Abstract
Background
Worry about deportation has been associated with cardiovascular disease risk factors in cross‐sectional research. No research has evaluated this association longitudinally or examined the association between deportation worry and incident cardiovascular disease outcomes.
Methods and Results
We used data from an ongoing community‐based cohort of 572 women primarily of Mexican origin. We estimated associations between self‐reported deportation worry and: (1) trajectories of blood pressure, body mass index, and waist circumference with linear mixed models, and (2) incident hypertension with Cox proportional hazards models. Nearly half (48%) of women reported “a lot,” 24% reported “moderate,” and 28% reported “not too much” deportation worry. Higher worry at baseline was associated with nonlinear systolic blood pressure and mean arterial pressure trajectories. For example, compared with not too much worry, a lot of worry was associated with a faster initial increase (β, interaction with linear year term: 4.10; 95% CI, 1.17–7.03) followed by a faster decrease in systolic blood pressure (β, interaction with quadratic year term: −0.80; 95% CI, −1.55 to −0.06). There was weak evidence of an association between deportation worry and diastolic blood pressure and no association with body mass index, waist circumference, or pulse pressure trajectories. Among 408 women without baseline hypertension, reporting a lot (hazard ratio, 2.17; 95% CI, 1.15–4.10) and moderate deportation worry (hazard ratio, 2.48; 95% CI, 1.17–4.30) were each associated with greater risk of incident hypertension compared with reporting not too much worry.
Conclusions
Deportation worry may contribute to widening disparities in some cardiovascular disease risk factors and outcomes over time.
Keywords: blood pressure, health disparities, hypertension, longitudinal cohort study, stress
Subject Categories: Hypertension, Epidemiology, Risk Factors
Clinical Perspective
What Is New?
In a community‐based cohort of Latina women, higher deportation worry was associated with steeper initial trajectories of systolic blood pressure and mean arterial pressure and greater hazard of incident hypertension. No association was observed with change in body mass index, waist circumference, or pulse pressure.
What Are the Clinical Implications?
Deportation worry may have adverse impacts on the trajectory of select cardiovascular risk factors and on hypertension risk.
Introduction
There is mounting concern that restrictive immigration policies and fear of deportation impact the health of immigrants and their family and community members.1, 2, 3, 4, 5 Such impacts could extend to cardiovascular disease (CVD) risk factors. Prior cross‐sectional research has documented significant associations between deportation worry and depression and anxiety,6, 7 poorer self‐rated health,8, 9 lower rates of healthcare utilization,2, 10, 11 and higher levels of inflammation,12 systolic blood pressure (SBP), pulse pressure (PP), waist circumference (WC), and body mass index (BMI).13
To our knowledge, no studies have evaluated the long‐term impacts of deportation worry on CVD trajectories. This research is critical, given that longitudinal blood pressure (BP) or weight outcomes have been shown to predict risk for subsequent CVD morbidity and mortality above and beyond measures captured at a single point in time.14, 15, 16, 17 Moreover, while one cross‐sectional analysis found no association between deportation worry and prevalent hypertension,13 deportation worry could have adverse impacts on incident outcomes that may develop over longer periods of time.
In the present study, we evaluated associations between deportation worry and longitudinal trajectories of CVD risk factors as well as incident hypertension among a community‐based cohort of adult women primarily of Mexican origin followed over a 4‐year period. We hypothesized that, relative to low deportation worry, reporting higher levels of deportation worry would be associated with widening disparities over time, including faster rates of increase in continuous CVD risk factors, and a greater risk of incident hypertension.
Methods
Data
Data are from the CHAMACOS (Center for the Health Assessment of Mothers and Children of Salinas) study, a longitudinal cohort study conducted in California's Salinas Valley, an agricultural region with a large Latino farmworker population.18 The first cohort (CHAM1) of women was recruited during pregnancy from community clinics between October 1999 and October 2000. Eligible women were 18 years or older, English‐ or Spanish‐speaking, eligible for Medi‐Cal (a state subsidized medical insurance plan), <20 weeks gestation, and planned to deliver at the county hospital. Of 1130 pregnant women approached, 601 agreed to participate and 531 remained in the study at the time of delivery. Women who declined to participate were more likely to be US‐born and English‐speaking, although they had similar age and parity to those who joined. A second cohort of 305 mothers of 9‐year‐old children (CHAM2) joined between January 2010 and September 2011 when CHAM1 children were 9 years old. Eligibility criteria for new participants mirrored those of the initial cohort (ie, mothers were 18 years and older at delivery, Spanish‐ or English‐speaking, eligible for Medi‐Cal during pregnancy, and received prenatal care in the Salinas Valley).
Mothers were first queried about deportation worry in visits that served as the baseline for the present analysis completed between March 2012 and August 2014. A total of 594 mothers (316 from CHAM1 and 278 from CHAM2) were surveyed as part of this baseline visit. Compared with women who did not complete the 2012–2014 visit, women who did were significantly older (about 2 years), but were not different in terms of nativity, years spent in the United States (for foreign‐born respondents), or educational attainment.
Follow‐up data were collected ≈2 (mean±SD: 2.16±0.19) and 4 years later (mean±SD: 4.26±0.30) (ie, May 2014 to August 2016 and December 2016 to November 2018) on 543 and 544 mothers who also completed the baseline (2012–2014) visit. Respondents were again asked about deportation worry at the 4‐year (2016–2018) follow‐up visit. Assessments were not used at a given wave if women were pregnant or missing information on pregnancy at the time of that assessment (37 at the 2012–2014 visit, 13 at 2‐year follow‐up, and 8 at 4‐year follow‐up).
Analyses of continuous outcomes were limited to women who had information on deportation worry in 2012–2014, data on prior depressive symptoms (a key potential confounder), and at least 1 valid clinical assessment at 1 of the 3 included study waves (Figure S1). Analyses of incident hypertension were further limited to those who were not classified as having hypertension at baseline. The majority of assessments were completed in the research office, although a small percentage were completed in participants’ homes (8% in 2012–2014, 9% at 2‐year follow‐up, and 8% at 4‐year follow‐up). Written informed consent was obtained from all participants. Study procedures were approved by the UC Berkeley Committee for Protection of Human Subjects. All authors have access to the data used for the present analysis and take responsibility for its integrity; the first author takes responsibility for data analysis. Data cannot be made publicly available because of National Institutes of Health Certificate of Confidentiality ethical restrictions that protect the confidentiality of participants in the CHAMACOS study. Requests about data access should be directed to eskenazi@berkeley.edu.
Measures
Worry about deportation
At the 2012–2014 visit, participants were asked the following question by bilingual interviewers: “We know that many families are worried about deportation, either for themselves or for their family and friends. How much worry would you say this causes you?” Response categories were: “not too much worry,” “a moderate amount of worry,” or “a lot of worry.” At the 4‐year follow‐up (2016–2018) visit, participants were asked the same question but given 4 possible response categories of “not at all worried,” “not much,” “moderately worried,” and “a lot of worry.”
Health outcomes
BMI was measured as weight in kilograms divided by squared height in meters. BMI assessments were based on a single weight measurement taken principally using a digital Tanita bioimpedence scale (Tanita TBF‐300A Body Composition Analyzer, Tanita Corporation), although ≈13% of women had weight measured with a digital scale (Tanita Baby and Mommy 1582, Tanita Corporation) because of personal preference or assessment at home. Barefoot standing height was measured with a wall‐mounted stadiometer (Seca 222, Seca).
WC was measured in triplicate at analytic baseline and in duplicate at the following visits by placing a measuring tape around the abdomen at 2 fingers above the umblicus, parallel to the floor; the average of the 2 or 3 measurements at each visit was calculated and used in analyses.
SBP and diastolic blood pressure (DBP) were measured with an automated oscillometric monitor (Dinamap 9300 or Dinamap Carescape 100) that was calibrated annually. The monitor was placed on the left arm after 2 minutes of rest. Three measurements were taken with 1 minute of rest between measurements and the average of the second 2 measurements was used in analyses. We calculated PP as DBP minus SBP, and mean arterial pressure (MAP) as SBP plus 3 times DBP over 3. Each of these BP‐related outcomes have been found to predict distinct cardiovascular end points.19
In primary analyses, missing BP values were addressed via multiple imputation (see below) and all respondents, including patients taking antihypertensives, were included. However, there was variation in assessment protocol across waves for patients taking antihypertensive medication. All women, including those taking medication, had BP assessed at analytic baseline and 2‐year follow‐up, whereas women taking antihypertensives were excused from BP assessment at 4‐year follow‐up. We therefore conducted sensitivity analyses that excluded respondents taking antihypertensives at the current or prior wave.
Before multiple imputation, BP values were set to missing at a given wave if respondents had <3 BP measurements taken at that wave (20 values set to missing). Values for BP, BMI, and WC were also set to missing before imputation if they were ±4 SDs about the mean for that wave (11 outliers detected across outcomes).
Presence of hypertension was determined based on self‐reported doctor diagnosis and measured BP at each wave. Data on doctor diagnosis were not collected at the 2‐year follow‐up, although at 4‐year follow‐up, diagnosed respondents were asked their age at diagnosis. Those who reported diagnosis between 2 and 5 years before the final assessment were classified as having a diagnosis at the 2‐year follow‐up. Individuals who self‐reported that they were ever diagnosed with hypertension/high BP or who had a measured SBP of >130 mm Hg OR DBP of >80 mm Hg were classified as having hypertension.20 We also evaluated associations with an alternative measure that used pre‐2017 hypertension guidelines (ie, cutoffs of ≥140 mm Hg SBP OR ≥90 mm Hg DBP).
Covariates
Covariates were selected based on a directed acyclic graph (Figure S2). They included respondents’ age in years, centered at the midpoint of the 4‐year follow‐up period, as well as a squared age term. We included categorical indicators of educational attainment (≤6th grade, >6th but <12th grade, and ≥12th grade) and nativity and years of residence in the United States (at analytic baseline) (≤15 years in the United States, >15 and ≤20 years in the United States, >20 years in the United States, and US–born), a binary indicator of marital status (married/living with partner versus single/divorced/widowed), a continuous measure of family income‐to‐poverty ratio at baseline, and an indicator of when the respondents enrolled in the cohort (ie, CHAM1 versus CHAM2). Finally, we controlled for depressive symptoms captured in a 2010–2011 study visit (the latest assessment point before the relevant study period) using the 20‐item Centers for Epidemiologic Studies—Depression (CES‐D) scale.21 We did not control for healthcare utilization or related measures that may be mediators (rather than confounders) of associations but report descriptive information on doctor's visits and insurance status for additional context.
Statistical Analyses
We first examined descriptive characteristics overall and by level of deportation worry at baseline. To evaluate whether deportation worry shifted substantially during assessments conducted after the 2016 Presidential election, we examined a cross‐tabulation of deportation worry measured at baseline and at the 4‐year follow‐up (2016–2018) visit.
We subsequently estimated linear mixed models of the relationship between baseline deportation worry and continuous health outcomes, adjusting for covariates. Models included an interaction term between deportation worry and years since baseline in order to evaluate differences in within‐person change in outcomes by baseline level of worry. We alternatively added an interaction between deportation worry and a quadratic term for years since baseline to allow for potential nonlinear patterns of change in health outcomes over the study period. Based on model fit statistics (Akaike information criterion and likelihood ratio tests), the addition of this quadratic term was preferred in models of SBP and MAP. Based on likelihood ratio tests, models that included subject‐specific random intercepts and subject‐specific random slopes were preferred. Models were estimated with an unstructured covariate matrix and robust standard errors. Across models, we calculated overall F tests for the measure of baseline deportation worry and the interaction between deportation worry and years since baseline.
Finally, we estimated Cox proportional hazards models to evaluate the relationship between deportation worry and the hazard of incident hypertension for patients who did not have hypertension at baseline. The proportional hazards assumption, evaluated via Wald tests for time‐varying versions of the outcome and each covariate, was met across all measures. Cox proportional hazard models were adjusted for all covariates and estimated with robust standard errors.
In all primary analyses, we accounted for missing data using multiple imputation for chained equations22 Thirty imputed data sets were generated and estimates were combined using Rubin's rules.23 We were not able to impute 2 cases as a result of missingness across many variables. We compared results using multiple imputation with results estimated using listwise deletion (Tables S1 and S2). Results were similar albeit less precise with the listwise deletion approach because of a smaller analytic sample.
To help account for possible selective dropout of respondents between study enrollment and baseline (2012–2014 visit) due to factors that might influence both deportation worry and outcomes, our models were weighted with stabilized inverse probability of attrition weights. Inverse probability of attrition weights were estimated with a logistic regression model of inclusion in the analytic sample on sociodemographic characteristics (eg, age, nativity/years in the United States) captured at enrollment and stabilized by including estimates of the inverse probability of being included in the sample (based on an intercept‐only logistic regression model) in the numerator.24
In sensitivity analyses we evaluated the robustness of results to alternative analytic samples that excluded: (1) women pregnant at any time between baseline and 4‐year follow‐up, given that changes in outcomes could have been driven by prepartum and postpartum changes in health; and (2) women born in the United States (Data S1). Analyses were conducted using STATA version 14 (StataCorp).
Results
A total of 572 respondents were included in the primary analyses of continuous outcomes. At the baseline visit, respondents were, on average, aged 39 years (Table 1). The majority (88%) were not born in the United States; 99% of immigrant women were born in Mexico. Among respondents who were neither pregnant nor missing pregnancy information at baseline (n=536), average BP values were in mean±SD: 113.7±15.0 mm Hg for SBP, 66±9.8 mm Hg for DBP, 83.2±11.5 mm Hg for MAP, 47.7±10.2 mm Hg for PP, 31.4 kg/m2±6.4 for BMI, and 101.8±15.4 cm for WC.
Table 1.
Descriptive Characteristics of Adult Women in the CHAMACOS Study, 2012–2014
| Overall (N=572) | Not at all Worried (n=161) | Moderate Worry (n=137) | A Lot of Worry (n=274) | Tests of Difference | |
|---|---|---|---|---|---|
| Age, mean±SD, y | 38.9 (5.3) | 38.2 (5.3) | 39.1 (5.4) | 39.1 (5.3) | P=0.19 |
| Currently married/living with a partner, No. (%) | 398 (69.6) | 107 (66.5) | 97 (70.8) | 194 (70.8) | P=0.57 |
| Educational attainment, No. (%) | |||||
| <6th grade | 245 (42.8) | 51 (31.7) | 49 (35.8) | 145 (52.9) | P<0.001 |
| 7th to 12th grade | 191 (33.4) | 50 (31.1) | 52 (38.0) | 89 (32.5) | |
| ≥12th grade | 136 (23.8) | 60 (37.3) | 36 (26.3) | 40 (14.6) | |
| Nativity/years in the United States, No. (%) | |||||
| US‐born | 69 (12.1) | 42 (26.1) | 16 (11.7) | 11 (4.0) | P<0.001 |
| >21 y | 162 (28.3) | 50 (31.1) | 39 (28.5) | 73 (26.6) | |
| 16 to 20 y | 165 (28.9) | 38 (23.6) | 42 (30.7) | 85 (31.0) | |
| <15 y | 176 (30.8) | 31 (19.3) | 40 (29.2) | 105 (38.3) | |
| Family income‐to‐poverty ratio, mean±SD | 0.77 (0.4) | 0.88 (0.5) | 0.83 (0.3) | 0.68 (0.3) | P<0.001 |
| Depressive symptoms (range: 0–20), mean±SD | 11.3 (10.9) | 9.31 (10.4) | 9.59 (8.5) | 13.20 (12.1) | P<0.001 |
| Elevated depressive symptoms (≥16), No. (%) | 161 (28.2) | 31 (19.3) | 29 (21.2) | 101 (36.9) | P<0.001 |
| Has health insurance, No. (%)a | 287 (50.2) | 96 (59.6) | 79 (57.7) | 112 (40.9) | P<0.001 |
| Past‐year doctor's visit, No. (%)a | 413 (72.2) | 112 (69.6) | 109 (79.6) | 192 (70.1) | P=0.11 |
| Cohort | |||||
| CHAM1 | 296 (51.8) | 85 (52.8) | 77 (56.2) | 134 (48.9) | P=0.36 |
| CHAM2 | 276 (48.3) | 76 (47.2) | 60 (43.8) | 140 (51.1) | |
| Weight outcomes, baselineb | (n=536) | (n=149) | (n=126) | (n=261) | |
| BMI, mean±SD | 31.4 (6.4) | 30.6 (6.1) | 31.0 (6.2) | 31.9 (6.6) | P=0.11 |
| BMI categories | |||||
| Normal/underweight | 69 (12.9) | 27 (18.1) | 13 (10.3) | 29 (11.1) | P=0.03 |
| Overweight | 186 (34.7) | 45 (30.2) | 56 (44.4) | 85 (32.6) | |
| Obese | 281 (52.4) | 77 (51.7) | 57 (45.2) | 147 (56.3) | |
| WC, cm, mean±SD | 101.8 (15.4) | 99.95 (14.9) | 101.1 (14.9) | 103.3 (15.7) | P=0.09 |
| BP outcomes, baselineb | |||||
| SBP, mm Hg, mean±SD | 113.7 (15.0) | 112.4 (13.8) | 114.9 (15.9) | 114.0 (15.7) | P=0.38 |
| DBP, mm Hg, mean±SD | 66.0 (9.8) | 66.4 (9.9) | 67.3 (9.9) | 65.3 (9.8) | P=0.18 |
| MAP, mm Hg, mean±SD | 83.2 (11.5) | 83.1 (11.5) | 84.2 (11.6) | 82.8 (11.6) | P=0.57 |
| PP, mm Hg, mean±SD | 47.7 (10.2) | 46.01 (8.9) | 47.6 (10.4) | 48.67 (10.7) | P=0.04 |
| Prevalent hypertension, No. (%) | 153 (28.5) | 40 (26.9) | 38 (30.2) | 75 (28.7) | P=0.26 |
| Doctor‐diagnosed hypertension‡ | 94 (61.4) | 28 (70.0) | 16 (42.1) | 50 (66.7) | P=0.02 |
BMI indicates body mass index; CHAM1, first cohort of the CHAMACOS study; CHAM2, second cohort of the CHAMACOS study; CHAMACOS, Center for the Health Assessment of Mothers and Children of Salinas; DBP, diastolic blood pressure; MAP, mean arterial pressure; PP, pulse pressure; SBP, systolic blood pressure; WC, waist circumference.
Not included as covariates because these are either potential mediators of the relationship between deportation worry and outcomes or possible colliders (ie, common outcomes of both exposure and outcome).
Descriptive characteristics of continuous outcome measures at 2012–2014 calculated for 536 women who were not pregnant and/or had nonmissing pregnancy information at the same visit.
Doctor‐diagnosed hypertension is calculated only for participants categorized as having hypertension at baseline and meant to show the proportion of patients whose hypertension was doctor‐diagnosed vs classified based on clinical blood pressure (BP) assessments.
Of the 572 respondents, 153 (28%) had hypertension at baseline, just under two thirds of whom reported doctor‐diagnosed hypertension. Another 11 respondents had no health assessment at 2‐ or 4‐year follow‐up, leaving 408 respondents with 95 new cases of hypertension for analyses of deportation worry and incident hypertension.
Nearly half (48%) of respondents reported a lot of worry about deportation at the baseline visit, 24% reported moderate worry, and 28% reported “not too much worry” (hereafter, for simplicity, “high,” “moderate,” and “low” worry). There were no differences in respondent age or baseline marital status across levels of baseline deportation worry, although there were substantial differences in nativity/years in the United States, educational attainment, baseline income‐to‐poverty ratio, and prior depressive symptoms.
From the baseline to the 4‐year follow‐up visit, ≈18.3% of the 507 respondents who reported on worry at both visits reported increased worry about deportation (ie, from not much to moderate or moderate to high worry); 27.2% of respondents reported lower worry about deportation (ie, from high to moderate/not much/not at all worried or moderate to not much/not at all worried), while the remaining 54.4% reported no change in deportation worry (Table S3). The overall prevalence of deportation worry remained similar at baseline and the 4‐year follow‐up visit.
High (but not moderate) deportation worry was associated with higher baseline BMI and higher baseline WC relative to low worry, but not with differences in trajectories of BMI or WC over time (Table 2; Figure 1, Panel A and Panel B).
Table 2.
Regression Coefficients and 95% CIs for Linear Mixed Models of Self‐Reported Deportation Worry and BP Trajectories for Adult Women in the CHAMACOS Study (N=572)
| BMI | WC | SBP | DBP | MAP | PP | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | |||||||
| Deportation worry (reference=not at all worried) | ||||||||||||
| Moderately worried | 0.88 (−0.47 to 2.24) | 2.19 (−1.13 to 5.52) | 2.51 (−1.10 to 6.12) | 1.51 (−0.86 to 3.88) | 1.41 (−1.30 to 4.12) | 1.25 (−1.07 to 3.56) | ||||||
| A lot of worry | 2.12 (0.94–3.29)* | 4.73 (1.82–7.63)† | 2.08 (−0.90 to 5.07) | 0.28 (−1.75 to 2.30) | 0.62 (−1.72 to 2.96) | 2.88 (0.89–4.87)† | ||||||
| Years since 2012 study wave | 0.02 (−0.15 to 0.20) | −0.93 (−1.43 to −0.44)* | −1.16 (−3.77 to 1.46) | 0.61 (−0.08 to 1.29) | −0.72 (−2.58 to 1.14) | 0.36 (−0.59 to 1.31) | ||||||
| Deportation worry×y | ||||||||||||
| Moderately worried×y | 0.01 (−0.17 to 0.19) | 0.16 (−0.43 to 0.74) | 1.60 (−1.97 to 5.18) | 0.32 (−0.36 to 1.00) | 1.75 (−0.66 to 4.15) | 0.27 (−0.59 to 1.13) | ||||||
| A lot of worry×y | −0.05 (−0.20 to 0.11) | −0.11 (−0.63 to 0.31) | 4.10 (1.17–7.03)† | 0.58 (0.03–1.12)‡ | 3.52 (1.38–5.65)† | 0.24 (−0.49 to 0.97) | ||||||
| Since 2012 study wave, y squared | 0.50 (−0.21 to 1.20) | 0.50 (−0.01 to 1.01) | ||||||||||
| Deportation worry×y squared | ||||||||||||
| Moderately worried×y squared | −0.23 (−1.14 to 0.67) | −0.32 (−0.91 to 0.27) | ||||||||||
| A lot of worry×y squared | −0.80 (−1.55 to −0.06)‡ | −0.73 (−1.27 to −0.19)‡ | ||||||||||
| Overall F test for deportation worry and deportation worry×time interaction | 3.16 | P=0.0131 | 3.03 | P=0.0164 | 3.43 | P=0.0022 | 2.34 | P=0.0526 | 3.03 | P=0.0058 | 2.95 | P=0.0191 |
| Overall F test for deportation worry×time interaction | 0.32 | P=0.7234 | 0.55 | P=0.5746 | 2.60 | P=0.0345 | 2.13 | P=0.1194 | 2.81 | P=0.0244 | 0.25 | P=0.7822 |
BMI indicates body mass index; BP, blood pressure; CHAMACOS, Center for the Health Assessment of Mothers and Children of Salinas; DBP, diastolic blood pressure; MAP, mean arterial pressure; PP, pulse pressure; SBP, systolic blood pressure; WC, waist circumference.*P<0.001. † P<0.01. ‡ P<0.05. Controls include age, age squared, nativity/years spent in the United States, educational attainment, income‐to‐poverty ratio and marital status at the 2012–2014 visit, a binary indicator of whether mothers were in the original vs refreshed cohorts of the study, and prior depressive symptoms (captured at a visit 3 years before the 2012–2014 visit). All models include a stabilized inverse probability of attrition weight to account for selective attrition before the 2012–2014 visit. Models specified with both subject‐specific random intercepts and subject‐specific random slopes.
Figure 1.
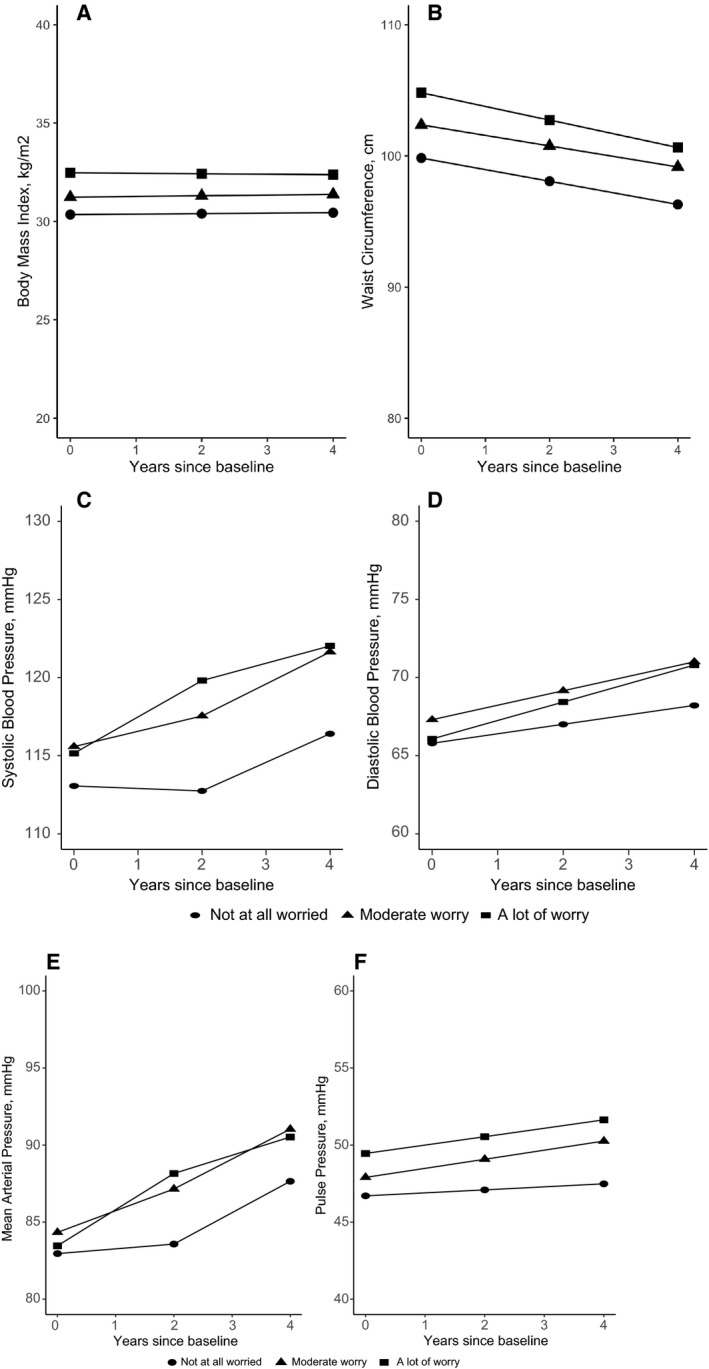
Predicted average values of body mass index (A), waist circumference (B), systolic blood pressure (C), diastolic blood pressure (D), mean arterial pressure (E), and pulse pressure (F) by deportation worry and years since baseline (2012–2014) for adult women of Mexican origin, in the CHAMACOS (Center for the Health Assessment of Mothers and Children of Salinas) study, (n=572). Predicted values generated from linear mixed models that adjust for sociodemographic characteristics and prior depressive symptoms. An interaction term between deportation worry and a quadratic term for years since the 2012–2014 visit was evaluated based on model fit statistics and included for models of systolic blood pressure and mean arterial pressure only. Follow‐up visits took place in 2014–2016 and 2016–2018, 2 and 4 years after the baseline visit, respectively. Source: CHAMACOS study.
Relative to the low worry reference group, high worry at baseline was associated with higher baseline (β, main effect term for a lot of worry: 2.08; 95% CI, −0.90 to 5.07), significantly faster initial increase (β, interaction with linear year term: 4.10; 95% CI, 1.17–7.03), followed by a significantly faster decrease in SBP (β, interaction with quadratic year term: −0.80, 95% CI, −1.55 to −0.06) (Table 2; Figure 1, Panel C). Estimated associations for moderate versus low worry followed similar patterns, although differences were of smaller magnitude and not significant.
Deportation worry was not associated with differences in baseline DBP or MAP. However, high (but not moderate) deportation worry was associated with a faster increase in DBP over the 4‐year period relative to low worry (β, interaction with linear year term: 0.58; 95% CI, 0.03–1.12) (Table 2; Figure 1, Panel D). Similar to patterns for SBP, reporting high worry was associated with a faster initial increase in MAP followed by a faster decline during the final wave compared with reporting low worry (Figure 1, Panel E). High (but not moderate) worry was associated with higher baseline PP compared with low worry but no differences in the longitudinal PP trajectories (Figure 1, Panel F).
When the analytic sample for analyses of BP trajectories was limited to 518 respondents who did not report taking antihypertensives at the current or previous wave, we observed the following differences: baseline differences in average SBP and DBP for those who reported high and moderate worry versus low worry were larger than in primary analyses, and associations between deportation worry and change in DBP were attenuated (Table S4 and Figure S3). Results otherwise remained the same.
Reporting high (hazard ratio, 2.17; 95% CI, 1.15–4.10) and moderate worry (hazard ratio, 2.24; 95% CI, 1.17–4.30) were each associated with greater risk of incident hypertension based on doctor diagnosis or cutoffs of 130 mm Hg SBP or 80 mm Hg DBP (Table 3). Results were of larger magnitude but less precise (ie, wider 95% CIs) when using pre‐2017 guidelines (ie, ≥140 mm Hg SBP or ≥90 mm Hg DBP) (Table S5).
Table 3.
HRs and 95% CIs for the Association Between Deportation Worry at 2012–2014 and Incident Hypertension (n=408)
| HR (95% CI) | |
|---|---|
| Deportation worry, 2012–2014 (reference=not at all worried) | |
| Moderately worried | 2.24 (1.17–4.30)a |
| A lot of worry | 2.17 (1.15–4.10)a |
The CHAMACOS (Center for the Health Assessment of Mothers and Children of Salinas study).
P<0.05. Hypertension based on self‐reported doctor diagnosis or cutoff of ≥130 mm Hg systolic blood pressure or ≥80 mm Hg diastolic blood pressure. Controls include age, age‐squared, nativity/years spent in the United States, educational attainment, income‐to‐poverty ratio and marital status at the 2012–2014 visit, a binary indicator of whether mothers were in the original vs refreshed cohorts of the study, and prior depressive symptoms (captured at a 2010–2011 study visit). All models include a (stabilized) inverse probability of attrition weight to account for selective attrition before the 2012–2014 visit.
Overall results were robust to the exclusion of: (1) women who were pregnant or missing pregnancy information at any point since baseline; and (2) US‐born women, respectively (Tables S6 through S8).
Discussion
There is growing concern about the impact of immigration policies on population health, including on CVD and related risk factors.25, 26, 27 Nevertheless, little is known about the longitudinal impacts of these policies on health outcomes in general or CVD outcomes or risk factors in particular. Using data from a cohort of adult women primarily of Mexican origin, we found that higher deportation worry was associated with steeper increases in BP over an ≈4‐year period, with the most robust findings for systolic pressure and MAP. We additionally found that women who reported higher levels of worry about deportation had a 2‐fold higher risk of incident hypertension than those who reported low deportation worry over the same period. Finally, there were no differences in PP, BMI, or WC trajectories by baseline level of deportation worry; baseline disparities in these outcomes by level of deportation worry persisted.
Overall, these findings suggest that level of deportation worry was associated with either widening disparities—in the case of SBP, MAP, and (to a lesser extent) DBP—or persistent disparities, in the case of PP, BMI, and WC. Findings are consistent with research documenting the impacts of other psychosocial stressors (eg, discrimination and socioeconomic position) on CVD risk factor trajectories as well as incident hypertension.28, 29, 30 When deportation worry is experienced chronically, it may contribute to elevated risk for high BP through pathways related to the dysregulation of the hypothalamic‐pituitary‐adrenal axis, including the excess secretion of proinflammatory cytokines and glucocorticoids.31, 32 Deportation worry may also impact CVD risk factors and hypertension by way of increased risk for depression, anxiety, and sleep problems.33, 34, 35, 36 In addition, individuals who are worried about possible deportation may reduce interactions with health and social service agencies and potential employers.5, 37, 38 This may have long‐term consequences for health by delaying the prevention and diagnosis of hypertension and other medical conditions, limiting access to healthy food and opportunities for physical and social activity, and contributing to additional (eg, financial) stressors.
Despite the overall evidence for widening disparities in CVD risk factors by prior deportation worry, there was evidence of slightly diminishing disparities in SBP and MAP from the second to the final outcome assessment. These patterns could have been caused by changes in deportation worry across the entire sample. This final assessment was performed in the aftermath of the 2016 Presidential election, a period marked by increased deportation worry among immigrants and their family members.39 In a descriptive comparison, we found that the overall prevalence of deportation worry remained stable between the 2012–2014 and 2016–2018 study waves; over half of those who reported on worry at both visits reported the same level of worry at these visits. The overall stability in deportation worry may reflect the fact that there were very high rates of deportation when deportation worry was first assessed (2012–2014),40 and deportation worry among US Latinos was also high during this time period.41 However, the remaining respondents reported change in deportation worry, including patterns of both increasing and decreasing worry. This underlying change in deportation worry could have driven converging trends in BP outcomes by the final study wave.
Another potential explanation for reduced differences in SBP and MAP by the final wave is that US‐born women had both slightly higher rates of attrition from the final study wave and higher average BP at analysis baseline (120 mm Hg compared with 112 mm Hg for immigrant women). The higher attrition of US‐born women may also explain the small apparent improvements in WC over the follow‐up period, given that US‐born women also had larger average WC at analysis baseline (ie, 108.6 cm compared with 100.7 cm for immigrant women).
Limitations
This analysis has several limitations. First, the cohort is based on a nonprobability sample and is restricted to adult women in midlife. Findings may not generalize to other communities or population subgroups (eg, men and older adults), although the prevalence of deportation worry at the 2012–2014 visit is similar to national figures reported for US Latinos around the same time.41
Second, deportation worry is measured with a single item, which may be more vulnerable to systematic biases (eg, in reporting patterns) or random variability than multi‐item scales. Future research should incorporate recently developed scales42 reflecting deportation worry and related constructs. The current measure also broadly refers to worry for one's self, family members, or friends. Deportation worry may have been most acute among individuals worried that they or immediate family members could be deported; information on respondents’ or family members’ documentation status was not collected because of confidentiality concerns. Observed associations may underestimate the impact of deportation worry for one's self or immediate family members.
Finally, it is possible that observed associations remain confounded by other psychosocial factors, including contemporaneous depressive symptoms. However, depressive symptoms and related psychosocial states are likely mediators of the association between deportation worry and the evaluated outcomes.33, 34, 35, 36 Even if more contemporaneous measures of depressive symptoms were available, conditioning on this potential mediator of the relationship between deportation worry and CVD risk factors/hypertension would have resulted in over‐control.
Conclusions
There is an urgent need to understand the impact of immigration policy and resulting deportation fears on CVD outcomes and related risk factors of immigrants and their family members. In one of few studies to evaluate the relationship between perceived deportation worry and CVD outcomes, and the first to evaluate these relationships longitudinally, we observed that deportation worry was associated with either persistent or widening disparities in key CVD risk factors and greater risk of incident hypertension among a cohort of women primarily of Mexican origin. Future research should continue to document the impacts of both immigration policies and deportation worry on the long‐term cardiovascular health of immigrants and their US‐born family members, and expand these efforts to other impacted subgroups and health outcomes.
Disclosures
None.
Supporting information
Data S1. Further Details Regarding Sensitivity Analyses.
Table S1. Regression Coefficients and 95% CIs for Linear Mixed Models of Self‐Reported Deportation Worry on Blood Pressure Trajectories for Adult Women in the CHAMACOS Study Using Listwise Deletion Rather Than Multiple Imputation
Table S2. HRs and 95% CIs for the Association Between Deportation Worry at 2012–2014 and Incident Hypertension Using Listwise Deletion Rather Than Multiple Imputation (n=371)
Table S3. Cross‐Tabulation of Self‐Reported Deportation Worry at 2012–2014 and 2016–2018 Visits Among Adult Women in the CHAMACOS Study (n=507)
Table S4. Regression Coefficients and 95% CIs for Linear Mixed Models of Self‐Reported Deportation Worry on Blood Pressure Trajectories for Adult Women in the CHAMACOS Study Who Were Not Taking Antihypertensives at a Given Study Wave or Previous Study Waves (n=518)
Table S5. HRs and 95% CIs for the Association Between Deportation Worry at 2012–2014 and Incident Hypertension Based on Pre‐2017 Guidelines (n=445)
Table S6. Regression Coefficients and 95% CIs for Linear Mixed Models of Self‐Reported Deportation Worry on Blood Pressure Trajectories for Adult Women in the CHAMACOS Study Who Were Not Pregnant/Nonmissing Pregnancy Data Throughout the 4‐Year Study Period (n=534)
Table S7. Regression Coefficients and 95% CIs for Linear Mixed Models of Self‐Reported Deportation Worry on Blood Pressure Trajectories for Adult Immigrant Women in the CHAMACOS Study (n=503)
Table S8. HRs and 95% CIs for the Association Between Deportation Worry at 2012–2014 and Incident Hypertension; Alternative Specifications to Primary Analyses
Figure S1. Flowchart tracking exclusion of women from primary analyses of the relationship between deportation worry cardiovascular disease risk factors and incident hypertension in the CHAMACOS (Center for the Health Assessment of Mothers and Children of Salinas) study.
Figure S2. Directed acyclic graph (DAG) used to guide analyses.
Figure S3. Predicted average values of cardiovascular disease (CVD) risk factors by deportation worry and years since baseline (2012–2014) for adult women of Mexican origin who did not report taking antihypertensive medication in the CHAMACOS (Center for the Health Assessment of Mothers and Children of Salinas) study (n=518).
(J Am Heart Assoc. 2019;8:e013086 DOI: 10.1161/JAHA.119.013086.)
This work was presented at the annual meeting of the Society for Epidemiologic Research, June 19, 2019, in Minneapolis, MN.
References
- 1. Novak NL, Geronimus AT, Martinez‐Cardoso AM. Change in birth outcomes among infants born to Latina mothers after a major immigration raid. Int J Epidemiol. 2017;46:839–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rhodes SD, Mann L, Simán FM, Song E, Alonzo J, Downs M, Lawlor E, Martinez O, Sun CJ, O'Brien MC, Reboussin BA, Hall MA. The impact of local immigration enforcement policies on the health of immigrant Hispanics/Latinos in the United States. Am J Public Health. 2015;105:329–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Torche F, Sirois C. Restrictive immigration law and birth outcomes of immigrant women. Am J Epidemiol. 2019;188:24–33. [DOI] [PubMed] [Google Scholar]
- 4. Wang JS, Kaushal N. Health and mental health effects of local immigration enforcement. National Bureau of Economic Research Working Paper. 2018. (24487).
- 5. White K, Blackburn J, Manzella B, Welty E, Menachemi N. Changes in use of county public health services following implementation of Alabama's immigration law. J Health Care Poor Underserved. 2014;25:1844–1852. [DOI] [PubMed] [Google Scholar]
- 6. Valdez CR, Padilla B, Valentine JL. Consequences of Arizona's immigration policy on social capital among Mexican mothers with unauthorized immigration status. Hisp J Behav Sci. 2013;35:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yoshikawa H. Immigrants Raising Citizens: undocumented Parents and Their Young children. New York, NY: Russell Sage Foundation; 2011. [Google Scholar]
- 8. Finch BK, Vega WA. Acculturation stress, social support, and self‐rated health among Latinos in California. J Immigr Health. 2003;5:109–117. [DOI] [PubMed] [Google Scholar]
- 9. Cavazos‐Rehg PA, Zayas LH, Spitznagel EL. Legal status, emotional well‐being and subjective health status of Latino immigrants. J Nat Med Assoc. 2007;99:1126–1131. [PMC free article] [PubMed] [Google Scholar]
- 10. Heyman JM, Núñez GG, Talavera V. Healthcare access and barriers for unauthorized immigrants in El Paso County, Texas. Fam Community Health. 2009;32:4–21. [DOI] [PubMed] [Google Scholar]
- 11. Maldonado CZ, Rodriguez RM, Torres JR, Flores YS, Lovato LM. Fear of discovery among Latino immigrants presenting to the emergency department. Acad Emerg Med. 2013;20:155–161. [DOI] [PubMed] [Google Scholar]
- 12. Martínez AD, Ruelas L, Granger DA. Household fear of deportation in relation to chronic stressors and salivary proinflammatory cytokines in Mexican‐origin families post‐SB 1070. SSM Popul Health. 2018;5:188–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Torres JM, Deardorff J, Gunier RB, Harley KG, Alkon A, Kogut K, Eskenazi B. Worry about deportation and cardiovascular disease risk factors among adult women: the Center for the Health Assessment of Mothers and Children of Salinas (CHAMACOS) study. Ann Behav Med. 2018;52:186–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Allen NB, Siddique J, Wilkins JT, Shay C, Lewis CE, Goff DC, Jacobs DR Jr, Liu K, Lloyd‐Jones D. Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. JAMA. 2014;311:490–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Allen N, Berry JD, Ning H, Van Horn L, Dyer A, Lloyd‐Jones DM. Impact of blood pressure and blood pressure change during middle age on the remaining lifetime risk for cardiovascular disease: the cardiovascular lifetime risk pooling project. Circulation. 2012;125:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pletcher MJ, Vittinghoff E, Thanataveerat A, Bibbins‐Domingo K, Moran AE. Young adult exposure to cardiovascular risk factors and risk of events later in life: the Framingham Offspring Study. PLoS One. 2016;11:e0154288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Song M, Hu FB, Wu K, Must A, Chan AT, Willett WC, Giovannucci EL. Trajectory of body shape in early and middle life and all cause and cause specific mortality: results from two prospective US cohort studies. BMJ. 2016;353:i2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Eskenazi B, Harley K, Bradman A, Weltzien E, Jewell NP, Barr DB, Furlong CE, Holland NT. Association of in utero organophosphate pesticide exposure and fetal growth and length of gestation in an agricultural population. Environ Health Perspect. 2004;112:1116–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Basu S, Hong A, Siddiqi A. Using decomposition analysis to identify modifiable racial disparities in the distribution of blood pressure in the United States. Am J Epidemiol. 2015;182:345–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2018;138: e426–e483. [DOI] [PubMed] [Google Scholar]
- 21. Radloff LC. The CES‐D scale, a self‐report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 22. Royston P, White IR. Multiple imputation by chained equations (MICE): implementation in STATA. J Stat Softw. 2011;45:1–20. [Google Scholar]
- 23. Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: Wiley; 1987. [Google Scholar]
- 24. Howe CJ, Cole SR, Lau B, Napravnik S, Eron JJ. Selection dias due to loss to follow up in cohort studies. Epidemiology. 2016;27:91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Morey BN. Mechanisms by which anti‐immigrant stigma exacerbates racial/ethnic health disparities. Am J Public Health. 2018;108:460–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Torres JM, Young MD. A life‐course perspective on legal status stratification and health. SSM Popul Health. 2016;2:141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Philbin MM, Flake M, Hatzenbuehler ML, Hirsch JS. State‐level immigration and immigrant‐focused policies as drivers of Latino health disparities in the United States. Soc Sci Med. 2018;199:29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Clarke P, O'Malley PM, Johnston LD, Schulenberg JE. Social disparities in BMI trajectories across adulthood by gender, race/ethnicity and lifetime socio‐economic position: 1986–2004. Int J Epidemiol. 2009;38:499–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Strand BH, Murray ET, Guralnik J, Hardy R, Kuh D. Childhood social class and adult adiposity and blood‐pressure trajectories 36‐53 years: gender‐specific results from a British birth cohort. J Epidemiol Community Health. 2012;66:512–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Janicki‐Deverts D, Cohen S, Matthews KA, Jacobs DR. Sex differences in the association of childhood socioeconomic status with adult blood pressure change: the CARDIA study. Psychosom Med. 2012;74:728–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Everson‐Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev Public Health. 2005;26:469–500. [DOI] [PubMed] [Google Scholar]
- 32. Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012;9:360–370. [DOI] [PubMed] [Google Scholar]
- 33. Räikkönen K, Matthews KA, Kuller LH. Trajectory of psychological risk and incident hypertension in middle‐aged women. Hypertension. 2001;38:798–802. [PubMed] [Google Scholar]
- 34. Cappuccio FP, Stranges S, Kandala NB, Miller MA, Taggart FM, Kumari M, Ferrie JE, Shipley MJ, Brunner EJ, Marmot MG. Gender‐specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall II Study. Hypertension. 2007;50:693–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gangwisch JE. A review of evidence for the link between sleep duration and hypertension. Am J Hypertens. 2014;27:1235–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cohen BE, Edmondson D, Kronish IM. State of the art review: depression, stress, anxiety, and cardiovascular disease. Am J Hypertens. 2015;28:1295–1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Toomey RB, Umaña‐Taylor AJ, Williams DR, Harvey‐Mendoza E, Jahromi LB, Updegraff KA. Impact of Arizona's SB 1070 immigration law on utilization of health care and public assistance among Mexican‐origin adolescent mothers and their mother figures. Am J Public Health. 2014;104:S28–S34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. White K, Yeager VA, Menachemi N, Scarinci IC. Impact of Alabama's immigration law on access to health care among Latina immigrants and children: implications for national reform. Am J Public Health. 2014;104:397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hugo Lopez M, Gonzalez‐Barrera A, Krogstad JM. More Latinos Have Serious Concerns About Their Place in America Under Trump. Washington, DC: Pew Research Center; 2018. [Google Scholar]
- 40. Gonzalez‐Barrera A, Krogstad JM. U.S. Deportations of Immigrants Reach Record High in 2013. Washington, DC: Pew Hispanic Trends Project; 2014. [Google Scholar]
- 41. Hugo Lopez M, Taylor P, Funk C, On Gonzalez‐Barrera A. Immigration Policy, Deportation Relief Seen as More Important than Citizenship: A Survey of Hispanics and Asian Americans. Washington, DC: Pew Research Center: Hispanic Trends; 2013. [Google Scholar]
- 42. Ayón C. Perceived immigration policy effects scale: development and validation of a scale on the impact of state‐level immigration policies on Latino immigrant families. Hisp J Behav Sci. 2017;39:19–33. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Further Details Regarding Sensitivity Analyses.
Table S1. Regression Coefficients and 95% CIs for Linear Mixed Models of Self‐Reported Deportation Worry on Blood Pressure Trajectories for Adult Women in the CHAMACOS Study Using Listwise Deletion Rather Than Multiple Imputation
Table S2. HRs and 95% CIs for the Association Between Deportation Worry at 2012–2014 and Incident Hypertension Using Listwise Deletion Rather Than Multiple Imputation (n=371)
Table S3. Cross‐Tabulation of Self‐Reported Deportation Worry at 2012–2014 and 2016–2018 Visits Among Adult Women in the CHAMACOS Study (n=507)
Table S4. Regression Coefficients and 95% CIs for Linear Mixed Models of Self‐Reported Deportation Worry on Blood Pressure Trajectories for Adult Women in the CHAMACOS Study Who Were Not Taking Antihypertensives at a Given Study Wave or Previous Study Waves (n=518)
Table S5. HRs and 95% CIs for the Association Between Deportation Worry at 2012–2014 and Incident Hypertension Based on Pre‐2017 Guidelines (n=445)
Table S6. Regression Coefficients and 95% CIs for Linear Mixed Models of Self‐Reported Deportation Worry on Blood Pressure Trajectories for Adult Women in the CHAMACOS Study Who Were Not Pregnant/Nonmissing Pregnancy Data Throughout the 4‐Year Study Period (n=534)
Table S7. Regression Coefficients and 95% CIs for Linear Mixed Models of Self‐Reported Deportation Worry on Blood Pressure Trajectories for Adult Immigrant Women in the CHAMACOS Study (n=503)
Table S8. HRs and 95% CIs for the Association Between Deportation Worry at 2012–2014 and Incident Hypertension; Alternative Specifications to Primary Analyses
Figure S1. Flowchart tracking exclusion of women from primary analyses of the relationship between deportation worry cardiovascular disease risk factors and incident hypertension in the CHAMACOS (Center for the Health Assessment of Mothers and Children of Salinas) study.
Figure S2. Directed acyclic graph (DAG) used to guide analyses.
Figure S3. Predicted average values of cardiovascular disease (CVD) risk factors by deportation worry and years since baseline (2012–2014) for adult women of Mexican origin who did not report taking antihypertensive medication in the CHAMACOS (Center for the Health Assessment of Mothers and Children of Salinas) study (n=518).


