Abstract
Objective:
Anorexia nervosa (AN) and obsessive-compulsive disorder (OCD) are highly comorbid. However, the factors that account for this comorbidity are poorly understood. We examined the core dimensions of AN and OCD and psychological and personality factors shared by both disorders.
Method:
In path analyses (N=732 women with either current AN or recovered from AN), we examined which factors were uniquely and independently associated with the core dimensions of AN and OCD. We also examined recovery from AN as a moderator.
Results:
When individuals with AN reported greater concern over mistakes, they endorsed more severity in both AN and OCD core dimensions. These unique associations existed above and beyond all other transdiagnostic personality and psychological factors and regardless of AN recovery status.
Conclusions:
Concern over mistakes partially accounts for severity in the core dimensions of both AN and OCD. Concern over mistakes may represent an important target in the etiology of AN and OCD.
Keywords: anorexia nervosa, obsessive-compulsive disorder, perfectionism, comorbidity, transdiagnostic, concern over mistakes
Anorexia nervosa (AN) and obsessive-compulsive disorder (OCD) are highly comorbid; OCD is found in 35–44% of patients with AN, and AN is found in 10% of female patients with OCD, a higher prevalence than population-based estimates for either disorder (LaSalle et al., 2004; Pinto, Mancebo, Eisen, Pagaon, & Rasmussen, 2006). Moreover, AN-OCD comorbidity is associated with both younger age of onset and poorer prognosis in patients with AN (Crane, Roberts, & Treasure, 2007; Simpson et al., 2013). Childhood OCD symptoms and obsessive-compulsive personality traits are often cited as risk factors for later AN (Anderluh, Tchanturia, & Rabe-Hesketh, 2003; Micali et al., 2011). Epidemiological evidence has long suggested a shared etiology between AN and OCD (Anttila et al., 2014; Micali et al., 2011; Steinhausen, Jakobsen, Helenius, Munk-Jorgensen, & Strober, 2015). Recent preliminary molecular genetic analyses using published AN and OCD genome-wide-association-study data and twin studies have also found that these disorders are positively correlated genetically (~55%; Anttila et al., 2014; Cederlöf et al., 2015; Mas et al., 2013). Such research suggests that AN and OCD may represent variations on a common phenotype with shared brain-behavioral etiological pathways (Steinglass & Walsh, 2006; Suda et al., 2014).
However, there has been little research exploring possible transdiagnostic factors (i.e., factors that lead to multiple disorders; Nolen-Hoeksema & Watkins, 2011) that confer risk to both AN and OCD. Identifying transdiagnostic factors assists in understanding the symptom heterogeneity and individual differences within both AN and OCD and ultimately can point towards treatments tailored to patients’ unique symptom patterns. In reviews of the neuroscience literature, the primary transdiagnostic focus has been on the associations between AN symptoms and compulsions in OCD. Both increased compulsivity—traits marked by inappropriate behavior that persists despite not assisting in achieving a goal and in undesirable consequences—and dysfunction in habit learning—behaviors that persist without a clear association with the outcome—have been proposed as potential transdiagnostic constructs that could explain AN and OCD commonalities (Godier & Park, 2015; Steinglass & Walsh, 2006).
Transdiagnostic Personality and Psychological Factors.
It is also possible that other transdiagnostic personality and psychological factors could help explain the relation between AN and OCD. The following personality factors: Neuroticism (i.e., a disposition toward negative emotionality in relation to uncertain or adverse events), conscientiousness (i.e., characterized by orderliness, disciplined nature, and exactness events), harm avoidance (i.e., a trait characterized by anxiety, behavioral inhibition, and inflexibility), and concern over mistakes (i.e., engaging in excessive worry over perceived errors) have all been found to be elevated in individuals with AN and OCD compared with healthy controls (Benatti, Dell’Osso, Arici, Hollander, & Altamura, 2014; Ettelt et al., 2008; Fassino et al., 2002; Klump et al., 2000). Although perfectionism in general has been found to be a risk factor for both AN and OCD (Altman & Shankman, 2009; Bulik et al., 2003), concern over mistakes, is most strongly associated with a diagnosis of AN (Bardone-Cone et al., 2007; Bulik et al., 2003) and is elevated in OCD compared with healthy controls (Lee et al., 2009; Suzuki, 2005). The following psychological factors were also relevant to both AN and OCD: impulsivity (i.e., the tendency to engage in rash action) and trait anxiety (a predisposition toward feelings of anxiety) (Altman & Shankman, 2009; Rosval et al., 2006) because both have been found to be elevated in patients with AN and OCD compared with healthy controls (Benatti et al., 2014; Ettelt et al., 2008; Sysko, Walsh, Schebendach, & Wilson, 2005; Wildes, Ringham, & Marcus, 2010). Though these factors have each been tested separately with OCD and AN, we are aware of no research examining a comprehensive model of AN-OCD comorbidity including all of these personality and psychological factors.
A Dimensional Approach.
Further, recent research has supported the importance of examining the overlap between these disorders through a dimensional approach (Altman & Shankman, 2009; Roncero et al., 2011). Focusing on specific dimensions, rather than diagnostic-level associations, allows for a clearer understanding of potential etiological pathways and may aid in more targeted treatment (e.g., Brown & Barlow, 2005). No research, to our knowledge, has examined the associations between the core dimensions of AN with core dimensions of OCD (obsessions and compulsions). Though there are several dimensions of AN that could be tested, the core dimensions of AN involve a preoccupation with and desire to lose weight (i.e., drive for thinness) that results in significantly low body weight and a disturbance in the way one’s body and shape is perceived (i.e., body dissatisfaction) (American Psychiatric Association, 2013; Garner et al., 1983). OCD is characterized by the experience of obsessions (i.e., recurrent and persistent thoughts or images that are intrusive), and/or compulsions (i.e., recurrent and persistent impulses to engage in an action) that are excessive and distressing. Therefore, the current analyses focused on the OCD dimensions of obsessions and compulsions and AN dimensions of drive for thinness and body dissatisfaction.
Aims and Hypotheses
The primary aim of the present study was to examine whether individual differences in the core dimensions of AN (drive for thinness and body dissatisfaction) and OCD (obsessions and compulsions) are associated using a large sample of women with AN. Our second aim was to investigate whether transdiagnostic personality and psychological factors shared in common by the two disorders could account for the associations between the core dimensions of AN and OCD in women with AN. This study will aid in hypothesis generation for future prospective studies.
We had two primary hypotheses. First, given that the theorized core transdiagnostic factors for AN and OCD is shared compulsivity and habit learning, we anticipated that associations between individual differences in the core dimensions of AN would be uniquely associated with compulsions, but not obsessions (Godier & Park, 2015; Steinglass & Walsh, 2006). Second, we expected that these proposed transdiagnostic personality and psychological factors—neuroticism, harm avoidance, conscientiousness, concern over mistakes, impulsivity, and anxiety—would be uniquely and independently (i.e., above and beyond zero-order correlations) associated with all three outcomes: drive for thinness, body dissatisfaction, and compulsivity (but not obsessions), given that they have independently been shown to be related to each of these outcomes in a non-combined model (e.g., Benatti, Dell’Osso, Arici, Hollander, & Altamura, 2014; Ettelt et al., 2008; Fassino et al., 2002; Klump et al., 2000) . We also predicted that these relationships would remain regardless of recovery from AN, suggesting that these associations are not simply state-dependent and present only when participants were symptomatic.
Method
Participants
Data were collected as part of the International Price Foundation Genetic Study of AN Trios, designed to identify genetic susceptibility loci of risk for eating disorders. A complete description of recruitment and data collection has been published previously (Reba et al., 2005). In brief, participants were recruited from nine sites in North America and Europe, including Pittsburgh (W.K.), New York (K.H.), Los Angeles (M.S.), Toronto (A.K., B.W.), Munich (M.F.), Pisa (A.R.), Fargo (J.M.), Baltimore (H.B., S.C.), and Tulsa (C.J.), between 2000 and 2003. Potential participants were identified through clinic databases, referral from clinicians with knowledge of the study, and advertisement through a variety of local and national media. The study was approved by local institutional review boards at all sites. Written informed consent was obtained before participation.
Participants were required to meet the following criteria: a) DSM-IV (American Psychiatric Association, 2000) lifetime diagnosis of AN, excluding the amenorrhea criterion; b) low weight less than 5th percentile of body mass index (BMI) for age and gender on the Hebebrand and colleagues (1996) chart from the National Health and Nutrition Examination Survey epidemiological sample; c) AN onset before age 25; d) weight controlled through restricting and/or purging, including vomiting, abuse of laxatives, diuretics, enemas, suppositories, or ipecac; e) age between 13 and 65; and f) the diagnosis of AN must have been met at least 3 years before study entry. The last criterion ensured that participants were unlikely to develop binge eating in the future because binge eating typically develops within the first three years after AN onset (Bulik et al., 1997; Tozzi et al., 2005). Because the primary aim of the study was to investigate genetic loci associated with AN, only Caucasian participants were included (participants could be included with one non-Caucasian grandparent). The final sample included 732 participants in total; thirty-five participants were excluded from this analysis due to missing data. Missing data was missing at random. In other words, there was no systematic reason for missingness. Therefore, we included only participants with full data in these analyses.
Measures
Outcome variables: Core Dimensions of AN and OCD
EDI-2.
Drive for Thinness and Body Dissatisfaction were assessed using the Eating Disorder Inventory-2 (EDI-2; Garner, 1990). The EDI-2 is a 91-item questionnaire of cognitive and behavioral eating disorder dimensions. The EDI-2 has been widely used in eating disorder (ED) research and is reported to successfully discriminate between subjects with and without EDs (Garner et al., 1983). The EDI-2 has strong convergent and discriminant validity (Garner et al., 1983). Participants reported on the severity of their eating disorder cognitions and behaviors during the time their eating concerns were the worst.
Yale-Brown Obsessive Compulsive Scale.
Obsessions and compulsions were assessed using the Yale–Brown Obsessive Compulsive Scale (YBOCS; Goodman et al., 1989). The YBOCS is a semi-structured interview designed to assess the severity of obsessive thoughts and compulsive behaviors. It has excellent inter-rater reliability (Pato et al., 1994). Participants reported on their current severity of obsessions and compulsions.
Independent variables: Transdiagnostic Personality and Psychological Factors.
Transdiagnostic Personality Factors
Neuroticism–Extraversion–Openness Personality Inventory.
Neuroticism and conscientiousness were assessed using the Neuroticism–Extraversion–Openness Personality Inventory (NEO PI-R; Costa & McCrae, 1992), a 240-item questionnaire of five major personality domains (neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness), based on the Five-Factor Model of personality. Neuroticism, which is one of the “Big Five” personality traits and is characterized by a disposition toward negative emotionality and impulsiveness in relation to uncertain or adverse events (Ormel et al., 2004), and conscientiousness, which indexes degree of organization, persistence, control and goal directed behavior, were included in the current study. Participants reported how much they agreed with a series of statements that reflect their current level of neuroticism and conscientiousness. The NEO PI-R has strong factor structure and convergent validity (Costa & McCrae, 1992).
Frost Multidimensional Perfectionism Scale.
Perfectionism/Concern over mistakes was assessed using the Frost Multidimensional Perfectionism Scale (FMPS; Frost et al., 1990), a 35-item self-report measure of perfectionism rated on a 5-point scale. Concern over mistakes indexes negative reactions to mistakes, the tendency to equate mistakes with a failure, and the belief that one will lose the respect of others because of mistakes (Bardone-Cone et al., 2007; Frost et al., 1990). Participants reported on the intensity of their perfectionism at the time when concerns about their eating were the worst. The FMPS has strong psychometric properties, including factor, construct, and convergent validity.
Temperament and Character Inventory-9.
Harm avoidance was assessed using the Temperament and Character Inventory-9 (Cloninger et al., 1993), a 240-item self-report measure of the personality traits. Temperament is hypothesized to be moderately heritable, stable throughout life, and mediated by neurotransmitter functioning. Harm avoidance assesses the tendency to inhibit behavior to avoid punishment. High harm avoidance indexes greater fear, shyness, pessimism, and worrying. Low harm avoidance indexes greater boldness, optimism, and confidence. The TCI has strong factor and convergent validity.
Transdiagnostic Psychological Factors
Spielberger State-Trait Anxiety Inventory.
Trait anxiety was assessed using the Spielberger State-Trait Anxiety Inventory (STAI Form Y-1; Spielberger et al., 1970), a self-report measure that includes a 20-item scale of current anxiety (state) and a 20-item scale of general levels of anxiety (trait). Participants rated how they ‘generally feel’ to form a trait anxiety scale. We used trait anxiety because we were interested in testing how much the individual feels anxiety in general, rather than transitory anxiety. The STAI has strong psychometric properties for measurement of both state and trait anxiety.
Barratt Impulsiveness Scale-11.
Impulsivity was assessed using the Barratt Impulsiveness Scale-11 (BIS-11; Barratt, 1965), a 30-item self-report measure of impulsiveness. The BIS includes three aspects of impulsiveness: cognitive, motor, and non-planning. The BIS had been shown to successfully discriminate the degree of impulse control in subgroups of women with eating disorders (Bulik et al., 1997) and all three subscales (cognitive impulsivity, motor impulsivity, and non-planning impulsivity) were included in analyses. Participants rated their current level of impulsivity.
Moderator variables
Recovery status.
Because no consensus on the definition of AN recovery exists (Bardone-Cone et al., 2010; Hoek, 2006), recovery was defined as occurring if the participant experienced at least one year without any eating disorder symptom (e.g., low weight, dieting, binge eating, inappropriate compensatory behaviors). To determine recovery status, all participants were interviewed about their eating disorder symptoms using the SCID module H. During the interview process, participants were asked whether they had experienced any of the symptoms on those measures in the last month. If they had no symptoms in the past month, participants were then asked how long ago the last symptom occurred. The number of months since last symptom was recorded. The sample yielded two groups, recovered (N = 134) and active ED (N = 563).
Path Analyses
All path models were tested in Mplus Version 7 (Muthén & Muthén, 1998) using the maximum likelihood estimator. We chose to use path analysis because it allows identification of unique relationships between correlated variables regardless of multicollinearity and overlapping variance (e.g., Loehin, 1998). We first conducted zero-order correlations of all AN and OCD core dimensions and the proposed transdiagnostic personality factors (neuroticism and conscientiousness, harm avoidance, concern over mistakes) and psychological factors (trait anxiety and impulsivity: cognitive, motor, and non-planning impulsivity). We then tested two path models: we examined drive for thinness and body dissatisfaction independently to a) increase power, and b) allow examination of any unique relationships with these constructs that might otherwise be obscured with the inclusion of both variables.
Our first model tested the association between the OCD core dimensions of obsessions, compulsions, and the AN core dimension of drive for thinness while examining the unique associations of transdiagnostic personality factors (neuroticism and conscientiousness, harm avoidance, concern over mistakes) and psychological factors (trait anxiety and cognitive, motor, and non-planning impulsivity) with these outcomes. Obsessions, compulsions, and drive for thinness were modeled as three simultaneous outcome measures, with paths from the eight personality and psychological factors to each of these three outcome measures. This model allowed us to test if each of the hypothesized transdiagnostic personality and psychological factors had a unique and independent (over and above the other factors) association with each of the three outcomes (obsessions, compulsions, drive for thinness).
Our second model tested the association between OCD core dimensions of obsessions, compulsions, and the AN core dimension of body dissatisfaction while examining the unique associations of the hypothesized transdiagnostic personality factors and psychological factors with these outcomes.
Model fit was evaluated using the: (a) comparative fit index (CFI; Bentler, 1990), (b) Tucker-Lewis incremental fit index (TLI; Tucker & Lewis, 1973), (c) root mean square error of approximation (RMSEA; Steiger & Lind, 1980), and (d) standardized root mean square residual (SRMR; Bentler, 1990; Joreskog & Sorbom, 1981). The magnitudes of these indices were evaluated according to recommendations by Hu and Bentler (Hu & Bentler, 1999); for the CFI and TLI, values of .90 and above were considered adequate, whereas values of 0.95 or above were considered very good; for the RMSEA and SRMR, values of 0.08 and below were considered adequate and 0.05 or less very good. We first tested these models with all possible paths included. If models were saturated (i.e., there were no remaining degrees of freedom), meaning that model fit was perfect, we ran models with non-significant paths removed to evaluate model fit.1
Finally, in order to examine the effects of recovery (defined as either recovered or active ED) on paths between the predictors and outcomes, we conducted multiple group testing in path analysis following the sequence of nested tests in path analysis recommended by Bollen (1989). We tested a model with unconstrained paths across groups (defined as either recovered or active ED) and compared this model to a model with constrained paths across groups (i.e., paths were constrained across recovered or active ED groups to have the same parameters). We then calculated the chi-square difference test to determine if variance existed across the constrained versus unconstrained model. Significant chi-square values would indicate that there is variance (moderation) across recovery status. Testing across recovered vs. active ED groups also helped account for the fact that some of our measures referred to the current time and some referred to the time when the ‘individual was most ill’. If there were no differences between recovered and active ED groups, this analysis provided additional evidence that the time of the participants’ report (current vs. most ill) did not impact these associations.
Results
Demographics and Comorbid Disorders
All participants had a diagnosis of AN. All participants were Caucasian and had an average age of 26.12 (SD = 7.81) years. Most participants were employed (61.6; n = 451), had completed some college (74.18%; n = 543) and were never married (67.36%; n = 483). A large percentage (54.36%; n = 393) had a comorbid diagnosis of OCD. Other diagnoses were generalized anxiety disorder (n = 99; 13.62%), agoraphobia (n = 21, 2.89%), major depressive disorder (n = 516, 72.27%), panic disorder (n = 99; 13.62%), post-traumatic stress disorder (n = 120, 17.12%), social phobia (n = 153, 21.22%), and specific phobia (n = 72, 9.99%).
Zero-order Correlations
Please see Table 1 for zero-order correlations. As expected, obsessions and compulsions were moderately and positively correlated with both drive for thinness and body dissatisfaction (all ps < .001). When participants reported greater obsessions and compulsions, they were also more likely to endorse greater drive for thinness and body dissatisfaction. The personality and psychological factors were all significantly and positively correlated with the core dimensions of AN and OCD.
Table 1.
Zero-order Correlations Among Obsessions, Compulsions, Drive for Thinness, Body Dissatisfaction, and Psychological and Personality Factors.
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Core Dimensions | ||||||||||||
| 1. Obsessions | --- | |||||||||||
| 2. Compulsions | 0.84** | --- | ||||||||||
| 3. Drive for thinness | 0.18** | 0.20** | --- | |||||||||
| 4. Body dissatisfaction | 0.19** | 0.21** | 0.65** | --- | ||||||||
| Personality Factors | ||||||||||||
| 5. Neuroticism | 0.25** | 0.25** | 0.24** | 0.29** | --- | |||||||
| 6. Conscientiousness | −0.02 | −0.05 | −0.01 | −0.06 | −0.43** | --- | ||||||
| 7. Concern over mistakes | 0.28** | 0.28** | 0.39** | 0.40** | 0.45** | .01 | --- | |||||
| 8. Harm avoidance | 0.24** | 0.23** | 0.23** | 0.28** | 0.68** | −.20** | 0.40** | --- | ||||
| Psychological Factors | ||||||||||||
| 9. Trait anxiety | 0.20** | 0.22** | 0.20** | 0.30** | 0.77** | −0.22** | 0.44** | 0.65** | --- | |||
| 10. Non-planning Impulsivity | 0.03 | 0.06 | −0.03 | 0.03 | 0.29** | −0.65** | −0.04 | 0.12** | 0.15** | --- | ||
| 11. Motor impulsivity | 0.03 | 0.04 | 0.03 | 0.08* | 0.21** | −0.55** | −0.02 | −0.08* | 0.03 | 0.60** | --- | |
| 12. Cognitive impulsivity | 0.17** | 0.20** | 0.15** | 0.15** | 0.55** | −0.44** | 0.20** | 0.33** | 0.51** | 0.38** | 0.38** | --- |
p < 0.05
p < 0.01
Model 1: Do Transdiagnostic Personality and Psychological Factors Explain Associations Between Obsessions, Compulsions, and Drive for Thinness?
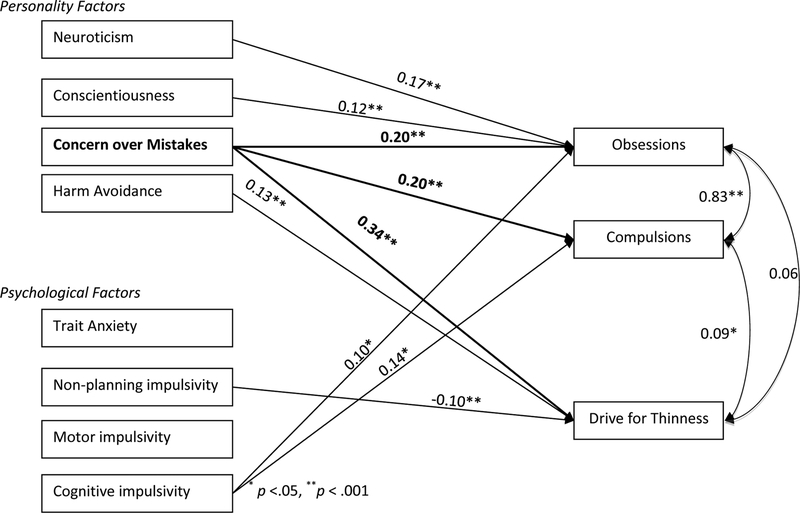
First, we tested a model including all transdiagnostic personality and psychological factors and obsessions, compulsions, and drive for thinness (Figure 1). The model was saturated and therefore, by definition, had perfect fit (CFI=1.00, TLI=1.00, RMSEA=0.00, SRMR=0.00). To determine model fit, we removed non-significant paths. This model with only significant paths had excellent fit (CFI=1.00, TLI=0.99, RMSEA=0.03; SRMR=0.02).
Figure 1.
Model of Obsessions, Compulsions, and Drive for Thinness. All paths modeled, only significant paths (βs) are included below. Bolded variables and paths denotes shared associations across OCD and AN
For obsessions, there were positive, unique (i.e., over and above the other factors) and significant paths from neuroticism (ß = 0.17, p < .001), conscientiousness (ß = 0.12, p < .001), concern over mistakes (ß = 0.20, p < .001), and cognitive impulsivity (ß = 0.10, p = .047). For compulsions, there were positive, unique (over and above all other factors), and significant paths from concern over mistakes (ß = 0.20, p < .001) and cognitive impulsivity (ß = 0.10, p = .019). For drive for thinness, there were unique and significant paths from concern over mistakes (ß = 0.34, p < .001), harm avoidance, (ß = 0.13, p < .001), and non-planning impulsivity (ß = −0.10, p = .050).
Concern over mistakes was the only variable to have significant and positive paths to all three outcomes (obsessions, compulsions, and drive for thinness) over and above all other variables. In this model, drive for thinness was significantly correlated with compulsions (r = 0.09; p = .017), but not with obsessions (r = 0.06, p > .050), suggesting there is remaining unexplained variance between compulsions and drive for thinness above and beyond the other paths in the model.
Model 2: Do Transdiagnostic Personality and Psychological Factors Explain Associations among Obsessions, Compulsions, and Body Dissatisfaction?
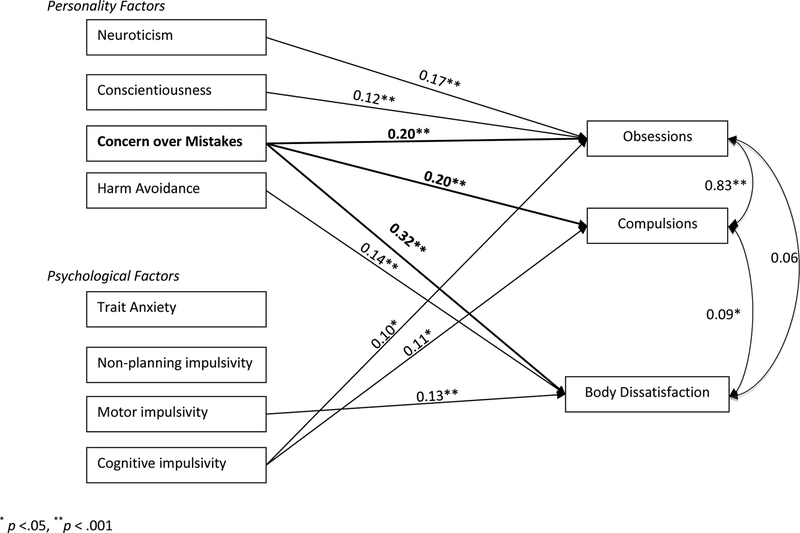
Next, we tested a model including all transdiagnostic personality and psychological factors and obsessions, compulsions, and body dissatisfaction (Figure 2). This model was saturated. To determine model fit, we removed non-significant paths. This model with only significant paths also had excellent fit (CFI=1.00, TLI=1.00, RMSEA=0.02; SRMR=0.02).
Figure 2.
Model of Obsessions, Compulsions, and Body Dissatisfaction. All paths modeled, only significant paths (βs) are included below. Bolded variables and paths denotes shared associations across OCD and AN.
For obsessions, similarly with drive for thinness, there were positive, unique and significant paths from neuroticism (ß = 0.17, p < .001), conscientiousness (ß=0.12, p < .001), concern over mistakes (ß=0.20, p < .001), and cognitive impulsivity (ß=0.10, p = .049). For compulsions, there were positive, unique and significant paths from concern over mistakes (ß=0.20, p < .001) and cognitive impulsivity (ß=0.11, p = .020). For body dissatisfaction, there were positive, unique and significant paths from concern over mistakes (ß=0.32, p < .001), harm avoidance (ß=0.14, p < .001), and motor impulsivity (ß=0.13, p = .005).
Concern over mistakes was the only variable to have significant and positive paths to all three outcomes (obsessions, compulsions, and body dissatisfaction) over and above all other variables. As with drive for thinness, body dissatisfaction was significantly correlated with compulsions (r = 0.09; p = .025), but not with obsessions (r = 0.06, p > .050), suggesting there was a unique association between compulsions and body dissatisfaction above and beyond the other paths in the model.
Multiple group analysis: Is recovery a moderator?
First, we tested the final Model 1 (obsessions, compulsions, and drive for thinness) with all non-significant paths removed (recovered n = 134 versus active ED n = 563). Chi-square analyses indicated that there was a significant difference between the constrained and unconstrained model (χ2 [15]=84.99 p < .001), suggesting that there were differences between the recovered and active ED groups. Regardless of recovery status, concern over mistakes had significant and positive paths to obsessions (ß = 0.23, p < .001 and ß = 0.253, p = .003 for active ED and recovered, respectively), compulsions (ß = 0.26, p < .001 and ß = 0.24, p = .006 for active ED and recovered, respectively), and drive for thinness (ß = 0.35, p < .001 and ß = 0.34, p < .001 for active ED and recovered, respectively). However, cognitive impulsivity had a significant and positive path to obsessions (ß = 0.16, p < .001) and compulsions (ß = 0.17, p < .001) only in individuals with active AN. Similarly, harm avoidance only had significant paths to drive for thinness in individuals with active AN (ß = 0.11, p < .001). In contrast, neuroticism had a significant path to obsessions only in individuals recovered from AN (ß = 0.17, p = .003). In individuals who had an active ED, when accounting for all of the psychological and personality factors, drive for thinness became significantly associated with obsessions (r = .09, p = .027) and compulsions (r = .15, p = .002). However, drive for thinness was no longer significantly associated with obsessions and compulsions (ps > .142) in recovered individuals.
Finally, we tested the impact of recovery on path estimates in Model 2 (obsessions, compulsions, and body dissatisfaction). Once again, in chi-square analyses, there was a significant difference between the constrained and unconstrained model (χ2 [15] = 60.19, p < .001), suggesting that there were differences between the recovered and active ED groups. Regardless of recovery, concern over mistakes had significant and positive paths to obsessions (ß = 0.17, p < .001 and ß = 0.17, p < .005 for active ED and recovered, respectively), compulsions (ß = 0.20, p < .001 and ß=0.16, p =.007 for active ED and recovered, respectively), and body dissatisfaction (ß = 0.26, p < .001 and ß = 0.36, p < .001 for active ED and recovered, respectively). Cognitive impulsivity had significant and positive paths to obsessions (ß = 0.23, p < .001) and compulsions (ß = 0.26, p < .001) only in the individuals with active AN. Similarly, harm avoidance (ß = 0.16, p < .001) and motor impulsivity (ß = 0.20, p < .001) also had significant and positive paths to body dissatisfaction only in the individuals with active AN. Neuroticism only had significant paths to obsessions in individuals recovered from AN (ß = 0.05, p < .005). In individuals with an active ED, when accounting for all of the psychological and personality factors, body dissatisfaction remained significantly associated with obsessions (r = .11, p = .017) and compulsions (r = .15, p < .001). However, body dissatisfaction was no longer significantly associated with obsessions and compulsions (ps > .158) in recovered individuals.
Discussion
We tested the associations between core dimensions of AN (body dissatisfaction and drive for thinness) and OCD (obsessions and compulsions) and transdiagnostic personality and psychological factors in women with a diagnosis of AN. We found support for our first hypothesis: the core symptoms of AN were associated with compulsions, but not obsessions when including the personality and psychological factors in the model (Godier & Park, 2015; Steinglass & Walsh, 2006). Although personality and psychological factors explained associations between obsessions and core dimensions of AN (i.e., correlations between obsessions and core dimensions of AN were non-significant once these factors were included in the model), we still found unique associations between compulsions and core dimensions of AN. As participants reported greater compulsions, their reported drive for thinness and body dissatisfaction was also greater, and/or vice versa.
Second, greater concern over mistakes was the only factor to have significant associations with the core dimensions of both AN and OCD while controlling for all other factors. When participants reported that they had greater concern over mistakes, they were more likely to also endorse more intense drive for thinness, body dissatisfaction, and obsessions and compulsions. These associations were found above and beyond all other transdiagnostic personality and psychological factors, regardless of AN recovery status. No other personality or psychological factors examined had associations with all core dimensions of AN and OCD. Within each disorder, greater cognitive impulsivity was uniquely associated with core dimensions of OCD (greater obsessions and compulsions) but only in individuals with active AN. Similarly, greater harm avoidance was uniquely associated with core dimensions of AN—greater drive for thinness and body dissatisfaction—but only in individuals with active AN.
Concern over Mistakes
Concern over mistakes represents a transdiagnostic personality trait associated across all core dimensions of AN and OCD including greater obsessions, compulsions, body dissatisfaction, and drive for thinness. Because this study is cross-sectional, we cannot investigate the temporality of the associations between concern over mistakes and AN and OCD symptoms. Thus, it is difficult to determine whether concern over mistakes is a risk factor for core dimensions of AN and OCD or a sequela of experience with the symptoms that define these disorders. For example, individuals with greater AN and OCD symptom severity may be more concerned about making mistakes because they face increased social scrutiny due to their psychiatric diagnosis or because the experience of having a psychiatric diagnosis alters their personality in other ways (Klump et al., 2004).
However, studies have also found evidence that concern over mistakes may be a premorbid risk factor for later dysfunction in the core dimensions of both AN and OCD. In retrospective studies, premorbid perfectionism is commonly cited as a risk factor for eating disorders in general and for AN in particular (Bardone-Cone et al., 2007; Bulik et al., 2003; Egan et al., 2011). In prospective studies, concern over mistakes predicts greater body dissatisfaction, importance of weight for social evaluation, and eating disorder risk (Boone et al., 2014; Wade et al., 2015). In particular, concern over mistakes leads to greater ineffectiveness and thus, greater risk for eating disorders in adolescent girls (Wade et al., 2015).
Compulsivity
Compulsivity has recently been theorized to be a primary driver of AN and OCD symptom comorbidity (Godier & Park, 2015; Steinglass & Walsh, 2006). In line with our first hypothesis, we found some support for these proposals in each model. Although, personality and psychological factors explained the associations between obsessions and core dimensions of AN, this was not true for compulsions. Even when personality and psychological factors were included, compulsivity continued to have significant and unique correlations with both drive for thinness and body dissatisfaction. Thus, our model was not able to fully explain why the severity of compulsions and core dimensions of AN are associated.
Limitations and Implications
The primary strength and limitation of the present study is that all participants had AN diagnoses. Although this permits examination of shared dimensions between AN and OCD in AN patients, these findings may not generalize to individuals with a primary diagnosis of OCD (i.e., without a diagnosis of AN) or to the general population. Additionally, our results are cross-sectional, and thus, we cannot make assumptions about causality (Maxwell & Cole, 2007). However, this research can serve as hypothesis generation for future prospective studies. Another major limitation was that our measures asked about either the current time or the time when the individual was most ill, creating discrepancies in the timing across measures and potential for recall bias. However, we accounted for these discrepancies by testing invariance in recovered versus active ED individuals (theorizing that individuals with an active ED would equate to assessment of both current and when most ill). We found that, regardless of recovery status, concern over mistakes was a factor for obsessions, compulsions, body dissatisfaction, and drive for thinness, suggesting that regardless of when asked, concern over mistakes remains a central factor in explaining the severity of the core features of OCD and AN. Additionally, we did not include Obsessive-Compulsive Personality Disorder (OCPD) in these analyses, which might account for some of our findings. Future research should test a model of shared vulnerability for OCPD and AN, with OCPD as both a potential outcome and as a potential confound for the traits considered here. Finally, our measures were all self-report and therefore hold the inherent limitations of self-report research, although we did strive to use measures with strong psychometric properties. Finally, our participants were primarily women, and this limits the generalizability of our findings to men or other genders with eating disorders.
Potential prevention and treatment implications from these findings may suggest that tailoring interventions for participants who score high on concern over mistakes could potentially alter developmental trajectories towards AN and OCD. This work also suggests a mechanism for why CBT for perfectionism can have wide-ranging effects on both anxiety and eating disorder symptoms (Handley et al., 2015). Assessing and reducing concern over mistakes through therapy, either through exposure or cognitive restructuring, could have beneficial effects for obsessions, compulsions, drive for thinness, and body dissatisfaction in individuals with AN.
Conclusion
We found that out of all the potential psychological and personality factors, concern over mistakes was the only factor associated with core dimensions of both AN and OCD in women with AN. These results provide novel insights into the transdiagnostic role concern over mistakes might play for AN and OCD and suggestive evidence that concern over mistakes may be an important target for both prevention and treatment for comorbid OCD in women with AN.
Funding
This research was supported by the National Institutes of Health Grant (MH66117). Dr. Zerwas is supported by a NIMH career development grant (K01MH100435). Dr. Bulik acknowledges funding from the Swedish Research Council (VR Dnr: 538-2013-8864). Dr. Strober was supported in part by the Franklin Mint Endowed Chair in Eating Disorders. The authors thank the Price Foundation for the support of the clinical collection of participants for the Price Foundation study.
The study funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflicts of Interest
CM Bulik reports: Shire (grant recipient, Scientific Advisory Board member) and Pearson and Walker (author, royalty recipient). Other authors have no conflicts of interest to report.
We also tested a model that included all four outcome variables (obsessions, compulsions, drive for thinness, and body dissatisfaction) in one model. There were no substantial changes to results when all outcomes were combined
References
- Altman SE, & Shankman SA (2009). What is the association between obsessive–compulsive disorder and eating disorders? Clinical Psychology Review, 29, 638–646. doi: 10.1016/j.cpr.2009.08.001 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition Text Revision. Washington, DC: American Psychiatric Press. [Google Scholar]
- Anderluh M, Tchanturia K, Rabe-Hesketh S, & Treasure J (2003). Childhood obsessive-compulsive personality traits in adult women with eating disorders: defining a broader eating disorder phenotype. American Journal of Psychiatry, 160, 242–247. doi: 10.1176/appi.ajp.160.2.242 [DOI] [PubMed] [Google Scholar]
- Anttila V, Bulik-Sullivan B, Finucane H, Ripke S, Malik R, & Pers T (2014). The Brainstorm project: a cross-phenotype analysis of 14 brain disorders by heritability-, constraint- and pathway-based methods, using genome-wide association data from 500,000 samples Paper presented at the American Society of Human Genetics Annual Meeting, San Diego, CA [Google Scholar]
- Bardone-Cone A, Schaefer LM, Maldonado CR, Fitzsimmons EE, Harney MB, Lawson MA, … Smith R (2010). Aspects of self-concept and eating disorder recovery: What does the sense of self look like when an individual recovers from an eating disorder? Journal of Social and Clinical Psychology, 29, 821–846.] [Google Scholar]
- Bardone-Cone A, Wonderlich SA, Frost RO, Bulik CM, Mitchell JE, Uppala S, & Simonich H (2007). Perfectionism and eating disorders: current status and future directions. Clinical Psychology Review, 27, 384–405. doi: 10.1016/j.cpr.2006.12.005 [DOI] [PubMed] [Google Scholar]
- Barratt ES (1965). Factor analysis of some psychometric measures of impulsiveness and anxiety. Psychological Reports, 16, 547–554. [DOI] [PubMed] [Google Scholar]
- Benatti B, Dell’Osso B, Arici C, Hollander E, & Altamura AC (2014). Characterizing impulsivity profile in patients with obsessive–compulsive disorder. International Journal of Psychiatry in Clinical Practice, 18, 156–160. doi: 10.3109/13651501.2013.855792 [DOI] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. doi: 10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Bollen K (1989). Structural equations with latent variables. New York: Wiley. [Google Scholar]
- Boone L, Soenens B, & Luyten P (2014). When or why does perfectionism translate into eating disorder pathology? A longitudinal examination of the moderating and mediating role of body dissatisfaction. Journal of Abnormal Psychology, 123, 412–418. doi: 10.1037/a0036254 [DOI] [PubMed] [Google Scholar]
- Brown TA, & Barlow DH (2005). Dimensional versus categorical classification of mental disorders in the fifth edition of the Diagnostic and statistical manual of mental disorders and beyond: Comment on the special section. Journal of Abnormal Psychology, 114, 551–556. doi: 10.1037/0021-843X.114.4.551 [DOI] [PubMed] [Google Scholar]
- Bulik C, Sullivan P, Fear J, & Joyce P (1997). Eating disorders and antecedent anxiety disorders: A controlled study. Acta Psychiatrica Scandinavica, 96, 101–107. doi: 10.1111/j.1600-0447.1997.tb09913.x [DOI] [PubMed] [Google Scholar]
- Bulik C, Tozzi F, Anderson C, Mazzeo S, Aggen S, & Sullivan P (2003). The relation between eating disorders and components of perfectionism. American Journal of Psychiatry, 160, 366–368. doi: 10.1176/appi.ajp.160.2.366 [DOI] [PubMed] [Google Scholar]
- Cederlöf M, Thornton LM, Baker J, Lichtenstein P, Larsson H, Ruck C, … Mataix-Cols D (2015). Etiological overlap between obsessive-compulsive disorder and anorexia nervosa: a longitudinal cohort, multigenerational family and twin study. World Psychiatry, 14, 333–338. doi: 10.1002/wps.20251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloninger CR, Svrakic DM, & Przybeck TR (1993). A psychobiological model of temperament and character. Archives of General Psychiatry, 50, 975–990. [DOI] [PubMed] [Google Scholar]
- Costa PT, & MacCrae RR (1992). Revised NEO personality inventory (NEO PI-R) and NEO five-factor inventory (NEO-FFI): Professional manual. Psychological Assessment Resources, Incorporated. [Google Scholar]
- Crane AM, Roberts ME, & Treasure J (2007). Are obsessive-compulsive personality traits associated with a poor outcome in anorexia nervosa? A systematic review of randomized controlled trials and naturalistic outcome studies. International Journal of Eating Disorders, 40, 581–588. doi: 10.1002/eat.20419 [DOI] [PubMed] [Google Scholar]
- Egan SJ, Wade TD, & Shafran R (2011). Perfectionism as a transdiagnostic process: a clinical review. Clinical Psychology Review, 31, 203–212. doi: 10.1016/j.cpr.2010.04.009 [DOI] [PubMed] [Google Scholar]
- Ettelt S, Grabe HJ, Ruhrmann S, Buhtz F, Hochrein A, Kraft S, … Maier W (2008). Harm avoidance in subjects with obsessive-compulsive disorder and their families. Journal of Affective Disorders, 107, 265–269. doi: 10.1016/j.jad.2007.08.017 [DOI] [PubMed] [Google Scholar]
- Fassino S, Abbate-Daga G, Amianto F, Leombruni P, Boggio S, & Rovera GG (2002). Temperament and character profile of eating disorders: a controlled study with the Temperament and Character Inventory. International Journal of Eating Disorders, 32, 412–425. doi: 10.1002/eat.10099 [DOI] [PubMed] [Google Scholar]
- Frost R, Marten P, Lahart C, & Rosenblate R (1990). The dimensions of perfectionism. Cognitive Therapy and Research, 14, 449–468. [Google Scholar]
- Garner D (1990). Eating Disorder Inventory-2 Professional Manual. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Garner D, Olmstead M, & Polivy J (1983). The eating disorders inventory: a measure of cognitive-behavioural dimensions of anorexia and bulimia In Darby P (Ed.), Anorexia nervosa: recent developments in research (pp. 173–184). New York: Liss, AR. [Google Scholar]
- Godier LR, & Park RJ (2015). A novel measure of compulsive food restriction in anorexia nervosa: validation of the Self-Starvation Scale (SS). Eating Behaviors, 17, 10–13. doi: 10.1016/j.eatbeh.2014.12.004 [DOI] [PubMed] [Google Scholar]
- Goodman W, Price L, Rasmussen S, Mazure C, Fleischmann R, Hill C, … Charney D (1989). The Yale-Brown Obsessive-Compulsive Scale (Y-BOCS): I. development, use, and reliability. Archives of General Psychiatry, 46, 1006–1011. [DOI] [PubMed] [Google Scholar]
- Handley AK, Egan SJ, Kane RT, & Rees CS (2015). A randomised controlled trial of group cognitive behavioural therapy for perfectionism. Behaviour Research and Therapy, 68, 37–47. doi: 10.1016/j.brat.2015.02.006 [DOI] [PubMed] [Google Scholar]
- Hebebrand J, Himmelmann GW, Heseker H, Schafer H, & Remschmidt H (1996). Use of percentiles for the body mass index in anorexia nervosa: diagnostic, epidemiological, and therapeutic considerations. International Journal of Eating Disorders, 19, 359–369. doi: [DOI] [PubMed] [Google Scholar]
- Hoek HW (2006). Incidence, prevalence and mortality of anorexia nervosa and other eating disorders. Current Opinion in Psychiatry, 19, 389–394. doi: 10.1097/01.yco.0000228759.95237.78 [DOI] [PubMed] [Google Scholar]
- Hu L. t., & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jöreskog KG, & Sörbom D (1981). LISREL V: Analysis of linear structural relationships by maximum likelihood and least squares methods: University of Uppsala, Department of Statistics. [Google Scholar]
- Klump KL, Bulik CM, Pollice C, Halmi KA, Fichter MM, Berrettini WH, … Kaye WH (2000). Temperament and character in women with anorexia nervosa. Journal of Nervous and Mental Disorders, 188, 559–567. [DOI] [PubMed] [Google Scholar]
- Klump KL, Strober M, Bulik CM, Thornton L, Johnson C, Devlin B, … Kaye, WH (2004). Personality characteristics of women before and after recovery from an eating disorder. Psychological Medicine, 34, 1407–1418. doi: 10.1017/S0033291704002442 [DOI] [PubMed] [Google Scholar]
- LaSalle VH, Cromer KR, Nelson KN, Kazuba D, Justement L, & Murphy DL (2004). Diagnostic interview assessed neuropsychiatric disorder comorbidity in 334 individuals with obsessive-compulsive disorder. Depression and Anxiety, 19, 163–173. doi: 10.1002/da.20009 [DOI] [PubMed] [Google Scholar]
- Lee JC, Prado HS, Diniz JB, Borcato S, da Silva CB, Hounie AG, … do Rosário MC (2009). Perfectionism and sensory phenomena: phenotypic components of obsessive-compulsive disorder. Comprehensive Psychiatry, 50, 431–436. doi: 10.1016/j.comppsych.2008.11.007 [DOI] [PubMed] [Google Scholar]
- Loehlin JC (1998). Latent variable models: An introduction to factor, path, and structural analysis. Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Mas S, Plana MT, Castro-Fornieles J, Gassó P, Lafuente A, Moreno E, … Lazaro L (2013). Common genetic background in anorexia nervosa and obsessive compulsive disorder: preliminary results from an association study. Journal of Psychiatric Research, 47, 747–754. doi: 10.1016/j.jpsychires.2012.12.015 [DOI] [PubMed] [Google Scholar]
- Maxwell SE, & Cole DA (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods, 12, 23–44. doi: 10.1037/1082-989X.12.1.23 [DOI] [PubMed] [Google Scholar]
- Micali N, Hilton K, Nakatani E, Heyman I, Turner C, & Mataix-Cols D (2011). Is childhood OCD a risk factor for eating disorders later in life? A longitudinal study. Psychological Medicine, 41, 2507–2513. doi: 10.1017/S003329171100078X [DOI] [PubMed] [Google Scholar]
- Muthén L, & Muthén B (1998). Mplus User’s Guide, 7th Edn: Muthén and Muthén; Los Angeles, CA. [Google Scholar]
- Nolen-Hoeksema S, & Watkins ER (2011). A heuristic for developing transdiagnostic models of psychopathology: Explaining multifinality and divergent trajectories. Perspectives on Psychological Science, 6, 589–609. doi: 10.1177/1745691611419672 [DOI] [PubMed] [Google Scholar]
- Ormel J, Rosmalen J, & Farmer A (2004). Neuroticism: a non-informative marker of vulnerability to psychopathology. Social Psychiatry and Psychiatric Epidemiology, 39, 906–912. [DOI] [PubMed] [Google Scholar]
- Pato M, Eisen J, & Pato C (1994). Rating scales for obsessive compulsive behavior In Hollander E, Zohar J, Marassati D, & Olivier B (Eds.), Current Insights in Obsessive Compulsive Disorder (pp. 77–91). New York: John Wiley & Sons. [Google Scholar]
- Pinto A, Mancebo MC, Eisen JL, Pagano ME, & Rasmussen SA (2006). The Brown Longitudinal Obsessive Compulsive Study: clinical features and symptoms of the sample at intake. Journal of Clinical Psychiatry, 67, 703–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reba L, Thornton L, Tozzi F, Klump KL, Brandt H, Crawford S, … Bulik CM (2005). Relationships between features associated with vomiting in purging-type eating disorders. International Journal of Eating Disorders, 38, 287–294. doi: 10.1002/eat.20189 [DOI] [PubMed] [Google Scholar]
- Roncero M, Perpiñá C, & García-Soriano G (2011). Study of obsessive compulsive beliefs: relationship with eating disorders. Behavioural and Cognitive Psychotherapy, 39, 457–470. doi: 10.1017/S1352465811000099 [DOI] [PubMed] [Google Scholar]
- Rosval L, Steiger H, Bruce K, Israël M, Richardson J, & Aubut M (2006). Impulsivity in women with eating disorders: problem of response inhibition, planning, or attention? International Journal of Eating Disorders, 39, 590–593. doi: 10.1002/eat.20296 [DOI] [PubMed] [Google Scholar]
- Simpson HB, Wetterneck CT, Cahill SP, Steinglass JE, Franklin ME, Leonard RC, … Riemann, BC (2013). Treatment of obsessive-compulsive disorder complicated by comorbid eating disorders. Cognitive Behavior Therapy, 42, 64–76. doi: 10.1080/16506073.2012.751124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C, Gorsuch R, & Luchene R (1970). The State-Trait Anxiety Inventory: Test manual for Form X. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Steiger J, & Lind J (1980). Statistically-based tests for the number of factors Paper presented at the Annual Spring Meeting of the Psychometric Society, Iowa City, IA. [Google Scholar]
- Steinglass J, & Walsh BT (2006). Habit learning and anorexia nervosa: a cognitive neuroscience hypothesis. International Journal of Eating Disorders, 39, 267–275. doi: 10.1002/eat.20244 [DOI] [PubMed] [Google Scholar]
- Steinhausen HC, Jakobsen H, Helenius D, Munk‐Jørgensen P, & Strober M (2015). A nation‐wide study of the family aggregation and risk factors in anorexia nervosa over three generations. International Journal of Eating Disorders, 48, 1–8. [DOI] [PubMed] [Google Scholar]
- Suda M, Brooks SJ, Giampietro V, Uher R, Mataix-Cols D, Brammer MJ, … Campbell IC. (2014). Provocation of symmetry/ordering symptoms in Anorexia nervosa: a functional neuroimaging study. PLoS ONE, 9, e97998. doi: 10.1371/journal.pone.0097998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki T (2005). Relationship Between Two Aspects of Perfectionism and Obsessive- Compulsive Symptoms. Psychological Reports, 96, 299–305. doi: 10.2466/pr0.96.2.299-305 [DOI] [PubMed] [Google Scholar]
- Sysko R, Walsh BT, Schebendach J, & Wilson GT (2005). Eating behavior among women with anorexia nervosa. American Journal of Clinical Nutrition, 82, 296–301. doi: 10.1093/ajcn/82.2.296 [DOI] [PubMed] [Google Scholar]
- Tozzi F, Thornton L, Klump K, Bulik C, Fichter M, Halmi K, … Kaye W (2005). Symptom fluctuation in eating disorders: correlates of diagnostic crossover. American Jounal of Psychiatry, 162, 732–740. doi: 10.1176/appi.ajp.162.4.732 [DOI] [PubMed] [Google Scholar]
- Tucker LR, & Lewis C (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38, 1–10. [Google Scholar]
- Wade TD, Wilksch SM, Paxton SJ, Byrne SM, & Austin SB (2015). How perfectionism and ineffectiveness influence growth of eating disorder risk in young adolescent girls. Behaviour Research and Therapy, 66, 56–63. doi: 10.1016/j.brat.2015.01.007 [DOI] [PubMed] [Google Scholar]
- Wildes JE, Ringham RM, & Marcus MD (2010). Emotion avoidance in patients with anorexia nervosa: Initial test of a functional model. International Journal of Eating Disorders, 43, 398–404. doi: 10.1002/eat.20730 [DOI] [PMC free article] [PubMed] [Google Scholar]