motor/sensory spastic paraparesis. The holospinal magnetic resonance (MR) revealed an intraaxial/intramedullary ill-defined expansile lesion with heterogeneous enhancement extending from the cervicothoracic junction to conus medullaris [Figure 1].
Figure 1:
Preoperative magnetic resonance imaging (MRI) with gadolinium showed an expansile intramedullary tumor of thoracic cord and conus medullaris with irregular heterogeneous enhancement and some cystic changes on sagittal (a and b) and axial (c) views in a 9-year-old patient with severe thoracolumbar scoliosis (d). After surgical treatment, 2 years follow-up MRI reveals an evidence of minimal cord herniation toward laminectomy sites and intramedullary cystic changes (sagittal T2 sequence), (e) with minimal enhancement on sagittal (f) and axial (g) views.
He underwent a T5-T11 laminectomy with tumor debulking (e.g., poor plane between tumor/cord) followed by expansile duraplasty. Postoperatively, he exhibited significant improvement of the paraparesis. As the histopathological exam showed a PMA, adjuvant therapy included spinal radiation [Figure 2]. Two years later, the patient improvement has continued and the follow-up MR showed no further progression [Figure 1].
Figure 2:
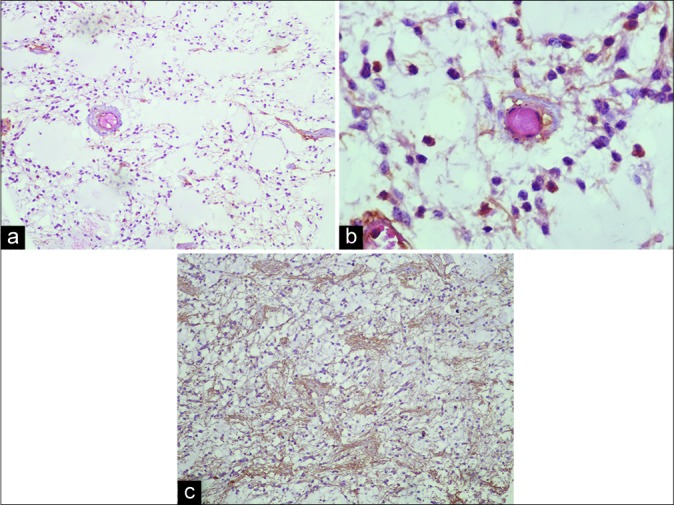
This shows histopathology of resected tumor. We could see hypocellular glial tumor, in which monomorphic piloid tumor cells are dispersed in a myxoid matrix (Hematoxylin and Eosin stain, ×100) (a). Furthermore, tendency of piloid perivascular cells to form a rosette-like structure without any Rosenthal fiber could be seen (Hematoxylin and Eosin stain, ×400, b). (c) Reveals a strong immunoreactivity of the tumor cells for glial fibrillary acidic protein (GFAP immunostaining, ×100, c).
DISCUSSION
PMA is the more aggressive type of astrocytoma that usually seen in child <4-year-old age and in hypothalamic/chiasmatic region.[8,9] PMA in spinal cord region is rare in the thoracic cord; this case is the tenth reported in the literature [Table 1].
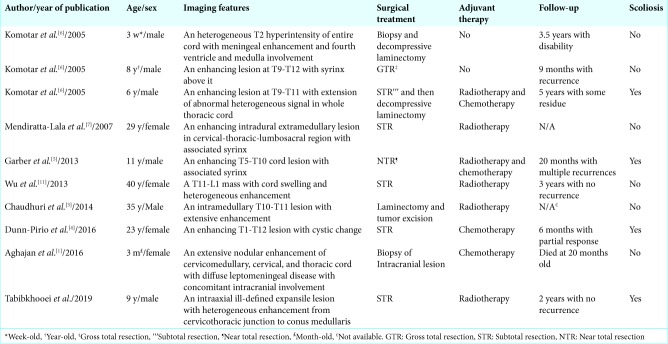
Table 1:
All reported cases of pilomyxoid astrocytoma of thoracic spine in the literature.
On imaging, we have no any distinct criteria for differentiation of PA from PMA.[6,7] However, histological findings include; a mucopolysaccharide matrix with monomorphic piloid cells, the absence of Rosenthal fibers, biphasic architecture, and eosinophilic granular bodies.[5,6]
Usually, in cases of intramedullary astrocytoma, we recommend only debulking the center of tumor (e.g., not beyond the ill-defined border between tumor/normal tissue), and then performing an expansile duraplasty, if indicated.
The addition of adjuvant radiation therapy is controversial. Many clinicians recommend safe surgical resection of the tumor followed by both radiotherapy and chemotherapy to improve survival.[5,10] In this case, the patient did receive radiation.
CONCLUSION
We present the rare case of a 9-year-old with a PMA of the thoracic cord and scoliosis who was effectively treated with a T5-T11 laminectomy, tumor debulking, duraplasty, and later adjuvant radiation therapy.
Footnotes
How to cite this article: Tabibkhooei A, Sadeghipour A, Fattahi A. Thoracolumbar pilomyxoid astrocytoma with spinal scoliosis: A case report and literature review. Surg Neurol Int 2019;10:235.
Contributor Information
Alireza Tabibkhooei, Email: tabibkhooei.a@iums.ac.ir.
Alireza Sadeghipour, Email: sadeghipour.alireza@gmail.com.
Arash Fattahi, Email: fatahi.a@iums.ac.ir.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Aghajan Y, Levy ML, Newbury RO, Crawford JR. Disseminated pilomyxoid astrocytoma in infancy with novel MUTYH mutation. BMJ Case Rep. 2016;2016:bcr2016217764. doi: 10.1136/bcr-2016-217764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bouaziz MC, Daghfous MS, Ladeb MF. Childhood scoliosis revealing spinal cord tumors. Eur Orthop Surg Traumatol. 2006;16:318–21. [Google Scholar]
- 3.Chaudhuri T, Jadava K. Pilomyxoid astrocytoma of the thoracic spinal cord in an adult: A case report and review of literature. Clin Cancer Invest J. 2014;3:329. [Google Scholar]
- 4.Dunn-Pirio AM, Howell E, McLendon RE, Peters KB. Single-agent carboplatin for a rare case of pilomyxoid astrocytoma of the spinal cord in an adult with neurofibromatosis Type 1. Case Rep Oncol. 2016;9:568–73. doi: 10.1159/000449406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garber ST, Bollo RJ, Riva-Cambrin JK. Pediatric spinal pilomyxoid astrocytoma. J Neurosurg Pediatr. 2013;12:511–6. doi: 10.3171/2013.8.PEDS1397. [DOI] [PubMed] [Google Scholar]
- 6.Komotar RJ, Carson BS, Rao C, Chaffee S, Goldthwaite PT, Tihan T. Pilomyxoid astrocytoma of the spinal cord: Report of three cases. Neurosurgery. 2005;56:191. doi: 10.1227/01.NEU.0000146212.95421.B3. [DOI] [PubMed] [Google Scholar]
- 7.Mendiratta-Lala M, Kader Ellika S, Gutierrez JA, Patel SC, Jain R. Spinal cord pilomyxoid astrocytoma: An unusual tumor. J Neuroimaging. 2007;17:371–4. doi: 10.1111/j.1552-6569.2006.00101.x. [DOI] [PubMed] [Google Scholar]
- 8.Samartzis D, Gillis CC, Shih P, O’Toole JE, Fessler RG. Intramedullary spinal cord tumors: Part I-epidemiology, pathophysiology, and diagnosis. Global Spine J. 2015;5:425–35. doi: 10.1055/s-0035-1549029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tihan T, Fisher PG, Kepner JL, Godfraind C, McComb RD, Goldthwaite PT, et al. Pediatric astrocytomas with monomorphous pilomyxoid features and a less favorable outcome. J Neuropathol Exp Neurol. 1999;58:1061–8. doi: 10.1097/00005072-199910000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Tobin MK, Geraghty JR, Engelhard HH, Linninger AA, Mehta AI. Intramedullary spinal cord tumors: A review of current and future treatment strategies. Neurosurg Focus. 2015;39:E14. doi: 10.3171/2015.5.FOCUS15158. [DOI] [PubMed] [Google Scholar]
- 11.Wu L, Yang T, Yang C, Xu Y. Primary pilomyxoid astrocytoma of the thoracolumbar spinal cord in an adult. Neurol India. 2013;61:677–9. doi: 10.4103/0028-3886.125376. [DOI] [PubMed] [Google Scholar]