Abstract
Cardiorespiratory fitness has been postulated as an independent predictor of several chronic diseases. We aimed to estimate the effect of Pilates on improving cardiorespiratory fitness and to explore whether this effect could be modified by a participant’s health condition or by baseline VO2 max levels. We searched databases from inception to September 2019. Data were pooled using a random effects model. The Cochrane risk of bias (RoB 2.0) tool and the Quality Assessment Tool for Quantitative Studies were performed. The primary outcome was cardiorespiratory fitness measured by VO2 max. The search identified 527 potential studies of which 10 studies were included in the systematic review and 9 in the meta-analysis. The meta-analysis showed that Pilates increased VO2 max, with an effect size (ES) = 0.57 (95% CI: 0.15–1; I2 = 63.5%, p = 0.018) for the Pilates group vs. the control and ES = 0.51 (95% CI: 0.26–0.76; I2 = 67%, p = 0.002) for Pilates pre-post effect. The estimates of the pooled ES were similar in both sensitivity and subgroup analyses; however, random-effects meta-regressions based on baseline VO2 max were significant. Pilates improves cardiorespiratory fitness regardless of the population’s health status. Therefore, it may be an efficacious alternative for both the healthy population and patients suffering from specific disorders to achieve evidenced-based results from cardiorespiratory and neuromotor exercises.
Keywords: aerobic capacity, cardiac rehabilitation, mind–body, Pilates, cardiorespiratory fitness, VO2 max, adults, prescription of exercise, systematic review, meta-analysis
1. Introduction
Strong evidence supports that higher levels of cardiorespiratory fitness (CRF) are associated with a lower risk of cardiovascular morbidity and mortality as well as all-cause mortality [1,2,3]. In addition, CRF decreases the risk of developing some specific diseases [4], such as chronic obstructive pulmonary disease (COPD) and lung or colorectal cancer [5,6], most of which are associated with a large burden of disease [7]. Furthermore, several studies have shown that higher levels of CRF may attenuate the negative association between CV risk factors and sedentary behaviours independent of physical activity [8,9,10,11]. Thus, CRF emerges as an independent predictor for several chronic diseases [12] and as a remarkable overall health status measure in different populations [12].
To improve CRF, current evidence suggests that physical exercise must reach a minimum intensity [13,14] of at least 45% oxygen uptake reserve in the general population and 70%–80% in athletes [15]. Greater improvements in maximal oxygen uptake (VO2 max) are obtained with vigorous physical exercises when compared with moderate intensity exercises [3]. Moreover, it has been suggested that some types of physical exercises that are not traditionally considered as cardiorespiratory exercises [16,17], such as Pilates, could increase CRF.
Pilates has become popular in recent years as a holistic exercise [16] focused on respiration, body control and accuracy of movements. Current evidence suggests positive effects of Pilates on respiratory muscle strength, balance, quality of life and overall physical performance [18,19,20,21,22,23,24]. These benefits are observed not only in the healthy population but also in those with specific disorders, such as chronic low back pain [16], multiple sclerosis [25], breast cancer [26] and Parkinson’s disease [27]. The neuromuscular stimulation achieved during Pilates [28] may be of sufficient intensity to improve CRF, providing benefits in VO2 max for individuals with different health conditions [29,30,31,32,33]. Thus, it seems that Pilates exercises include a mind–body component [34] that could have a beneficial impact in different populations.
However, evidence for the comparative benefits of Pilates vs. other physical exercises in terms of VO2 max remains inconclusive [22,35], and there are no studies that have evaluated oxygen consumption during Pilates sessions. Therefore, it is difficult to assess whether Pilates exercises reach the minimum intensity needed to improve CRF. We conducted this systematic review and meta-analysis to determine the effectiveness of Pilates on CRF as measured through VO2 max. Moreover, we explored whether the effect of Pilates on CRF could be modified by the participant’s health condition or baseline VO2 max level.
2. Materials and Methods
2.1. Search Strategy and Study Selection
The present review and meta-analysis were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [36] and follow the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions [37]. This study was registered through PROSPERO with registration number CRD42019124054.
We conducted a systematic literature search in the following databases: MEDLINE (via PubMed), Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE (via Scopus), Web of Science and the Physiotherapy Evidence Database (PEDro), from each database’s inception until September 2019 for studies aimed at determining the effectiveness of the Pilates method on CRF as measured through VO2 max. The search algorithm was conducted using PICO’s strategy (type of studies, participants, interventions, comparators and outcome assessment) and combined Medical Subject Headings, free-terms and matching synonyms of the following related words: (1) population: adults, “middle aged”, “young adult”; (2) intervention: Pilates, mind–body, “exercise movement techniques”; (3) outcome: “cardiorespiratory fitness”, “aerobic fitness”, “aerobic capacity”, “heart rate”; and (4) comparator: control conditions or another physical exercise. In addition, we searched the citations included in the identified publications deemed eligible for our study. The complete search strategy for MEDLINE is presented in Table 1.
Table 1.
Strategy for MEDLINE.
| Population | Intervention | Outcome |
|---|---|---|
| Adults | Pilates | “Cardiorespiratory fitness” |
| OR | OR | OR |
| Middle aged | Mind-body | “Aerobic fitness” |
| OR | OR | OR |
| Young adult | Exercise Movement Techniques (Mesh) | “Aerobic capacity” |
| OR | ||
| “Heart rate” | ||
| OR | ||
| Cardiorespiratory fitness (Mesh) |
2.2. Eligibility Criteria
Two initial reviewers (RFR and CAB) independently examined the titles and abstracts of retrieved articles to identify suitable studies. Those studies in which the title and abstract were related to the aim of the present review were included for full text request. We included studies that (1) were conducted as randomised controlled trials (RCTs), non-randomised controlled trials (non-RCTs) or pre-post studies; (2) included a mean participant age ≥18 years; (3) involved participants in any health condition; and (4) were based on at least one exercise intervention described as “Pilates” (mat, machine or both). Studies were excluded if (1) outcome measurements were not reported as VO2 max values, or (2) they were not written in English, Spanish or Portuguese. A third reviewer (VMV) resolved cases of initial reviewer disagreement.
Ethical Aspects
The present systematic review and meta-analysis were performed by collecting and analysing data from previous studies in which informed consent had been obtained by the respective original investigators. Therefore, this study was exempt from ethics approval.
2.3. Data Extraction and Quality Assessment
Two authors (RFR and CAB) independently extracted the following information from the included studies: First author’s name and year of publication; study design; characteristics of the participants included; mean age; sample size and percentage of female subjects; weekly frequency, period and modality of Pilates intervention; supervision of the intervention by a certified instructor; use of a detailed exercise protocol; the reported measurement of VO2 max; the device used to measure VO2 max; and main results. A third reviewer (VMV) resolved cases of author disagreement.
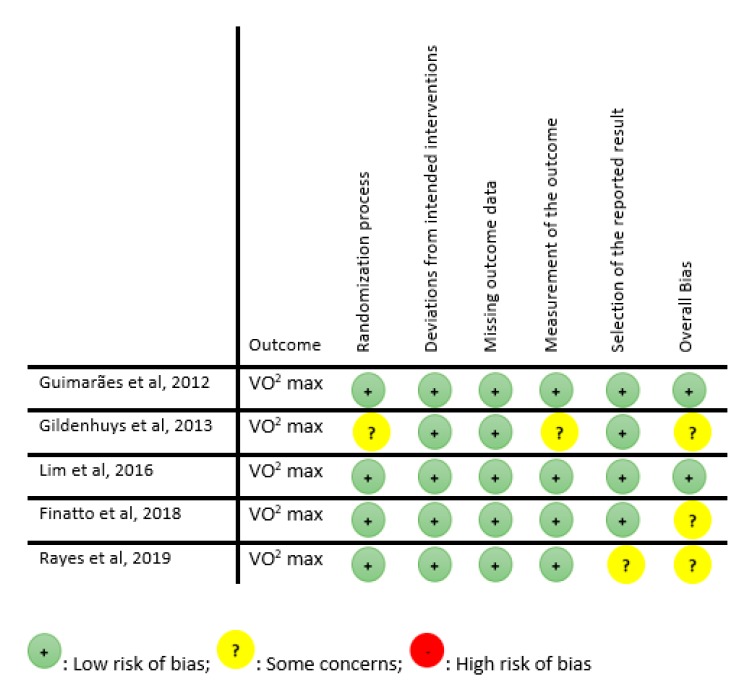
The risk of bias of RCTs was assessed using the Cochrane risk-of-bias tool for randomised trials (RoB 2.0) [38], in which five domains were evaluated: Randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Each domain was assessed for risk of bias. Studies were graded as (1) “low risk of bias” when a low risk of bias was determined for all domains; (2) “some concerns” if at least one domain was assessed as raising some concerns, but not to be at high risk of bias for any single domain; or (3) “high risk of bias” when high risk of bias was reached for at least one domain or the study judgement included some concerns in multiple domains [38].
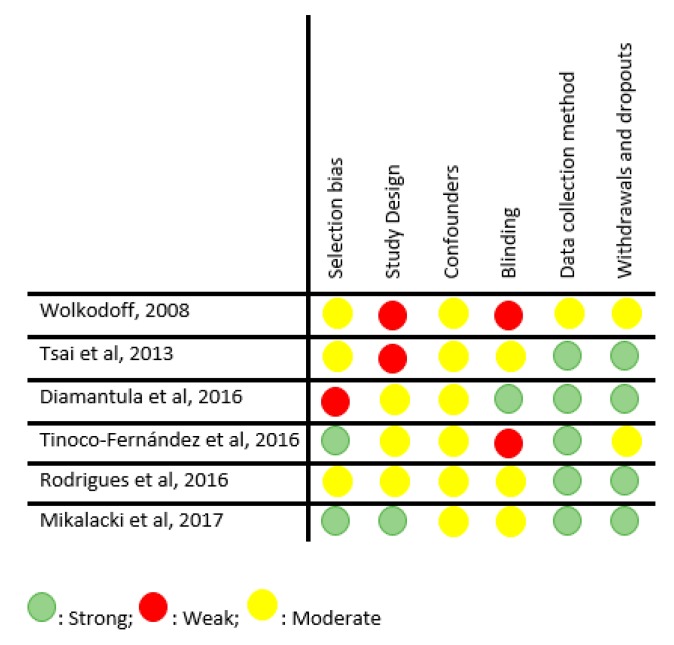
For pre-post studies and non-RCTs we used the Quality Assessment Tool for Quantitative Studies [39], in which seven domains were evaluated: Selection bias, study design, confounders, blinding, data collection methods, withdrawals and dropouts. Each domain was considered strong, moderate or weak. Studies were classified as “low risk of bias” if they presented no weak ratings; “moderate risk of bias” when there was at least one weak rating; or “high risk of bias” if there were two or more weak ratings [39].
Risk of bias was independently assessed by two reviewers (RFR and CAB). A third reviewer (VMV) was consulted in case of disagreement.
2.4. Data Analysis
Primary data extracted from each study included mean VO2 max, standard deviation of pre-post intervention and sample size. Effect sizes (ES) and related 95% confidence intervals (CIs) were calculated for each study [40]. The Dersimonian and Laird random effects method [41] was used to compute pooled ES estimates and respective 95% CIs. We estimated the pooled ES for the effect of Pilates vs. the control group (CG). The heterogeneity of results across studies was evaluated using the I2 statistic, with I2 values of 0%–30% considered “not important” heterogeneity; >30%–50% representing moderate heterogeneity; >50%–80% representing substantial heterogeneity, and >80%–100% representing considerable heterogeneity. The corresponding p-values and 95%CI for I2 were also considered [42]. Finally, we conducted two additional analyses: (i) the pre-post ES of Pilates on the intervention group (Appendix A), and (ii) the mean difference of Pilates vs. CG (Appendix B).
For all the analyses, when studies reported data on two intervention groups of Pilates, the effects of both groups were pooled in order to calculate the average effect size. Finally, when studies reported more than one intervention, we only considered the Pilates intervention for conducting this meta-analysis.
A sensitivity analysis was conducted by removing each included study to assess the robustness of the summary estimates. Further, subgroup analysis based on participants’ health status and random-effects meta-regression by baseline VO2 max values were conducted to determine their potential effect on the pooled ES estimates. Finally, publication bias was evaluated through visual inspection of funnel plots and Egger’s regression asymmetry test for the assessment of small-study effects [43]. Statistical analyses were performed using StataSE software, version 15 (StataCorp, College Station, TX, USA).
3. Results
3.1. Systematic Review
3.1.1. Study Selection
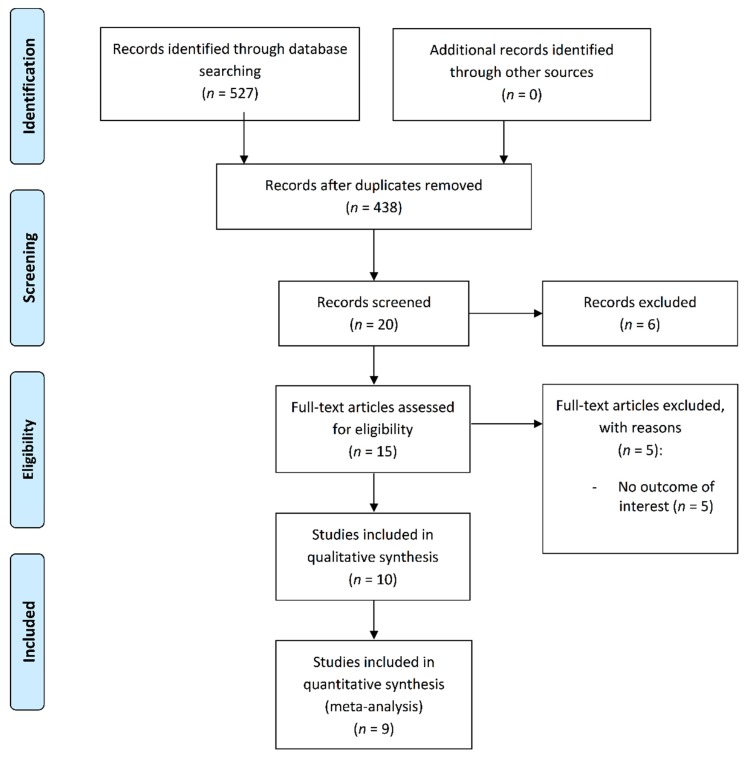
The search strategy identified 527 potential studies for inclusion. Of these, 10 studies were included in the systematic review. Only nine studies were included in the meta-analysis because one study [44] did not provide the required data to calculate ES (Figure 1).
Figure 1.
Flow of the included studies.
3.1.2. Study and Intervention Characteristics
Study and intervention characteristics are summarised in Table 2. Of the 10 included studies, five were RCTs [22,29,33,35,45], two were non-RCTs [31,44] and three were pre-post studies [30,32,46]. All the studies were conducted between 2008 and 2019 and included a total of 332 participants, of which 223 were in Pilates groups (67%) and 109 in control groups (33%). The age of the participants ranged between 18 and 66 years; four studies were conducted in women only [22,31,32,46]. Furthermore, seven studies were conducted in a healthy population, including people described in the primary studies as people without health disorders or specific pathologies [22,31] (four in sedentary individuals [30,32,44,46] and one in trained runners [33]) and three studies were conducted in populations with specific health disorders, including those described in the primary studies as suffering some diseases or specific health disorders such as heart failure [35], chronic stroke [29] and overweight/obesity [45].
Table 2.
The included studies.
| Author | Design | Participants’ Characteristics | Mean Age | Sample Size (% Female) | Frequency | Period | Type of Pilates | Certified Instructor | Detailed Protocol | Outcome Measure | Outcome Results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wolkodoff 2008 [44] | CT | Sedentary (healthy) | PG = 23–64 |
n = 20 PG = 14 (85.7%) CG = 6 (83.3%) |
40′/3.2xwk | 8wks | Both | NA | Yes | -Peak VO2 mL/kg/min (Oxycon Mobile) |
CG change = 0.38 PG change = 6.06 17% of change in PG |
| Guimarães et al., 2012 [35] | RCPT | Heart failure | PG = 46 ± 12 CRG = 44 ± 11 |
n = 16 PG = 8 (38%) CRG = 8 (19%) |
60′/2xwk | 16wks | Mat | Yes | Yes | -Peak VO2 mLO2/kg/min (Vmax 229 model, SensorMedics, Yorba Linda, CA, USA) |
PG: improvements in peak VO2 (p = 0.01) Comparing both groups, PG showed greater improvement on peak VO2 (p = 0.02) |
| Gildenhuys et al., 2013 [22] | RCT | Elderly women (healthy) | PG = 66 ± 5 CG = 65 ± 5 |
n = 50 PG = 25 (100%) CG = 25 (100%) |
60′/3xwk | 8wks | Mat | Yes | NA | -VO2 max mL.kg−1 min−1 (6minWalk; indirect equation) | PG did not significantly improve VO2 max (p = 0.247) |
| Lim HS et al., 2016 [29] | RCT | Chronic stroke | PG = 63 ± 8 CG = 62 ± 7 |
n = 20 PG = 10 (40%) CG = 10 (50%) |
3xwk | 8wks | Mat | Yes | Yes | -VO2 max mL/min -VO2 max per kg (metabolic analyzer: Quark b2, COSMED, Italy 2011) |
PG: VO2 max and VO2 max per kg increased significantly CG: VO2 max per kg diminished significantly |
| Diamantoula et al., 2016 [46] | Q-E | Sedentary women (healthy) | PG = 26 ± 5 AP = 21.3 ± 2 |
PG land = 20 (100%) AP = 20 (100%) |
2xwk | 2years | Mat/aqua | NA | NA | -VO2 max mL/min (Ergometer cycle (Amila kh803), following the Astrand-Ryhming test, based on heart rate in submaximal effort) | No differences between groups, better VO2 max in total for both groups |
| Tinoco- Fernández et al., 2016 [30] | Q-E | Sedentary students (healthy) | PG = 18–35 |
n = 45 PG = 45 (78%) |
60′/3xwk | 10wks | Mat | Yes | Yes | -VO2 max L/kg/min -VO2 max L/min (MasterScreen CPX apparatus) |
Increment in peak VO2 and VO2 max |
| Rodrigues et al., 2016 [32] | Q-E | Sedentary women (healthy) | PG = 23 ± 2 | PG = 10 (100%) | 45′/2xwk | 11wks | Both | NA | Yes | -VO2 max mL.kg−1 min−1 portable metabolic system (VO2000®, MedGraphics®, St. Paul, MN, USA) |
Peak VO2 tended to increase, but the differences were not statistically significant |
| Mikalacki et al., 2017 [31] | CT | Adult women (healthy) | PG = 48 ± 7 CG = 47 ± 7 |
n = 64 PG = 36 (100%) CG = 28 (100%) |
55–60′/2xwk | NA | NA | NA | NA | -Relative VO2 max -Absolute VO2 max (Medisoft, model 870c) |
PG: significant increase on relative VO2max, absolute VO2 max -CG: not significant changes |
| Finatto et al., 2018 [33] | RCT | Trained runners (healthy) | PG = 18 ± 1 CG = 18 ± 1 |
n = 32 PG = 15–13 NA % CG = 16–15 |
60′/1xwk | 12wks | Mat | Yes | NA | -VO2 max mL.kg−1.min−1 (VO2000 (Medgraphics, Ann Arbor, USA) |
PG: significantly higher values on VO2 max (p < 0.001) |
| Rayes et al., 2019 [45] | RCT | Overweight/obese | PG = 55.9 ± 6.6 CG = 45.5 ± 9.3 |
n = 60 NA% PG = 22 CG = 25/17 |
60′/3xwk | 8wks | Both | Yes | Yes | -VO2 max (mL/kg/min) (motorized treadmill; Inbrasport, ATL, Porto Alegre, Brazil) |
PG: Significant improvement on VO2 max CG: not significant changes |
CT: controlled trial; RCT: randomised controlled trial; RCPT: randomised controlled pilot trial; Q-E: quasi-experimental; PG: Pilates group; CG: control group; AP: Aqua-Pilates group; NA: not available; wk: week; VO2 max: maximal oxygen uptake.
In control groups, participants were encouraged to continue with their routine physical activity or to obtain conventional treatment. Among control groups, two studies did not allow structured physical exercise [22,45]; one did not describe the control group activity [31]; and one performed the running conventional program [33] and two studies the conventional rehabilitation programs [29,35].
Concerning the characteristics of the Pilates interventions, the majority of studies consisted of two or three 40–60 min sessions, three times per week, over 8–16 weeks. The mean attendance at the Pilates sessions was 88.2% (80%–100%). Among the 10 studies, six described the Pilates intervention as Pilates mat [22,29,30,33,35,46], three studies combined both modalities (mat and machine) [32,44,45] and one did not report the Pilates modality [31]. Moreover, six studies were conducted by a certified instructor [22,29,30,33,35,45] or with a detailed exercise protocol [29,30,32,34,44,45].
The outcome, VO2 max, was directly measured in nine studies (two with a cycloergometer and seven with a treadmill) [29,30,31,32,33,35,45,46,47] and one study [22] used an algorithm based on heart rate to estimate VO2 max values. The studies assessed participants at the end of the Pilates intervention, an no study measured VO2 max during the Pilates session.
3.1.3. Quality Assessment and Risk of Bias
Five RCTs were assessed according to the RoB 2.0 tool [38], of which two were assessed as “low risk of bias” and three as “some concerns” (Figure 2). The remaining five studies (non-RCTs and pre-post studies) were assessed according to the Quality Assessment Tool for Quantitative Studies [39], of which two were classified as “low risk of bias”, two as “moderate risk of bias” and one as high risk of bias (Figure 3).
Figure 2.
Quality assessment for RCT (RoB 2.0).
Figure 3.
Quality assessment for non-RCT.
3.2. Data Synthesis
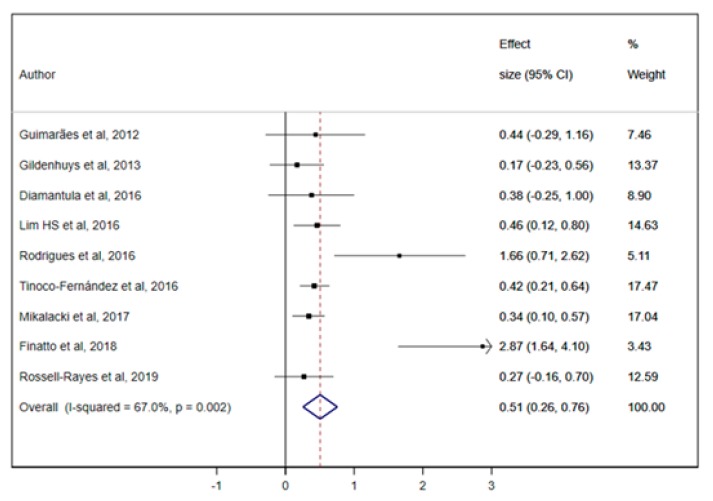
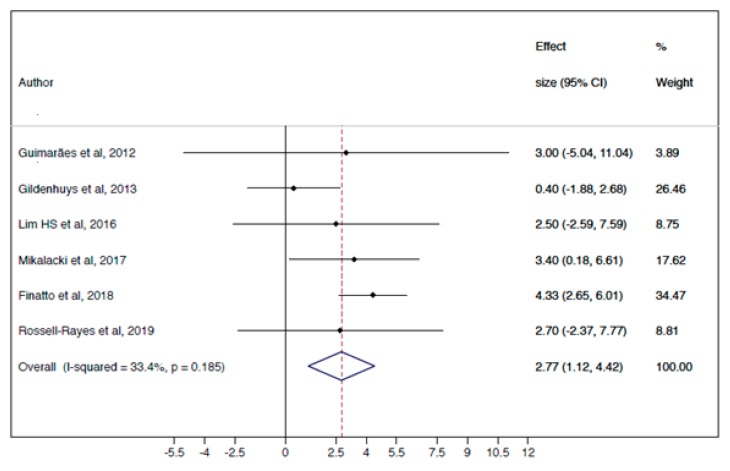
3.2.1. Meta-Analysis
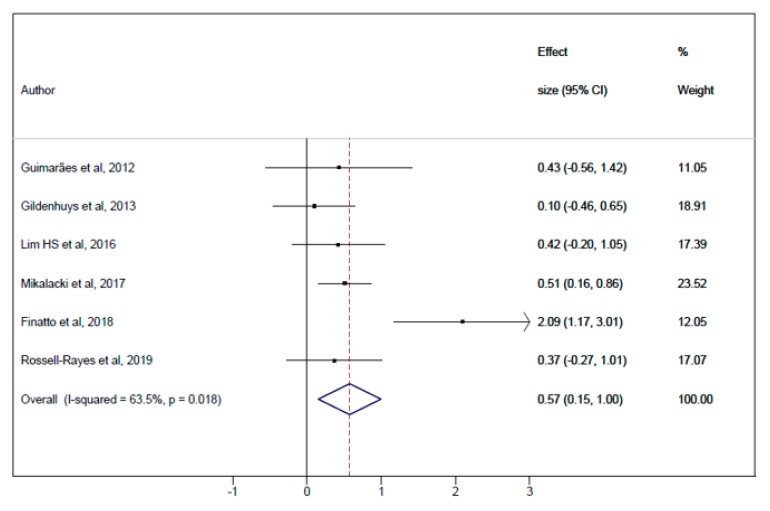
The pooled ES for the effect of Pilates vs. CG on CRF was 0.57 (95% CI: 0.15–1.00; I2 = 63.5%, p = 0.02) (Figure 4) and for Pilates pre-post ES was 0.51 (95% CI: 0.26–0.76; I2 = 67%, p < 0.01) (Figure A1, Appendix A). The mean difference analysis of Pilates vs. CG was 2.77 (95% CI: 1.12–4.42; I2 = 33.4%, p = 0.19) (Figure A3, Appendix B).
Figure 4.
Meta-analysis for Pilates Method vs. control group (pooled ES analysis).
3.2.2. Sensitivity and Meta-Regression Analyses
After removing studies from the analyses individually, none substantially modified the pooled ES estimate in Pilates vs. CG (Table 3), Pilates pre-post effect on intervention (Table A1, Appendix A) and mean difference of Pilates vs. CG. (Table A5, Appendix B). The subgroup analyses by participants’ health conditions modified the pooled ES estimate for Pilates vs. CG (Table 4) and mean difference of Pilates vs. CG (Table A6, Appendix B), but not for Pilates pre-post effect on intervention (Table A2, Appendix A).
Table 3.
Sensitivity analyses.
| Pilates Method vs. Control Author, Year | ES | LL | UL | I2 |
|---|---|---|---|---|
| Guimarães et al., 2012 [35] | 0.6 | 0.12 | 1.08 | 70.8 |
| Gildenhuys et al., 2013 [22] | 0.69 | 0.20 | 1.18 | 64.4 |
| Lim HS et al., 2016 [29] | 0.62 | 0.10 | 1.14 | 70.7 |
| Mikalacki et al., 2017 [31] | 0.62 | 0.03 | 1.22 | 70.8 |
| Finatto et al., 2018 [33] | 0.4 | 0.16 | 0.64 | 0 |
| Rossell-Rayes et al., 2019 [45] | 0.63 | 0.12 | 1.15 | 70.4 |
ES: Effect size; LL: Lower limit; UL: Upper limit.
Table 4.
Subgroup analyses by participants’ health status.
| Pilates Method vs. Control | ||||
|---|---|---|---|---|
| ES | LL | UL | I2 | |
| Healthy | 0.80 | −0.05 | 1.65 | 85 |
| Unhealthy | 0.40 | −0.01 | 0.81 | 0 |
ES: Effect size; LL: Lower limit; UL: Upper limit.
The random-effects meta-regression models by VO2 max baseline levels were significant for Pilates vs. CG (p = 0.03) (Table 5) and for Pilates pre-post effect on intervention (p = 0.05) (Table A3, Appendix A) but not for mean difference of Pilates vs. CG (p = 0.08) (Table A7, Appendix B).
Table 5.
Meta-regression analyses by VO2 max baseline values.
| Coefficient | p | |
|---|---|---|
| Pilates Method vs. control | 0.04 | 0.03 * |
VO2 max: Maximal oxygen uptake (mL/kg/min); * Significant at p ≤ 0.05.
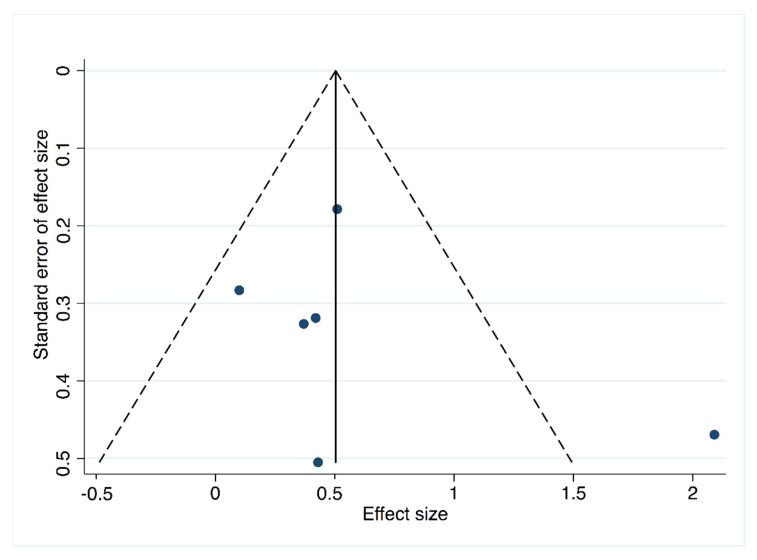
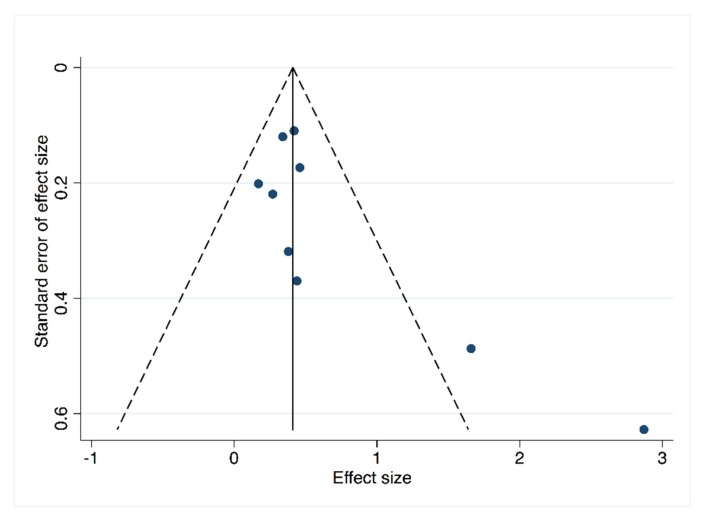
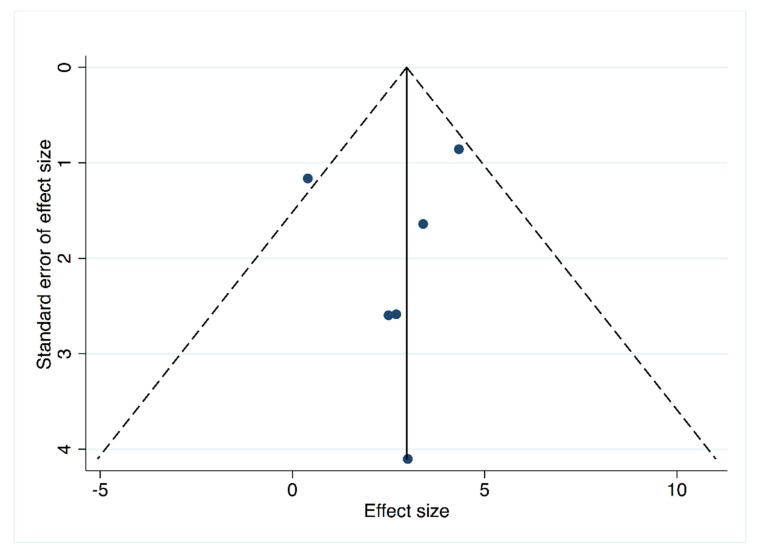
3.2.3. Publication Bias
A significant publication bias was not found in Pilates vs. CG studies, as evidenced by both the funnel plot (Figure 5) asymmetry and an Egger’s test (p = 0.465) (Table 6), nor in the mean difference of Pilates vs. CG by funnel plot asymmetry (Figure A4, Appendix B) and an Egger’s test (p = 0.69) (Table A8, Appendix B). However, in Pilates pre-post effect studies publication bias was found (p = 0.07) (Table A4, Appendix A).
Figure 5.
Funnel plot for Pilates vs control group.
Table 6.
Publication bias by Egger’s test.
| Coefficient | p-Value | |
|---|---|---|
| Pilates method vs. control group | 1.64 | 0.47 |
4. Discussion
This systematic review and meta-analysis were performed to determine the effectiveness of Pilates interventions for improvement of CRF measured through VO2 max. Our findings highlight that Pilates is an alternative exercise to improve VO2 max values. Furthermore, our results were substantially modified by participants’ health conditions for Pilates vs. control group analyses but not for Pilates pre-post effect on intervention; otherwise, baseline VO2 max values could influence CRF improvement.
Although some studies [22,35,45,46] have failed to show significant changes in CRF after Pilates intervention, no study has reported negative effects of Pilates on the CRF levels, and therefore the positive clinical implications should not be underestimated. Additionally, more significant benefits of Pilates on CRF were achieved when other activities, such as running, were included [33] and this could be explained through a synergistic relationship between these training methods.
Evidence suggests that people with lower levels of CRF are more sensitive to improvement of this parameter [47]. Accordingly, in our study estimates of pooled ES were higher in those studies in which participants had lower baseline CRF levels, such as people with health disorders. Conversely, our meta-regression analyses suggested that higher levels of VO2 max at baseline are related with higher ES of the Pilates intervention. These findings should cautiously be interpreted since they may indicate that the effect of Pilates in those studies with higher VO2 max levels at baseline were distortedly overestimated. Probably these biased estimates were a consequence of reporting results in absolute terms (change in VO2 max in ml) instead of in relative terms (percentage of increase in VO2 max), but could have clinical implications suggesting that Pilates exercise is an effective rehabilitation strategy for several disorders, including some cardiac pathologies. Moreover, Pilates exercise showed high compliance levels indicating that it may be better tolerated than the aerobic exercises typically employed in rehabilitation programs.
Three potential sources of improvement may explain the positive impact of Pilates intervention on CRF: Strengthening of the lumbopelvic region, increased flexibility of the ribcage and breathing exercises. First, the strengthening of lumbopelvic and core muscles induced by Pilates may produce a more efficient movement pattern in upper and lower limbs, as well as greater strength in expiratory muscles [19,33]. Second, due to the flexibility improvement, a more efficient mobility pattern of the ribcage may be achieved [30]. Finally, the breathing techniques adopted during Pilates training may increase lung capacity [29] and functionality of intercostal muscles [17]. On these bases, improved ventilation efficiency would be achieved, resulting in a higher flow of oxygenated blood into muscle tissues [35], enhanced local circulation [19,30] and muscle oxidative capacity [45], and less energy waste. Therefore, Pilates could reach the minimum intensity required to improve CRF [13,14] although no published study has verified this.
Our systematic review and meta-analysis present some limitations that must be stated. First, it was not possible to blind Pilates interventions and some of the included studies did not provide details about the randomisation sequence or allocation concealment. Second, considerable levels of heterogeneity were observed in the analyses, and we cannot omit this fact. Third, the heterogeneity of participants’ health conditions and the dose and intensity of the Pilates intervention could potentially affect our estimates. Fourth, significant publication bias was evidenced by Egger’s test and unpublished results could modify the findings of the present meta-analysis. Fifth, it should be highlighted the difficulty to comply with a full training program by very busy professionals, thus, this concern should not be neglected in the implementation of our results. Sixth, rarely it is possible to measure VO2 max directly in clinical settings, thus other more applicable procedures for indirect measurement of VO2 max should be used. Seventh, although subgroup analyses by participants’ health conditions modified the ES estimates, these results should be cautiously considered due to the lack of studies in each subgroup. Finally, due to the lack of long-term assessments, we could not determine whether the benefits to CRF measured through VO2 max are preserved over time. Therefore, our results should be cautiously considered.
5. Conclusions
In summary, our results support Pilates as an effective intervention to improve CRF in both healthy people and individuals with disorders related to aerobic capacity. Despite this, further studies should be conducted, including short- and long-term measurements to determine the intensity level reached by VO2 max during Pilates intervention and whether CRF improvement is preserved over time.
Acknowledgments
We are grateful to Movi-fitness, FSE and JCCM for the fellowship contract of R.F.-R.
Appendix A
Analyses for Pilates pre-post effect on intervention (A1–A6: Meta-analysis, sensitivity analysis, subgroup analysis, meta-regression, publication bias and funnel plot).
AppendixFigure A1. Meta-analysis.
Figure A1.
Meta-analysis for Pilates pre-post effect on intervention.
AppendixTable A1. Sensitivity analysis.
Table A1.
Sensitivity analyses for Pilates pre-post effect on intervention.
| Pilates Method Intervention | ||||
|---|---|---|---|---|
| Author, Year | ES | LL | UL | I2 |
| Guimarães et al., 2012 [35] | 0.52 | 0.25 | 0.79 | 71.1 |
| Gildenhuys et al., 2013 [22] | 0.57 | 0.29 | 0.84 | 69.1 |
| Diamantoula et al., 2016 [46] | 0.53 | 0.25 | 0.80 | 71.1 |
| Lim HS et al., 2016 [29] | 0.53 | 0.24 | 0.83 | 71 |
| Rodrigues et al., 2016 [32] | 0.43 | 0.20 | 0.65 | 60.1 |
| Tinoco-Fernández et al., 2016 [30] | 0.56 | 0.24 | 0.89 | 71.1 |
| Mikalacki et al., 2017 [31] | 0.57 | 0.26 | 0.89 | 70.5 |
| Finatto et al., 2018 [33] | 0.39 | 0.24 | 0.54 | 19.6 |
| Rossell-Rayes et al., 2019 [45] | 0.55 | 0.27 | 0.83 | 70.6 |
ES: Effect Size; LL: Lower Limit; UL: Upper limit.
AppendixTable A2. Subgroup analysis.
Table A2.
Subgroup analyses by participants’ health status.
| Pilates Method Intervention | ||||
|---|---|---|---|---|
| ES | LL | UL | I2 | |
| Healthy | 0.64 | 0.26 | 1.02 | 78.9 |
| Unhealthy | 0.39 | 0.14 | 0.64 | 0 |
ES: Effect Size; LL: Lower Limit; UL: Upper limit.
AppendixTable A3. Random effect meta-regression by baseline VO2 max values.
Table A3.
Meta-regression analysis by VO2 max baseline values.
| Coefficient | p-Value | |
|---|---|---|
| Pilates Method intervention | 0.05 | 0.05 * |
VO2 max: Maximal oxygen uptake (mL/kg/min); * Significant at p ≤ 0.05.
AppendixTable A4. Publication bias (table).
Table A4.
Publication bias by Egger’s test.
| Coefficient | p-Value | |
|---|---|---|
| Pilates Method intervention | 2.19 | 0.07 * |
* Significant at p < 0.1.
AppendixFigure A2. Funnel plot (figure).
Figure A2.
Funnel plot for Pilates pre-post effect on intervention.
Appendix B. Mean Difference Analyses for Pilates vs. CG (B1–B6: Meta-Analysis, Sensitivity Analysis, Subgroup Analysis, Meta-Regression, Publication Bias and Funnel Plot)
AppendixFigure A3. Meta-analysis.
Figure A3.
Meta-analysis for Pilates vs. control group (mean difference).
AppendixTable A5. Sensitivity analysis.
Table A5.
Sensitivity analyses for Pilates vs. control group.
| Pilates vs. Control Group | |||
|---|---|---|---|
| Author, Year | MD | 95% CI | I2 |
| Guimarães et al., 2012 [35] | 2.24 | 0.89, 4.58 | 46.7 |
| Gildenhuys et al., 2013 [22] | 3.88 | 2.53, 5.24 | 0.0 |
| Lim HS et al., 2016 [29] | 2.77 | 0.85, 4.69 | 46.5 |
| Mikalacki et al., 2017 [31] | 2.59 | 0.48, 4.69 | 46.2 |
| Finatto et al., 2018 [33] | 1.71 | 0.09, 3.33 | 0.0 |
| Rossell-Rayes et al., 2019 [45] | 2.25 | 0.82, 4.67 | 46.7 |
MD: Mean difference; CI: Confidence interval.
AppendixTable A6. Subgroup analysis.
Table A6.
Subgroup analyses by participants’ health status.
| Pilates vs. Control Group | MD | 95% CI |
|---|---|---|
| Healthy | 2.77 | 1.12, 4.42 |
| Unhealthy | 2.67 | −0.61, 5.95 |
MD: Mean difference; CI: Confidence interval.
AppendixTable A7. Random effect meta-regression by baseline VO2 max values.
Table A7.
Meta-regression analysis by VO2 max baseline values.
| Coefficient | p-Value | |
|---|---|---|
| Pilates vs. control group | 0.09 | 0.08 |
VO2 max: Maximal oxygen uptake (mL/kg/min).
AppendixTable A8. Publication bias (table).
Table A8.
Publication bias by Egger’s test.
| Coefficient | p-Value | |
|---|---|---|
| Pilates vs. control group | −0.50 | 0.69 |
AppendixFigure A4. Funnel plot (figure).
Figure A4.
Funnel plot for Pilates vs. control group (mean difference).
Author Contributions
Conceptualization, R.F.-R. and I.C.-R.; methodology, R.F.-R., C.Á.-B. and I.C.-R.; software, I.C.-R.; validation, A.I.T.-C. and A.F.-M.; formal analysis, R.F.-R.; investigation, R.F.-R. and A.I.T.-C.; resources, R.F.-R. and A.F.-M.; data curation, C.Á.-B. and V.M.-V.; writing—original draft preparation, R.F.-R. and C.Á.-B.; writing—review and editing, V.M.-V.; visualization, A.I.T.-C. and A.F.-M.; supervision, V.M.-V. and C.Á.-B.
Funding
This study was funded by Apadrina la Ciencia.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Blair S.N., Kohl H., III, Paffenbarger R.J., Clark D.G., Cooper K.H., Gibbons L.W. Physical Fitness and All-Cause Mortality. Jama. 1989;262:2395–2401. doi: 10.1001/jama.1989.03430170057028. [DOI] [PubMed] [Google Scholar]
- 2.Blair J.B., Kampert H.W., Kohl C.E., III, Barlow C.A., Macera R.S., Paffenbarger L.W., Jr., Gibbons S.N. The Influences of cardiovascular fitness and other precursers on cardiovascular disease and all-cause mortality in men and women. Aerobics center longitudinal study. J. Am. Med. Assoc. 1996;276:205–210. doi: 10.1001/jama.1996.03540030039029. [DOI] [PubMed] [Google Scholar]
- 3.Garber C.E., Blissmer B., Deschenes M.R. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 4.Croci I., Coombes J.S., Sandbakk S.B. Non-alcoholic fatty liver disease: Prevalence and all-cause mortality according to sedentary behaviour and cardiorespiratory fitness. The HUNT Study. Prog. Cardiovasc. Dis. 2019;62:127–134. doi: 10.1016/j.pcad.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Pozuelo-Carrascosa D.P., Alvarez-Bueno C., Cavero-Redondo I., Morais S., Lee I.M., Martínez-Vizcaíno V. Cardiorespiratory fitness and site-specific risk of cancer in men: A systematic review and meta-analysis. Eur. J. Cancer. 2019;113:58–68. doi: 10.1016/j.ejca.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Steell L., Ho F.K., Sillars A. Dose-response associations of cardiorespiratory fitness with all-cause mortality and incidence and mortality of cancer and cardiovascular and respiratory diseases: The UK Biobank cohort study. Br. J. Sports Med. 2019;53:1371–1378. doi: 10.1136/bjsports-2018-099093. [DOI] [PubMed] [Google Scholar]
- 7.Mathers C.D., Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:2011–2030. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davidson T., Vainshelboim B., Kokkinos P., Myers J., Ross R. Cardiorespiratory fitness versus physical activity as predictors of all-cause mortality in men. Am. Heart J. 2018;196:156–162. doi: 10.1016/j.ahj.2017.08.022. [DOI] [PubMed] [Google Scholar]
- 9.Lavie C.J., Wisløff U., Després J.-P. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement From the American Heart Association. Circulation. 2016;134:e653–e659. doi: 10.1161/cir.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 10.Kodama S. Cardiorespiratory Fitness as a Quantitative Predictor of All-Cause Mortality and Cardiovascular Events. J. Am. Med. Assoc. 2009;301:2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 11.Lee C.D., Blair S.N., Jackson A.S. Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men. Am. J. Clin. Nutr. 1999;69:373–380. doi: 10.1093/ajcn/69.3.373. [DOI] [PubMed] [Google Scholar]
- 12.Harber M.P., Kaminsky L.A., Arena R. Impact of Cardiorespiratory Fitness on All-Cause and Disease-Specific Mortality: Advances Since 2009. Prog. Cardiovasc. Dis. 2017;60:11–20. doi: 10.1016/j.pcad.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 13.American College of Sports Medicine American College of Sports Medicine Position Stand. Med. Sci. Sport Exerc. 1998;30:975–991. doi: 10.1249/01.MSS.0000115224.88514.3A. [DOI] [PubMed] [Google Scholar]
- 14.Pescatello L., Arena R., Riebe D., Thompson P. ACSM’s Guidelines for Exercsie Testing and Prescription. 9th ed. Wolters Kluwer Health; Philadelphia, PA, USA: 2014. pp. 269–299. [Google Scholar]
- 15.Swain D.P., Franklin B.A. VO(2) reserve and the minimal intensity for improving cardiorespiratory fitness. Med. Sci. Sport Exerc. 2002;34:152–157. doi: 10.1097/00005768-200201000-00023. [DOI] [PubMed] [Google Scholar]
- 16.Eliks M., Zgorzalewicz-Stachowiak M., Zeńczak-Praga K. Application of Pilates-based exercises in the treatment of chronic non-specific low back pain: State of the art. Postgrad. Med. J. 2019;95:41–45. doi: 10.1136/postgradmedj-2018-135920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lau C., Yu R., Woo J. Effects of a 12-Week hatha yoga intervention on cardiorespiratory endurance, muscular strength and endurance, and flexibility in Hong Kong Chinese Adults: A controlled clinical trial. Evid. Based Complement. Altern Med. 2015;2015:958727. doi: 10.1155/2015/958727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Souza R.O.B., de Faria Marcon L., de Arruda A.S.F., Pontes Junior F.L., de Melo R.C. Effects of Mat Pilates on Physical Functional Performance of Older Adults. Am. J. Phys. Med. Rehabil. 2018;97:414–425. doi: 10.1097/PHM.0000000000000883. [DOI] [PubMed] [Google Scholar]
- 19.De Alvarenga G.M., Charkovski S.A., Dos Santos L.K., da Silva M.A.B., Tomaz G.O., Gamba H.R. The influence of inspiratory muscle training combined with the Pilates method on lung function in elderly women: A randomized controlled trial. Clinics. 2018;73:e356. doi: 10.6061/clinics/2018/e356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sarmento L.A., Pinto J.S.S.T., da Silva A.P.P., Cabral C.M.N., Chiavegato L.D. Effect of conventional physical therapy and Pilates in functionality, respiratory muscle strength and ability to exercise in hospitalized chronic renal patients: A randomized controlled trial. Clin Rehabil. 2017;31:508–520. doi: 10.1177/0269215516648752. [DOI] [PubMed] [Google Scholar]
- 21.Tozim B.M., Navega M.T. Effect of pilates method on inspiratory and expiratory muscle strength in the elderly. Rev. Bras. Cineantropometria Desempenho Hum. 2018;20:1–9. doi: 10.5007/1980-0037.2018v20n1p1. [DOI] [Google Scholar]
- 22.Gildenhuys G., Fourie M., Shaw I., Shaw B., Toriola A., Witthuhn J. Evaluation of Pilates training on agility, functional mobility and cardiorespiratory fitness in elderly women: Health and fitness. Afr. J. Phys. Act. Health Sci. 2013;19:505–512. [Google Scholar]
- 23.Irez G.B., Ozdemir R.A., Evin R., Irez S.G., Korkusuz F. Integrating pilates exercise into an exercise program for 65+ year-old women to reduce falls. J. Sport Sci. Med. 2011;10:105–111. [PMC free article] [PubMed] [Google Scholar]
- 24.De Siqueira Rodrigues B.G., Ali Cader S., Bento Torres N.V.O., de Oliveira E.M., Martin Dantas E.H. Pilates method in personal autonomy, static balance and quality of life of elderly females. J. Bodyw. Mov. Ther. 2010;14:195–202. doi: 10.1016/j.jbmt.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 25.Sánchez-Lastra M.A., Martínez-Aldao D., Molina A.J., Ayán C. Pilates for people with multiple sclerosis: A systematic review and meta-analysis. Mult. Scler. Relat. Disord. 2019;28:199–212. doi: 10.1016/j.msard.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 26.Espíndula R.C., Nadas G.B., Rosa M.I.D., Foster C., Araújo F.C.D., Grande A.J. Pilates for breast cancer: A systematic review and meta-analysis. Rev Assoc Med. Bras. 2006;63:1006–1011. doi: 10.1590/1806-9282.63.11.1006. [DOI] [PubMed] [Google Scholar]
- 27.Mollinedo-Cardalda I., Cancela-Carral J.M., Vila-Suárez M.H. Effect of a Mat Pilates Program with TheraBand on Dynamic Balance in Patients with Parkinson’s Disease: Feasibility Study and Randomized Controlled Trial. Rejuvenation Res. 2017;21:423–430. doi: 10.1089/rej.2017.2007. [DOI] [PubMed] [Google Scholar]
- 28.Teixeira de Carvalho F., de Andrade Mesquita L.S., Pereira R., Neto O.P., Amaro Zangaro R. Pilates and Proprioceptive Neuromuscular Facilitation Methods Induce Similar Strength Gains but Different Neuromuscular Adaptations in Elderly Women. Exp. Aging Res. 2017;43:440–452. doi: 10.1080/0361073X.2017.1369624. [DOI] [PubMed] [Google Scholar]
- 29.Lim H.S., Kim Y.L., Lee S.M. The effects of Pilates exercise training on static and dynamic balance in chronic stroke patients: A randomized controlled trial. J. Phys. Ther. Sci. 2016;28:1819–1824. doi: 10.1589/jpts.28.1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tinoco-Fernández M., Jiménez-Martín M., Sánchez-Caravaca M.A., Fernández-Pérez A.M., Ramírez-Rodrigo J., Villaverde-Gutiérrez C. The Pilates method and cardiorespiratory adaptation to training. Res. Sport Med. 2016;24:281–286. doi: 10.1080/15438627.2016.1202829. [DOI] [PubMed] [Google Scholar]
- 31.Mikalački M., Čokorilo N., Ruiz-Montero P.J. The effects of a pilates-aerobic program on maximum exercise capacity of adult women. Rev. Bras. Med. Esporte. 2017;23:246–249. doi: 10.1590/1517-869220172303156004. [DOI] [Google Scholar]
- 32.Rodrigues A.Q., Martins F.M., Barbosa A.C., Figueiredo P.S., Lima M.O., Vieira E.R. Effects of an eleven-week pilates exercise program on progressive-speed walking capacity in sedentary young women: A pilot study. Hum. Mov. 2016;17:102–106. doi: 10.1515/humo-2016-0011. [DOI] [Google Scholar]
- 33.Finatto P., Da Silva E.S., Okamura A.B., Almada B.P., Oliveira H.B., Peyre-Tartaruga L.A. Pilates training improves 5-km run performance by changing metabolic cost and muscle activity in trained runners. PLoS ONE. 2018;13:e0194057. doi: 10.1371/journal.pone.0194057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wells C., Kolt G.S., Bialocerkowski A. Defining Pilates exercise: A systematic review. Complement. Ther. Med. 2012;20:253–262. doi: 10.1016/j.ctim.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 35.Guimarães G.V., Carvalho V.O., Bocchi E.A., d’Avila V.M. Pilates in Heart Failure Patients: A Randomized Controlled Pilot Trial. Cardiovasc. Ther. 2012;30:351–356. doi: 10.1111/j.1755-5922.2011.00285.x. [DOI] [PubMed] [Google Scholar]
- 36.Moher D., Liberati A., Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement (Chinese edition) J. Chinese Integr. Med. 2009;7:889–896. doi: 10.3736/jcim20090918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Higgins J.P.T., Green S. The Cochrane Collaboration; 2011. [(accessed on 22 October 2019)]. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) Available online: http://crtha.iums.ac.ir/files/crtha/files/cochrane.pdf. [Google Scholar]
- 38.Sterne J.A.C., Savović J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., Cates C.J., Cheng H.-Y., Corbett M.S., Eldridge S.M., et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ Effect. Public Health Pract. Proj. 1998:2–5. doi: 10.1136/bmj.l4898. in press. [DOI] [PubMed] [Google Scholar]
- 39.Armijo-Olivo S., Stiles C.R., Hagen N.A., Biondo P.D., Cummings G.G. Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological research. J. Eval. Clin. Pract. 2012;18:12–18. doi: 10.1111/j.1365-2753.2010.01516.x. [DOI] [PubMed] [Google Scholar]
- 40.Thalheimer W., Cook S. How to calculate effect sizes from published research articles: A simplified methodology. Work Res. 2002;1:1–9. doi: 10.1113/jphysiol.2004.078915. [DOI] [Google Scholar]
- 41.Schwarzer G. In: Methods for Meta-analysis in Medical Research. Sutton A.J., Abrams K.R., Jones D.R., Sheldon T.A., Song F., editors. Wiley; Chichester, UK: 2000. No. of pages: Xvii+317. Statist. Med. 2003, 22, 3112–3114. [DOI] [Google Scholar]
- 42.Higgins J.P.T., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 43.Sterne J.A.C., Egger M., Smith G.D. Investigating and dealing with publication and other biases in meta-analysis. Br. Med. J. 2001;323:101–105. doi: 10.1136/bmj.323.7304.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wolkodoff N., Peterson S., Miller J. The Fitness Effects of A Combined Aerobic and Pilates Program An Eight-Week Study Using The Stamina AeroPilates Pro XP555. AeroPilates Pro XP 555 Study. 2008 doi: 10.5897/ERR2014.1790. [DOI] [Google Scholar]
- 45.Rayes A.B.R., de Lira C.A.B., Viana R.B. The effects of Pilates vs. aerobic training on cardiorespiratory fitness, isokinetic muscular strength, body composition, and functional tasks outcomes for individuals who are overweight/obese: A clinical trial. PeerJ. 2019;7:e6022. doi: 10.7717/peerj.6022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Diamantoula P., Nikolaos A., Helen S. Aqua pilates versus land pilates: Physical fitness outcomes. J. Phys. Educ. Sport. 2016;16:573–578. doi: 10.7752/jpes.2016.02090. [DOI] [Google Scholar]
- 47.Daussin F.N., Ponsot E., Dufour S.P. Improvement of VO2max by cardiac output and oxygen extraction adaptation during intermittent versus continuous endurance training. Eur. J. Appl. Physiol. 2007;101:377–383. doi: 10.1007/s00421-007-0499-3. [DOI] [PubMed] [Google Scholar]