Abstract
Objective
The purpose of this commentary is to discuss the philosophical and hypothetical underpinnings of chiropractic and consider whether there is a need for chiropractic to have a questioning philosophy and theory-driven process to guide future scientific endeavors in the profession.
Discussion
The earliest beliefs of the chiropractic founders centered on chiropractic vertebral subluxation but differed on whether this was a static, bone-out-of-place misalignment or a lesion whereby joints had lost their normal direction or range of motion. More recently, new hypotheses such as dyskinesia, inflammation, and neuroplasticity attempt to explain the purported clinical effects of chiropractic. Yet practitioners and students advocate for both traditional viewpoints that typically tout misalignment and embrace a science of chiropractic. I propose that chiropractors should not have to choose between philosophy and science. Instead, they should advocate for adoption of a modern questioning philosophy that not only informs their clinical questions and drives their theories, but also that is in turn influenced by outcomes from their research. Such a questioning philosophy is in stark contrast with the dogma that some have mislabeled as “philosophy” in the profession. I recommend that a review of chiropractic hypotheses and a theory-driven research process is needed to help guide the profession’s research agenda given its wide range of clinical activities and limited resources. As the chiropractic profession increasingly embraces evidence-informed practice, enhanced integration within the wider health care community may then result in further gains in utilization.
Conclusion
Theory-driven research that results from and subsequently informs a questioning philosophy may expose truths related to practice behaviors, activities, and outcomes, and spur more complete integration of chiropractic within the wider health care community.
Introduction
Now more than ever before, people are using chiropractic care as their first choice for back pain treatment.1,2 This is an increase in utilization compared with findings from less rigorous survey studies performed in the past decades.1, 2, 3 In this era, patients are going to chiropractors regardless of what type of technique the chiropractor is using (eg, looking for a short leg, CVS [chiropractic vertebral subluxation], or dyskinesia with inflammation). The profession is now celebrating its 125th anniversary, and I wonder if there is a role for a questioning philosophy and theory-driven process to guide future scientific endeavors in the profession?
Therefore, the purpose of this commentary is to review the philosophical and hypothetical underpinnings of chiropractic and discuss if there is a need for chiropractic to have a questioning philosophy and theory-driven process to guide future scientific endeavors in the profession.
Discussion
Early Theories
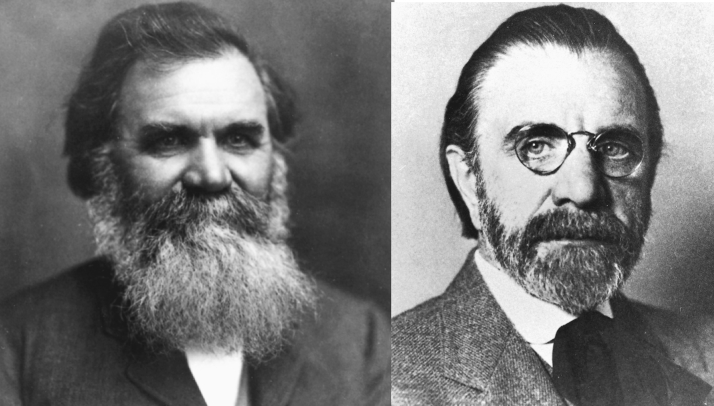
The founding father of chiropractic, D. D. Palmer, and his son B. J. Palmer (Fig 1), purported that bones out of place in the spine were the cause of dis-ease (ie, misalignment hypothesis), along with accidents and poisons.4,5 D. D. Palmer did not initially use the term subluxation to describe spinal lesions, but instead by 1902 was reporting in issue 29 of The Palmer School’s The Chiropractic that “ . . . if any part is found out of place adjust it . . . “6 In the same issue appears the testimony of C. C. Gardner, assistant ticket agent at the C.R.I.& P. Depot in Davenport, Iowa, who wrote that Palmer described his wife’s problem: “ . . . the cause of all her trouble was a luxation in a lumbar vertebra . . . wrenched enough so that there was pressure on those nerves which gave her so much pain.”6 So in Palmer’s early writing, he advocated both bone-out-of-place “luxation” and nerve pressure to explain the spinal lesions chiropractors treated, but did not initially use the term subluxation.7
Fig 1.
Founder of chiropractic D. D. Palmer (left) and son B. J. Palmer.
Subluxation as a Fixation
One of Palmer’s first students, Oakley Smith, DC, coined the term subluxation to describe the lesion chiropractors treat, and by fall 1906 he and 2 other graduates of the Palmer School, Solon Massey Langworthy and Minora Paxson, wrote the first chiropractic textbook, Modernized Chiropractic (Fig 2).8 However, their definition—as opposed to the simple misalignment hypothesis—focused on restricted motion within the joint’s normal end range, providing support for the modern fixation hypothesis: “A simple subluxated vertebra differs from a normal vertebra only in its field of motion and the center of its field of motion. . . .”9
Fig 2.
Oakley Smith (left), Solon Massey Langworthy (center), and Minora Paxson wrote the first chiropractic textbook and were the first to write about subluxation.
By 1910, D. D. would write his massive The Chiropractor’s Adjuster and formally adopt Smith’s term subluxation.4 Although in subsequent writings both Palmers permanently embraced Smith’s subluxation term, they both rejected the early fixation hypothesis of Langworthy-Smith-Paxson. By 1919, B. J. Palmer reported why the Palmer School had adopted x-rays as part of chiropractic assessment of spinal lesions: “We had already settled how a cure occurred; we did not care much about pathological plates . . . the advent of the X-Ray into Chiropractic was to prove that vertebral subluxations did actually exist. . . . ”[emphasis original]10
B. J. Palmer’s decision to support the misalignment hypothesis over the fixation hypothesis had an impact on the future course of chiropractic. Of the 23 chiropractic adjustment techniques, 20 (ie, 14 of 16 upper cervical and 6 of 6 full spine techniques) originated from this early emphasis.10 Both upper cervical and full spine techniques subsequently developed different philosophical approaches; however, 1 group initially favored the simplistic misalignment hypothesis and for decades ignored the more complicated fixation hypothesis.10
For the next 60 years, the competing chiropractic national organizations engaged in debates regarding the scope of practice, but rarely was misalignment hypothesis, let alone the very existence of CVS, challenged by chiropractic leaders or scientists. A plethora of subluxation hypotheses were developed by a number of chiropractors during that time, most of whom developed a treatment technique during this period, and a few advocated for serious scientific inquiry into the profession’s foundations and core beliefs.11,12 Yet a serious research enterprise did not exist until the 1970s.
Modern Science for Chiropractic Begins in 1972
An event that spurred development of research in chiropractic occurred as a result of Congress including chiropractic adjustment as a covered service in the US Medicare program in 1972.13 This inclusion led to a radiographic and clinical operational definition of CVS. The recognition of the Council on Chiropractic Education in 1974 as the sole chiropractic accrediting agency recognized by the US Office of Education led to more faculty members at US chiropractic schools having degrees in science as a prequalification to teaching science coursework.14, 15, 16 A second event occurred with federal funding for a multidisciplinary conference to review the status of spinal manipulation in 1976. The resulting scientific monograph, from the National Institutes of Neurological Diseases and Stroke (NINDS) conference,17 included a paper by Joseph Janse, DC, then president of the National College of Chiropractic, that outlined many major hypotheses chiropractors or scientists had held regarding spinal manipulation, leading to their publication and widespread dissemination for the first time.18
A third event was the creation of the first-ever peer-reviewed chiropractic scientific journal in 1978 that was also fully indexed in Index Medicus, the Journal of Manipulative and Physiological Therapeutics.19,20 An increasing number of students would be taught not merely by other chiropractors but by academics and scientists, who would also contribute research to scrutinize chiropractic hypotheses and contribute to the development, publication, and debate regarding practice guidelines.21, 22, 23 In the Journal of Manipulative and Physiological Therapeutics, chiropractors would see publication of studies ranging from quasi-experimental research designs to clinical analog investigations and from randomized clinical trials (RCTs) to meta-analyses and the development of evidence-based treatment guidelines by scientists and peers. Moreover, some chiropractors were for the first time supporting and adopting the principles and practices of science as had other health care professionals.
Subsequent to these events and possibly as a direct result of them, a rich research culture began to develop in the United States for the first time, promoting evidence-informed practice that included, for example, development of the Association of Chiropractic Colleges, International Conference on Spinal Manipulation, and later Research Agenda Conference Meetings, where scientists would begin to debate not just research findings from their studies, but the very philosophies that underpinned chiropractic practice.19,24, 25, 26, 27, 28, 29, 30
Does a Health Care Profession Need Philosophy?
Chiropractic is not the only health care profession that struggles with its diversity of viewpoints and opinions, and certainly its members are not the first to opine regarding whether there is a need for a philosophy. As pointed out recently, the Nobel Laureate in 1965 for quantum physics, Richard Feynman, purportedly stated that “philosophy of science is as useful to scientists as ornithology is to birds. No matter, or even in spite of, the theories of the former, the latter can fly all too well.”31 Notwithstanding the protestations of Feynman and other scientists, Andreoletti and Maugeeri31 point out that philosophy done right can be beneficial to the field of medicine. Professor Sir Karl Popper’s philosophical observation that no theory is ultimately provable led to falsification, which has subsequently provided the overarching framework for modern biomedical research. For chiropractic authors such as Charlton,32 the current purported philosophical discourse in chiropractic is hardly being accomplished in the correct arena, by professors of philosophy trained in philosophical discourse, representing the various chiropractic colleges. Instead, he offered that “The obfuscation of the issue of philosophy as if there is an entity called “Chiropractic Philosophy,” when there probably is not, is a major impediment to clarity of thinking in chiropractic. . . . “ As Senzon11 so aptly points out, chiropractic’s founder D. D. Palmer’s aim was in some ways neo-Kantian in his vision and reflected attempts to unite disparities found in modernity, including specifically “science, art, and philosophy as well as body, mind, soul, and spirit in his definition of chiropractic.”11
Yet the inclusion of spirit and soul into Palmer’s definition of chiropractic set the stage for traditionalists who advocated for concepts such as CVS and the spine as the center of good health as opposed to others who argued for practice that focuses on musculoskeletal problems with or without a philosophy; it may be further complicated by groups within both camps that advocate for evidence-based techniques and treatments, as opposed to others who seemingly ignore the clinical application of knowledge gained by scientific research.22,28,33, 34, 35
Scientists in other health professions36 point out that philosophy should guide the process of research rather than be detached from it. For example, in the nursing profession, Ivey points out that the philosophical view of the research method chosen may dictate use of a phenomenological theoretical approach. She offers that qualitative methods may reveal answers to research questions that traditional outcomes and data-driven studies are not designed to detect, apt for fields like nursing, psychology, and other health science research. In the field of nutrition, scientists wrote of the philosophy of evidence-based principles and practice in nutrition as hinging on 3 fundamental principles: (a) understanding the best available evidence; (b) how to decide the relative trustworthiness of evidence; and (c) in addition to evidence, considerations must always include a tradeoff between potential benefits and risks, burden, and costs associated with alternative treatments and strategies, considering each patients’ perspective, values, and preferences.37 Further, in writing about the international Choosing Wisely movement and its success, Bobbio and Vernero38 discussed its philosophy (summarized in their campaign slogan “Doing more does not mean doing better . . . “) and application in Italy. This philosophy was used to improve clinical appropriateness by reducing unnecessary tests and treatments and increase the dialogue between physicians and patients. It now includes 44 societies of physicians, nurses, pharmacists, and physiotherapists that “identified 230 recommendations about tests, treatments and procedures commonly used in Italy’s clinical practice that do not provide any benefit to most patients but may cause harm.” They concluded that this philosophy had helped shape their approach to improving health care in Italy and serves as an example for how a philosophy can help to guide a health care profession and its practices.
Influence of Traditional Chiropractic Philosophy on Research
A growing number of chiropractors embrace scientific inquiry informing their practice activities, yet others eschew scientific knowledge that does not harmonize with their philosophy.39 Hence, although both the statements and practice activities of chiropractors support nearly all of the US Centers for Disease Control Healthy People goals, including exercise advice and training for patients, there are some who choose to go against these recommendations. For example, a study of Canadian chiropractors showed that a few practitioners continue to disparage immunization as a public health measure. It is believed that the reason for this is that it runs counter to their stated philosophy.40,41 Scientists refer to such philosophical inflexibility as dogma, unacceptable to the wider health care community.41,42
Certainly for the chiropractic profession, Keating33,43 stated that although subluxation syndrome (ie, a lesion that may cause spine pain) can yield testable hypotheses, the subluxation hypothesis (ie, that a spine lesion may be the cause of all dis-ease) is largely untested:
The dogma of subluxation is perhaps the greatest single barrier to professional development for chiropractors. It skews the practice of the art in directions that bring ridicule from the scientific community and uncertainty among the public. Failure to challenge subluxation dogma perpetuates a marketing tradition that inevitably prompts charges of quackery. . . . Commitment to this dogma undermines the motivation for scientific investigation of subluxation as a hypothesis, and so perpetuates the cycle.33
As Keating points out, the inflexibility of holding to subluxation hypothesis may be one of the main barriers to scientific validation of any aspect of it, and that continuing traditional chiropractic philosophy (for example, research performed to prove the effects of CVS) may create a barrier to the acknowledgment of truths that would otherwise be revealed by research committed to falsification. For example, research could be performed to determine whether leg check outcomes vary directly or indirectly with improvement with other purported mediator and outcome variables of subluxation, such as pressure pain thresholds and Oswestry disability.44,45 The textbook of chiropractic theory that I wrote included a 9-step process needed to determine the validity of any subluxation hypothesis. There may be only a few of which have been accomplished to date for any particular hypothesis.46 Hence, although research by advocates of traditional chiropractic philosophy may accept the research findings that support some aspects of their practice, such as for the treatment of acute or chronic neck or back pain or headaches, they may reject research that questions routine use of x-ray to detect misalignments because not x-raying every patient may run counter to their core beliefs and philosophy. The recent review of subluxation hypotheses from the founding of the profession to the modern era authored by Senzon11,12,47, 48, 49, 50, 51, 52, 53, 54 underscores a problem. Most of the reference citations used in this historical treatise are supported by little clinical validity research.
Further complicating the question of traditional chiropractic philosophy is the conundrum that practitioners and students appear to support both traditional chiropractic philosophy and evidence-informed practice. A recent survey of North American chiropractic students found they support evidence-based practice and a role for chiropractic to eliminate vertebral subluxation/vertebral subluxation complex. As the authors suggest, “These two key points may seem contradictory, suggesting cognitive dissonance.”1 One may ask how can traditional chiropractic philosophy adapt if it is confronted with clinical research that runs counter to its core precepts, such as x-rays to detect misalignment, subluxation that triggers abnormal nerve flow, and correction of the cause of all dis-ease, as opposed to immunization and antibiotics to prevent and control infectious disease?
Role of a Questioning Philosophy in Guiding Research
Most if not all of the US chiropractic colleges claim to be officially committed to evidence-based chiropractic. At least that was the opinion of Robert Cooperstein55 when he discussed the merger of the research and technique departments at the Palmer West Chiropractic College:
Scientifically based chiropractic professors should not rant and rave about “The Subluxation” and “The Adjustment”; good science by its very nature automatically desanctifies the standard totems. . . . Likewise, it is more difficult to promote generic technique than brand-name techniques, which bear the stamp of the guru and the insignia of religious conviction. . . . This powerful trend should act as a mandate to the colleges and the journals to reconcile clinical chiropractic and clinical uncertainty.55
As Cooperstein55 recounted the difficulties of merging the 2 departments, he wrote of the pre-merger experience as one in which technique instructors felt research faculty lived in ivory towers without practical clinical experience, and that research faculty had basically concluded technique instructors were clueless about research findings. In contrast, the Palmer West post-merger era is one in which technique and research faculty often attend the same conferences, work on the same papers, and have shared experiences with more camaraderie.
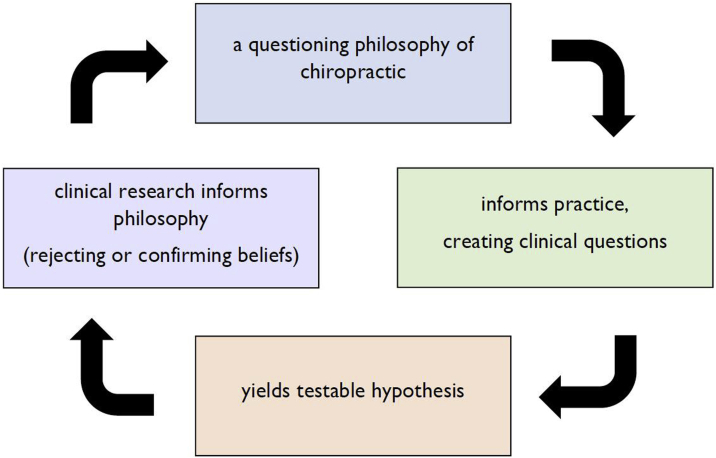
The experience at Palmer-West shows an example that chiropractic does not need to choose between the use of chiropractic techniques based upon traditional chiropractic philosophy and the philosophy of evidence-informed application of chiropractic techniques. In other health care professions, philosophy helps inform clinical practices and yields testable hypotheses that when studied reinform the philosophy that had inspired the research (Fig 3). Keating advocated for such a critical thinking approach for development of a philosophy of science within the chiropractic profession,56 while Charlton32 spoke of a new questioning approach to replace “rumination and rhetoric,” instead advocating for philosophy as a tool to better understand our practice and guide research.
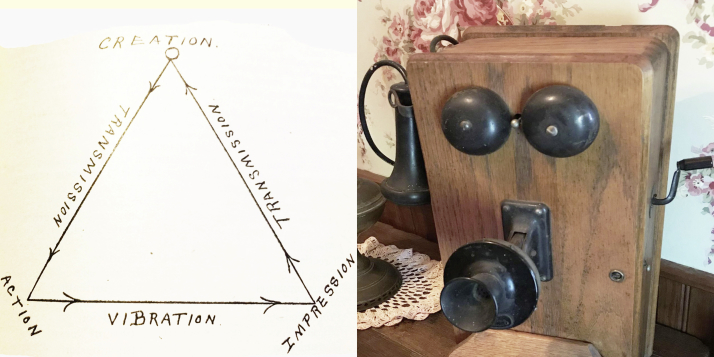
Fig 3.
A questioning philosophy of chiropractic can lead clinicians in their search for answers derived from clinical practice.
Senzon57 refers to Leach and Reed58 in addition to Keating59 as dismissivists for advocating separation of all “premodern” traditional philosophy, including innate and universal intelligence, from development of clinical questions, testable hypotheses, and scientific processes vis-à-vis an empirical worldview based on scientific materialism: “And yet, with any attempt to update, revise, and evolve the philosophy of chiropractic, there is always the danger of dogmatic thinking, scientism, and dismissivist approaches based on limited perspectives, methods, and worldviews.”57
He instead advocates for application of integral pluralism as a method for constructing a philosophy of chiropractic to overcome the obstacle of limited perspectives, since it “ . . . developed as a late-postconventional approach to all known forms of knowledge acquisition and interpretation, is congruent with chiropractic’s original early postconventional approach and ideal to assist the chiropractic profession to evolve its worldviews for the 21st century.”57 Senzon suggests that it would be a backward step for chiropractic to abandon its “more comprehensive approach to life and reality” with its mind-body-spirit emphasis57 even as American society is embracing these holistic approaches.3,57
Scientists in other fields continue to embrace philosophy and spiritual implications of their work to develop testable hypotheses and refine their philosophies and theories. Examples of this include Wernher von Braun, NASA engineer and designer of the Saturn rockets that propelled man to the moon, and more recently Nobel Peace Prize–winning physicist and self-professed Christian William Phillips, who stated:
I see an orderly, beautiful universe in which nearly all physical phenomena can be understood from a few simple mathematical equations. I see a universe that, had it been constructed slightly differently, would never have given birth to stars and planets, let alone bacteria and people. And there is no good scientific reason for why the universe should not have been different. Many good scientists have concluded from these observations that an intelligent God must have chosen to create the universe with such beautiful, simple, and life-giving properties. Many other equally good scientists are nevertheless atheists. Both conclusions are positions of faith.60,61
If the study of physics can include mind-body-spiritual considerations and implications, then perhaps chiropractors and their patients, who come from all walks and faiths, including both Christians and atheists, can do the same. Allowing for a questioning philosophy of chiropractic that embraces mind-body-spirit including a role for prayer, while advocating for scientific inquiry to further inform that philosophy, would support those students and doctors who want both traditional philosophy and evidence-based practice. But how might a questioning philosophy be put into practice in chiropractic?
Leaders and philosophers who advocate for traditional chiropractic philosophy should acknowledge a role for science in informing and, when indicated, amending the profession’s core beliefs. I suggest that they should refrain from doing research to prove subluxation exists or to prove adjustments work. They should not rigidly hold on to scientifically unsupported concepts such as the safety pin cycle and misalignment hypothesis that are clinically informed by leg checks and x-rays. Instead, they should consider a philosophy that acknowledges chiropractic has wellness benefits beyond back pain that could inspire its advocates to ask their institutions to follow up on recent evidence. For example, chiropractic manipulation (adjustments) may result in lower inflammatory cytokines (eg, nitrous oxide, interleukin 1, and interleukin 6) and increased anti-inflammatory biomarkers (ie, interleukin 10).62 Confirmation of an anti-inflammatory effect of SM might have profound whole health implications that would be recognized by other health care professions, media, and the public.62 Similarly, chiropractic institutions with a philosophy that nerve balance can only be restored by use of specific adjustments could support research to determine whether the new findings of neuroplastic changes after chiropractic are more robust in patients receiving chiropractic adjustments based on specific radiographic measurements (eg, x-ray listings) as opposed to cohorts that received only nonspecific diversified adjustments without benefit of x-ray listings.63,64 Such research could test the misalignment hypothesis and offer evidence for or against the necessity for chiropractors using x-ray listings. On the other hand, should a body of research fail to support the usefulness of x-ray listings, at some point evidence-based chiropractors must be willing to abandon x-ray markings as a meaningful clinical tool to detect spinal lesions absent red flags for disease. If this were the case, they should instead incorporate scientifically supported measures into their practices. These may include tests for pain provocation, compliance, pressure pain thresholds, or disability questionnaires for which there is growing clinical validation.65, 66, 67, 68, 69, 70 Embracing new information not only would drive the profession toward more evidence-informed practice, but also could help to integrate chiropractic more seamlessly into the health care system.71
Does a Health Care Profession Need Theories?
Historically, a number of reasons have been offered for why chiropractors cannot or need not try to do research. Traditional chiropractic philosophy points to the CVS as the cause of dis-ease in the body and the chiropractic adjustment as its only remedy.72 Tonelli and Callahan73 sympathize with traditional chiropractors and suggest that complementary and alternative medicine (CAM) cannot be evidence-based. They propose that the methods for obtaining knowledge in chiropractic must be coherent with our profession’s paradigm and theories. They posit further that because CAM practices focus on the health of a particular individual, quantitative methods and population-based research may not be the ideal approach for assessing benefits of chiropractic practice. However, they only allow that CAM practices like chiropractic should not have to be evidence based, at least by the current narrow definition (ie, by use of the gold standard meta-analysis of randomized controlled trials). They propose that instead of clinical controlled trials and other quantitative approaches, development of knowledge should proceed through alternative epistemological approaches more germane to these professions. Since the writing of their paper, chiropractic scientists have already moved beyond their question, producing provocative basic science and clinical research, publishing in both chiropractic and nonchiropractic biomedical journals, on subjects ranging from rat models of dyskinesia to public health studies, and from randomized clinical studies of the effects of spinal manipulation on response of inflammatory cytokines to altered neuroplastic phenomena measured by somatosensory evoked potentials.64,74, 75, 76
Other fields of biological and clinical sciences regularly use hypothesis development and theory as tools to advance their domains. Longo and Soto77 argue that theories organize knowledge and construct objectivity in the field of biology, for example, by focusing on the specific organisms, the individuals, as they undergo constant change. They consider that humans continue to refer to “sunrise” and “sunset” nearly half a millennium after Copernicus determined the notion of a heliocentric planetary system—and that we are exposed to this information regarding the earth’s rotation around the sun since childhood—as support for the words of Dennett: “There is no such thing as philosophy-free science; there is only science whose philosophical baggage is taken on board without examination.”77 They advocate for hypothesis development and theories to explain observed phenomena. Others such as Camargo and Medina78 point out that medicine may not be quite as scientific as it purports to be in clinical practice, especially if it is good medicine for the individual. Hence, even when armed with powerful biological “weapons” in the care of individual patients in medical practice—just as chiropractors argue for their practices—clinicians necessarily are unable to always adhere to a strict systematic set of rules presupposed by the words scientific medicine. In other words, hypotheses and theories cannot yet explain every outcome, let alone dictate the course every clinician should take for every patient. Indeed, the struggle for use of theory to organize knowledge has been reported by medical doctors with regard to Chinese medicine and acupuncture,79 by social scientists advocating for “a broader conceptualization of theory that reaches across disciplines,”80 by public health scientists arguing for epidemiological theories that expose power and unjust social relations as producing health inequities,81 and by psychologists looking for unifying theories that explain the role of physician-initiated empathy on the role of healing.82 The debates over use of philosophy and theory extend well beyond the borders of chiropractic and this brief discussion. That said, it is clear from the majority of authors that proper use of these disciplines may, notwithstanding their limitations, inform both our clinicians and their patients, and ultimately help improve care outcomes.
Were the Medical Theorists Right? Is Relief in Our Head?
In the 1970s, organized medicine influenced media sources like Consumer Reports, Erma Bombeck, and Ann Landers’ articles to include anti-chiropractic rhetoric.83, 84, 85, 86 These communications influenced the public as well as doctors. They suggested that if someone went to a chiropractor and felt better, it was because the pain was unrelated to a physical problem but was just “in our head.”84,87, 88, 89 So was the medical propaganda at the time correct? Was pain relief after chiropractic imaginary?
Among the hypotheses that Joseph Janse, DC, presented in the NINDS conference that have seen promising subsequent study (Table 1) was the fixation hypothesis, first described by chiropractors Langworthy, Smith, and Paxson.9 This theory has been supported by subsequent osteopathic scientific literature,90, 91, 92, 93, 94 and was reintroduced into the chiropractic mainstream by Earl Homewood, DC, in 1962.95 Recently Evans et al96,97 and others98,99 reported methods for measuring spinal compliance associated with spinal fixation. Henderson et al’s100,101 work introduced the notions of buckling and reinforced Panjabe’s notion of dyskinesia within the joint neutral zone, and Pickar et al’s102,103 work on muscle spindle response to manipulative and mobilizing thrusts in animal models has similarly been pioneering. Since the NINDS conference, spinal fixation has been associated with the immobilization degeneration hypothesis, advanced by new discoveries using animal models, magnetic resonance imaging, and markers of inflammation.102,104, 105, 106, 107, 108 The neurodystrophy hypothesis, which includes the idea that immunity and inflammatory reactions may be altered by nerve activity changes as a result of spinal lesions, was offered by Janse, who cited Leonard Faye’s 1967 heuristic subluxation complex and the writings of other chiropractors like R. J. Watkins.109,110 Charles “Skip” Lantz, PhD, DC,12,69 helped introduce chiropractors to the idea that inflammation may result from spinal lesions such as subluxation, and the inflammation hypothesis has seen promising support after inquiry by chiropractic scientists in the past decade.74,76,111 Similarly, scientists began to investigate blood pressure changes after chiropractic in tests of the somatoautonomic hypothesis.98 Subsequent related inquiry provides support for the neuroplasticity hypothesis (ie, changes in central processing after spinal lesions may be reversed by chiropractic, associated with reduced pain and disability and enhanced task and sport performance).64,112,113 Janse reported on the subluxation hypothesis as a misalignment, but in this area subsequent research has been less supportive.114 Chiropractic professional guidelines no longer advocate for imaging before providing adjustments for most back pain cases because most patients with severe back pain improve after chiropractic regardless of x-ray or advanced imaging findings of misalignment or the presence of intervertebral disc herniation.115, 116, 117 Henderson101 argues that scientists may yet detect dyskinesia within a spine range of motion and that future studies on long-term rather than the short-term displacements observed to date may one day provide support for the misalignment hypothesis. In this regard, it is interesting that the cervical hypolordosis/forward head tilt first reported in the early chiropractic scientific literature by myself118 and exhaustively studied by other chiropractors119,120 is now being studied by physical therapy researchers, some of whom advocate for x-ray to monitor the condition121,122 Further validity research to determine whether there is a role for chiropractic and exercise, possibly aided by a specific type of traction, to treat this form of postural deformity or dyskinesia/subluxation is certainly warranted based on these promising studies. As just briefly explored here, research on these hypotheses in the last few decades began to explain how the manual techniques chiropractors use may have provided more than the imaginary benefit medical physicians and their surrogates once theorized.
Table 1.
1975 NINDS Conference Hypotheses Seeing Promising Subsequent Study in Research Referenced in PubMed by 2019
| Original 1975 NINDS Description | Search Words | Number of Pubmed results in July 2019 |
|---|---|---|
| Fixation hypothesis | ||
| spinal dysfunction | 367 | |
| spine manipulation, stiffness | 124 | |
| manipulable spinal lesion | 11 | |
| chiropractic spine compliance | 29 | |
| Immobilization degeneration hypothesis | ||
| Inflammation, spine pain | 1454 | |
| Immobilization, degeneration | 342 | |
| Neurodystrophy hypothesis | ||
| Inflammation, spine pain | 1454 | |
| neurodystrophy | 27 | |
| Subluxation hypothesis | ||
| forward head posture | 792 | |
| spinal dysfunction | 367 | |
| chiropractic subluxation | 218 | |
| Somatoautonomic reflex hypothesis | ||
| autonomic nervous system, spinal manipulation | 96 | |
| Neuroplasticity, spinal manipulation | 47 | |
| visceral responses, spinal manipulation | 10 |
Quantitative versus Qualitative Research
When a health care profession has an unending number of clinical questions but little manpower and funding for research, prioritization of the needs of patients and clinicians would seem to be a paramount consideration. Orthodox Western medicine clings to the RCT as the gold standard for detection of causality and to provide an evidence basis for practice, and certainly chiropractic scientists have increasingly completed these types of inquiries. However, Keating123 and I69 called for such quantitative outcomes-based studies to begin to incorporate the use of the most clinically promising potential mediator variables of spinal lesions embedded into these studies, as a means of addressing clinician concerns and questions. In this way, for example, as opposed to merely confirming the nonvalidity of mediator variables already questioned but continuing to be used in clinical practice (eg, leg checks), chiropractic scientists could explore the validity for measures called for by the Centers for Medicare & Medicaid Services guidelines for diagnosis of segmental dysfunction, (eg, which technique better measures tenderness in the spine that correlates with clinical outcomes, static manual palpation, or measurement of pressure pain thresholds by use of a force gauge?), pain provocation tests (instead of x-rays), and biological markers (instead of thermography). Scientists could determine whether the mediator variables covaried (directly or inversely) with the outcome variables in RCTs, and so answer both larger questions payers and governments want answered about chiropractic efficacy, while at the same time beginning to answer chiropractic clinical questions that may help direct patient care in our offices.
Health care research is moving from science to meta-science. Examples of this include asking how much knowledge is attained by scientists in a given health care profession124 and big data generated by easy access to increasing streams of digital variables that seem to acquire more and more attention.125 Some argue it becomes even more important to remember the distinction between exploratory data analysis facilitating hypothesis generation as opposed to confirmatory approaches that lead to hypothesis validation (or invalidation).125 Advocating for more qualitative research methods for clinical medicine, Caliebe et al125 point out that big data are only of low to moderate quality, because they are observational, uncontrolled, and only seemingly complete. They cite a chorus of others who conclude that “‘more data,’ does not always imply ‘more information’” and that perhaps it is time for more “1-person trials”125 such as single-subject and quasi-experimental research designs advocated by Center and Leach126 in addition to Keating.56,127 In this regard, there are numerous qualitative research designs that might be well suited for exploring the myriad chiropractic clinical questions, that are certainly within the reach of even budget-conscious research departments at all chiropractic institutions of higher learning, if not equally by the growing number of scientist/practitioners within the field.
Why Theory-Driven Research?
Efforts to prioritize research have been limited and a scoping review and assessment to determine the current status of chiropractic hypotheses has yet to be performed. Aside from some textbooks and conference proceedings,30,56,69,128,129 chiropractic scientists rarely discuss their hypotheses within the context of larger theory and do not generally design theory-based interventions seen in other health care professions. There are a number of reasons why a scoping review of chiropractic hypothesis and a theory-driven research approach may benefit the chiropractic profession.
Use of quantitative methods like classic RCTs in the past decades may have positioned chiropractors as equal or slightly superior for treatment of lower back pain, strengthening the position of broad scope practitioners that advocate for evidence-informed practice, but did not explain why, for example, 12% of patients with magnetic resonance imaging-confirmed lumbar herniated discs in 1 study did not respond favorably to chiropractic.130 Patients at the outer margins of the bell curve deserve answers as well, as do the chiropractic clinicians who treat them. Yet, these questions are beyond the reach of RCTs. Longo and Soto77 explain that in biological research changes occur relentlessly—as opposed to fixed properties observed in physics and mathematics—and that a theoretical framework is needed to even begin to understand the context of a differential cause that might be measured, for example, in an RCT. Recounting the condition of biology before D. D. Palmer first began to conceptualize a new health care field, these authors state that there were 2 main currents, “ . . . vitalism and physicalism. The vitalists proclaimed the independence of Biology from Physics while the physicalists expected to reduce Biology to Physics.”77 That this tension continues between theoretical and statistical approaches is underscored by their conclusion: “We biologists need to address the relentless change of the living objects and their individuality, their incessant change of symmetries, and their creativity.”77
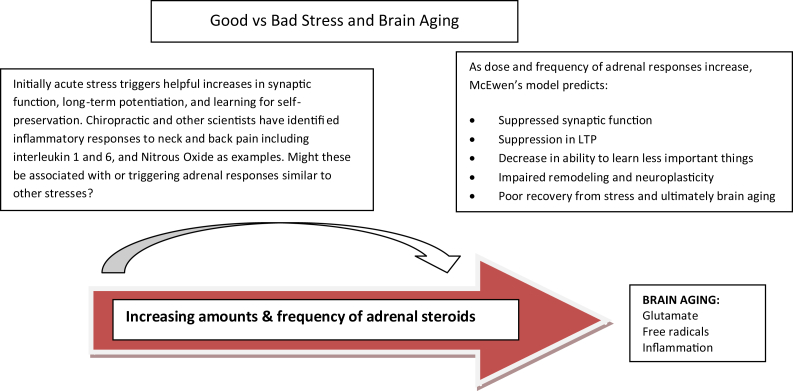
Currently the profession has relied on outcomes-based research that could only possibly provide evidence-informed applications for such easy-to-reach problems like neck and back pain. In contrast, a more qualitative and theory-based approach, such as is used in other allied health professions and that has been advocated for use in CAM research, could address needs of clinicians wishing to know more about how chiropractic works, and whether it works for many other applications ranging from infants with colic to carpal tunnel syndrome, and from children with attention deficit disorder to adults with spinal stenosis. A focus on mediator variables may help clinicians to understand better ways to monitor patient progress and perform evidence-based clinical tests that inform our practice behaviors and measure patient outcomes. A theory-driven approach that responds to the needs of both patients and clinicians and that dovetails with modern research on stress may confirm our newer research findings. For example, building on the work of Hans Selye, MD, PhD, who pioneered stress research in the past century,50 in the past 50 years neuroendocrinologist McEwen and colleagues have refined theory on how the adrenal response to stress affects neuroplasticity and leads to aging and damages the brain.131 A chiropractic theory-driven approach may well build on both McEwen et al as well as modern chiropractic research findings of reduction in inflammatory cytokines and positive changes in neural plasticity after chiropractic (Fig 4).131, 132, 133 New hypotheses may provide a more compelling message to the millennials and other health care providers than the early theories that were developed by our forbearers (Fig 5).
Fig 4.
Adaptation of McEwen model of good versus bad stress, showing dose response of increasing amounts and frequency of adrenal steroids in response to acute stressors having initially beneficial effects such as facilitation of long-term potentiation and memory. However, at some point increasing amounts and frequency of adrenal steroids result in suppression of synaptic function and long-term potentiation, and impairs remodeling and neuroplasticity in the central nervous system. In a modern adaptation of Selye’s classic earlier work, chiropractic scientists and others are providing intriguing evidence that spinal lesions and specifically low back pain may trigger these same phenomena, and for the first time provide evidence that spinal manipulation and adjustments may help reverse the deleterious effects on neuroplasticity associated with back pain, similar to the role for pharmacological and behavioral therapies McEwen advocates for anxiety and depression. In either case, the interventions (in the case of chiropractic, by triggering release of anti-inflammatory such as interleukin 10) may provide a window of plasticity whereby permanent therapeutic gains may be achieved, and provide the basis for a new hypothesis for chiropractic. LTP, long-term potentiation.
Fig 5.
Craven’s original chiropractic theory (left, c1920) was based on late 19th century cutting-edge science; this is from the same science that produced the author’s grandfather’s early party line wall telephone (right, c1920). We should develop a more modern approach using today’s thinking that will replace the late 19th century-based traditional chiropractic philosophy with a questioning philosophy and 21st century science.
Chiropractic could engage in health promotion by being supported by research that demonstrates that patients with chronic spine pain may have other chronic diseases and mental disorders134; have lower physical functional status than multiply comorbid patients without chronic spine pain135; have some of the same risk factors for herniated disc such as smoking136; are multiply comorbid when presenting to the chiropractor and other CAM offices137; and may develop such central nervous system effects as shrinkage of the prefrontal cortex, amygdala, and cingulate gyrus.64,138 Pain relief after chiropractic may not be merely imaginary as medical theorists once thought, but may be the result of a physical problem that affects the central nervous system and is literally in the head. Further research is needed to determine not only whether amelioration of chronic spine pain by spinal manipulation can improve health, but also whether other aspects of chiropractic care such as exercise instruction, nutrition counseling, and other in-office health promotion activities are effective in improving wellness and lowering disability. Such research would be critically useful for greater integration of chiropractic into the health care system and may help the professions heal from the rift partly fueled by decades of unsubstantiated claims and unyielding philosophy long proffered by those in both the chiropractic and medical professions.
In this regard, although research involving big data is necessary, smaller-scale qualitative studies fostered through an overarching theory-driven approach may be also useful in bridging the knowledge gap and helping us understand better, for example, how the chiropractor/patient relationship results in greater satisfaction than reported with so many other types of interventions, even when other previously thought important outcomes are not improved.3,139 Those in support of traditional chiropractic philosophy should acknowledge all truths revealed through a questioning philosophy and theory-driven approach, and not adhere dogmatically to unsupported thinking after it has been disproven or remains unproven.
Metaphors based on 100-year-old science may help chiropractors communicate difficult concepts to some patients. However, knowledge and application of modern philosophy-informed and theory-driven research has the potential to reveal truths, improve patient care, and provide better integration within the greater health care delivery system.
There is growing evidence for a serious research enterprise even among the traditionalists. A turn to a more questioning philosophy and theory-driven research that more adequately addresses practice questions may be expected to yield greater improvements in practice procedures and patient outcomes, and further integration of chiropractic into the health care community. It just may be that it is time for chiropractors to endorse a questioning philosophy and science of manipulation even as society now appears to be embracing their profession, and for the very problems for which patients most seek their services.140 It may well be that 125 years after chiropractic’s discovery, it is time for evidence-informed and theory-driven chiropractic practice.
Limitations
This commentary was written from my point of view and does not necessarily capture all views of this important topic. This paper does not include in-depth background on the various types of research that have been done in the chiropractic profession, therefore some material may have been missed. Further, there has been to date no scoping review of current chiropractic hypotheses and theory, and attempts here to review this broad topic have been meager at best. Finally, various arguments for or against philosophical and theory-based approaches to foster evidence-based chiropractic practice have only been generally and briefly discussed.
Rapid developments regarding inflammation and neuroplasticity correlating with spine pain underscore the need for a number of scientists to come together to begin to develop a current theory of chiropractic that is informed by a questioning philosophy. Certainly a literature review and development of a theoretical framework is indicated, and may inform the profession’s scientists, leaders, and other stakeholders who may wish to further prioritize an updated chiropractic research agenda. Discussion and theory development by a broad group of stakeholders—including both traditionalists and musculoskeletal chiropractors who advocate for evidence-based practice—would necessarily greatly improve the generalizability of suggestions offered here. A review and discussion of chiropractic theory by a number of scientists is needed to begin to develop a framework for a theory-driven process that could accompany such a philosophical approach.
Conclusion
Modern health care professionals often embrace philosophy. Philosophy can serve as a description for what we collectively believe. When applied in the practice setting, it guides our thinking, resulting in clinical questions naturally derived from our practice activities. When these questions are made into testable hypotheses and subjected to inquiry, the findings ultimately strengthen or refute the very philosophical underpinnings of our practices. By use of a questioning philosophy all truths related to practice behaviors, activities, and outcomes are brought to light, ultimately leading to improvements in procedures and outcomes. Traditional chiropractic philosophy, however, has often been of the unquestioning variety, unable to trigger changes in practice or procedures, nor in the philosophy itself. Hence, this approach limited truths applied to practice, since it incorporated research findings only if they were convenient to the original Palmerian philosophy, or some close variation. It is proposed that 125 years after its birth, the use of integral pluralism may be a philosophical method well suited for the evolution of chiropractic into the 21st century, where a more questioning philosophy is needed to move the profession forward.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): R.L.
Design (planned the methods to generate the results): R.L.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): R.L.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): R.L.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): R.L.
Literature search (performed the literature search): R.L.
Writing (responsible for writing a substantive part of the manuscript): R.L.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): R.L.
References
- 1.Gliedt J.A., Hawk C., Anderson M. Chiropractic identity, role and future: a survey of North American chiropractic students. Chiropr Man Therap. 2015;23(1):4. doi: 10.1186/s12998-014-0048-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feuerstein M., Marcus S.C., Huang G.D. National trends in nonoperative care for nonspecific back pain. Spine J. 2004;4(1):56–63. doi: 10.1016/j.spinee.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Weeks W.B., Goertz C.M., Meeker W.C., Marchiori D.M. Public perceptions of doctors of chiropractic: results of a national survey and examination of variation according to respondents’ likelihood to use chiropractic, experience with chiropractic, and chiropractic supply in local health care markets. J Manipulative Physiol Ther. 2015;38(8):533–544. doi: 10.1016/j.jmpt.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Palmer D.D. Portland Printing House Co; Portland, OR: 1910. Text-Book of the Science, Art and Philosophy of Chiropractic: For Students and Practitioners. [Google Scholar]
- 5.Palmer B.J., Craven J.H. 4th ed. Palmer School of Chiropractic; Davenport, IA: 1920. The Philosophy of Chiropractic. [Google Scholar]
- 6.Palmer DD. The Chiropractic. How to get well and keep well without using poisonous drugs. 1902(189):1-2.
- 7.Johnson C. Use of the term subluxation in publications during the formative years of the chiropractic profession. J Chiropr Humanit. 2011;18(1):1–9. doi: 10.1016/j.echu.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson C. Modernized chiropractic reconsidered: beyond foot-on-hose and bones-out-of-place. J Manipulative Physiol Ther. 2006;29(4):253–254. doi: 10.1016/j.jmpt.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 9.Smith O.G., Langworthy S.M., Paxon M.C. Lawrence Press; Cedar Rapids, IA: 1906. Modernized Chiropractic. [Google Scholar]
- 10.Young K.J. Evaluation of publicly available documents to trace chiropractic technique systems that advocate radiography for subluxation analysis: a proposed genealogy. J Chiropr Humanit. 2014;21(1):1–24. doi: 10.1016/j.echu.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Senzon S.A. The chiropractic vertebral subluxation part 1: introduction. J Chiropr Humanit. 2018;25:10–21. doi: 10.1016/j.echu.2018.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Senzon S.A. The chiropractic vertebral subluxation part 10: integrative and critical literature from 1996 and 1997. J Chiropr Humanit. 2018;25:146–168. doi: 10.1016/j.echu.2018.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Chiropractic Association Chiropractic in Medicare timeline. American Chiropractic Association. https://www.acatoday.org/Portals/60/Medicare/ACA%20Chiro%20Timeline%202019.pdf Available at:
- 14.Council on Chiropractic Education Historical development of the Council on Chiropractic Education. http://www.cce-usa.org/history.html Available at:
- 15.Coulter I., Adams A., Coggan P., Wilkes M., Gonyea M. A comparative study of chiropractic and medical education. Altern Ther Health Med. 1998;4(5):64–75. [PubMed] [Google Scholar]
- 16.Wardwell W.I. Mosby; St. Louis, MO: 1992. Chiropractic: History and Evolution of a New Profession. [Google Scholar]
- 17.Goldstein M., editor. Introduction, summary, and analysis. The research status of spinal manipulative therapy; Feb. 2-4, 1975. Government Printing Office; Washington, DC: 1975. [Google Scholar]
- 18.Janse J. History of the development of chiropractic concepts; chiropractic terminology. In: Goldstein M., editor. The Research Status of Spinal Manipulative Therapy. (NIH) 76-998. Government Printing Office; Bethesda, MD: 1975. pp. 25–42. [Google Scholar]
- 19.Evans M.E., Rupert R. The Council on Chiropractic Education’s new wellness standard: a call to action for the chiropractic profession. Chiropr Osteopat. 2006;14:23. doi: 10.1186/1746-1340-14-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Keating J.C., Jr., Caldwell S., Nguyen H., Saljooghi S., Smith B. A descriptive analysis of the Journal of Manipulative and Physiological Therapeutics, 1989-1996. J Manipulative Physiol Ther. 1998;21(8):539–552. [PubMed] [Google Scholar]
- 21.Guidelines for Chiropractic Quality Assurance and Practice Parameters. Aspen Publishers, Inc; Burlingame, CA: 1992. Proceedings of the Mercy Center Consensus Conference; Jan 25-30, 1992. [Google Scholar]
- 22.Ammendolia C., Taylor J.A., Pennick V., Cote P., Hogg-Johnson S., Bombardier C. Adherence to radiography guidelines for low back pain: a survey of chiropractic schools worldwide. J Manipulative Physiol Ther. 2008;31(6):412–418. doi: 10.1016/j.jmpt.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 23.Triano J.J. Literature syntheses for the Council on Chiropractic Guidelines and Practice Parameters: methodology. J Manipulative Physiol Ther. 2008;31(9):645–650. doi: 10.1016/j.jmpt.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 24.Bryans R., Descarreaux M., Duranleau M. Evidence-based guidelines for the chiropractic treatment of adults with headache. J Manipulative Physiol Ther. 2011;34(5):274–289. doi: 10.1016/j.jmpt.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 25.Hawk C., Schneider M.J., Haas M. Best practices for chiropractic care for older adults: a systematic review and consensus update. J Manipulative Physiol Ther. 2017;40(4):217–229. doi: 10.1016/j.jmpt.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 26.Bussieres A.E., Stewart G., Al-Zoubi F. Spinal manipulative therapy and other conservative treatments for low back pain: a guideline from the Canadian Chiropractic Guideline Initiative. J Manipulative Physiol Ther. 2018;41(4):265–293. doi: 10.1016/j.jmpt.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 27.Haas M., Bronfort G., Evans R.L. Chiropractic clinical research: progress and recommendations. J Manipulative Physiol Ther. 2006;29(9):695–706. doi: 10.1016/j.jmpt.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 28.Innes S.I., Leboeuf-Yde C., Walker B.F. How comprehensively is evidence-based practice represented in councils on chiropractic education (CCE) educational standards: a systematic audit. Chiropr Man Therap. 2016;24(1):30. doi: 10.1186/s12998-016-0112-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lawrence D.J., Meeker W.C. Commentary: the National Workshop to Develop the Chiropractic Research Agenda: 10 years on, a new set of white papers. J Manipulative Physiol Ther. 2006;29(9):690–694. doi: 10.1016/j.jmpt.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 30.Triano J.J., Goertz C., Weeks J. Chiropractic in North America: toward a strategic plan for professional renewal—outcomes from the 2006 Chiropractic Strategic Planning Conference. J Manipulative Physiol Ther. 2010;33(5):395–405. doi: 10.1016/j.jmpt.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 31.Andreoletti M., Maugeri P. Does medicine need philosophy? Oral Dis. 2019 doi: 10.1111/odi.13143. [DOI] [PubMed] [Google Scholar]
- 32.Charlton K.H. A chiropracticness test. Chiropr Osteopat. 2005;13:24. doi: 10.1186/1746-1340-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keating J.C., Jr., Charlton K.H., Grod J.P., Perle S.M., Sikorski D., Winterstein J.F. Subluxation: dogma or science? Chiropr Osteopat. 2005;13(1):17. doi: 10.1186/1746-1340-13-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khorsan R., Smith M., Hawk C., Haas M. A public health Immunization Resource Web site for chiropractors: discussion of current issues and future challenges for evidence-based initiatives for the chiropractic profession. J Manipulative Physiol Ther. 2009;32(6):500–504. doi: 10.1016/j.jmpt.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 35.Mirtz T.A., Perle S.M. The prevalence of the term subluxation in North American English-Language Doctor of chiropractic programs. Chiropr Man Therap. 2011;19:14. doi: 10.1186/2045-709X-19-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ivey J. Phenomenology vs philosophy in healthcare research. Ped Nurs. 2019;45(2) 93,98. [Google Scholar]
- 37.Johnston B.C., Seivenpiper J.L., Vernooij R.W.M. The philosophy of evidence-based principles and practice in nutrition. Mayo Clin Proc Innov Qual Outcomes. 2019;3(2):189–199. doi: 10.1016/j.mayocpiqo.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bobbio M., Vernero S. Choosing wisely, the reasons for its success. Monaldi Arch Chest Dis. 2019;89(2) doi: 10.4081/monaldi.2019.1104. [DOI] [PubMed] [Google Scholar]
- 39.Keating J.C., Jr., Sawyer C.E. Which philosophy of chiropractic? J Manipulative Physiol Ther. 1988;11(4):325–328. [PubMed] [Google Scholar]
- 40.Busse J.W., Wilson K., Campbell J.B. Attitudes towards vaccination among chiropractic and naturopathic students. Vaccine. 2008;26(49):6237–6243. doi: 10.1016/j.vaccine.2008.07.020. [DOI] [PubMed] [Google Scholar]
- 41.Gleberzon B., LM, Schmidt C., Ogrady J. On Vaccination & Chiropractic: when ideology history perception politics and jurisprudence collide. J Can Chiropr Assoc. 2013;57(3):205–213. [PMC free article] [PubMed] [Google Scholar]
- 42.McMurtry A., Wilson K., Clarkin C. The development of vaccination perspectives among chiropractic, naturopathic and medical students: a case study of professional enculturation. Adv Health Sci Educ Theory Pract. 2015;20(5):1291–1302. doi: 10.1007/s10459-015-9602-4. [DOI] [PubMed] [Google Scholar]
- 43.Keating J.C., Jr. Shades of straight: diversity among the purists. J Manipulative Physiol Ther. 1992;15(3):203–209. [PubMed] [Google Scholar]
- 44.Keating J.C., Jr. Purpose-straight chiropractic: not science, not health care. J Manipulative Physiol Ther. 1995;18(6):416–418. [PubMed] [Google Scholar]
- 45.Keating J.C. Scientific epistemology and the status of chiropractic: we are what we do. Eur J Chiropr. 1993;41(3):81–88. [Google Scholar]
- 46.Leach R.A. Evidence-based chiropractic: critical thinking in the private-practice setting. J Am Chiropr Assoc. 2005;42(1):37–46. [Google Scholar]
- 47.Senzon S.A. The chiropractic vertebral subluxation part 2: the earliest subluxation theories from 1902 to 1907. J Chiropr Humanit. 2018;25:22–35. doi: 10.1016/j.echu.2018.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Senzon S.A. The chiropractic vertebral subluxation part 9: complexes, models, and consensus from 1979 to 1995. J Chiropr Humanit. 2018;25:130–145. doi: 10.1016/j.echu.2018.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Senzon S.A. The chiropractic vertebral subluxation part 8: terminology, definitions, and historicity from 1966 to 1980. J Chiropr Humanit. 2018;25:114–129. doi: 10.1016/j.echu.2018.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Senzon S.A. The chiropractic vertebral subluxation part 7: technics and models from 1962 to 1980. J Chiropr Humanit. 2018;25:99–113. doi: 10.1016/j.echu.2018.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Senzon S.A. The chiropractic vertebral subluxation part 6: renaissance of D.D. Palmer’s paradigm from 1949 to 1961. J Chiropr Humanit. 2018;25:86–98. doi: 10.1016/j.echu.2018.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Senzon S.A. The chiropractic vertebral subluxation part 5: the first research era from 1928 to 1949. J Chiropr Humanit. 2018;25:67–85. doi: 10.1016/j.echu.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Senzon S.A. The chiropractic vertebral subluxation part 4: new perspectives and theorists from 1916 to 1927. J Chiropr Humanit. 2018;25:52–66. doi: 10.1016/j.echu.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Senzon S.A. The chiropractic vertebral subluxation part 3: complexity and identity from 1908 to 1915. J Chiropr Humanit. 2018;25:36–51. doi: 10.1016/j.echu.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cooperstein R. Technique research: how one chiropractic college [Palmer West] gets it done. JACA Online. 2008;45(1):12–14. [Google Scholar]
- 56.Keating J.C.J. 1st ed. Stockton Foundation for Chiropractic Research; Stockton, CA: 1992. Toward a Philosophy of the Science of Chiropractic: A Primer for Clinicians. [Google Scholar]
- 57.Senzon S.A. Constructing a philosophy of chiropractic: evolving worldviews and postmodern core. J Chiropr Humanit. 2011;18(1):39–63. doi: 10.1016/j.echu.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Leach R.A., Phillips R.B. Philosophy: foundation for theory development. In: Leach R.A., editor. The Chiropractic Theories: A Textbook of Scientific Research. 4th ed. Lippincott, Williams & Wilkins; Baltimore, MD: 2004. pp. 43–56. [Google Scholar]
- 59.Keating J.C. Rationalism and empericism vs. the philosophy of science in chiropractic. Chiropr Hist. 1990;10(2):23–30. [PubMed] [Google Scholar]
- 60.Catholic Straight Answers Quotes from famous scientists about God. http://catholicstraightanswers.com/assets/RCIA-Scientists-Quotes.pdf Available at: Accessed October 25, 2019.
- 61.Phillips W.D. Does science make belief in god obsolete? Fair Observer. November 10, 2013 [Google Scholar]
- 62.Kovanur-Sampath K., Mani R., Cotter J., Gisselman A.S., Tumilty S. Changes in biochemical markers following spinal manipulation-a systematic review and meta-analysis. Musculoskelet Sci Pract. 2017;29:120–131. doi: 10.1016/j.msksp.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 63.Haavik H., Niazi I.K., Jochumsen M. Chiropractic spinal manipulation alters TMS induced I-wave excitability and shortens the cortical silent period. J Electromyogr Kinesiol. 2018;42:24–35. doi: 10.1016/j.jelekin.2018.06.010. [DOI] [PubMed] [Google Scholar]
- 64.Haavik H., Niazi I.K., Holt K., Murphy B. Effects of 12 weeks of chiropractic care on central integration of dual somatosensory input in chronic pain patients: a preliminary study. J Manipulative Physiol Ther. 2017;40(3):127–138. doi: 10.1016/j.jmpt.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 65.Leboeuf-Yde C., Kyvik K.O. Is it possible to differentiate people with or without low-back pain on the basis of test of lumbopelvic dysfunction? J Manipulative Physiol Ther. 2000;23(3):160–167. doi: 10.1016/s0161-4754(00)90245-8. [DOI] [PubMed] [Google Scholar]
- 66.Lisi A.J., Cooperstein R., Morschhauser E. An exploratory study of provocation testing with padded wedges: can prone blocking demonstrate a directional preference? J Manipulative Physiol Ther. 2004;27(2):103–108. doi: 10.1016/j.jmpt.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 67.Schneider M., Erhard R., Brach J., Tellin W., Imbarlina F., Delitto A. Spinal palpation for lumbar segmental mobility and pain provocation: an interexaminer reliability study. J Manipulative Physiol Ther. 2008;31(6):465–473. doi: 10.1016/j.jmpt.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 68.Leach R.A., Owens E.F., Jr., Giesen J.M. Correlates of myoelectric asymmetry detected in low back pain patients using hand-held post-style surface electromyography. J Manipulative Physiol Ther. 1993;16(3):140–149. [PubMed] [Google Scholar]
- 69.Leach R. 4th ed. Lippincott, Williams & Wilkins; Baltimore, MD: 2004. The Chiropractic Theories: A Textbook of Scientific Research. [Google Scholar]
- 70.Gorrell L.M., Beath K., Engel R.M. Manual and instrument applied cervical manipulation for mechanical neck pain: a randomized controlled trial. J Manipulative Physiol Ther. 2016;39(5):319–329. doi: 10.1016/j.jmpt.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 71.Seaman D.R., Soltys J.R. Straight chiropractic philosophy as a barrier to Medicare compliance: a discussion of 5 incongruent issues. J Chiropr Humanit. 2013;20(1):19–26. doi: 10.1016/j.echu.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Leach R.A. Chiropractic research: attitudes that hinder. Chiropractic. 1988;1(1):14–17. [Google Scholar]
- 73.Tonelli M.R., Callahan T.C. Why alternative medicine cannot be evidence based. Acad Med. 2001;76(12):1213–1220. doi: 10.1097/00001888-200112000-00011. [DOI] [PubMed] [Google Scholar]
- 74.Song X.J., Huang Z.J., Song W.B. Attenuation effect of spinal manipulation on neuropathic and postoperative pain through activating endogenous anti-inflammatory cytokine interleukin 10 in rat spinal cord. J Manipulative Physiol Ther. 2016;39(1):42–53. doi: 10.1016/j.jmpt.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 75.Johnson C., Baird R., Dougherty P.E. Chiropractic and public health: current state and future vision. J Manipulative Physiol Ther. 2008;31(6):397–410. doi: 10.1016/j.jmpt.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 76.Teodorczyk-Injeyan J.A., McGregor M., Triano J.J., Injeyan H.S. Elevated production of nociceptive CC-chemokines and sE-selectin in patients with low back pain and the effects of spinal manipulation. Clin J Pain. 2018;34(1):68–75. doi: 10.1097/AJP.0000000000000507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Longo G., Soto A.M. Why do we need theories? Prog Biophys Mol Biol. 2016;122(1):4–10. doi: 10.1016/j.pbiomolbio.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.De Camargo K., Jr., Coeli C.M. Theory in practice: why “good medicine” and “scientific medicine” are not necessarily the same thing. Adv Health Sci Educ Theory Pract. 2006;11(1):77–89. doi: 10.1007/s10459-005-6924-7. [DOI] [PubMed] [Google Scholar]
- 79.Lu A.P., Jia H.W., Xiao C., Lu Q.P. Theory of traditional Chinese medicine and therapeutic method of diseases. World J Gastroenterol. 2004;10(13):1854–1856. doi: 10.3748/wjg.v10.i13.1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Moore G.F., Evans R.E. What theory, for whom and in which context? Reflections on the application of theory in the development and evaluation of complex population health interventions. SSM Popul Health. 2017;3:132–135. doi: 10.1016/j.ssmph.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Krieger N., Dorling D., McCartney G. Mapping injustice, visualizing equity: why theory, metaphors and images matter in tackling inequalities. Public Health. 2012;126(3):256–258. doi: 10.1016/j.puhe.2012.01.028. [DOI] [PubMed] [Google Scholar]
- 82.Decety J., Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci. 2015;8:457. doi: 10.3389/fnbeh.2014.00457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Botta J. Chiropractors: healers or quacks? Part 1: the 80-year war with science. Consumer Reports. September 1975:542–547. [PubMed] [Google Scholar]
- 84.Wilk et al v AMA et al. U.S. no. 76 C 3777. 1987.
- 85.Cohen H.H. Wilk v. American Medical Association--AMA enjoined from advocating boycott of chiropractors; individual choice endorsed. Med Staff Couns. 1988;2(2):63–69. [PubMed] [Google Scholar]
- 86.Holthaus D. Wilk decision has impact--one year later. Hospitals. 1988;62(15):50. [PubMed] [Google Scholar]
- 87.Chiropractors: healers or quacks? The eighty-year war with science. Del Med J. 1977;49(5):277–300. [PubMed] [Google Scholar]
- 88.Wardwell W. Public regulation of chiropractic. J Natl Med Assn. 1961;53:166–172. [PMC free article] [PubMed] [Google Scholar]
- 89.Sabatier J.A. At your own risk: the case against chiropractic. JAMA. 1969;209(11):1712. [PubMed] [Google Scholar]
- 90.Korr I. Plenum; New York, NY: 1978. Neurobiologic mechanisms in manipulative therapy. [Google Scholar]
- 91.Denslow J.S., Korr I.M., Krems A.D. Quantitative studies of chronic facilitation in human motoneuron pools. Am J Physiol. 1947;150:229–238. doi: 10.1152/ajplegacy.1947.150.2.229. [DOI] [PubMed] [Google Scholar]
- 92.Patterson M.M. Calling for theories that test the underlying osteopathic concepts. J Am Osteopath Assoc. 1990;90(9) 785, 789. [PubMed] [Google Scholar]
- 93.Patterson M.M., Steinmetz J.E. Long-lasting alterations of spinal reflexes: a potential basis for somatic dysfunction. Manual Med. 1986;2:38–42. [Google Scholar]
- 94.Patterson M.M. Manipulation for low back pain ahead of its time … but now is the time. J Am Osteopath Assoc. 1999;99(1):18. [PubMed] [Google Scholar]
- 95.Homewood A.E. private; Thornhill, Ontario: 1962. The Neurodynamics of the Vertebral Subluxation. [Google Scholar]
- 96.Leach R.A., Parker P.L., Veal P.S. PulStar differential compliance spinal instrument: a randomized interexaminer and intraexaminer reliability study. J Manipulative Physiol Ther. 2003;26(8):493–501. doi: 10.1016/S0161-4754(03)00106-4. [DOI] [PubMed] [Google Scholar]
- 97.Evans J.M., Hill C.R., Leach R.A., Collins D.L. The minimum energy hypothesis: a unified model of fixation resolution. J Manipulative Physiol Ther. 2002;25(2):105–110. doi: 10.1067/mmt.2002.121412. [DOI] [PubMed] [Google Scholar]
- 98.Cao D.Y., Reed W.R., Long C.R., Kawchuk G.N., Pickar J.G. Effects of thrust amplitude and duration of high-velocity, low-amplitude spinal manipulation on lumbar muscle spindle responses to vertebral position and movement. J Manipulative Physiol Ther. 2013;36(2):68–77. doi: 10.1016/j.jmpt.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Funabashi M., Nougarou F., Descarreaux M., Prasad N., Kawchuk G.N. Spinal tissue loading created by different methods of spinal manipulative therapy application. Spine (Phila Pa 1976) 2017;42(9):635–643. doi: 10.1097/BRS.0000000000002096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Henderson C.N., Cramer G.D., Zhang Q., DeVocht J.W., Sozio R.S., Fournier J.T. Introducing the external link model for studying spine fixation and misalignment: current procedures, costs, and failure rates. J Manipulative Physiol Ther. 2009;32(4):294–302. doi: 10.1016/j.jmpt.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 101.Henderson C.N. The basis for spinal manipulation: chiropractic perspective of indications and theory. J Electromyogr Kinesiol. 2012;22(5):632–642. doi: 10.1016/j.jelekin.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 102.Pickar J.G., Kang Y.M. Paraspinal muscle spindle responses to the duration of a spinal manipulation under force control. J Manipulative Physiol Ther. 2006;29(1):22–31. doi: 10.1016/j.jmpt.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 103.Reed W.R., Pickar J.G., Sozio R.S., Liebschner M.A.K., Little J.W., Gudavalli M.R. Characteristics of paraspinal muscle spindle response to mechanically assisted spinal manipulation: a preliminary report. J Manipulative Physiol Ther. 2017;40(6):371–380. doi: 10.1016/j.jmpt.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Degenhardt B.F., DN, Johnson J.C., Towns L.C. Role of osteopathic manipulative treatment in altering pain biomarkers: a pilot study. J Am Osteopath Assoc. 2007;107(9):387–400. [PubMed] [Google Scholar]
- 105.Pickar J.G. Neurophysiological effects of spinal manipulation. Spine J. 2002;2(5):357–371. doi: 10.1016/s1529-9430(02)00400-x. [DOI] [PubMed] [Google Scholar]
- 106.Arnbak B., Jensen R.K., Manniche C. Identification of subgroups of inflammatory and degenerative MRI findings in the spine and sacroiliac joints: a latent class analysis of 1037 patients with persistent low back pain. Arthritis Res Ther. 2016;18(1):237. doi: 10.1186/s13075-016-1131-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Koeppen D., Piepenbrock C., Kroppenstedt S., Cabraja M. The influence of sagittal profile alteration and final lordosis on the clinical outcome of cervical spondylotic myelopathy. A Delta-Omega-analysis. PLoS One. 2017;12(4) doi: 10.1371/journal.pone.0174527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Altun I. Cytokine profile in degenerated painful intervertebral disc: variability with respect to duration of symptoms and type of disease. Spine J. 2016;16(7):857–861. doi: 10.1016/j.spinee.2016.03.019. [DOI] [PubMed] [Google Scholar]
- 109.Faye LJ. VSC Position Paper. In: Anglo European Chiropractic College Curriculum Notes. chirosci-list@silcom.com. Accessed March 26, 2012.
- 110.Watkins R.J. Subluxation terminology since 1746. J Can Chiropr Assoc. 1968;12(4):20–24. [Google Scholar]
- 111.Kolberg C., Horst A., Moraes M.S. Peripheral oxidative stress blood markers in patients with chronic back or neck pain treated with high-velocity, low-amplitude manipulation. J Manipulative Physiol Ther. 2015;38(2):119–129. doi: 10.1016/j.jmpt.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 112.Hotz-Boendermaker S., Marcar V.L., Meier M.L., Boendermaker B., Humphreys B.K. Reorganization in secondary somatosensory cortex in chronic low back pain patients. Spine (Phila Pa 1976) 2016;41(11):E667–E673. doi: 10.1097/BRS.0000000000001348. [DOI] [PubMed] [Google Scholar]
- 113.Haavik H., Niazi I.K., Jochumsen M., Sherwin D., Flavel S., Turker K.S. Impact of spinal manipulation on cortical drive to upper and lower limb muscles. Brain Sci. 2016;7(1) doi: 10.3390/brainsci7010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Funk M.F., Frisina-Deyo A.J., Mirtz T.A., Perle S.M. The prevalence of the term subluxation in chiropractic degree program curricula throughout the world. Chiropr Man Therap. 2018;26(1) doi: 10.1186/s12998-018-0191-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hawk C., Schneider M., Dougherty P., Gleberzon B.J., Killinger L.Z. Best practices recommendations for chiropractic care for older adults: results of a consensus process. J Manipulative Physiol Ther. 2010;33(6):464–473. doi: 10.1016/j.jmpt.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 116.Jenkins H.J. Awareness of radiographic guidelines for low back pain: a survey of Australian chiropractors. Chiropr Man Therap. 2016;24:39–48. doi: 10.1186/s12998-016-0118-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bussieres A., TJ, Peterson C. Diagnostic imaging practice guidelines for musculoskeletal complaints in adults—an evidence-based approach—part 3: spinal disorders. J Manipulative Phyisol Ther. 2008;31(1):33–88. doi: 10.1016/j.jmpt.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 118.Leach R.A. An evaluation of the effect of chiropractic manipulative therapy on hypolordosis of the cervical spine. J Manipulative Physiol Ther. 1983;6(1):17–23. [PubMed] [Google Scholar]
- 119.Harrison D.D., Harrison D.E., Tadeusz J.J. Modeling of the sagittal cervical spine as a method to discriminate hypolordosis. Spine. 2004;29(22):2485–2492. doi: 10.1097/01.brs.0000144449.90741.7c. [DOI] [PubMed] [Google Scholar]
- 120.Cooperstein R., Perle S.M., Gleberzon B.J., Peterson D.H. Flawed trials, flawed analysis: why CBP should avoid rating itself. J Can Chiropr Assoc. 2006;50(2):97–102. [PMC free article] [PubMed] [Google Scholar]
- 121.Quek J., Pua Y.H., Clark R.A., Bryant A.L. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man Ther. 2013;18(1):65–71. doi: 10.1016/j.math.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 122.Gong W. The effects of cervical joint manipulation, based on passive motion analysis, on cervical lordosis, forward head posture, and cervical ROM in university students with abnormal posture of the cervical spine. J Phys Ther Sci. 2015;27:1609–1611. doi: 10.1589/jpts.27.1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Keating J.C., Jr. To hunt the subluxation: clinical research considerations. J Manipulative Physiol Ther. 1996;19(9):613–619. [PubMed] [Google Scholar]
- 124.Fanelli D. A theory and methodology to quantify knowledge. R Soc Open Sci. 2019;6(4):181055. doi: 10.1098/rsos.181055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Caliebe A., Leverkus F., Antes G., Krawczak M. Does big data require a methodological change in medical research? BMC Med Res Methodol. 2019;19(1):125. doi: 10.1186/s12874-019-0774-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Center D.B., Leach R.A. The multiple baseline across subjects design: proposed use in research. J Manipulative Physiol Ther. 1984;7(4):231–236. [PubMed] [Google Scholar]
- 127.Keating J.C., Jr., Calderon L. Clinical research preparation for chiropractors: implementing a scientist-practitioner model. J Manipulative Physiol Ther. 1987;10(3):124–129. [PubMed] [Google Scholar]
- 128.Gatterman M. 2nd ed. Lippincott, Williams & Wilkins; Baltimore, MD: 2004. Chiropractic Management of Spine Related Disorders. [Google Scholar]
- 129.Triano J.J. The subluxation complex: outcome measure of chiropractic diagnosis and treatment. Chiropr Tech. 1990;2:114–120. [Google Scholar]
- 130.Leemann S., Peterson C.K., Schmid C., Anklin B., Humphreys B.K. Outcomes of acute and chronic patients with magnetic resonance imaging-confirmed symptomatic lumbar disc herniations receiving high-velocity, low-amplitude, spinal manipulative therapy: a prospective observational cohort study with one-year follow-up. J Manipulative Physiol Ther. 2014;37(3):155–163. doi: 10.1016/j.jmpt.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 131.McEwen B.S. Redefining neuroendocrinology: epigenetics of brain-body communication over the life course. Front Neuroendocrinol. 2018;49:8–30. doi: 10.1016/j.yfrne.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 132.Gould E., Galea L.A.M. Fifty years of stress and more to come: a tribute to Bruce S. McEwen. Front Neuroendocrinol. 2018;49:1–2. doi: 10.1016/j.yfrne.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 133.Sheline Y.I., Liston C., McEwen B.S. Parsing the hippocampus in depression: chronic stress, hippocampal volume, and major depressive disorder. Biol Psychiatry. 2019;85(6):436–438. doi: 10.1016/j.biopsych.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 134.Von Korff M., Crane P., Lane M. Chronic spinal pain and physical-mental comorbidity in the United States: results from the national comorbidity survey replication. Pain. 2005;113(3):331–339. doi: 10.1016/j.pain.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 135.Fanuele J.C., Birkmeyer N.J., Abdu W.A., Tosteson T.D., Weinstein J.N. The Impact of spine problems on the health status of patients: Have we underestimated the effect? Spine (Phila Pa 1976) 2000;25(12):1509–1514. doi: 10.1097/00007632-200006150-00009. [DOI] [PubMed] [Google Scholar]
- 136.Jhawar B.S., FC, Colditz G.A., Stampfer M.J. Cardiovascular risk factors in herniated disc. Spine J. 2006;6:684–691. doi: 10.1016/j.spinee.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 137.Hawk C., Ndetan H., Evans M.W., Jr. Potential role of complementary and alternative health care providers in chronic disease prevention and health promotion: an analysis of National Health Interview Survey data. Prev Med. 2012;54(1):18–22. doi: 10.1016/j.ypmed.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 138.May A. Chronic pain may change the structure of the brain. Pain. 2008;137(1):7–15. doi: 10.1016/j.pain.2008.02.034. [DOI] [PubMed] [Google Scholar]
- 139.Weisman K., Markman E.M. Theory-based explanation as intervention. Psychon Bull Rev. 2017;24(5):1555–1562. doi: 10.3758/s13423-016-1207-2. [DOI] [PubMed] [Google Scholar]
- 140.Bussieres A.E., Al Zoubi F., Stuber K. Evidence based practice research utilization and knowledge translation in chiropractic: a scoping review. BMC Complement Altern Med. 2016;16:216–231. doi: 10.1186/s12906-016-1175-0. [DOI] [PMC free article] [PubMed] [Google Scholar]