Abstract
Background:
In anterior cruciate ligament (ACL) reconstruction, hamstring tendon autografts <8 mm have been associated with increased failure rates. There has been no established modality by which orthopaedic surgeons can preoperatively predict graft sizes.
Purpose/Hypothesis:
The purposes of this study were to (1) determine whether routine magnetic resonance imaging (MRI) measurement of hamstring tendon cross-sectional area (CSA) can reliably be used by sports medicine fellowship–trained orthopaedic surgeons to predict graft size and (2) determine whether radiologists and sports medicine surgeons are able to discriminate grafts below a predetermined cutoff value. We hypothesized that radiologists will find a correlation between MRI measurement and intraoperative graft size. Similarly, orthopaedic surgeons will be able to correctly estimate the graft size based on MRI measurement.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
Included in this study were 30 consecutive patients (15 women and 15 men) (mean age, 23 years [range, 13-43 years]) for whom MRI-determined hamstring tendon CSA and graft size measurements could be compared. Patients were included if they had a preoperative MRI demonstrating acute ACL rupture and were scheduled with 1 of 3 surgeons for a reconstruction performed using the ST and GR tendons. Operative data were collected over 1 year. Sectra imaging software was used to measure the CSA of the semitendinosus (ST) and gracilis (GR) tendons on the preoperative MRIs. Control measurements were performed intraoperatively using a graft sizing block with 0.5-mm increments. Simple linear regression analysis was used to evaluate the ability of MRI measurements to predict autograft size. Logistic regression was used to determine the minimum CSA for a graft of 8 mm. The intraclass correlation coefficient (ICC) was used to evaluate interrater reliability.
Results:
MRI CSA measurement of the average STGR (ST CSA added to the GR CSA) was a significant predictor of graft size (adjusted R 2 = 0.186; P < .001). The 3 measurements with the strongest correlations with graft size were the ST at the medial femoral condyle (MFC), the STGR at the MFC, and the average STGR. The minimum CSA for the average STGR on MRI to achieve a graft size of 8 mm was 17.168 mm2 (P < .001). The area under the receiver operating characteristic curve was 0.765. The overall ICC was 0.977.
Conclusion:
Routine preoperative MRI can be used by both radiologists and orthopaedic surgeons to predict the expected ACL autograft size and identify those below a cutoff of 8 mm. This will help in preoperative planning and graft selection.
Keywords: knee, anterior cruciate ligament, ACL, radiology, magnetic resonance imaging, MRI
The anterior cruciate ligament (ACL) is one of the most commonly injured ligaments of the knee.17 Although it has often been reported that ACL reconstructions have success rates of 90% to 95%, recent studies16,18 have shown that there may be higher rates of graft failure and lower rates of return to activity than this figure suggests. Cutoffs for minimum hamstring tendon autograft diameter were previously placed at 7 mm,2 but newer literature5,16,18 supports a 6.8 times greater relative risk of graft failure for grafts below 8 mm.
Although hamstring tendon autografts have several benefits, there is considerable variability of hamstring tendon size in the population. To date, there has been no prospective analysis comparing sports medicine–trained orthopaedic surgeons with radiologists in using routine magnetic resonance imaging (MRI) to predict graft size. On the basis of the results of Hollnagel et al’s11 study, we determined the ability of MRI to predict autografts of sufficient size in hamstring tendon ACL reconstructions. We hypothesized that radiologists will find a correlation between MRI measurement and intraoperative graft size. Similarly, we hypothesized that orthopaedic surgeons will be able to correctly estimate the graft size based on MRI measurement.
Methods
Data Collection
This was a test validation study of 30 consecutive patients, all of whom were operated on by 1 of the 3 surgeons included in this study (C.J., B.J., T.K.). Data were originally collected for 32 patients, however 2 patients were excluded because of anatomic abnormalities precluding measurement of both tendons on MRI. The average patient age was 23 years (range, 13-43 years); 15 patients were women and 15 were men. Data were prospectively collected on 4-strand hamstring tendon ACL reconstructions performed in 1 regional hospital system. At this institution, all patients who undergo ACL reconstruction have a diagnostic MRI preoperatively. Patients were enrolled if they had a preoperative MRI performed on one of the system-based scanners that demonstrated ACL rupture and were scheduled for a 4-strand hamstring tendon reconstruction using the semitendinosus (ST) and gracilis (GR) tendons. Patients were excluded if they had multiligamentous injuries, previous ACL reconstructions, or acute or previous injuries affecting the ST or GR tendons.2,22,11 Institutional review board approval was obtained through the institution to access patient records through the electronic medical record.
Preoperative Measurement Instrumentation
A musculoskeletal radiologist (K.W.), along with the 3 orthopaedic surgeons (C.J., B.J., T.M.), preoperatively reviewed the MRI images for all patients in the study and recorded their measurements of cross-sectional area (CSA) before surgery. Predictive values of graft size were not determined preoperatively, allowing each of the reviewers (K.W., C.J., B.J., T.K.) to be blinded to the expectations of the intraoperative graft diameter.
Standard MRIs as ordered for evaluation of acute knee pathology were used. Both 1.5-T and 3.0-T MRIs were used. The typical parameters for the turbo spin echo T2 fat-suppressed axial images utilized in the study were as follows: repetition time = 3600; echo time = 50; field of view = 100 mm; matrix = 384 × 288; and slice thickness = 3 mm. Images were acquired with a dedicated multichannel knee coil designed for that specific MRI unit except when the patient's size or condition would not allow the placement of the knee coil. No modifications were made to enhance coil alignment for visualization of the hamstring tendons. Although the routine protocol entails coronal, sagittal oblique, and axial planes of view, only the axial plane was used in the analysis, as this provided the best view of the CSAs of the tendons.
An instructional document outlining the measurement protocol and technique was produced for all the reviewers to use, so that the measurement process would be standardized. This was done to help generalize the data to clinical situations where surgeons would perform measurements only relying on an instructional document for education and utilization purposes.
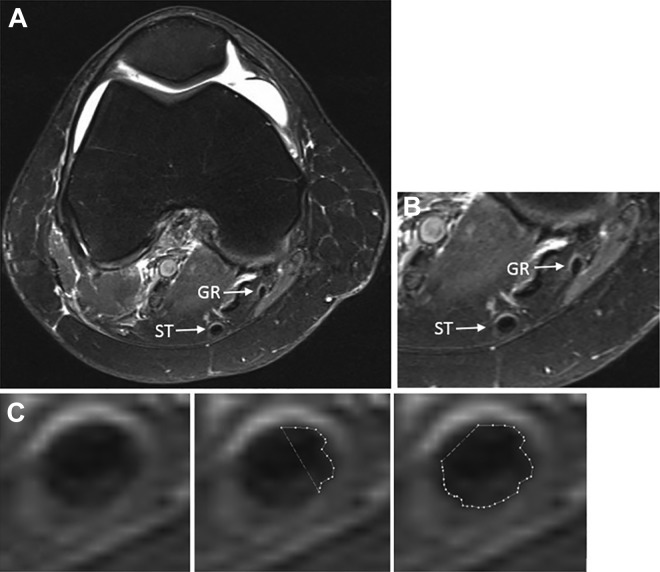
Bickel et al2 described the use of the region-of-interest tool in a picture archiving and communication system (PACS) workstation to predict graft size. The tool is used by manually tracing an area, which the software uses to calculate the CSA in mm2. Hollnagel et al11 used measurements at the widest point of the medial femoral condyle (MFC) and at the level of the joint line (JL) (Figure 1) for the ST tendon alone, the GR tendon alone, and the 2 tendons together (STGR). Accordingly, the CSA of each tendon was measured at the maximum magnification at which individual voxels were visible, but the entire tendon was still appreciable for measurement. Hollnagel et al showed this to be applicable to both 1.5-T and 3.0-T MRI.
Figure 1.
(A) Axial view of the right knee at the widest point of the medial femoral condyle. (B) Magnified view at the same level showing the semitendinosus (ST) and gracilis (GR) tendons. (C) Demonstration of the use of the region-of-interest tool to trace the cross-sectional area of the ST tendon.
Intraoperative Measurement Instrumentation
All grafts were harvested using the same operative technique and graft harvesting device by each of the 3 operating surgeons. The control intraoperative measurement was performed using a graft sizing block. The bundled ST and GR tendons were whipstitched together (Figure 2) and measured by sliding them through individually sized tunnels of 0.5-mm increments in the graft sizing block (Figure 3).9 The standard intraoperative measurement device was modified with a cap to prevent extrusion of the graft and inaccurate measurements. The diameter of the graft was determined by the smallest hole through which the graft could pass. Intraoperative measurements of graft size for the study patients were retrieved from the electronic health records of the institution where the study was conducted.
Figure 2.

Intraoperative photograph of the harvested semitendinosus and gracilis tendons folded over and whipstitched together to form a 4-bundle autograft.
Figure 3.

After the graft was formed, each was measured using a graft sizing block with 0.5-mm increments. The sizing block was modified to include a cap that prevented extrusion of the graft. Each graft was considered to fit the smallest hole through which the widest point of the graft could pass.
Statistical Analysis
Statistical analysis was performed using RStudio and JMP. Statistical significance was set at P < .05. Statistical analysis was performed for all reviewers and at all levels. Unless otherwise specified, analyses were performed using the STGR averaged across the MFC and JL (STGR AVG). Plotly graphing software (Plotly) was used to produce graphs of a simple linear regression (SLR). An SLR was used to determine the strength of the linear relationship between MRI tendon CSA and intraoperative graft diameter. Simple logistic regression was used to evaluate the minimum CSA to yield a graft of 8 mm. Predictor variables in the regression analysis were the preoperative MRI measurements. Those measurements that fell below the CSA thresholds were deemed positive values. Receiver operating characteristic (ROC) curves were generated based on the logistic regression output to evaluate the utility of the test to discriminate grafts above this threshold. For interrater reliability, the intraclass correlation coefficient (ICC) was used. A standard scale provided by Landis and Koch13 to evaluate interrater agreement was used, in which ICC < 0 indicated poor; 0-0.20, slight; 0.21-0.40, fair; 0.41-0.60, moderate; 0.61-0.80, substantial; and 0.81-1.00, almost perfect agreement. The Pearson correlation coefficients were also calculated between the MRI measurements of each reviewer. Because the Pearson correlation coefficients do not evaluate agreement, the ICC was used.12 Based on a power analysis for correlation performed before data collection, a sample size of 29 patients was required to reach a power of 80%.
Results
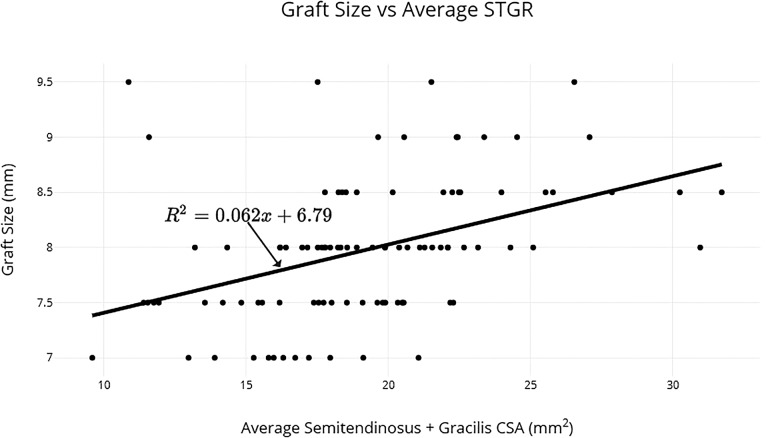
The SLR analysis showed that MRI measurement of STGR was a significant predictor of intraoperative ACL graft size (Figure 4). The equation for this model is
Figure 4.
Scatter plot displaying the relationship between semitendinosus + gracilis (STGR) cross-sectional area (CSA), averaged between the medial femoral condyle and the joint line. A regression line is plotted over the data.
where P < .001 and adjusted R 2 = 0.186.
This model takes into account the measurements by all reviewers as a whole. The strength of the relationship is moderate (R 2 < 0.20),8 because approximately 18.6% of the variance in graft diameter can be explained by the average STGR CSA. For all reviewers, r values for significant correlations ranged from 0.271 to 0.693 (Table 1). The individual measurements that were found to have the strongest correlations with graft diameter were the ST at the MFC and the GR at the MFC. The STGR at the MFC had the strongest correlation (r = 0.492) and was actually stronger than the average STGR (r = 0.439) because of the weak correlation found at the JL (r = 0.347).
Table 1.
Correlation Coefficients (r) Between Stated MRI Measurements and Intraoperative Graft Sizea
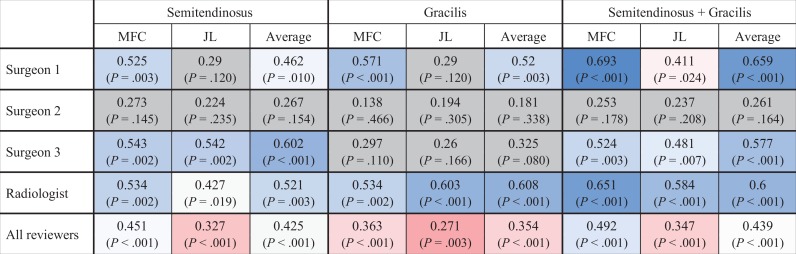
|
aHigher r values are in blue, intermediate in white, and lower values in red. Gray shading indicates nonsignificance (P > .05). JL, joint line; MFC, medial femoral condyle.
The simple logistic regression analysis showed that the minimum CSA for the average STGR on MRI to achieve a graft size of 8 mm was 17.168 mm2 based on all reviewers' measurements (Table 2). Based on the scale provided by Landis and Koch,13 the overall agreement of the surgeons with the radiologist was rated as almost perfect (Table 3). Surgeons 1 and 2 also had almost perfect agreement with the radiologist, but the agreement of surgeon 3 was rated as slight.13
Table 2.
Minimum Magnetic Resonance Imaging CSA to Achieve an 8-mm Grafta
| Minimum CSA (mm2) for 8 mm | P | |
|---|---|---|
| ST at MFC | 10.429 | 9.54e-05 |
| ST at JL | 9.694 | .000899 |
| GR at MFC | 5.698 | .000148 |
| GR at JL | 5.460 | .00159 |
| STGR at MFC | 17.016 | 1.31e-05 |
| STGR at JL | 16.124 | .000237 |
| STGR AVG | 17.168 | 2.43e-05 |
aData presented for all reviewers. CSA, cross-sectional area; GR, gracilis; JL, joint line; MFC; medial femoral condyle; ST, semitendinosus; STGR, semitendinosus + gracilis.
Table 3.
ICCs Calculated Between the Radiologist’s and the Surgeons’ Measurements of the Average Semitendinosus CSA added to the Gracilis CSAa
| ICC | Lower CI | Upper CI | |
|---|---|---|---|
| Surgeon 1 | 0.978 | 0.917 | 1.039 |
| Surgeon 2 | 0.828 | 0.35 | 1.311 |
| Surgeon 3 | 0.285 | –1.684 | 2.254 |
| Overall | 0.977 | 0.914 | 1.041 |
aCSA, cross-sectional area; ICC, intraclass correlation coefficient.
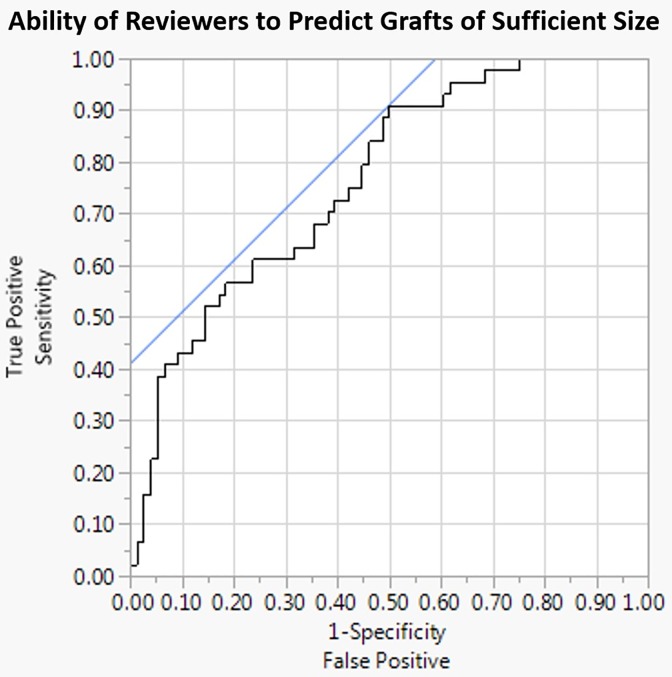
The logistic regression model was used to generate ROC curves for each of the measurements with the strongest correlations with graft size (Figure 5 and Table 4). The areas under the curve (AUC) for the ST at the MFC, the STGR at the MFC, and the average STGR were 0.738, 0.772, and 0.765, respectively.
Figure 5.
Receiver operating characteristic curve for all reviewers based on the minimum magnetic resonance imaging cross-sectional area (CSA) of the average semitendinosus CSA + gracilis CSA (STGR) to achieve an 8-mm autograft. This curve displays the ability of the average STGR to discriminate values above and below the 8-mm cutoff point. A blue line is drawn at 45° tangent to the curve to display the point that maximizes sensitivity and specificity.10 The point at which this line intersects with the curve corresponds to a CSA of approximately 21.1 mm2.
Table 4.
Area Under the Receiver Operating Curve for Each Reviewer
| Area Under the Curve | SEa | Asymptotic Significanceb | Asymptotic 95% CI | ||
|---|---|---|---|---|---|
| Reviewer | Lower Bound | Upper Bound | |||
| Surgeon 1 | 0.842 | 0.072 | .002 | 0.7 | 0.984 |
| Surgeon 2 | 0.722 | 0.108 | .045 | 0.511 | 0.934 |
| Surgeon 3 | 0.823 | 0.077 | .004 | 0.672 | 0.974 |
| Radiologist | 0.856 | 0.07 | .001 | 0.72 | 0.993 |
aUnder the nonparametric assumption.
bNull hypothesis: true area = 0.5.
Discussion
Background and Rationale
When presented intraoperatively with a hamstring tendon graft of insufficient size, physicians must choose to use the graft as harvested, or to use the ipsilateral patellar tendon, or to harvest additional tendons from the contralateral leg, or to use allograft material. Reliable graft size prediction would allow physicians to preoperatively select a graft and to improve informed consent by more accurately discussing possible choices with patients.1,2,22 Several methods have been proposed to predict hamstring tendon autograft size preoperatively. Anthropometric parameters have been used, but none has been consistently correlated with intraoperative graft size.3,14,15,19,20,21 MRI determination of autograft size, on the other hand, may provide accurate, reliable predictive ability. Chan et al4 compared MRI measurement with anthropometric measurements in prediction of intraoperative graft size and found much stronger correlations for MRI measurement (r = 0.98) compared with anthropometric parameters (r < 0.5). Nevertheless, they only reported correlation values for the ST and GR in combination with the bone–patellar tendon–bone, and hence a correlation for the hamstring tendons alone was not available for comparison. Galanis et al7 similarly found a stronger predictive ability of MRI to determine intraoperative autograft size compared with ultrasound for single- and double-bundle autografts.
Previous studies have provided good evidence of the probable correlation between MRI CSA of ST and GR and intraoperative graft diameter. Using routine internal derangement MRI, Hollnagel et al11 was able to predict intraoperative autograft size. That study also found that there were strong correlations (r = 0.63 for the average ST and GR tendons), even with MRIs that had different magnetic field strengths (1.5 T and 3.0 T).
While the availability of musculoskeletal fellowship–trained radiologists has become more common, they are not available to all orthopaedic providers. Even if radiologist determination of potential graft size is available, surgeons may feel more comfortable with independent, personal confirmation of graft size, especially when used for informed consent discussions. It is therefore important to evaluate whether radiologists and orthopaedic surgeons can independently use MRI to identify autografts of insufficient size.
Overall, the results of this study showed that MRI measurement of the ST and GR tendons is a useful approach to predict sufficient ACL graft size. This SLR function can be used to predict graft size above or below an established 8-mm cutoff for intraoperative graft sizes. For all reviewers, the values of STGR at the MFC, the JL, and on average were 17.016 mm2, 16.124 mm2, and 17.168 mm2, respectively. Of all the measurements, the STGR at the MFC provided the most consistent and strongest prediction of the intraoperative autograft diameter (r = 0.492; P < .001), as well as the largest AUC value (0.772). Measurement at the MFC produced stronger correlation values 75% of the time compared with those done at the JL. This could have been because of the splaying of the tendons, especially the GR, as they approach their insertion points in the joint. The ST provided the best correlation values for all reviewers, but this trend was not apparent for each individual.
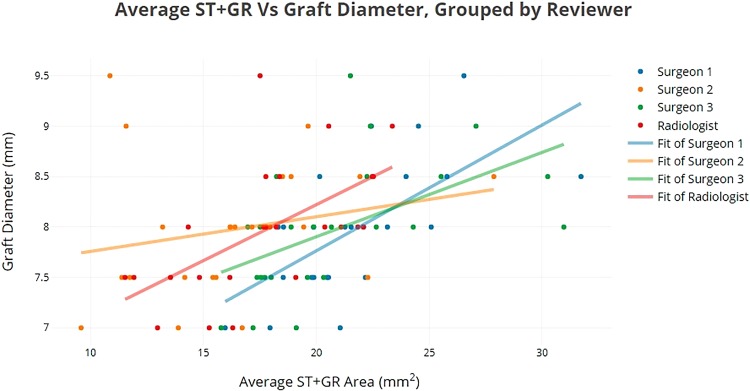
The radiologist showed consistent statistically significant correlations in his measurements, and some of the surgeons found stronger correlations for specific measurements. There was a learning period in which the measurements taken by the surgeons became more similar to those taken by the radiologist. Nevertheless, some early measurements decreased the overall correlations found by some of the surgeons (Table 1), especially surgeon 2. Even with this variation, all reviewers demonstrated an ability to discern a correlation between MRI measurement of the ST and GR and graft size (Table 5 and Figure 6). In addition, all were able to discriminate MRI hamstring tendon CSA that would translate to a graft below 8 mm in diameter.
Table 5.
Values of Variables for the Model Equation (Figure 6) Specified for Each Reviewer
| β0 | β1 | P | R 2 | |
|---|---|---|---|---|
| Surgeon 1 | 5.16 | 0.13 | <.001 | 0.415 |
| Surgeon 2 | 7.33 | 0.04 | .164 | 0.347 |
| Surgeon 3 | 6.21 | 0.08 | <.001 | 0.309 |
| Radiologist | 5.88 | 0.12 | <.001 | 0.337 |
Figure 6.
Scatter plot of average semitendinosus (ST) cross-sectional area (CSA) + gracilis (GR) CSA, with individual regression lines. The equations of the lines follow the model equation explained in the text and have the values specified in Table 5.
The AUC curve was 0.765 for all reviewers. The ROC curve displays the range of sensitivity and specificity values at different decision thresholds. Since it is more important to detect those below an 8-mm cutoff, sensitivity is preferred over specificity. The point at which the line displayed in Figure 5 intersects with the curve displays such a scenario, in which sensitivity is 91% and specificity is 50%, corresponding to an average STGR measurement of 21.1 mm2. The value for the minimum CSA of the average STGR (17.168 mm2) from this study is smaller than the radiologist’s cutoffs from the Hollnagel et al11 study (20.55 mm2 for the 1.5 T group and 20.86 mm2 for the 3 T group), but the value that maximizes sensitivity (21.1 mm2) is consistent with that of Hollnagel et al. Erquicia et al6 found an STGR cutoff of 25.5 mm2, while Leiter et al14 found the same value to be 14.5 mm2. Recently, Grawe et al9 found a value of 21.64 mm2 to be sufficient for an 8-mm graft. This shows that the data from the current study are generally in line with previously published work, although there is variability between these studies. It could be because of differences in cutoff calculation methods and individual and institutional MRI protocol differences, as well as differences in sample size and sex ratios.
Limitations
There are several limitations to this study. Recruitment limited the sample size. Although there was a large potential pool of patients, insurance restrictions precluded many patients from using the MRI machines in the study institution’s facilities. Three patients were also lost to follow-up between scheduling and the reconstruction. Two patients were excluded because of abnormalities from anatomic variation or MRI recording. Nevertheless, this study has several advantages. It required no change in imaging protocols, no additional intervention to each patient’s treatment plan, and no additional cost. It also provided evidence that surgeon-based measurements could be performed that could identify hamstring tendons of potentially insufficient size before ACL reconstruction.
Conclusion
This study showed that routine MRI measurements of hamstring tendon CSA are predictive of intraoperative ACL graft sizes, allowing improved preoperative planning and graft selection options for ACL reconstruction. The radiologist and surgeons were all able to discriminate grafts of insufficient size with high sensitivity, although there were some variations between the reviewers. Further studies are necessary to study the differences in measurement technique that could cause such variation and to provide more information on intrarater reliability.
Acknowledgment
The authors acknowledge Allison Tegge, PhD, Fralin Biomedical Research Institute at Virginia Tech Carilion, for statistical support and instruction.
Footnotes
One or more of the authors declared the following potential conflict of interest or source of funding: K.H. has received educational support from CDC Medical. C.J. has received educational support from Arthrex and consulting fees from DePuy/Mitek. B.J. has stock in Baxter, Bristol-Myers-Squibb, Eli Lilly, Pfizer, and Zimmer. J.G. has received grants from Arthrex and DJO and educational support from Arhrex, Smith & Nephew, and Orthopedic Systems. T.M. has received consulting fees from DePuy/Mitek. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Carilion Institutional Review Board.
References
- 1. Beyzadeoglu T, Akgun U, Tasdelen N, Karahan M. Prediction of semitendinosus and gracilis autograft sizes for ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1293–1297. [DOI] [PubMed] [Google Scholar]
- 2. Bickel BA, Fowler TT, Mowbray JG, Adler B, Klingele K, Phillips G. Preoperative magnetic resonance imaging cross-sectional area for the measurement of hamstring autograft diameter for reconstruction of the adolescent anterior cruciate ligament. Arthroscopy. 2008;24(12):1336–1341. [DOI] [PubMed] [Google Scholar]
- 3. Çeliktaş M, Gölpinar A, Köse Ö, Sütoluk Z, Çelebi K, Sarpel Y. Prediction of the quadruple hamstring autograft thickness in ACL reconstruction using anthropometric measures. Acta Orthop Traumatol Turc. 2013;47(1):14–18. [DOI] [PubMed] [Google Scholar]
- 4. Chan KW, Kaplan K, Ong CC, Schweitzer ME, Sherman OH. Using magnetic resonance imaging to determine preoperative autograft sizes in anterior cruciate ligament reconstruction. Bull NYU Hosp Jt Dis. 2012;70(4):241. [PubMed] [Google Scholar]
- 5. Conte EJ, Hyatt AE, Gatt CJ, Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30(7):882–890. [DOI] [PubMed] [Google Scholar]
- 6. Erquicia JI, Gelber PE, Doreste JL, Pelfort X, Abat F, Monllau JC. How to improve the prediction of quadrupled semitendinosus and gracilis autograft sizes with magnetic resonance imaging and ultrasonography. Am J Sports Med. 2013;41(8):1857–1863. [DOI] [PubMed] [Google Scholar]
- 7. Galanis N, Savvidis M, Tsifountoudis I, et al. Correlation between semitendinosus and gracilis tendon cross-sectional area determined using ultrasound, magnetic resonance imaging and intraoperative tendon measurements. J Electromyogr Kinesiol. 2016;26:44–51. [DOI] [PubMed] [Google Scholar]
- 8. Goyal S, Matias N, Pandey V, Acharya K. Are pre-operative anthropometric parameters helpful in predicting length and thickness of quadrupled hamstring graft for ACL reconstruction in adults? A prospective study and literature review. Int Orthop. 2016;40(1):173–181. [DOI] [PubMed] [Google Scholar]
- 9. Grawe BM, Williams PN, Burge A, et al. Anterior cruciate ligament reconstruction with autologous hamstring: can preoperative magnetic resonance imaging accurately predict graft diameter? Orthop J Sports Med. 2016;4(5):2325967116646360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med. 2013;4(2):627–635. [PMC free article] [PubMed] [Google Scholar]
- 11. Hollnagel KF, Johnson BM, Whitmer KK, Hanna AO, Miller TK. Prediction of autograft hamstring size for anterior cruciate ligament reconstruction using MRI. Clin Orthop Relat Res. 2019;477(12):2677–2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jinyuan LI, Wan TA, Guanqin CH, Yin LU, Changyong FE. Correlation and agreement: overview and clarification of competing concepts and measures. Shanghai Arch Psychiatry. 2016;28(2):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159. [PubMed] [Google Scholar]
- 14. Leiter J, Elkurbo M, McRae S, Chiu J, Froese W, MacDonald P. Using pre-operative MRI to predict intraoperative hamstring graft size for anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;25(1):229–235. [DOI] [PubMed] [Google Scholar]
- 15. Ma CB, Keifa E, Dunn W, Fu FH, Harner CD. Can pre-operative measures predict quadruple hamstring graft diameter? Knee. 2010;17(1):81–83. [DOI] [PubMed] [Google Scholar]
- 16. Magnussen RA, Lawrence JTR, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. [DOI] [PubMed] [Google Scholar]
- 17. Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13(3):184–188. [DOI] [PubMed] [Google Scholar]
- 18. Mariscalco MW, Flanigan DC, Mitchell J, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy. 2013;29(12):1948–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Park SY, Oh H, Park S, Lee JH, Lee SH, Yoon KH. Factors predicting hamstring tendon autograft diameters and resulting failure rates after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1111–1118. [DOI] [PubMed] [Google Scholar]
- 20. Pinheiro LFB, de Andrade MAP, Teixeira LEM, et al. Intra-operative four-stranded hamstring tendon graft diameter evaluation. Knee Surg Sports Traumatol Arthrosc. 2011;19(5):811–815. [DOI] [PubMed] [Google Scholar]
- 21. Reboonlap N, Nakornchai C, Charakorn K. Correlation between the length of gracilis and semitendinosus tendon and physical parameters in Thai males. J Med Assoc Thai. 2012; 95(suppl 10):S142–S146. [PubMed] [Google Scholar]
- 22. Wernecke G, Harris IA, Houang MTW, Seeto BG, Chen DB, MacDessi SJ. Using magnetic resonance imaging to predict adequate graft diameters for autologous hamstring double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(8):1055–1059. [DOI] [PubMed] [Google Scholar]