Abstract
High-energy traumas frequently result in lumbar spine fractures such as spondyloptosis is the maximum expression of instability and severity. The management of spondyloptosis is complex and, essentially, surgical. It usually presents with irreversible neurological compromise. This paper aimed to present a case of lumbar spondyloptosis and its early confrontation, partial neurological involvement, and progressive postoperative retrieval.
Clinical case
A male patient aged 42 years had multiple injuries with asymmetric paraparesis and sphincter involvement. Computed tomography (CT) revealed L3 vertebral spondyloptosis detached from the rest of the spine, spinal canal stenosis, sagittal imbalance, and angular kyphosis. Surgical resolution was defined by performing an en bloc corpectomy through lumbotomy and the installation of an expandable cage with posterior transpedicular fixation of L2–L4, thereby recovering the spinal canal diameter, lumbar lordosis, sagittal balance, and improving motor function progressively.
Conclusion
Complex spinal injuries warrant an early resolution by a trained surgical team to ensure normal spinal parameters and to achieve a progressive neurological recovery.
Keywords: Trauma, Lumbar vertebrae, Intraoperative neurophysiological monitoring, Lordosis, Spinal fusion
1. Introduction
Spinal trauma is an important cause of morbidity and mortality, and leads to disability in the young working population. Thoracolumbar spine fractures most commonly affect the thoracolumbar junction. The goal of fracture treatment is to obtain and maintain a stable reduction that leads to early mobilization and satisfactory function, and to restore sagittal alignment [1].
Within the traumatic spine pathology, vertebral spondyloptosis corresponds to the maximum expression of instability. This is defined as subluxation of >100% of a vertebral body on another [2]. It is usually associated with a severe neurological deficit. Indeed, a complete paraplegia was estimated in 80% of cases [3]. Traumatic spondyloptosis relates to high-speed traumas [4]. Thus, it is not an uncommon association with other injuries, which result in multisystem collateral damage, where multidisciplinary intervention becomes essential [5].
Treatment is essentially surgical, with several existing options. These include fixation, fusion, and corpectomy with cage installation. Spondyloptosis is a surgical challenge, depending on the complexity and high variability of the presentation in the spine. Surgical reconstruction provides the best outcome because it restores the stability of the spine and facilitates early rehabilitation [2]. Spine surgeons must adapt and solve this challenging scenario despite having no experience given the infrequency of this spinal trauma presentation.
Traumatic spondyloptosis is extremely rare, with a paucity of case reports in the literature [6]. Thus, we decided to present a case of traumatic L3 spondyloptosis and disassociated spinal column subsequent to bilateral pedicle fracture and disco-ligament disruption.
2. Clinical case
The case involved a 42-year-old man who had a high-energy polytraumatism with a major impact in the thoracoabdominal region by a tree while he was working. He developed an asymmetric paraparesis and sphincter involvement. A thoracolumbar spine computed tomography (CT) study was performed and revealed L3 vertebral spondyloptosis detached from the rest of the spine, subsequent to a bilateral pedicle fracture, with the spinal canal stenosis associated with sagittal imbalance and angular kyphosis.
The patient had a multisystem trauma with fractures of the right-side ribs from the ninth to the 11th ribs and of the left-side ribs from the sixth to the 12th rib. He had a left hemopneumothorax that required a chest drain. Furthermore, the patient had a big retroperitoneal hematoma adjacent to the site of spondyloptosis, having fractures of both the transverse processes of L2. He had no cranial trauma.
A surgical resolution was defined by performing en bloc corpectomy (Fig. 1) via left-sided retroperitoneal lumbotomy with vascular surgeon assistance and patient in supine position, emptying a retroperitoneal hematoma, and the installation of an expandable cage between L2 and L4 (Fig. 2). Disco-ligaments L2–L3 and L3–L4 were partially attached to the L3 vertebral body and were removed before cage installation. Furthermore, fixation with transpedicular screws L2–L4 was performed with patient in prone position, repair of the posterior tension band (Fig. 3), without laminectomy. The entire procedure was performed under intraoperative neurophysiological monitoring.
Fig. 1.
L3 vertebral body removed en bloc via the anterolateral approach.
Fig. 2.
Left lumbotomy showing the psoas, great vessels, and expandable cage in position.
Fig. 3.
Intraoperative lateral radiographic image showing the final construct.
The patient progressed satisfactorily and was hemodynamically stable. The chest drain was removed on the fourth day of installation. The postoperative CT scan of the thoracolumbar spine demonstrated the return diameter of the spinal canal, lumbar lordosis, and overall sagittal balance (Fig. 4). The treatment gradually improved the patient's motor function in the lower extremities postoperatively, making him self-sufficient in the short-term follow-up. However, he remained with bowel compromise and left foot paresis, but was able to walk.
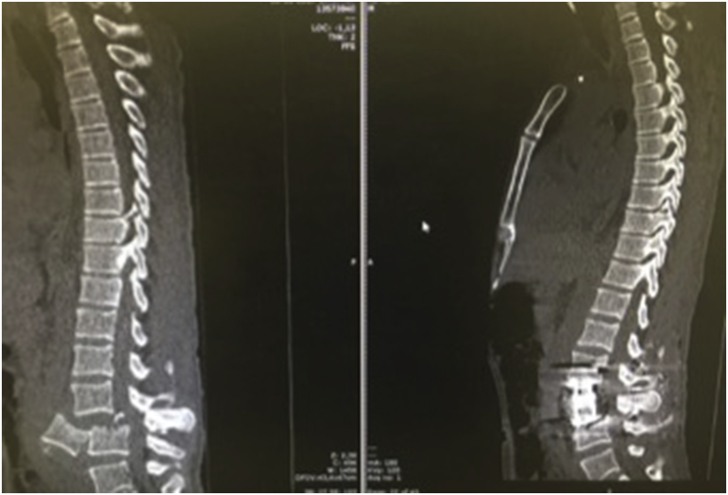
Fig. 4.
Sagittal computed tomography scan of the thoracolumbar spine. The left image shows L3 vertebral body spondyloptosis and sagittal imbalance, and the right image shows the recovery of sagittal balance.
3. Discussion
Traumatic lumbar spondyloptosis is rare but most frequently occurs at the L4–L5 and L5–S1 levels, and is associated with severe neurological deficit. However, some patients have an intact neurological function despite the fracture and complete lumbar dislocation. Gitelman et al. reported a case of spondyloptosis with full preservation of the neurological function [3]. Similarly, Abdel-Fattah et al. reported a case where the removal of the vertebral body kept the spinal canal decompressed, with consequent neurological indemnity after a high-energy traumatic event [7].
Lumbar injuries confer a risk on the cauda equina nerve roots. Partial neurological damage provides a greater chance of independence in daily life activities. However, early recognition of injuries and early treatment are crucial in preservation and neurological recovery. This was possible in the present case owing to the optimal management with early treatment by a multidisciplinary team.
Spondyloptosis is an unequivocal sign of instability. In the lumbar spine, the surgical treatment depends on the location of the vertebral body fracture. However, posterior instrumentation, with or without anterior column reconstruction, has become the standard treatment for most unstable lumbosacral spine injuries. Pedicle screw fixation has been shown to provide superior stability when used in conjunction with anterior instrumentation [8].
Several options of approach are available, and the appropriate approach is chosen according to the patient's conditions and the preferences of the surgical team. Most often, the posterior approach is preferred. Fattahi et al. presented a case of spondyloptosis at T7–T8 that resulted in paraplegia and was treated with a single spondylectomy and posterior fusion of T5–T11 [9]. In other cases, the anterolateral approach is used for an oblique corridor anterior to the psoas muscle and lateral to the great vessels. Independent of the used technique, the objective is to obtain the reduction and overall alignment of the spine with consequent early mobilization of the patient to reduce medical morbidity.
In the present case, we preferred to perform a lumbotomy with a retroperitoneal approach, with a surgical corridor similar to that in oblique lateral interbody fusion, assisted by a vascular surgeon, allowing favorable exposure, handling of the psoas and great vessels without damage, emptying the large retroperitoneal hematoma, and a resection of the vertebral body and replacement of the expandable cage. On the basis of our local experience, we believe that the isolated cases of expulsion of the vertebral body, detached from other osteoligamentous structures, approach via retroperitoneal lumbotomy for vertebral body replacement and subsequent reinforcement with a transpedicular posterior approach should be the rule.
The use of intraoperative neurophysiological monitoring is mandatory in cases of severe spinal trauma with partial neurological involvement. Currently, this tool plays a role in patients with severe paraparesis and forecasts future performance status. In the latter, it has been complemented with D-wave evaluation through an epidural catheter distal to the lesional site, even in the absence of motor evoked potentials (MEP) and indicates neurological recovery [10]. This was not possible in our case because the level of damage could not be determined in the D-wave recording. However, motor evoked potentials were highly compatible with the preoperative clinical condition of the patient, who remained without changes throughout the follow-up period.
4. Conclusion
Traumatic lumbar spondyloptosis is severe and infrequent, and represents a high degree of spinal instability. When the vertebra is detached from the rest of the spine through bilateral pedicle fractures, a patient could present with incomplete neurological involvement. The resolution of the same is surgical and complex, requiring specialized equipment, early confrontation to restore spinal stability and reduce associated neurological and medical morbidity.
References
- 1.Lee Y.C., Selby M., Zotti M., Roy D., Freeman B. Minimally invasive stabilization for thoracolumbar and lumbar fractures: a comparative study with short segment open Schanz screw constructs. J Spine Surg. 2019;5(1):13–18. doi: 10.21037/jss.2019.01.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amesiya R., Orwotho N., Nyati M., Mugarura R., Sabakaki E. Traumatic spondyloptosis of the lumbar spine: a case report. J. Med. Case Rep. 2014;8:453. doi: 10.1186/1752-1947-8-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gitelman A., Most M.J., Stephen M. Traumatic thoracic spondyloptosis without neurologic deficit and in situ treatment with fusion. Am J Orthop (Belle Mead NJ) 2009;38:E162–E165. [PubMed] [Google Scholar]
- 4.Mishra A., Agrawal D., Gupta D., Sinha S., Satyarthee G., Singh P. Traumatic spondyloptosis: a series of 20 patients. J. Neurosurg. Spine. 2015;22(6):647–652. doi: 10.3171/2014.10.SPINE1440. [DOI] [PubMed] [Google Scholar]
- 5.Garg M., Kumar A., Sawarkar D., Singh P., Agarwal D., Kale S. Traumatic lateral spondyloptosis: case series. World Neurosurg. 2018;113:E166–E171. doi: 10.1016/j.wneu.2018.01.206. [DOI] [PubMed] [Google Scholar]
- 6.Chatani K., Yoshioka M., Hase H., Hirasawa Y. Complete previous fracture-dislocation of the fourth lumbar vertebra. Spine. 1994;19(6):726–729. doi: 10.1097/00007632-199403001-00015. [DOI] [PubMed] [Google Scholar]
- 7.Abdel-Fattah H., Rizk A.H. Complete fracture-dislocation of the lower lumbar spine with spontaneous neurologic decompression. Clin. Orthop. Relat. Res. 1990;251:140–143. [PubMed] [Google Scholar]
- 8.Gabel B.C., Curtis E., Gonda D., Ciacci J. Traumatic L5 posterolateral spondyloptosis: a case report and review of the literature. Cureus. 2015;7(6):e277. doi: 10.7759/cureus.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fattahi A., Daneshi A. Traumatic thoracic spine spondyloptosis treated with spondylectomy and fusion. Surg. Neurol. Int. 2018;9(1):158. doi: 10.4103/sni.sni_204_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Costa P., Faccani G., Sala F., Montalenti E., Giobbe M.L., Deletis V. Neurophysiological assessment of the injured spinal cord: an intraoperative approach. Spinal Cord. 2014;52(10):749–757. doi: 10.1038/sc.2014.138. [DOI] [PubMed] [Google Scholar]