Abstract
Background
The ART (Arterial Revascularization Trial) showed no difference in survival at 10 years between patients assigned to the single versus bilateral internal thoracic artery grafting strategies. This finding is in contrast with the results of most observational studies, where the use of 2 internal thoracic arteries has been associated with improved survival.
Methods and Results
We selected propensity‐matched studies from the most comprehensive observational meta‐analysis on the long‐term outcomes of patients receiving 1 versus 2 internal thoracic arteries. Individual participant survival data from each study and the ART were reconstructed using an iterative algorithm that was applied to solve the Kaplan‐Meier equations. The reconstructed individual participant survival data were aggregated to obtain combined survival curves and Cox regression hazard ratios with 95% CIs. Individual participant survival data were obtained from 14 matched observational studies (24 123 patients) and the ART. The 10‐year survival of the control group of ART was significantly higher than that of the matched observational studies (hazard ratio, 0.86; 95% CI, 0.80–0.93). The 10‐year survival of the experimental group of ART was significantly lower than that of the bilateral internal thoracic artery group of the observational studies (hazard ratio, 1.11; 95% CI, 1.03–1.20).
Conclusions
Both the improved outcome of the control arm and the lower beneficial effect of the intervention had played a role in the difference between observational evidence and ART.
Keywords: coronary artery bypass graft surgery, coronary artery disease, revascularization
Subject Categories: Cardiovascular Surgery, Revascularization, Chronic Ischemic Heart Disease, Myocardial Infarction
Disagreement between observational and randomized evidence is common in medicine and is mainly caused by selection and publication bias and hidden confounders in observational studies. However, because of their high complexity and costs, large‐scale randomized trials are lacking for most of our research questions and, currently, <12% of the clinical guidelines in the cardiovascular field are based on the results of randomized studies.1
The ART (Arterial Revascularization Trial) is the only large randomized trial comparing the clinical outcomes of patients submitted to coronary artery bypass grafting using 2 versus 1 internal thoracic artery (ITA).2 In ART, no difference in survival at 10 years was found between patients assigned to the 2 revascularization strategies. This finding is in contrast with the results of most observational studies, where the use of 2 ITAs has generally been associated with improved survival.3 Of note, on the basis of the observational evidence, the use of 2 ITAs is a class IIA recommendation in current guidelines.4
The suggested explanations for the contradiction between ART and the observational evidence are as follows: (1) the improved outcomes of the control arm (because of the Hawthorne effect, the high rate of use of the radial artery, or the high compliance with guideline‐directed secondary prevention) or (2) the reduced effect of the experimental intervention (because of the diluting effects of high crossover rate from experimental to control group, issues in the delivery of the intervention, or lack of true biological effect).5 Identification of the main mechanism may not only shed light on the use of bilateral ITAs but also on the methodological differences between randomized and observational evidence, and it may inform decision making for guidelines and recommendations development and health policy strategies.
We compared the outcome of the experimental and control groups in ART with the correspondent groups in observational studies. As a summary of the observational evidence, we selected the most comprehensive observational meta‐analysis on the long‐term outcomes of patients receiving 1 versus 2 ITAs3 and included only the propensity‐matched studies (considered the highest quality of observational evidence). Accordingly, individual participant survival data from 14 matched observational studies (24 123 patients) and the ART were reconstructed using an iterative algorithm that was applied to solve the Kaplan‐Meier equations. The details of patients in the individual studies are summarized in the Table.6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19 The reconstructed individual participant survival data were aggregated to obtain combined survival curves and Cox regression hazard ratios (HRs) with 95% CIs.20
Table 1.
Characteristics of Patients in Included Studies
| No. of PSM Patients | Age, y | Female, % | Radial Artery, % | OPCABG, % | ONCABG, % | Complete Revascularization, % | EuroSCORE | STS Score | Mean/Median Follow‐Up, y | Completeness of Follow‐Up, % | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study, Year | BITA | SITA | BITA | SITA | BITA | SITA | BITA | SITA | BITA | SITA | BITA | SITA | BITA | SITA | BITA | SITA | BITA | SITA | ||
| Benedetto, 20146 | 750 | 750 | NR | NR | 23 | 23 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 4.8±3.2 (PSM sample) | 100 |
| Dalén, 20147 | 558 | 558 | 64.4±11.1 | 64.4±11.1 | 25.9 | 25.9 | 16.3 | 11.8 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 7.5 | 100 |
| Grau, 20158 | 1006 | 1006 | 60±9 | 60±9 | 10.4 | 10.4 | NR | NR | 50 | 50 | 50 | 50 | NR | NR | NR | NR | 1.1 | 1.3 |
BITA, 10.9±5 SITA, 10.1±5 |
100 |
| Joo, 20129 | 366 | 366 | 60.4±9.1 | 60.4±9.1 | 39.8 | 39.8 | NR | NR | 100 | 100 | 0 | 0 | 94.5 | 92.2 | NR | NR | NR | NR |
BITA, 6.9±2.1 SITA, 7.1±2.7 |
98.1 |
| Kinoshita, 201510 | 412 | 412 | 69±8 | 69±8 | 16 | 16 | NR | NR | 100 | 100 | 0 | 0 | NR | NR | NR | NR | NR | NR |
PSM BITA, 5.6±3.3 PSM SITA, 4.9±3.2 |
99 |
| Kurlansky, 201011 | 2197 | 2197 | 62.9±10.0 | 62.9±10.0 | 14.9 | 14.9 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
BITA, 12.7 SITA, 11.1 |
BITA=96.7 SITA=98.3 |
| Lytle, 200412 | 1152 | 1152 | 57.5±8.1 | 57.5±8.1 | 12 | 12 | NR | NR | NR | NR | NR | NR | 91 | 89 | NR | NR | NR | NR |
BITA, 16.2±2.4 SITA, 16.3±2.5 |
100 |
| Mohammadi, 201413 | 111 | 111 | 54.6±9.5 | 54.6±9.5 | 9.3 | 9.3 | NR | NR | NR | NR | NR | NR | NR | NR | 7.3±6.9 | 7.7±8.2 | NR | NR |
PSM BITA, 8.6±5.1 PSM SITA, 7.7±5.5 |
92.7 |
| Nasso, 201214 | 3584 | 3584 | 67.3±9.3 | 67.3±9.3 | 20.4 | 20.4 | 0 | 0 | NR | NR | NR | NR | 98.6 | 98.5 | NR | NR | NR | NR | 3.1 | 98 |
| Navia, 201615 | 485 | 485 | 63.7±9.1 | NR | 9.8 | NR | NR | NR | 98.4 | 98.4 | 1.6 | 1.6 | NR | NR | NR | NR | NR | NR | Median, 5.5 (IQR, 2.6–8.8) | 95 |
| Pettinari, 201416 | 892 | 892 | 73.2±2.8 | 73.2±2.8 | 26.1 | 26.1 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 3.1 | 100 |
| Rosenblum, 201617 | 306 | 306 | 59.0±10.1 | 59.0±10.1 | 15.5 | 15.5 | NR | NR | 93.5 | 79.1 | 6.5 | 20.9 | NR | NR | NR | NR | 11.2±8.7 | 11.7±9.0 | Median, 2.8 (IQR, 1.1–4.9) | 100 |
| Schwann, 201618 | 551 | 551 | 59.8±10.2 | 59.8±10.2 | 12 | 12 | 0 | 0 | 2 | 5 | 98 | 95 | NR | NR | NR | NR | NR | NR | NR | 100 |
| Toumpoulis, 200619 | 490 | 490 | 63.6±9.9 | 63.6±9.9 | 44.9 | 44.9 | NR | NR | 5.5 | 7.1 | NR | NR | NR | NR | 6.8±3.3 | 6.9±3.3 | NR | NR | 4.7±3.0 | 99.1 |
Data are given as mean±SD, unless otherwise indicated. BITA indicates bilateral internal thoracic artery; IQR, interquartile range; NR: not reported; ONCABG: on‐pump coronary artery bypass grafting; PSM: propensity score matched; SITA, single internal thoracic artery.
We found that the 10‐year survival of the control group of ART was significantly higher than that of the matched observational studies (HR, 0.86; 95% CI, 0.80–0.93; Figure [left]). The 10‐year survival of the experimental group of ART was significantly lower than that of the bilateral ITA group of the observational studies (HR, 1.11; 95% CI, 1.03–1.20). The HRs for the comparisons between the 2 groups in ART and in the matched observational studies were 0.96 (95% CI, 0.79–1.17) and 0.65 (95% CI, 0.62–0.69), respectively. The HR for the comparison between the experimental group in ART and the control arm of the observational studies was 0.89 (95% CI, 0.85–0.94). Similar results were obtained in a sensitivity analysis considering ART as‐treated results (comparing patients who received multiple arterial grafts with those who received a single arterial graft; Figure [right]).
Figure 1.
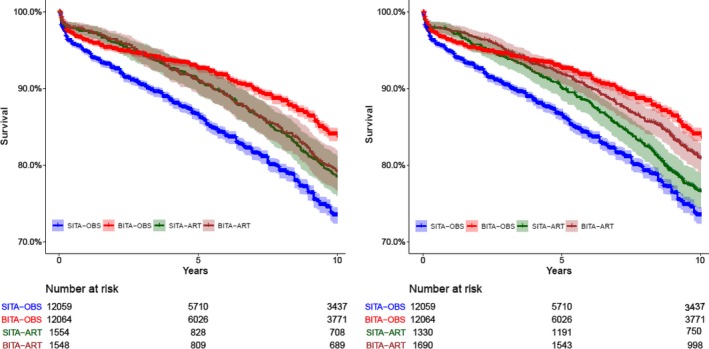
Reconstructed Kaplan‐Meier curves from individual participant‐derived data from propensity score–matched observational studies and the ART (Arterial Revascularization Trial) intention‐to‐treat (left) and as‐treated analysis (right). The hazard ratios for the as‐treated analysis were as follows: single internal thoracic artery (SITA)–ART vs SITA‐observational (OBS), 0.84 (95% CI, 0.74–0.95); multiple arterial grafts (MAG)–ART vs bilateral internal thoracic artery (BITA)–OBS, 1.19 (95% CI, 1.05–1.35); MAG‐ART vs SITA‐ART, 0.78 (95% CI, 0.67–0.92); and MAG‐ART vs SITA‐OBS, 0.67 (95% CI, 0.59–0.75).
The disagreement between the results of ART and of the observational evidence has been intensely debated. The neutral results of ART have been attributed to either the improved outcome of the control group or the lower effectiveness of the intervention.5 The first had been explained by the frequent (21.8%) use of the radial artery in the single ITA group and/or the high compliance with guideline‐directed medical therapy. The latter has been attributed to the high (13.9%) crossover rate from the experimental to the control group and to the limited experience of some of the ART surgeons.
Our results suggest that both explanations may be true, although the better outcome of the control arm is slightly predominant. The differences compared with the observational evidence were similar for the intention‐to‐treat and as‐treated analyses, suggesting that hidden confounders and treatment allocation bias in observational studies persist even after propensity matching, heavily disfavoring the control treatment group.3 Implications of our work may extend beyond coronary surgery and inform other efforts of comparative risk‐benefit analysis of complex medical or surgical cardiovascular interventions.
This analysis has limitations and must be considered exploratory. Meta‐analyses of observational studies have bias and confounders. Important data (eg, surgeon experience and details of secondary prevention) were not reported by most observational studies. In addition, digitalization and reconstruction of survival curves, although widely accepted,20 has intrinsic limitations related to the quality of the initial input and the level of information provided in the original publication. Finally, in the absence of individual patient data, the role of nonproportional hazards and censoring patterns on the outcomes could not be determined.
In conclusion, this meta‐analytic exploration of the disagreement between the results of ART and the previous observational evidence suggests that both the improved outcome of the control arm and the lower beneficial effect of the intervention had played a role and confirm the strong bias and confounders inherent even in propensity‐matched observational studies. Large randomized trials are key in answering important clinical questions and should be prioritized by health bodies and funding agencies.
Disclosures
None.
(J Am Heart Assoc. 2019;8:e014638 DOI: 10.1161/JAHA.119.014638.)
References
- 1. Tricoci P, Allen JM, Kramer JM, Califf RM, Smith SC. Scientific evidence underlying the ACC/AHA clinical practice guidelines. JAMA. 2009;301:831–841. [DOI] [PubMed] [Google Scholar]
- 2. Taggart DP, Benedetto U, Gerry S, Altman DG, Gray AM, Lees B, Gaudino M, Zamvar V, Bochenek A, Buxton B, Choong C, Clark S, Deja M, Desai J, Hasan R, Jasinski M, O'Keefe P, Moraes F, Pepper J, Seevanayagam S, Sudarshan C, Trivedi U, Wos S, Puskas J, Flather M; Arterial Revascularization Trial Investigators . Bilateral versus single internal‐thoracic‐artery grafts at 10 years. N Engl J Med. 2019;380:437–446. [DOI] [PubMed] [Google Scholar]
- 3. Gaudino M, Di Franco A, Rahouma M, Tam DY, Iannaccone M, Deb S, D'Ascenzo F, Abouarab AA, Girardi LN, Taggart DP, Fremes SE. Unmeasured confounders in observational studies comparing bilateral versus single internal thoracic artery for coronary artery bypass grafting: a meta‐analysis. J Am Heart Assoc. 2018;6:7 DOI: 10.1161/JAHA.117.008010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Neumann FJ, Sousa‐Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group . 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165. [DOI] [PubMed] [Google Scholar]
- 5. Head SJ, Kappetein AP. Coronary bypass surgery—an art for dedicated surgeons. N Engl J Med. 2019;380:489–491. [DOI] [PubMed] [Google Scholar]
- 6. Benedetto U, Amrani M, Gaer J, Bahrami T, de Robertis F, Simon AR, Raja SG; Harefield Cardiac Outcomes Research Group . The influence of bilateral internal mammary arteries on short‐and long‐term outcomes: a propensity score matching in accordance with current recommendations. J Thorac Cardiovasc Surg. 2014;148:2699–2705. [DOI] [PubMed] [Google Scholar]
- 7. Dalén M, Ivert T, Holzmann MJ, Sartipy U. Bilateral versus single internal mammary coronary artery bypass grafting in Sweden from 1997–2008. PLoS One. 2014;9:e86929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grau JB, Johnson CK, Kuschner CE, Ferrari G, Shaw RE, Brizzio ME, Zapolanski A. Impact of pump status and conduit choice in coronary artery bypass: a 15‐year follow‐up study in 1412 propensity‐matched patients. J Thorac Cardiovasc Surg. 2015;149:1027–1033. [DOI] [PubMed] [Google Scholar]
- 9. Joo H‐C, Youn Y‐N, Yi G, Chang B‐C, Yoo K‐J. Off‐pump bilateral internal thoracic artery grafting in right internal thoracic artery to right coronary system. Ann Thorac Surg. 2012;94:717–724. [DOI] [PubMed] [Google Scholar]
- 10. Kinoshita T, Asai T, Suzuki T. Off‐pump bilateral skeletonized internal thoracic artery grafting in patients with chronic kidney disease. J Thorac Cardiovasc Surg. 2015;150:315–321. [DOI] [PubMed] [Google Scholar]
- 11. Kurlansky PA, Traad EA, Dorman MJ, Galbut DL, Zucker M, Ebra G. Thirty‐year follow‐up defines survival benefit for second internal mammary artery in propensity‐matched groups. Ann Thorac Surg. 2010;90:101–108. [DOI] [PubMed] [Google Scholar]
- 12. Lytle BW, Blackstone EH, Sabik JF, Houghtaling P, Loop FD, Cosgrove DM. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg. 2004;78:2005–2014. [DOI] [PubMed] [Google Scholar]
- 13. Mohammadi S, Kalavrouziotis D, Cresce G, Dagenais F, Dumont E, Charbonneau E, Voisine P. Bilateral internal thoracic artery use in patients with low ejection fraction: is there any additional long‐term benefit? Eur J Cardiothorac Surg. 2014;46:425–431. [DOI] [PubMed] [Google Scholar]
- 14. Nasso G, Popoff G, Lamarra M, Romano V, Coppola R, Bartolomucci F, Giglio MD, Romeo F, Tavazzi L, Speziale G. Impact of arterial revascularization in patients undergoing coronary bypass. J Card Surg. 2012;27:427–433. [DOI] [PubMed] [Google Scholar]
- 15. Navia DO, Vrancic M, Piccinini F, Camporrotondo M, Dorsa A, Espinoza J, Benzadon M, Camou J. Myocardial revascularization exclusively with bilateral internal thoracic arteries in T‐graft configuration: effects on late survival. Ann Thorac Surg. 2016;101:1775–1781. [DOI] [PubMed] [Google Scholar]
- 16. Pettinari M, Sergeant P, Meuris B. Bilateral internal thoracic artery grafting increases long‐term survival in elderly patients. Eur J Cardiothorac Surg. 2014;47:703–709. [DOI] [PubMed] [Google Scholar]
- 17. Rosenblum JM, Harskamp RE, Hoedemaker N, Walker P, Liberman HA, de Winter RJ, Vassiliades TA, Puskas JD, Halkos ME. Hybrid coronary revascularization versus coronary artery bypass surgery with bilateral or single internal mammary artery grafts. J Thorac Cardiovasc Surg. 2016;151:1081–1089. [DOI] [PubMed] [Google Scholar]
- 18. Schwann TA, Hashim SW, Badour S, Obeid M, Engoren M, Tranbaugh RF, Bonnell MR, Habib RH. Equipoise between radial artery and right internal thoracic artery as the second arterial conduit in left internal thoracic artery‐based coronary artery bypass graft surgery: a multi‐institutional study. Eur J Cardiothorac Surg. 2016;49:188–195. [DOI] [PubMed] [Google Scholar]
- 19. Toumpoulis IK, Anagnostopoulos CE, Balaram S, Swistel DG, Ashton RC, DeRose JJ. Does bilateral internal thoracic artery grafting increase long‐term survival of diabetic patients? Ann Thorac Surg. 2006;81:599–606. [DOI] [PubMed] [Google Scholar]
- 20. Guyot P, Ades A, Ouwens MJ, Welton NJ. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan–Meier survival curves. BMC Med Res Methodol. 2012;12:9. [DOI] [PMC free article] [PubMed] [Google Scholar]


