Abstract
Background
It is critically important to assess the prognostic value of NT-proBNP in the form of repeated measures among children undergoing surgery for congenital heart defects (CHD). The aim of the present study is to assess the value of repeated perioperative NT-proBNP in evaluating the time dependent and temporal trajectory in prognostics diagnosis during the perioperative period in a large series of children with CHD.
Methods
Repeated measures of NT-proBNP from 329 consecutive children with CHD were obtained before and 1, 12, and 36 h after surgery, respectively. For fully utilizing longitudinal characteristics, we employed parallel cross-sectional logistic regression, a two stage mixed effect model and trajectories over time analysis to mine the predictive value of perioperative NT-proBNP on the binary outcome of prolonged intensive care unit (ICU) stay.
Results
The two stage mixed effects model confirmed that both the mean NT-proBNP level (aOR = 1.46, P = 0.001) and the time trends had prognostic value on the prediction of prolonged ICU stay. In the fully adjusted logistic regression analyses based on gaussian distributions, “rapidly rising NT-proBNP” put the subjects at 5.4-times higher risk of prolonged ICU stay compared with “slowly rising” group (aOR = 5.40, P = 0.003).
Conclusions
Comprehensive assessment of the time dependent and temporal trajectory in perioperative NT-proBNP, indicated by repeated measurements, can provide more accurate identification of children with higher risk of prolonged ICU stay after CHD surgery.
Keywords: NT-proBNP, Congenital heart defects, Repeated measures, Prognosis
Background
Congenital heart disease (CHD) accounts for nearly 1/3 of all major congenital anomalies (9 per 1000 live births) [1]. Although the improvements in surgical intervention have significantly benefited children with CHD, the incidence of adverse postoperative outcomes remains about 27% [2]. Thus, the identification of prognostic biomarkers for adverse outcome could confer multiple benefits. The guidelines published by the European Society of Cardiology(2016) recommend the clinical biomarkers Brain natriuretic peptide (BNP) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) for diagnosis and prognosis of heart failure [3]. At present, some evidence have pointed out the prognostic value of BNP after surgical intervention for CHD in pediatrics [4–7]. Compared to BNP, NT-proBNP transportation is more stable, and its half-life in serum is longer than that of BNP [8]. Therefore, NT-proBNP becomes more important and better marker of cardiac strain over time.
Some researches pointed out the prognostic value of NT-proBNP after surgical intervention for CHD. Walsh [9] et al. found the preoperative NT-proBNP level was a significant predictor of duration of intensive care unit (ICU) stay and peak postoperative level was a predictor of the intensity of overall medical management. They attained NT-proBNP preoperatively and at 2, 12, 24, 48 and 72 h after surgery and just used related analysis to explore the relation between NT-proBNP level and outcome. Goei [10] et al. demonstrated that the difference in NT-proBNP between pre and postoperative was the strongest independent predictor of cardiac outcome. They applied multivariate Cox regression analyses to evaluate the relation between the change in NT-proBNP levels and the study end point. And Michael [11] et al. also assessed a reduction in NT-proBNP had a lower subsequent rate of cardiovascular death or HF hospitalization. Qu [12] et al. have confirmed that time-varying NT-proBNP level, particularly 1-h postoperative levels, had prognostic value on the prediction of outcome after surgery.
Compared with a single measurement, perioperative serial NT-proBNP measurements were more accurate in predicting postoperative adverse events, since it can take into account the hemodynamic stress caused by anesthesia and surgery [10, 13]. However, there is no general consensus on methods for examining data with a longitudinal repeated variable and non-time-varying outcome. Chronological order is often ignored in routine characteristics. In order to overcome the shortcomings from routine characteristics and in-depth dig the values of repeated measurement data, the use of time dependent assessment based on the approach of two stage mixed effects model for clinical trial analyses has recently gained broad supports [14, 15]. This model is more flexible than the previous approaches, and does not require sphericity of the covariance data structure [16]. And this model characterizes within-subject patterns of longitudinal measurements, and the association between features of the longitudinal measurements process and the duration of outcome events. Therefore, our study would use this model to assess NT-proBNP prognostic value of the time dependent effect.
In addition, temporal trajectory of NT-proBNP levels in patients has been confirmed to be the powerful diagnostic and prognostic indicator available in treatment of kidney or heart disease [17–19]. Trajectories over time allow to assess how the measured data has changed through two or more assessment points. In this study, we would combined the temporal trajectory analysis to dig more prognostic value from the repeated perioperative NT-proBNP.
Therefore, the aim of the present study is to assess the value of repeated perioperative NT-proBNP in evaluating the time dependent and temporal trajectory in prognostics diagnosis.
Methods
Subjects and data collection
This retrospective study was conducted at Guangzhou Women and Children’s Medical Center. We derived the data from the clinical system databases, 364 eligible consecutive patients undergoing CHD surgery at this hospital between June and December 2014. Patients younger than 18 years with CHD who underwent cardiac surgery were eligible for the study. Children who had preoperative arrhythmia (potentially malignant ventricular arrhythmias and high-degree atrioventricular block), rheumatic heart disease, infective endocarditis, myocarditis, pericardial disease, renal dysfunction, or neoplasms, or who could not be separated from cardiopulmonary bypass (CPB) were excluded. Thus, results from 329 cases were presented in this study, which with complete clinical information were included.
Plasma NT-proBNP levels were determined in each patient at preoperative, 1 h, 12 h and 36 h postoperatively, respectively. The NT-proBNP levels were measured with a commercially available fluorescence immunoassay (competitive Enzyme Immuno Assay; ReLIA II, Shenzhen, China) and Multi-Detection Microlpate Reader (VICTOR X5; PerkinElmer, Waltham, Mass). Clinical and biochemical data were collected retrospectively form the medical records, including patient demographics (age, weight, gender), the Risk Adjustment in Congenital Heart Surgery, version 1(RACHS-1) score, Cardiopulmonary bypass (CPB) duration, aorta cross clamp (ACC) time and follow-up measurements after surgery: the duration of Intensive Care Unit (ICU). The primary outcome measure was the prolonged ICU stay, as the short-term adverse outcome to estimate prognostic [20].. And the patients were divided two groups: ICU stay <= 3 days and ICU stay > 3 days according to the mean duration of ICU stay, which was 3.0 days with a median (interquartile range [IQR]) of (2–5) days (As shown in Additional file 1: Figure S1).
Data analysis
Continuous variables were showed as mean and standard deviation and compared by using the 1-way analysis of variance for 2-group comparisons. Categorical variables were expressed as percentages and compared by using the Fisher exact test or the X2 test. NT-proBNP were compared between the two groups and was log-transformed to obtain normality. A parallel cross-sectional logistic regression model was built to evaluate the relation between NT-proBNP and prolonged ICU stay. Multivariate regression analyses were adjusted for cardiac risk factors and factors recognized to influence NT-proBNP levels: age, gender, RACHS-1, Weight, CPB time and ACC time.
Statistical analysis was performed using R software, version 3.3.2. The package of nlme was used for two stage mixed effects analysis. Mclust package was the optimal model for parameterized Gaussian mixture clustering by hierarchical clustering. The results of the logistic regression model analyses are presented as odds ratios (ORs) with 95% CIs. P < 0.05 considered statistically significant.
In addition, we applied two methods, time dependent assessment and trajectories over time, to explore whether the change of NT-proBNP could predict the postoperative recovery of children patients undergoing CHD surgery. For time dependent assessment, we proposed a two stage mixed effects model as followed. In stage 1, the longitudinally time-varying NT-proBNP level was first modeled using a linear mixed effects (LME) model. In the second stage, best linear unbiased predictor (BLUP) estimated of the random coefficients from LME model were used as predictors in a logistic regression model.
For trajectories over time, the statistical analysis also included two steps. First, subject-specific NT-proBNP levels were clustered based on Gaussian distributions with a predetermined number of clusters (K). Correspondingly, each subject was grouped into one of the K clustered trajectories. Second, to examine the association between trajectory groups over 4 peri-operative assessment points and the binary outcome of prolonged ICU stay, we regressed Yi on this trajectory index along with the covariates as:
| 1 |
where Ci is the clustering trajectory index, which may be more than one-dimensional when K > 2.
Second, we added clusters of NT-proBNP into the logistic regression model adjusted other risk factors to assess the effect of trajectories over time of NT-proBNP with the CHD pediatric prognostics after surgery.
Results
Study group characteristics
The patients’ clinical characteristics were listed in Table 1. Patients were grouped according to length of stay in the ICU: group1, 3 days or less (n = 181; 55.02%) and group 2, more than 3 days (n = 148; 44.98%). With the exception of gender, all the other clinical baseline characteristics showed significant differences between the two groups (all P < 0.001) (Table 2).
Table 1.
Clinical characteristics of children undergoing congenital heart disease surgery
| Characteristics | ICU stay <=3 days |
|---|---|
| Type of congenital heart disease | |
| Ventricular septal defect | 163(49.59) |
| Atrial septal defect | 34(10.47) |
| Total anomalous pulmonary venous connection | 12(3.58) |
| Tetralogy of Fallot | 24(7.44) |
| Transposition of the great arteries | 23(6.89) |
| Pulmonary atresia | 18(5.51) |
| Complete atrioventricular septal defect | 14(4.13) |
| Coarctation | 15(4.68) |
| Double outlet right ventricle | 5(1.65) |
| Interrupted aortic arch | 2(0.55) |
| Pulmonary stenosis | 5(1.38) |
| Other types of CHD | 14(4.13) |
| NT-proBNP level, pg/ml | |
| Before surgery | 2744.28±5158.85 |
| 1h after surgery | 2564.19±4363.56 |
| 12h after surgery | 6797.01±6260.35 |
| 36h after surgery | 4727.21±4321.34 |
| Gender | |
| Female | 117(35.56) |
| Male | 212(64.44) |
| RACHS-1 score | |
| I/II | 251(76.29) |
| III/IV | 78(23.71) |
| Age, d | 416.93±753.44 |
| Weight, kg | 7.05±5.39 |
| Cardiopulmonary bypass time, min | 84.87±45.47 |
| Aortic crossclamp time, min | 43.66±26.26 |
Categorical data are showed as n (%) responding group respectively. Continuous variables are showed as mean ± standard deviation. ICU Intensive Care Unit, RACHS-1 Risk Adjustment for Congenital Heart Surgery-1
Table 2.
Clinical characteristics of children with ICU stay time equal or less than 3 days and children with ICU stay time greater than 3 days undergoing CHD correction
| Characteristics | ICU stay <=3 days | ICU stay >3 days | p |
|---|---|---|---|
| Patient number | 181(55.02) | 148(44.98) | |
| NT-proBNP level, pg/ml | |||
| Before surgery | 1214.07±2935.61 | 4615.68±6500.49 | <0.001 |
| 1h after surgery | 1045.29±1743.52 | 4421.76±5686.58 | <0.001 |
| 12h after surgery | 4714.70±5379.54 | 9343.61±6320.02 | <0.001 |
| 36h after surgery | 3076.17±2474.08 | 6746.39±5158.98 | <0.001 |
| Gender | |||
| Female | 68(37.57) | 49(33.11) | 0.42 |
| Male | 113(62.43) | 99(66.89) | |
| RACHS-1 score | |||
| I/II | 165(91.16) | 86(58.11) | <0.001 |
| III/IV | 16(8.84) | 62(41.89) | |
| Age, d | 573.62±900.76 | 225.31±450.45 | <0.001 |
| Weight, kg | 8.56±6.38 | 5.20±2.94 | <0.001 |
| Cardiopulmonary bypass time, min | 66.40±25.82 | 107.46±53.41 | <0.001 |
| Aortic crossclamp time, min | 34.57±16.46 | 54.78±31.25 | <0.001 |
Categorical data are showed as n (%) responding group respectively. Continuous variables are showed as mean ± standard deviation. ICU Intensive Care Unit. RACHS-1 Risk Adjustment for Congenital Heart Surgery-1
The higher level of perioperative NT-proBNP was a potential prognostic factor for longer stay in ICU. In both groups, the level of postoperative NT-proBNP showed a rising trend regardless of preoperative condition and reached the peak at 12 h after operation (Fig. 1).
Fig. 1.
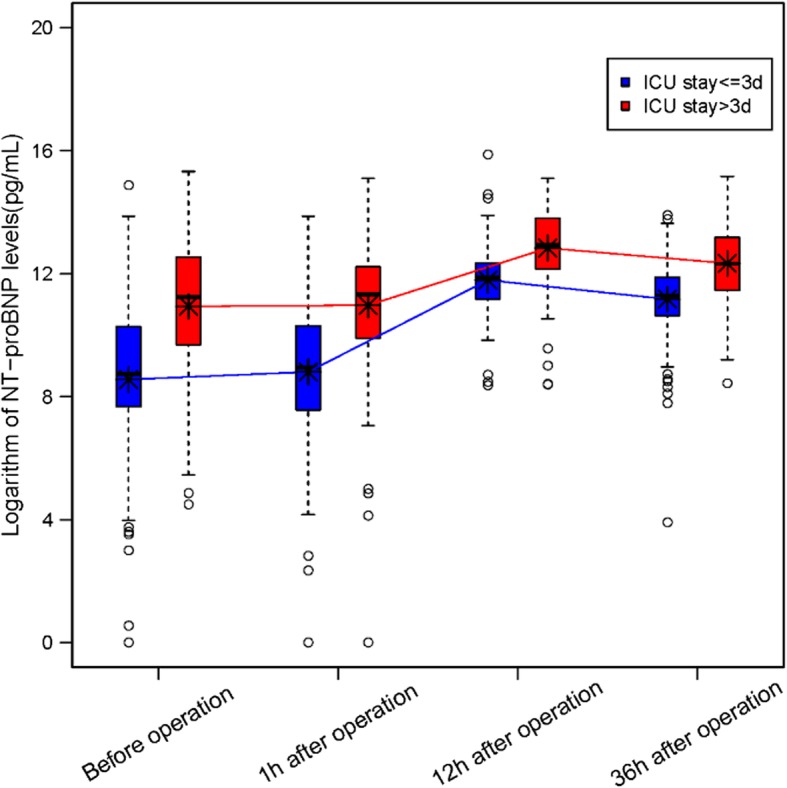
The comparisons of NT-proBNP levels between two groups at different time. Group 1(ICU stay <=3 days, blue color) and group 2(ICU stay > 3, red color) at before surgery, 1 hour, 12 hours, 36 hours after CHD surgery. Boxes show the interquartile range, and solid black lines show the median of NT-proBNP levels. Asterisks present the mean of NT-proBNP levels. All the NT-proBNP levels were logarithm transformed
Prognostic value of time independent assessment of perioperative NT-proBNP on prolonged ICU stay
Parallel cross-sectional logistic regression models for prognostic value of time independent assessment are presented in Table 2. After adjustment for potential confounding factors, the values of NT-proBNP at each of the four times were non-statistically significant associated with prolonged ICU stay (Table 3).
Table 3.
Prognostic value of time independent assessment of repeated perioperative NT-proBNP on prolonged ICU stay
| Variables | Estimate | SE | ORa | 95% CI | p |
|---|---|---|---|---|---|
| Method Parallel cross-sectional logistic regression models | |||||
| Before surgery | 0.17 | 0.094 | 1.19 | 0.99 to 1.43 | 0.070 |
| 1h after surgery | 0.083 | 0.10 | 1.09 | 0.89 to 1.34 | 0.42 |
| 12h after surgery | 0.086 | 0.18 | 1.09 | 0.77 to 1.57 | 0.64 |
| 36h after surgery | 0.24 | 0.17 | 1.27 | 0.91 to 1.81 | 0.16 |
SE standard error, OR odds ratio, CI confidence interval. a-Models adjusted for age, gender, weight, cardiopulmonary bypass time, aorta cross clamp time, and RACHS-1 score
Prognostic value of time dependent assessment of perioperative NT-proBNP on prolonged ICU stay
We used two stage mixed effects model to further investigate the time dependent prognostic value of NT-proBNP. As exhibited in Table 4, patient-specific intercepts and visit-specific slopes were first extracted from Stage 1 and then continuously modeled in Stage 2. The results suggested that there was an association between the patient-specific intercepts and prolonged ICU stay(β = 0.38, SE = 0.11, aOR = 1.46, P = 0.001). Controlled factors mentioned in Table 4 and the time effect, this model showed the higher level of NT-proBNP predicted the higher risk of prolonged ICU stay. Furthermore, compared with before surgery, two effect estimates for both 12 h and 36 h postoperative time points were statistically significant (P = 0.01 and 0.004, respectively). This demonstrated that both the mean NT-proBNP exposure level and the time trends, as indicated by the patient-specific intercept and visit-specific slopes, respectively, were associated with prolonged ICU stay.
Table 4.
Prognostic value of time dependent assessment of perioperative NT-proBNP on prolonged ICU stay (Two stage mixed effects model)
| Variables | Estimate | SE | ORa | 95% CI | p |
|---|---|---|---|---|---|
| The first submodel | |||||
| Intercept | 10.74 | 0.53 | 4.60×104 | 1.64×104 to 1.29×105 | <0.0001 |
| Time points | |||||
| Before surgery | Reference | ||||
| 1h after surgery | 0.15 | 0.12 | 1.16 | 0.93 to 1.46 | 0.19 |
| 12h after surgery | 2.63 | 0.12 | 13.90 | 11.07 to 17.45 | <0.0001 |
| 36h after surgery | 2.07 | 0.12 | 7.89 | 6.29 to 9.91 | <0.0001 |
| Gender | |||||
| Female | Reference | ||||
| Male | -0.13 | 0.086 | 0.88 | 0.74 to 1.04 | 0.12 |
| RACHS-1 | |||||
| I/II | Reference | ||||
| III/IV | 0.52 | 0.12 | 1.68 | 1.32 to 2.14 | <0.0001 |
| Age, d | -0.14 | 0.046 | 0.87 | 0.79 to 0.95 | 0.002 |
| Weight, kg | -1.18 | 0.12 | 0.31 | 0.24 to 0.39 | <0.0001 |
| CPB time, min | 0.41 | 0.10 | 1.51 | 1.23 to 1.85 | <0.0001 |
| ACC time, min | 0.069 | 0.064 | 1.07 | 0.95 to 1.21 | 0.28 |
| The second submodel | |||||
| NT-proBNP levels | 0.38 | 0.11 | 1.46 | 1.19 to 1.84 | 0.001 |
| Time points | |||||
| Before surgery | Reference | ||||
| 1h after surgery | 0.51 | 0.28 | 1.67 | 0.98 to 2.90 | 0.06 |
| 12h after surgery | -1.91 | 0.76 | 0.15 | 0.03 to 0.65 | 0.01 |
| 36h after surgery | 1.59 | 0.55 | 4.92 | 1.72 to 14.89 | 0.004 |
| Gender | |||||
| Female | Reference | ||||
| Male | 0.09 | 0.19 | 1.09 | 0.76 to 1.60 | 0.64 |
| RACHS-1 | |||||
| I/II | Reference | ||||
| III/IV | 0.87 | 0.36 | 2.38 | 1.20 to 5.02 | 0.02 |
| Age, d | -1.08 | 3.18 | 0.34 | 6.7×10-4 to 1.82×102 | 0.73 |
| Weight, kg | 1.03 | 0.92 | 2.81 | 0.45 to 17.25 | 0.26 |
| CPB time, min | -2.33 | 1.75 | 0.097 | 0.003 to 3.56 | 0.18 |
| ACC time, min | -0.69 | 3.17 | 0.50 | 0.001 to 258.16 | 0.83 |
SE standard error, OR odds ratio, CI confidence interval, CPB cardiopulmonary bypass, ACC aorta cross clamp, RACHS-1 Risk Adjustment for Congenital Heart Surgery-1. a-Models adjusted for age, gender, weight, cardiopulmonary bypass time, aorta cross clamp time, and RACHS-1 score
The prognostic value of perioperative NT-proBNP levels trajectories on prolonged ICU stay
According to Bayesian information criterion (BIC), the number of clusters chose was two, based on Post−/Pre-(log NT-proBNP) ratio. The average ratios of the NT-proBNP levels within each cluster by time point were displayed in Fig. 2. The trajectory of NT-proBNP levels of cluster 1 elevated slowly over time, whereas rose rapidly in cluster 2. In detail, 87% of subjects fell into cluster 1 and 13% of them fell into cluster 2.
Fig. 2.
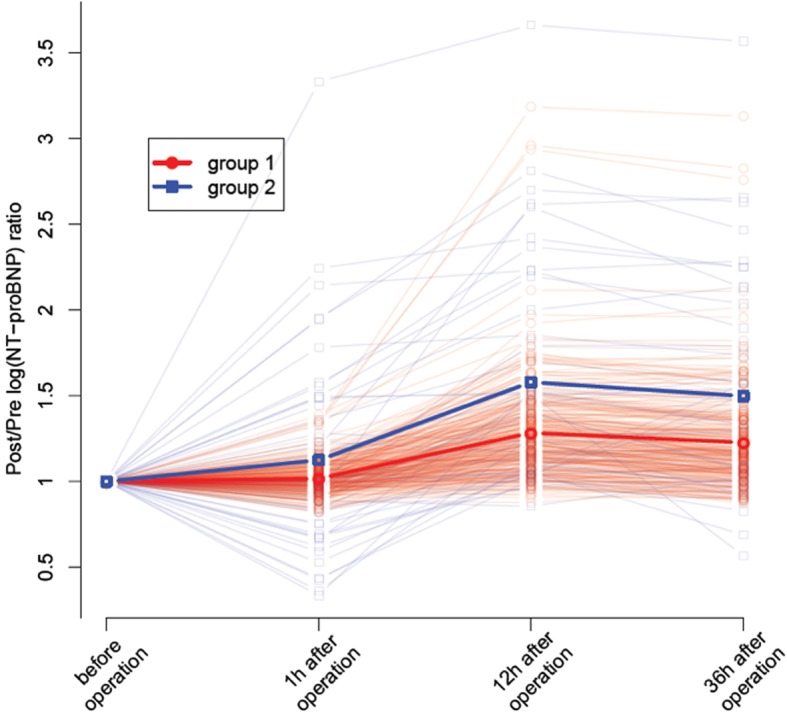
Comparisons of postoperative changes of NT-proBNP ratios over time between two clusters by Gaussian mixture clustering model. Red solid line represents mean of slowly rising group. Blue solid line represents mean of fast rising group. Semi-transparant lines represents ratio of NT-proBNP levels in every children with CHD undergoing cardiac surgery. The scale of y axis is log transformed
We then modeled each clustering index in relation to odds of suffering a prolonged ICU stay. As indicated in Table 5, compared with the odds for children in cluster 1, the odds of suffering a prolonged ICU stay for children in cluster 2 was 5.4 times (β = 1.67, SE = 0.56, aOR = 5.40, P = 0.003). It means that patients with rising rapidly NT-proBNP levels postoperative might have poorer postoperative recovery.
Table 5.
Prognostic value of trajectories over time of repeated perioperative NT-proBNP on prolonged ICU stay
| Variables | Estimate | SE | OR | 95% CI | p |
|---|---|---|---|---|---|
| Intercept | -7.83 | 1.97 | 4.0×10-4 | 7.27×10-6 to 1.70×10-2 | <0.0001 |
| Trajectories over time | |||||
| Cluster 1 | Reference | ||||
| Cluster 2 | 1.67 | 0.56 | 5.40 | 1.82 to 16.76 | 0.003 |
| Gender | |||||
| Female | Reference | ||||
| Male | -0.12 | 0.31 | 0.89 | 0.48 to 1.62 | 0.70 |
| RACHS-1 | |||||
| I/II | Reference | ||||
| III/IV | 0.46 | 0.45 | 1.59 | 0.66 to 3.84 | 0.30 |
| Age, d | 0.17 | 0.19 | 1.19 | 0.81 to 1.73 | 0.36 |
| Weight, kg | -2.81 | 0.60 | 0.060 | 0.02 to 0.18 | <0.0001 |
| CPB time, min | 2.51 | 0.42 | 12.33 | 5.68 to 29.54 | <0.0001 |
| ACC time, min | -0.46 | 0.22 | 0.63 | 0.39 to 0.95 | 0.03 |
SE standard error, OR odds ratio, CI confidence interval, CPB cardiopulmonary bypass, ACC aorta cross clamp, RACHS-1 Risk Adjustment for Congenital Heart Surgery-1. a-Models adjusted for age, gender, weight, cardiopulmonary bypass time, aorta cross clamp time, and RACHS-1 score
Discussion
The principal findings of this study are as follows: (1) the higher perioperative NT-proBNP level prolonged ICU stay for pediatric patients with CDH after surgery; (2) both the mean NT-proBNP exposure level and the time trends were associated with prolonged ICU stay; (3) patients with rising rapidly perioperative NT-proBNP level suffer higher risk of prolonged ICU stay.
Firstly, we carried out assessment of prognostic value within other influence factors (CPB time, ACC time, gender, age, weight and RACHS-1 score). Some studies have pointed out that CPB duration is an independent predictor of adverse outcomes after cardiac surgery [21]. CPB also influenced BNP/NT-proBNP levels proportionally, which was confirmed in our first sub-model of two stage mixed effects model. The inconsistencies among previous findings that prolonged ACC time significantly correlated with major post-operative adverse events [22], were due to strong correlation between CPB time and ACC time [23]. Here, we found the correlation coefficient was 0.84 (P < 0.001) in our results (Additional file 1: Figure S2). Regardless of the variable of CPB time, length of ACC time restored predictive ability correctly in multiple models (data not shown). RACHS-1 was created to compare in-hospital mortality for children undergoing CHD surgery and demonstrated available for prediction of ICU stay length [24]. To a certain extent, our results supported that, RACHS-1 risk category was positively correlated with length of ICU stay in two stage mixed effect model. Other variables, such as age and gender almost showed not significant association with adverse outcomes.
Increasing evidence pointed out that the change in NT-proBNP have been shown to play key roles as prognostic biomarkers in patient undergoing cardiac surgery for CHD correction [10, 25]. Similar results were reported that the higher NT-proBNP could predict the longer duration of ICU stay [9] . Our results found that children stay in ICU longer than 3 days showed higher level NT-proBNP at each time point, which confirmed NT-proBNP has predictive value in pediatric CHD patient undergoing surgery. Otherwise, our result showed the peak level of NT-proBNP at 12 h after surgery, which Jiangbo had discuss before [12]. Then we further developed a parallel cross-sectional logistic regression model with covariate, like age or gender, to analysis the predictive value of each time point. However, the result of this model showed that NT-proBNP levels at each time point had no significant effect on the incidence of prolonged ICU stay. According to previous study [11, 12], we assumed that the time effect might play a role. So, we chose two stage mixed effects model to investigate time dependent prognostic value of perioperative NT-proBNP. Results from this model indicated that the mean level of NT-proBNP, especially at the 12 h and 36 h postoperative time points, significantly correlated to duration of ICU stay. Surprisingly, compared to the level of before surgery, NT-proBNP levels at 12 h after surgery, the peak level after surgery, was negatively associated with outcome event. After considering the time effect of the NT-proBNP with prolong.
ed. ICU stay, the peak NT-proBNP level become negative effect with the risk of longer prolonged ICU. It suggested that it is not accurate enough to judge the prognosis of CHD children solely based on the indicators of a single time point, like the peak time point.
So we further used temporal trajectory analysis to dig more prognostic value of temporal trajectories of perioperative NT-proBNP levels in patients. Although NT-proBNP has been confirmed to be the powerful diagnostic and prognostic indicator available in treatment of kidney or heart disease [17–19], to our knowledge, this is the first study to assess the prognostic value of temporal trajectory of longitudinal NT-proBNP levels by clustering model in children undergoing cardiac surgery for CHD. When patients undergo surgical procedures, the NT-proBNP levels at specific time points was closely related to individual basal secretion, so using conventional characteristic directly to predict the incidence of heart defects was highly susceptible. In our study, the time trajectory of NT-proBNP was proven to be a better prognostic indicator, since it can reflect an acute change in volume state or left ventricular function that influenced subsequent risk of adverse event. Clinicians might could judge the prognosis of patients by considering the speed of changes of NT-proBNP to adjust their medical decision.
Conclusions
In conclusion, compared with single measurement, repeated measures of perioperative NT-proBNP levels were regarded as a more valuable predictor of ICU stay time length for CHD children undergoing open heart operation. Both the mean NT-proBNP exposure levels and the time trends were associated with prolonged ICU stay, and patients with rising rapidly perioperative NT-proBNP level suffer higher risk of prolonged ICU stay. Further studies are needed to confirm how the time trajectory of NT-proBNP can be used in clinical practice to predict postoperative risk and if repeated measurements of perioperative NT-proBNP should be performed during postoperative management to identify CHD children at high risk of adverse events.
Supplementary information
Additional file 1. Figure S1. The vioplot of duration of ICU stay among 329 patients. Black box shows the interquartile range, solid white point shows the median of NT-proBNP levels, and black lines extend out from the box are up and down whiskers lines. The external shape with pink color is the kernel density estimation, which presents the population distribution among ICU stay time. Figure S2. The dash line showed CPB duration strongly correlated with AACC time. Cardiopulmonary bypass (CPB) duration strongly correlated with Aortic cross-clamping (ACC) time. Dash line is the regression between CPB duration and ACC time. Correlation coefficient is 0.84 and p value is less than 0.001.
Acknowledgments
The authors thank the doctors and nurses at the Department of Heart Center, Guangzhou Women and Children’s Medical Center, in particular Xinxin Chen, MD, and his team of surgeons.
We are grateful to all of the subjects and their caretakers.
Abbreviations
- ACC
Aorta cross clamp
- BLUP
Best linear unbiased predictor
- BNP
Brain natriuretic peptide
- CHD
Congenital heart defects
- CPB
Cardiopulmonary bypass (CPB) duration
- ICU
Intensive care unit
- LME
Linear mixed effects
- NT-proBNP
N-terminal pro-B-type natriuretic peptide
- RACHS-1
the Risk Adjustment in Congenital Heart Surgery, version 1
Authors’ contributions
FL and LZ edited the manuscript. FL, LZ and HL conceived and designed the study. All authors reviewed and revised the manuscript. All authors read and approved the manuscript. YC, WC and RG as pediatric doctors took part in designing of the study and gave clinical advices. HL participated the work of analysis. XC, HX and HL were responsible for ensuring that all listed authors have approved the manuscript and guiding the whole study.
Funding
This work was supported by the Guangzhou Institute of Pediatrics/Guangzhou Women and Children’s Medical Center [NO: KCP-2016-002] and the National Natural Science Foundation of China (Grant no.81401755). The first funding supported us to carry out this study including design and data collection. And the second funding mainly provided us sources to learn the statistics methods and scientific research. Both of the funding supported us to accomplish the study and the manuscript.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
This work was approved by the commit of Guangzhou Women and Children’s Medical Center. The use of human subjects in this research has complied with all the relevant national regulations and institutional policies. All participants in the study gave their written informed consent. The research was approved by the author’s equivalent committee.
Consent for publication
All of authors have agreed to publication on BMC Pediatrics.
Competing interests
No conflict of interest exits in the submission of this manuscript. All authors have read and approved this version of the article, and due care has been taken to ensure the integrity of the work.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Fangqin Lin and Lingling Zheng contributed equally to this work.
Contributor Information
Xinxin Chen, Email: chenxinxin@gwcmc.org.
Huimin Xia, Email: huimin.xia876001@gmail.com.
Huiying Liang, Email: lianghuiying@hotmail.com.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12887-019-1830-y.
References
- 1.van der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ, Roos-Hesselink JW. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;58(21):2241–2247. doi: 10.1016/j.jacc.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 2.Parker DM, Everett AD, Stabler ME, Vricella L, Jacobs ML, Jacobs JP, Parikh CR, Pasquali SK, Brown JR. Novel biomarkers improves prediction of 365-day readmission after pediatric congenital heart surgery. Ann Thorac Surg. 2019. [DOI] [PMC free article] [PubMed]
- 3.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 4.Hsu JH, Keller RL, Chikovani O, Cheng H, Hollander SA, Karl TR, Azakie A, Adatia I, Oishi P, Fineman JR. B-type natriuretic peptide levels predict outcome after neonatal cardiac surgery. J Thorac Cardiov Sur. 2007;134(4):939–945. doi: 10.1016/j.jtcvs.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 5.Niedner MF, Foley JL, Riffenburgh RH, Bichell DP, Peterson BM, Rodarte A. B-type natriuretic peptide: perioperative patterns in congenital heart disease. Congenit Heart Dis. 2010;5(3):243–255. doi: 10.1111/j.1747-0803.2010.00396.x. [DOI] [PubMed] [Google Scholar]
- 6.Nahum E, Pollak U, Dagan O, Amir G, Frenkel G, Birk E. Predictive value of B-type natriuretic peptide level on the postoperative course of infants with congenital heart disease. Isr Med Assoc J. 2013;15(5):216–220. [PubMed] [Google Scholar]
- 7.Cantinotti M, Giordano R, Scalese M, Molinaro S, della Pina F, Storti S, Arcieri L, Murzi B, Marotta M, Pak V, et al. Prognostic role of BNP in children undergoing surgery for congenital heart disease: analysis of prediction models incorporating standard risk factors. Clin Chem Lab Med. 2015;53(11):1839–1846. doi: 10.1515/cclm-2014-1084. [DOI] [PubMed] [Google Scholar]
- 8.Mir TS, Haun C, Lilje C, Laer S, Weil J. Utility of N-terminal brain natriuretic peptide plasma concentrations in comparison to lactate and troponin in children with congenital heart disease following open-heart surgery. Pediatr Cardiol. 2006;27(2):209–216. doi: 10.1007/s00246-005-1152-8. [DOI] [PubMed] [Google Scholar]
- 9.Walsh R, Boyer C, LaCorte J, Parnell V, Sison C, Chowdhury D, Ojamaa K. N-terminal B-type natriuretic peptide levels in pediatric patients with congestive heart failure undergoing cardiac surgery. J Thorac Cardiovasc Surg. 2008;135(1):98–105. doi: 10.1016/j.jtcvs.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 10.Goei D, van Kuijk JP, Flu WJ, Hoeks SE, Chonchol M, Verhagen HJM, Bax JJ, Poldermans D. Usefulness of repeated N-terminal pro-B-type natriuretic peptide measurements as incremental predictor for long-term cardiovascular outcome after vascular surgery. Am J Cardiol. 2011;107(4):609–614. doi: 10.1016/j.amjcard.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 11.Zile MR, Claggett BL, Prescott MF, McMurray JJV, Packer M, Rouleau JL, Swedberg K, Desai AS, Gong JJ, Shi VC, et al. Prognostic implications of changes in N-terminal pro-B-type natriuretic peptide in patients with heart failure. J Am Coll Cardiol. 2016;68(22):2425–2436. doi: 10.1016/j.jacc.2016.09.931. [DOI] [PubMed] [Google Scholar]
- 12.Qu JB, Liang HY, Zhou N, Li LJ, Wang YF, Li JB, Cui YQ. Perioperative NT-proBNP level: potential prognostic markers in children undergoing congenital heart disease surgery. J Thorac Cardiov Sur. 2017;154(2):631–640. doi: 10.1016/j.jtcvs.2016.12.056. [DOI] [PubMed] [Google Scholar]
- 13.Sandhu S, Har BJ, Aggarwal SG, Kavanagh KM, Ramadan D, Exner DV, Investigators R. Predictive value of repeated versus single N-terminal pro B-type natriuretic peptide measurements early after-myocardial infarction. Pace. 2009;32:S86–S89. doi: 10.1111/j.1540-8159.2008.02259.x. [DOI] [PubMed] [Google Scholar]
- 14.Donohue MC, Aisen PS. Mixed model of repeated measures versus slope models in Alzheimer's disease clinical trials. J Nutr Health Aging. 2012;16(4):360–364. doi: 10.1007/s12603-012-0047-7. [DOI] [PubMed] [Google Scholar]
- 15.Andersen SW, Millen BA. On the practical application of mixed effects models for repeated measures to clinical trial data. Pharm Stat. 2013;12(1):7–16. doi: 10.1002/pst.1548. [DOI] [PubMed] [Google Scholar]
- 16.Maurissen JP, Vidmar TJ. Repeated-measure analyses: which one? A survey of statistical models and recommendations for reporting. Neurotoxicol Teratol. 2017;59:78–84. doi: 10.1016/j.ntt.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 17.Roberts MA, Hare DL, Sikaris K, Ierino FL. Temporal trajectory of B-type natriuretic peptide in patients with CKD stages 3 and 4, dialysis, and kidney transplant. Clin J Am Soc Nephrol. 2014;9(6):1024–1032. doi: 10.2215/CJN.08640813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beltrami Matteo, Ruocco Gaetano, Ibrahim Aladino, Lucani Barbara, Franci Beatrice, Nuti Ranuccio, Palazzuoli Alberto. Different trajectories and significance of B-type natriuretic peptide, congestion and acute kidney injury in patients with heart failure. Internal and Emergency Medicine. 2017;12(5):593–603. doi: 10.1007/s11739-017-1620-1. [DOI] [PubMed] [Google Scholar]
- 19.Greene SJ, Maggioni AP, Fonarow GC, Solomon SD, Bohm M, Kandra A, Prescott MF, Reimund B, Hua TA, Lesogor A, et al. Clinical profile and prognostic significance of natriuretic peptide trajectory following hospitalization for worsening chronic heart failure: findings from the ASTRONAUT trial. Eur J Heart Fail. 2015;17(1):98–108. doi: 10.1002/ejhf.201. [DOI] [PubMed] [Google Scholar]
- 20.Qu Jiangbo, Liang Huiying, Zhou Na, Li Lijuan, Wang Yanfei, Li Jianbin, Cui Yanqin. Perioperative NT-proBNP level: Potential prognostic markers in children undergoing congenital heart disease surgery. The Journal of Thoracic and Cardiovascular Surgery. 2017;154(2):631–640. doi: 10.1016/j.jtcvs.2016.12.056. [DOI] [PubMed] [Google Scholar]
- 21.Salis S, Mazzanti VV, Merli G, Salvi L, Tedesco CC, Veglia F, Sisillo E. Cardiopulmonary bypass duration is an independent predictor of morbidity and mortality after cardiac surgery. J Cardiothor Vasc An. 2008;22(6):814–822. doi: 10.1053/j.jvca.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Al-Sarraf N, Thalib L, Hughes A, Houlihan M, Tolan M, Young V, McGovern E. Cross-clamp time is an independent predictor of mortality and morbidity in low- and high-risk cardiac patients. Int J Surg. 2011;9(1):104–109. doi: 10.1016/j.ijsu.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Nissinen J, Biancari F, Wistbacka JO, Peltola T, Loponen P, Tarkiainen P, Virkkila M, Tarkka M. Safe time limits of aortic cross-clamping and cardiopulmonary bypass in adult cardiac surgery. Perfusion-Uk. 2009;24(5):297–305. doi: 10.1177/0267659109354656. [DOI] [PubMed] [Google Scholar]
- 24.Larsen SH, Pedersen J, Jacobsen J, Johnsen SP, Hansen OK, Hjortdal V. The RACHS-1 risk categories reflect mortality and length of stay in a Danish population of children operated for congenital heart disease. Eur J Cardio-Thorac. 2005;28(6):877–881. doi: 10.1016/j.ejcts.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 25.Cuypers JAAE, Eindhoven JA, Slager MA, Opic P, Utens EMWJ, Helbing WA, Witsenburg M, van den Bosch AE, Ouhlous M, van Domburg RT, et al. The natural and unnatural history of the Mustard procedure: long-term outcome up to 40 years. Eur Heart J. 2014;35(25):1666. doi: 10.1093/eurheartj/ehu102. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Figure S1. The vioplot of duration of ICU stay among 329 patients. Black box shows the interquartile range, solid white point shows the median of NT-proBNP levels, and black lines extend out from the box are up and down whiskers lines. The external shape with pink color is the kernel density estimation, which presents the population distribution among ICU stay time. Figure S2. The dash line showed CPB duration strongly correlated with AACC time. Cardiopulmonary bypass (CPB) duration strongly correlated with Aortic cross-clamping (ACC) time. Dash line is the regression between CPB duration and ACC time. Correlation coefficient is 0.84 and p value is less than 0.001.
Data Availability Statement
Not applicable.


