Abstract
Background: The prognostic role of the translational factor, elongation factor-1 alpha 1 (EEF1A1), in colon cancer is unclear. Objectives: The present study aimed to investigate the expression of EEF1A in tissues obtained from patients with stage II and III colon cancer and analyze its association with patient prognosis. Methods: A total of 281 patients with colon cancer who underwent curative resection were analyzed according to EEF1A1 expression. Results: The five-year overall survival in the high-EEF1A1 group was 87.7%, whereas it was 65.6% in the low-EEF1A1 expression group (hazard ratio (HR) 2.47, 95% confidence interval (CI) 1.38–4.44, p = 0.002). The five-year disease-free survival of patients with high EEF1A1 expression was 82.5%, which was longer than the rate of 55.4% observed for patients with low EEF1A1 expression (HR 2.94, 95% CI 1.72–5.04, p < 0.001). Univariate Cox regression analysis indicated that age, preoperative carcinoembryonic antigen level, adjuvant treatment, total number of metastatic lymph nodes, and EEF1A1 expression level were significant prognostic factors for death. In multivariate analysis, expression of EEF1A1 was an independent prognostic factor associated with death (HR 3.01, 95% CI 1.636–5.543, p < 0.001). EEF1A1 expression was also an independent prognostic factor for disease-free survival in multivariate analysis (HR 2.54, 95% CI 1.459–4.434, p < 0.001). Conclusions: Our study demonstrated that high expression of EEF1A1 has a favorable prognostic effect on patients with colon adenocarcinoma.
Keywords: cancer biomarker, colon adenocarcinoma, elongation factor-1 alpha 1, prognosis, translation factor
1. Introduction
Colon cancer is the second leading cause of cancer-related death worldwide, with an incidence of 9.2% [1]. Although curative surgical resection of primary lesions and post-operative adjuvant treatment contribute to the prevention of early recurrence in patients with high-risk stage II and III colon cancer, the recurrence rate after curative surgery remains at 20%–30% [2]. To prolong disease-free survival (DFS) after curative surgery and avoid unnecessary over-treatment of patients, more accurate prognostic tools are required. However, a few clinical prognostic factors, such as the presence of obstructive symptoms, number of retrieved regional lymph nodes, pathologic tumor and nodal stage, and features associated with micrometastatic potential including vascular, lymphatic, and perineural invasion, have been used to select patients that may benefit from adjuvant therapies [3]. Although other molecular signatures, such as microsatellite status, BRAF (v-Raf murine sarcoma viral oncogene homolog B) and KRAS (V-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog) mutations, molecular signatures, and immune infiltration, have been suggested as potential prognosticators, more sophisticated prognostic biomarkers need to be identified [1,3].
To identify accurate and definitive molecular biomarkers for human malignancies, we previously developed a neural network-based model, Wx, which is optimized to select gene sets based on the discriminative index between combination pairs of K class [4]. In our previous report, we applied our Wx model to a pan-cancer cohort from The Cancer Genome Atlas (TCGA) RNA-Seq dataset, consisting of 12 different types of cancer and normal samples, and obtained 14 genes distinguishing cancer tissues from normal tissues with high accuracy. Tissue elongation factor 1 alpha 1 (EEF1A1) was one of the 14 biomarker genes extracted using the Wx model. Interestingly, it was also identified by Martinez-Ledesma et al. using the same discriminative concept to compare colon adenocarcinoma to normal tissues [5].
EEF1A1 is a ubiquitous protein that functions in peptide elongation during mRNA translation and is the second-most abundant protein after actin in eukaryotic proteomes [6,7]. As a translational factor, EEF1A delivers the aminoacylated-tRNA to the ribosome, as a ternary complex comprising EEF1A–GTP (Guanosine-5’-triphosphate)–aminoacylated-tRNA, to decode mRNA. There are two isoforms of EEF1A, namely EEF1A1 and EEF1A2, which were mapped to chromosomes 6q14 and 2q13.3, respectively [8]. EEF1A1 and EEF1A2 share more than 95% DNA and protein identity [9]. EEF1A1 is expressed in most cells, whereas EEF1A2 is present only in the brain, heart, and skeletal muscle [10]. Although the functional significance of their tissue-specific expression patterns is unknown, they are thought to have the same enzymatic function in protein translation. Several studies have revealed that EEF1A is not only a translation factor but also involved in many non-canonical functions including oncogenesis, protein degradation, pro-apoptotic or anti-apoptotic activity, and cytoskeleton modulation [10,11,12,13]. Notably, many studies have shown that EEF1A is a prognostic factor for several solid tumors such as ovary [11,14], breast [15,16,17], lung [18], pancreas [19,20], stomach [21,22], prostate [23], and liver cancers [24,25]. Based on the previous results from the Wx neural network-based feature selection algorithm and those reporting the role of EEF1A1 in human solid cancer, we hypothesized that EEF1A1 is related to the prognosis of patients with colon adenocarcinoma. In this study, we investigated the expression of EEF1A in tissues from patients with stage II and III colon cancer and analyzed its association with patient prognosis.
2. Methods
2.1. Identification of Prognostic Biomarker Genes Using the Wx Algorithm with TCGA Database
Genes distinguishing cancer from normal samples were identified by applying the Wx algorithm to a pan-cancer cohort containing 6210 samples with 12 different types of cancer, using mRNA-Seq data from TCGA. In this study, we re-analyzed the mRNA-Seq data of 327 colon adenocarcinomas (287 cancer and 40 normal samples) to identify biomarker candidate genes using the Wx algorithm. The Wx algorithm ranks genes based on the discriminative index score, which reflects the classification power of distinction between groups (e.g., cancer vs. normal). The detailed method has been described previously [4].
2.2. Patients and Tissue Samples
Medical records of patients with colon cancer who have undergone curative surgery at Incheon St. Mary’s hospital between 2010 and 2013 were reviewed. Their tissue microarrays (TMAs) for immunohistochemistry were obtained. If available, fresh-frozen tumor tissues and paired normal adjacent tissues from patients were used for RNA extraction. Demographic and clinicopathological data for these patients were reviewed retrospectively from the medical records. Variable factors including age, sex, sidedness of colon cancer, pathologic staging, histology, and lymphatic, venous, and perineural invasion were analyzed, and tumors were staged according to the pathological tumor/node/metastasis (pTNM) classification (8th edition) of the Union for International Cancer Control. The study was approved by the Institutional Review Board of Incheon St. Mary’s hospital, the Catholic University of Korea (OC15TISI0050). Informed consent was waived considering the retrospective study design.
2.3. Quantitative Reverse Transcription PCR (qRT-PCR)
Total RNA was isolated from tumors and adjacent normal tissues of patients with colon cancer using the WelPrepTM Total RNA Isolation Reagent (Welgene, Daegu, Korea) and gentleMACS Dissociator (Miltenyi Biotec, Bergisch Gladbach, Germany), according to the manufacturer’s protocols. To analyze mRNA levels, qRT-PCR assays were performed using a BioFACTTM A-Star Real-time PCR Kit including SFCgreen® I (BioFACT, Daejeon, Korea) after reverse transcription with ELPIS RT Prime Kit (Elpis-Biotech, Daejeon, Korea). mRNA levels were normalized to those of ribosomal protein L32 (RPL32).
2.4. Tissue Microarray Construction and Immunohistochemistry
Formalin-fixed paraffin-embedded colon cancer samples from patients who underwent surgery were included in a TMA after careful review by two experienced pathologists. TMAs were prepared with a tissue array and were composed of 69 cores per TMA, with a core diameter of 2 mm. The cores were derived from separate sources and treated as individual cases, and not as duplicates from a single source. Cases that presented as colon cancer had sufficient material for two cores, whereas normal tissues could be used to generate one core. A set comprising 14 slides was stained by immunohistochemistry. The antibodies used for the study included a mouse monoclonal antibody against EEF1A1 (sc-21758) from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA), which was used according to the manufacturer’s instructions at a dilution of 1:100 after optimization. Immunohistochemical staining was carried out with the Ventana BenchMark ULTRA (Tucson, AZ, USA) using the ultraView Universal DAB detection kit. This included standard de-paraffinization, blocking of endogenous peroxidase and biotin, incubation with primary and secondary antibodies, and development with DAB (di-aminobenzidine). The slides were counterstained with hematoxylin and eosin (H&E).
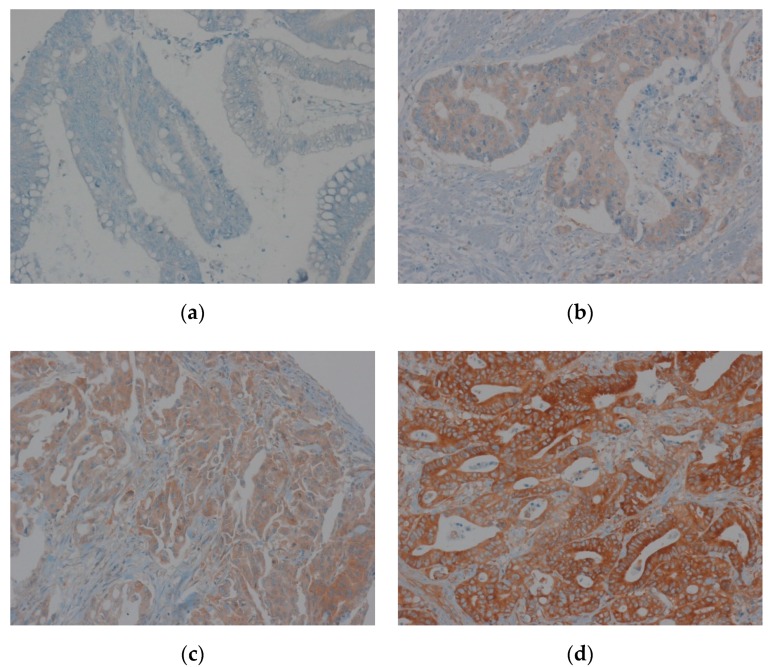
2.5. Evaluation of Immunohistochemical Staining of EEF1A1
Immunohistochemical staining for EEF1A1 revealed its cytoplasmic expression in most tumor cells. Staining intensity was graded from 0 to 3 (0 = no expression, 1 = weak, 2 = moderate, and 3 = strong). The extent was graded from 0 to 2 (0 = 0%, 1 = 1%–50%, 2 = 51%–100% of cells) (Figure 1). The intensity and extent scores were added to obtain a composite score. Patients with composite scores of 0–2 were classified into the low-EEF1A1 expression group and those with scores of 3–6 were included in the high-expression group. The results were analyzed by two pathologists who were blinded to the clinical data.
Figure 1.
Immunohistochemical staining of elongation factor-1 alpha 1 (EEF1A1) in colon adenocarcinoma tissue. (a) Staining intensity 0; (b) staining intensity 1; (c) staining intensity 2; (d) staining intensity 3.
2.6. Statistical Analysis
Categorical values were presented as means and percentages, and non-categorical values were presented as median values and ranges. The Chi-squared test and one-way analysis of variance were performed to compare differences among means and medians, respectively. The Kaplan–Meier method was used to calculate survival rates. DFS was defined as the period from the date of curative operation of colon cancer to the date of recurrence based on medical records. Overall survival (OS) was defined as the period from the date of curative operation of colon cancer to the date of death due to any cause. Right colon cancer was defined as cancer originating from the ascending colon to the splenic flexure and left colon cancer was defined as originating from the descending colon to the sigmoid colon. A p-value < 0.05 was considered to indicate statistical significance. Differences in survival rates across each patient group were examined by the log-rank test. A Cox proportional-hazards model was used for univariate and multivariate analyses. All analyses were performed with SPSS for windows (version 25.0, SPSS, Inc., Chicago, IL, USA).
3. Results
3.1. Baseline Characteristics of the Study Population
A total of 281 patients with colon cancer who underwent curative resection as the primary treatment were retrospectively analyzed. Of them, 132 patients (47.0%) had stage II disease, whereas the remaining 149 (53.0%) had stage III lesions. Among patients with stage II, 89 (67.4%) were administered post-operative adjuvant treatment. The median pre-operative carcinoembryonic antigen (CEA) value was 3.34 ng/mL (range: 0.08–1926.6 ng/mL). The KRAS status was identified in only 143 patients and KRAS mutations were observed in 52 (36.4%) tumor tissues. The detailed demographic features of these patients are summarized in Table 1.
Table 1.
Baseline characteristics of colon cancer patients stratified based on EEF1A1 expression.
| EEF1A1-Low (n = 42) | EEF1A1-High (n = 239) | p-Value | |
|---|---|---|---|
| Age (years) | |||
| <65 | 22 (52.4%) | 113 (47.3%) | 0.616 |
| ≥65 | 20 (47.6%) | 126 (52.7%) | |
| Sex | |||
| Male | 26 (61.9%) | 129 (54.0%) | 0.402 |
| Female | 16 (38.1%) | 110 (46.0%) | |
| Body mass index (BMI) (kg/m2) | |||
| <18.5 | 2 (4.8%) | 17 (7.1%) | 0.839 |
| 18.5–25.0 | 23 (54.7%) | 124 (51.9%) | |
| >25.0 | 17 (40.5%) | 98 (41.0%) | |
| Number of comorbid diseases | |||
| 0 | 23 (54.8%) | 101 (42.3%) | 0.265 |
| 1 | 10 (23.8%) | 84 (35.1%) | |
| ≥2 | 9 (21.4%) | 54 (22.6%) | |
| Location of primary cancer | |||
| Left | 20 (47.6%) | 152 (63.6%) | 0.059 |
| Right | 22 (52.4%) | 87 (36.4%) | 0.059 |
| Pre-operative carcinoembryonic antigen (CEA) | |||
| <5 ng/mL | 27 (64.3%) | 151 (63.4%) | 1.000 |
| >5 ng/mL | 15 (35.7%) | 87 (36.6%) | |
| Bowel obstruction or perforation | |||
| No | 32 (76.2%) | 215 (90.0%) | 0.019 |
| Yes | 10 (23.8%) | 24 (10.0%) | |
| Adjuvant chemotherapy | |||
| No | 11 (76.2%) | 50 (20.9%) | 0.424 |
| Yes | 31 (73.8%) | 189 (79.1%) | |
| Stage (tumor/node/metastasis, TNM) | |||
| II | 15 (35.7%) | 117 (49.0%) | 0.132 |
| III | 27 (64.3%) | 122 (51.0%) | |
| pT stage | |||
| 2 | 1 (2.4%) | 10 (4.2%) | 0.097 |
| 3 | 30 (71.4%) | 197 (82.4%) | |
| 4 | 11 (26.2%) | 32 (13.4%) | |
| pN stage | 0.076 | ||
| 0 | 15 (35.7%) | 118 (49.4%) | |
| 1 | 18 (42.9%) | 62 (25.9%) | |
| 2 | 9 (21.4%) | 59 (24.7%) | |
| Differentiation | 0.319 | ||
| Well | 1 (2.4%) | 6 (2.5%) | |
| Moderate | 36 (87.8%) | 223 (93.3%) | |
| Poor | 4 (9.8%) | 10 (4.2%) | |
| Perineural invasion | 0.083 | ||
| No | 21 (50.0%) | 155 (64.9%) | |
| Yes | 21 (50.0%) | 84 (35.1%) | |
| Venous invasion | 0.503 | ||
| No | 37 (88.1%) | 199 (83.3%) | |
| Yes | 5 (11.9%) | 40 (16.7%) | |
| Lymphatic invasion | 0.610 | ||
| No | 27 (64.3%) | 141 (59.0%) | |
| Yes | 15 (35.7%) | 98 (41.0%) | |
| Number of harvested lymoh nodes | 23.5 (10–63) | 22 (4–115) | 0.259 |
| Number of metastatic lymph nodes | 1 (0–15) | 1 (0–18) | 0.560 |
| Metastatic lymphnodes/harvested lymph nodesratio | 4.9 (0–66.7) | 2.6 (0–100) | 0.943 |
| KRAS 1 | 0.811 | ||
| Wild-type | 14 (66.7%) | 77 (63.1%) | |
| Mutant | 7 (33.3%) | 45 (36.9%) |
1KRAS; V-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog gene.
3.2. mRNA Expression of EEF1A1 in Human Colon Cancer Tissues Compared to That in Normal Adjacent Tissues
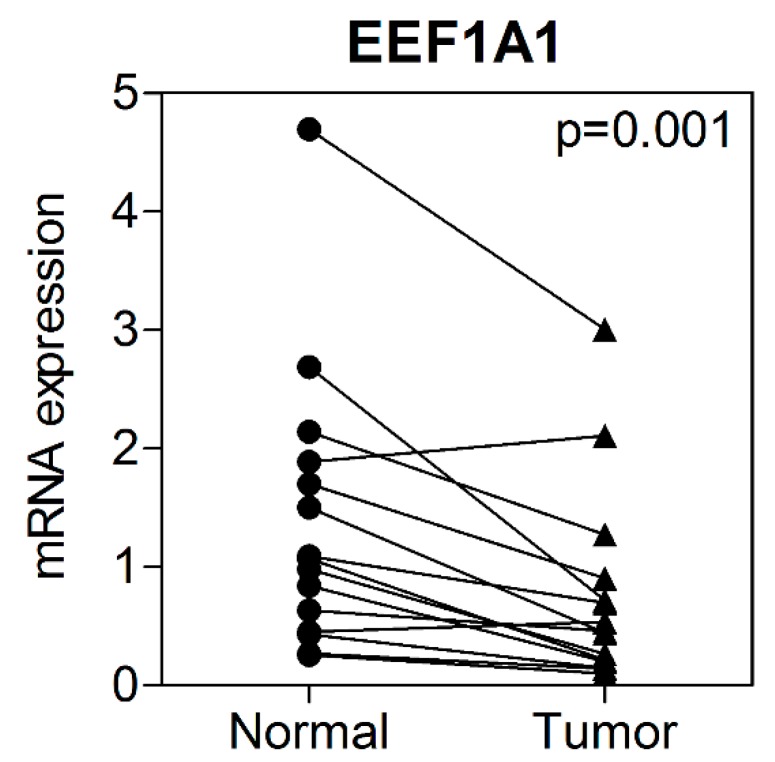
Of the total study population, EEF1A1 mRNA expression levels were investigated in 15 patients from whom fresh tumor and adjacent normal tissue could be harvested. EEF1A1 mRNA levels were significantly reduced in the tumor tissues compared to those in the normal adjacent tissue (Figure 2).
Figure 2.
Expression of EEF1A1 in colon cancer tissue and normal adjacent tissue.
3.3. Correlation between EEF1A1 Expression and Clinicopathological Characteristics
EEF1A1 immunostaining was typically negative or very weakly positive in the perinuclear cytoplasmic area of the normal colonic mucosa. In the tissue with positive EEF1A1 immunostaining, diffuse cytoplasmic staining was observed in tumor cells. The intensity of EEF1A1 was as follows: intensity 0:19 patients (6.8%), 1:86 (30.6%), 2:139 (49.5%), and 3:37 (13.2%). According to composite scores, 42 (14.9%) patients were classified as having low EEF1A1 expression, whereas 239 patients (85.1%) were classified as having high expression (Table S1). Stage, age, sex, harvested lymph node during surgery, and the proportion of patients administered post-operative adjuvant treatment did not differ between patients with low and high expression. Intestinal obstruction or perforation, due to primary colon cancer, was more frequently observed in patients with low EEF1A1 expression than in those with high expression. Patients with low EEF1A1 expression tended to have a larger proportion of right-sided tumors than those with high expression, although this result was not significant. KRAS mutations were not associated with EEF1A1 expression (p = 0.399). Other patient clinicopathological characteristics, according to EEF1A1 expression, are listed in Table 1.
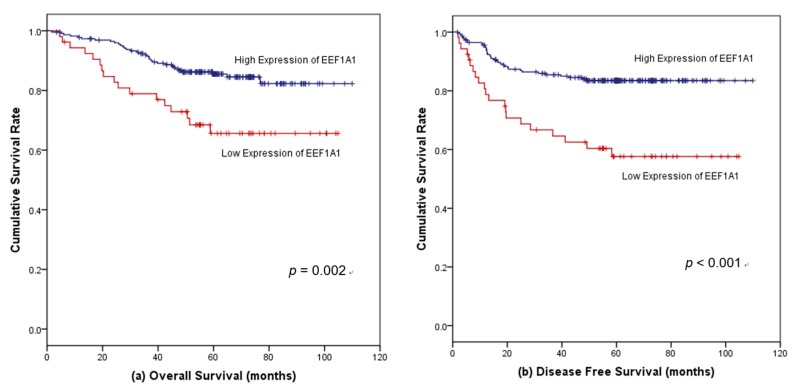
3.4. Survival Outcomes According to EEF1A1 Expression
The median follow-up period was 59.9 months (range 1.7–110.0 months). Considering all patients, the five-year OS in the high-EEF1A1 group was 87.7%, whereas it was 65.6% in the low-EEF1A1 expression group (p = 0.002, hazard ratio (HR) = 2.47, 95% confidence interval (CI) = 1.38–4.44) (Figure 3a). The five-year DFS of patients with high EEF1A1 expression was 82.5%, which was longer than the rate of 55.4% observed for patients with low EEF1A1 expression (p < 0.001, HR = 2.94, 95% CI = 1.72–5.04) (Figure 3b).
Figure 3.
Kaplan–Meier survival curves according to EEF1A1 protein expression in all colon cancer patients. (a) High EEF1A1 expression was significantly associated with favorable overall survival (OS) and (b) disease-free survival (DFS).
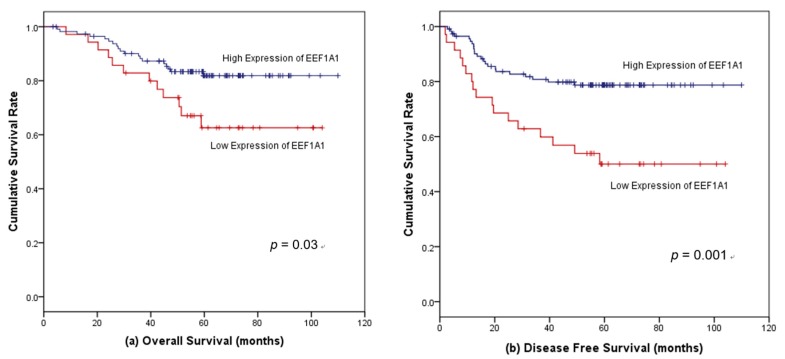
For stage II cancer, the 5-year OS of patients with high EEF1A1 expression tended to be longer than that of patients with low EEF1A1 expression (89.0% vs. 71.1%, p = 0.051, HR = 2.68, 95% CI = 0.96–7.43). The 5-year DFS of patients with high EEF1A1 was 88.0%, compared to 75.4% for those with low EEF1A1 (p = 0.134, HR = 2.30, 95% = CI 0.75–7.07). Among patients with stage II disease who were not administered post-operative adjuvant treatment, those with high EEF1A1 expression had a longer OS (5-year OS rate, 87.7%) than those with low EEF1A1 levels (57.1%) (p = 0.026). This survival difference according to EEF1A1 expression was not observed for patients administered adjuvant treatment after stage II disease (p = 0.985). For stage III cancer, the 5-year OS was 88.1% for patients with high EEF1A1 expression and 62.6% for those with low EEF1A1 (p = 0.030, HR = 2.22, 95% CI = 1.06–4.50) (Figure 4a). Among patients with stage III disease, the 5-year DFS for patients in the high-EEF1A1 group was 78.7%, compared to 50.0% for those with low EEF1A1 (p = 0.001, HR = 2.72, 95% = CI 1.45–6. 09) (Figure 4b).
Figure 4.
Kaplan–Meier survival curves according to EEF1A1 protein expression in stage III colon cancer patients. (a) High EEF1A1 expression was significantly associated with favorable overall survival (OS) and (b) disease-free survival (DFS).
3.5. Factors Associated with Survival in Patients with Stages II and III Colon Cancer
Univariate Cox regression analysis indicated that age, pre-operative CEA levels, adjuvant treatment, total number of metastatic lymph nodes, and EEF1A1 expression levels were significant prognostic factors for death. Based on multivariate analysis, the expression of EEF1A1 retained its independence as a prognostic factor associated with death (HR = 3.01, 95% CI = 1.636–5.543, p < 0.001) (Table 2). EEF1A1 expression was also an independent prognostic factor for recurrence based on multivariate analysis (HR = 2.54, 95% CI = 1.459–4.434, p-value < 0.001). Other significant prognostic markers for DFS included pre-operative CEA level and TNM stage (Table 3).
Table 2.
Cox regression analysis of overall survival for 281 patients with curatively-resected colon cancer.
| Crude Hazard Ratio (95% CI) | p-Value | Adjusted Hazard Ratio (95% CI) | p-Value | |
|---|---|---|---|---|
| Age ≥ 65 (years) | 5.08 (2.468–10.462) | <0.001 | 5.93 (2.810–12.493) | <0.001 |
| Male | 1.31 (0.738–2.316) | 0.358 | ||
| BMI (reference: <18.5 kg/m2) | ||||
| 18.5–25.0 (kg/m2) | 1.17 (0.355–3.853) | 0.796 | ||
| >25.0 (kg/m2) | 0.98 (0.290–3.330) | 0.978 | ||
| Number of comorbid diseases (reference: 0) | ||||
| 1 | 1.02 (0.520–1.985) | 0.964 | ||
| ≥2 | 1.02 (0.776–2.963) | 0.223 | ||
| Right-sided location of primary cancer | 1.45 (0.827–2.527) | 0.196 | ||
| Pre-operative CEA ≥ 5 ng/mL | 1.794 (1.030–3.126) | 0.039 | 1.76 (1.008–3.027) | 0.058 |
| Combined bowel obstruction or perforation at initial diagnosis | 1.286 (0.578–2.859) | 0.537 | ||
| Adjuvant chemotherapy | 2.240 (1.247–4.024) | 0.007 | 0.034 | |
| Stage III | 1.509 (0.852–2.672) | 0.158 | ||
| Differentiation (reference: well) | ||||
| Moderate | 0.508 (0.123–2.096) | 0.349 | ||
| Poor | 0.531 (0.075–3.773) | 0.527 | ||
| Perineural invasion | 1.443 (0.827–2.516) | 0.197 | ||
| Venous invasion | 1.545 (0.791–3.017) | 0.203 | ||
| Lymphatic invasion | 1.542 (0.886–2.685) | 0.120 | ||
| Number of harvested lymph nodes | 0.996 (0.792–1.021) | 0.756 | ||
| Number of metastatic lymph nodes | 1.078 (1.004–1.156) | 0.037 | 1.350 (0.718–2.539) | 0.351 |
| KRAS1 mutated cancer | 2.020 (0.779–5.236) | 0.148 | ||
| Low EEF1A1 expression | 2.560 (1.380–4.749) | 0.003 | 3.01 (1.636–5.543) | <0.001 |
1KRAS; V-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog gene.
Table 3.
Cox regression analysis of disease-free survival for 281 patients with curatively-resected colon cancer.
| Crude Hazard Ratio (95% CI) | p-Value | Adjusted Hazard Ratio (95% CI) | p-Value | |
|---|---|---|---|---|
| Age ≥ 65 (years-old) | 1.44 (0.852–2.442) | 0.172 | ||
| Male | 1.18 (0.697–2.008) | 0.533 | ||
| BMI (reference: <18.5 kg/m2) | 0.651 | |||
| 18.5–25.0 (kg/m2) | 0.69 (0.271–1.800) | 0.457 | ||
| >25.0 (kg/m2) | 0.98 (0.290–3.330) | 0.978 | ||
| Number of comorbid diseases (reference: 0) | ||||
| 1 | 1.04 (0.567–1.891) | 0.909 | ||
| ≥2 | 1.15 (0.593–2.216) | 0.685 | ||
| Right-sided location of primary cancer | 1.24 (0.730–2.103) | 0.428 | ||
| Pre-operative CEA ≥ 5 ng/mL | 2.35 (1.397–3.966) | 0.001 | 2.23 (1.308–3.806) | 0.003 |
| Combined bowel obstruction or perforation at initial diagnosis | 0.88 (0.379–2.057) | 0.773 | ||
| Adjuvant chemotherapy | 1.09 (0.578–2.066) | 0.785 | ||
| Stage III | 2.22 (1.256–3.908) | 0.006 | 25.80 (3.087–215.562) | 0.003 |
| Differentiation (reference: well) | 0.645 | |||
| Moderate | 0.51 (0.123–2.096) | 0.349 | ||
| Poor | 0.53 (0.075–3.773) | 0.527 | ||
| Perineural invasion | 1.34 (0.796–2.268) | 0.268 | ||
| Venous invasion | 1.19 (0.604–2.364) | 0.610 | ||
| Lymphatic invasion | 1.52 (0.901–2.546) | 0.117 | ||
| Number of harvested lymph nodes | 1.01 (1.002–1.026) | 0.021 | 1.02 (0.994–1.042) | 0.150 |
| Number of metastatic lymph nodes | 1.10 (1.034–1.171) | 0.003 | 0.24 (0.029–1.953) | 0.182 |
| KRAS 1 mutated cancer | 1.42 (0.665–3.036) | 0.364 | ||
| Low EEF1A1 expression | 2.86 (1.619–5.042) | <0.001 | 2.54 (1.459–4.434) | <0.001 |
1KRAS; V-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog gene.
4. Discussion
EEF1A1 was a biomarker used to distinguish between cancer and normal tissue in our previous study, using a neural network-based feature selection algorithm. In the present study, we investigated EEF1A1 expression and its prognostic significance for patients with stage II and III colon cancer who underwent curative resection. The results revealed that EEF1A1 mRNA was decreased in tumor tissue compared to that in normal tissue. Patients with low expression of EEF1A1 showed poorer survival outcomes in terms of both DFS and OS compared to those with higher expression. The expression level of EEF1A1 was found to be an independent prognostic factor for survival outcomes. Among stage II patients not administered adjuvant treatment, a poorer OS outcome was observed for those with low EEF1A1 expression than for those with high EEF1A1 expression. Among patients with stage III colon cancer, those with low EEF1A1 expression had a shorter OS than those with high EEF1A1 expression. We determined the prognostic effect of EEF1A1 on human colon cancer. To the best of our knowledge, this is the first study to investigate the prognostic value of EEF1A1 expression in human colon cancer.
The physiological role of EEF1A1 in eukaryotic protein synthesis involves recruiting amino-acylated tRNA to the ribosome during the elongation phase of translation. It also plays various non-canonical roles including cytoskeleton modulation, protein degradation, apoptosis, and oncogenesis [12,13]. Particularly, EEF1A1 has been reported to be a pro-apoptotic protein in previous studies. Ruest et al. reported that myotube death is accelerated by the induction of the homologous gene [26], EEF1A-1/EF-1α. Borradaile et al. demonstrated that induction of EEF1A1 is involved in lipotoxic cell death secondary to oxidative stress [27]. Bosutti et al. compared the mRNA levels of EEF1A1, EEF1A2, and other pro-apoptotic genes (p66 and c-MYC) in skeletal muscles between severely traumatized patients and healthy volunteers [28]; the results showed upregulation of muscle EEF1A1 and p66 in the traumatized patient group, which was significantly related to the proteolysis rate. Thus, pro-apoptotic function is a possible mechanism underlying the protective effect of EEF1A1 against tumor development or progression. However, the tumor suppressive role of EEF1A1 in colon adenocarcinoma remains unclear. EEF1A1 expression has been determined to be independent of KRAS mutations in our study, suggesting that the expression of EEF1A1 is unlikely to involve KRAS-related colon adenocarcinoma. However, one study suggested that posttranslational changes in EEF1A1 might affect the KRAS pathway. Liu et al. suggested an association between EEF1A1 and KRAS-related tumorigenicity [29], demonstrating that neoplastic cell growth induced by oncogenic KRAS signaling may be associated with methylation of EEF1A1 at the mRNA or protein level. Additionally, the results of the current study revealed that EEF1A1 expression was associated with tumor location, and right-sided colon cancers tended to show lower expression of EEF1A1, although the correlation with tumor sidedness was not significant. The biological role of EEF1A1 in colon adenocarcinoma and its correlation with tumor sidedness will be evaluated in our next study.
Based on our results, high expression of EEF1A1 indicates a favorable survival prognosis for patients with colon cancer, and at the mRNA level, EEF1A1 was found to be downregulated in tumor tissues compared to that in normal tissues. Lin et al. revealed that EEF1A1 protein is overexpressed in estrogen/progesterone receptor (ER/PR)-positive and lymph node-negative breast cancers, which have relatively favorable outcomes compared to ER/PR-negative and lymph node-positive cases [30]. However, at the mRNA transcript level, low EEF1A1 expression was an independent poor-prognostic factor with ER/PR-positive tumors; breast cancer-specific post-transcriptional regulatory events may be responsible for this discordance between the expression of EEF1A1 mRNA and protein [30]. Further, Hassan et al. investigated the mRNA transcript levels of EEF1A isoforms across different cancers such as lung, breast, gastric, brain, prostate, liver, and colon cancers using the Oncomine and TCGA databases [31]. In colon cancer, EEF1A1 mRNA expression levels were significantly low in patients with a high risk of recurrence compared to those in patients with a low risk, which was also consistent with our findings. Interestingly, based on our results, patients who did not undergo treatment for stage II colon cancer showed differences in OS according to EEF1A1 expression. In patients with stage II disease, EEF1A1 could serve as a potential biomarker for selecting candidates who may benefit from adjuvant treatment.
In contrast to our results, studies have reported that EEF1A downregulation leads to decreased expression of pAkt1, consequently inhibiting proliferation and invasion and promoting apoptosis in HCC (Hepato cellular carcinoma) cells [16]. In stomach cancer, EEF1A1 has been reported to promote gastric cancer cell migration and invasion [21]. Such contradictory reports regarding the role of EEF1A1 in tumorigenesis may be due to the fact that it plays fundamental roles in various cellular functions [12]. Even in the same cancer, EEF1A1 may act in an opposing manner with respect to different subtypes or stages. For example, Hassan et al. suggested that higher EEF1A1 expression [31], which is otherwise a favorable biomarker for breast cancer, can be an indicator of poor OS, particularly in the basal subtype.
Our study has some limitations, such as its retrospective design. Further, the KRAS status was not verified in all populations. However, we analyzed a relatively homogeneous population, which compensates for these limitations. To the best of our knowledge, this is the first study to analyze the prognostic role of EEF1A1 in human colon cancer.
5. Conclusions
In conclusion, EEF1A1 may have a favorable prognostic effect on human colon adenocarcinoma, indicating that its loss can lead to poorer survival outcomes. Different expression levels of EEF1A protein in stages II and III of colon cancer may be independent prognostic markers of DFS and OS. Further studies are recommended to determine the mechanism underlying this correlation.
Supplementary Materials
The following are available online at https://www.mdpi.com/2077-0383/8/11/1903/s1, Table S1: Expression profile of EEF1A1.
Author Contributions
Conceptualization, E.K.J. and J.H.H. methodology, J.K., N.Y., and L.-s.M.; software, S.P. and K.K.; validation, J.S.K. and Y.-H.A.; formal analysis, E.K.J., J.K., N.Y., and L.-s.M.; investigation, J.S.K. and Y.-H.A.; resources, J.H.H. and J.H.K.; data curation, E.K.J. and J.H.H.; writing—original draft preparation, E.K.J. and J.H.H.; writing—review and editing, L.-s.M., Y.H.K., and J.H.B.; visualization, E.K.J. and J.H.H.; supervision, J.H.H. and J.H.B.; project administration, J.H.H. and J.H.B.; funding acquisition, J.H.H.
Funding
The authors wish to acknowledge the financial support of the Catholic Medical Center Research Foundation provided in the program year of 2018 and the translational R&D project through the institute for Bio-medical convergence, Incheon St. Mary’s Hospital, the Catholic University of Korea, and the Catholic medical center research foundation.
Conflicts of Interest
Sungsoo Park is an employee of Deargen Inc. The other authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Puccini A., Berger M.D., Zhang W., Lenz H.J. What We Know about Stage II and III Colon Cancer: It’s Still Not Enough. Target. Oncol. 2017;12:265–275. doi: 10.1007/s11523-017-0494-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Auclin E., Zaanan A., Vernerey D., Douard R., Gallois C., Laurent-Puig P., Bonnetain F., Taieb J. Subgroups and prognostication in stage III colon cancer: Future perspectives for adjuvant therapy. Ann. Oncol. 2017;28:958–968. doi: 10.1093/annonc/mdx030. [DOI] [PubMed] [Google Scholar]
- 4.Park S., Shin B., Shim S.W., Choi Y., Kang K., Kang K. Wx: A neural network-based feature selection algorithm for transcriptomic data. Sci. Rep. 2019;9:10500. doi: 10.1038/s41598-019-47016-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martinez-Ledesma E., Verhaak R.G., Treviño V. Identification of a multi-cancer gene expression biomarker for cancer clinical outcomes using a network-based algorithm. Sci. Rep. 2015;5:11966. doi: 10.1038/srep11966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee S., Francoeur A.M., Liu S., Wang E. Tissue-specific expression in mammalian brain, heart, and muscle of S1, a member of the elongation factor-1 alpha gene family. J. Biol. Chem. 1992;267:24064–24068. [PubMed] [Google Scholar]
- 7.Condeelis J. Elongation factor 1 alpha, translation and the cytoskeleton. Trends Biochem. Sci. 1995;20:169–170. doi: 10.1016/S0968-0004(00)88998-7. [DOI] [PubMed] [Google Scholar]
- 8.Lund A., Knudsen S.M., Vissing H., Clark B., Tommerup N. Assignment of human elongation factor 1alpha genes: EEF1A maps to chromosome 6q14 and EEF1A2 to 20q13.3. Genomics. 1996;36:359–361. doi: 10.1006/geno.1996.0475. [DOI] [PubMed] [Google Scholar]
- 9.Thornton S., Anand N., Purcell D., Lee J. Not just for housekeeping: Protein initiation and elongation factors in cell growth and tumorigenesis. J. Mol. Med. 2003;81:536–548. doi: 10.1007/s00109-003-0461-8. [DOI] [PubMed] [Google Scholar]
- 10.Abbas W., Kumar A., Herbein G. The eEF1A Proteins: At the Crossroads of Oncogenesis, Apoptosis, and Viral Infections. Front. Oncol. 2015;5:75. doi: 10.3389/fonc.2015.00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anand N., Murthy S., Amann G., Wernick M., Porter L.A., Cukier I.H., Collins C., Gray J.W., Diebold J., Demetrick D.J., et al. Protein elongation factor EEF1A2 is a putative oncogene in ovarian cancer. Nat. Genet. 2002;31:301–305. doi: 10.1038/ng904. [DOI] [PubMed] [Google Scholar]
- 12.Ejiri S. Moonlighting functions of polypeptide elongation factor 1: From actin bundling to zinc finger protein R1-associated nuclear localization. Biosci. Biotechnol. Biochem. 2002;66:1–21. doi: 10.1271/bbb.66.1. [DOI] [PubMed] [Google Scholar]
- 13.Lamberti A., Caraglia M., Longo O., Marra M., Abbruzzese A., Arcari P. The translation elongation factor 1A in tumorigenesis, signal transduction and apoptosis: Review article. Amino Acids. 2004;26:443–448. doi: 10.1007/s00726-004-0088-2. [DOI] [PubMed] [Google Scholar]
- 14.Pinke D.E., Kalloger S.E., Francetic T., Huntsman D.G., Lee J.M. The prognostic significance of elongation factor eEF1A2 in ovarian cancer. Gynecol. Oncol. 2008;108:561–568. doi: 10.1016/j.ygyno.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 15.Kulkarni G., Turbin D.A., Amiri A., Jeganathan S., Andrade-Navarro M.A., Wu T.D., Huntsman D.G., Lee J.M. Expression of protein elongation factor eEF1A2 predicts favorable outcome in breast cancer. Breast Cancer Res. Treat. 2007;102:31–41. doi: 10.1007/s10549-006-9315-8. [DOI] [PubMed] [Google Scholar]
- 16.Pecorari L., Marin O., Silvestri C., Candini O., Rossi E., Guerzoni C., Cattelani S., Mariani S.A., Corradini F., Ferrari-Amorotti G., et al. Elongation Factor 1 alpha interacts with phospho-Akt in breast cancer cells and regulates their proliferation, survival and motility. Mol. Cancer. 2009;8:58. doi: 10.1186/1476-4598-8-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tomlinson V.A., Newbery H.J., Wray N.R., Jackson J., Larionov A., Miller W.R., Dixon J.M., Abbott C.M. Translation elongation factor eEF1A2 is a potential oncoprotein that is overexpressed in two-thirds of breast tumours. BMC Cancer. 2005;5:113. doi: 10.1186/1471-2407-5-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kawamura M., Endo C., Sakurada A., Hoshi F., Notsuda H., Kondo T. The prognostic significance of eukaryotic elongation factor 1 alpha-2 in non-small cell lung cancer. Anticancer Res. 2014;34:651–658. [PubMed] [Google Scholar]
- 19.Cao H., Zhu Q., Huang J., Li B., Zhang S., Yao W., Zhang Y. Regulation and functional role of eEF1A2 in pancreatic carcinoma. Biochem. Biophys. Res. Commun. 2009;380:11–16. doi: 10.1016/j.bbrc.2008.12.171. [DOI] [PubMed] [Google Scholar]
- 20.Duanmin H., Chao X., Qi Z. eEF1A2 protein expression correlates with lymph node metastasis and decreased survival in pancreatic ductal adenocarcinoma. Hepatogastroenterology. 2013;60:870–875. doi: 10.5754/hge12869. [DOI] [PubMed] [Google Scholar]
- 21.Li X., Li J., Li F. P21 activated kinase 4 binds translation elongation factor eEF1A1 to promote gastric cancer cell migration and invasion. Oncol. Rep. 2017;37:2857–2864. doi: 10.3892/or.2017.5543. [DOI] [PubMed] [Google Scholar]
- 22.Yang S., Lu M., Chen Y., Meng D., Sun R., Yun D., Zhao Z., Lu D., Li Y. Overexpression of eukaryotic elongation factor 1 alpha-2 is associated with poorer prognosis in patients with gastric cancer. J. Cancer Res. Clin. Oncol. 2015;141:1265–1275. doi: 10.1007/s00432-014-1897-7. [DOI] [PubMed] [Google Scholar]
- 23.Scaggiante B., Dapas B., Bonin S., Grassi M., Zennaro C., Farra R., Cristiano L., Siracusano S., Zanconati F., Giansante C., et al. Dissecting the expression of EEF1A1/2 genes in human prostate cancer cells: The potential of EEF1A2 as a hallmark for prostate transformation and progression. Br. J. Cancer. 2012;106:166–173. doi: 10.1038/bjc.2011.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen S.L., Lu S.X., Liu L.L., Wang C.H., Yang X., Zhang Z.Y., Zhang H.Z., Yun J.P. eEF1A1 Overexpression Enhances Tumor Progression and Indicates Poor Prognosis in Hepatocellular Carcinoma. Transl. Oncol. 2018;11:125–131. doi: 10.1016/j.tranon.2017.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang J., Zheng C., Shao J., Chen L., Liu X., Shao J. Overexpression of eEF1A1 regulates G1-phase progression to promote HCC proliferation through the STAT1-cyclin D1 pathway. Biochem. Biophys. Res. Commun. 2017;494:542–549. doi: 10.1016/j.bbrc.2017.10.116. [DOI] [PubMed] [Google Scholar]
- 26.Ruest L.B., Marcotte R., Wang E. Peptide elongation factor eEF1A-2/S1 expression in cultured differentiated myotubes and its protective effect against caspase-3-mediated apoptosis. J. Biol. Chem. 2002;277:5418–5425. doi: 10.1074/jbc.M110685200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Borradaile N.M., Buhman K.K., Listenberger L.L., Magee C.J., Morimoto E.T., Ory D.S., Schaffer J.E. A critical role for eukaryotic elongation factor 1A-1 in lipotoxic cell death. Mol. Biol. Cell. 2006;17:770–778. doi: 10.1091/mbc.e05-08-0742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bosutti A., Scaggiante B., Grassi G., Guarnieri G., Biolo G. Overexpression of the elongation factor 1A1 relates to muscle proteolysis and proapoptotic p66(ShcA) gene transcription in hypercatabolic trauma patients. Metabolism. 2007;56:1629–1634. doi: 10.1016/j.metabol.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Liu S., Hausmann S., Carlson S.M., Fuentes M.E., Francis J.W., Pillai R., Lofgren S.M., Hulea L., Tandoc K., Lu J., et al. METTL13 Methylation of eEF1A Increases Translational Output to Promote Tumorigenesis. Cell. 2019;176:491–504. doi: 10.1016/j.cell.2018.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin C.Y., Beattie A., Baradaran B., Dray E., Duijf P.H.G. Contradictory mRNA and protein misexpression of EEF1A1 in ductal breast carcinoma due to cell cycle regulation and cellular stress. Sci. Rep. 2018;8:13904. doi: 10.1038/s41598-018-32272-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hassan M.K., Kumar D., Naik M., Dixit M. The expression profile and prognostic significance of eukaryotic translation elongation factors in different cancers. PLoS ONE. 2018;13:e0191377. doi: 10.1371/journal.pone.0191377. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.