Abstract
This study examines how ADHD-related symptoms and impairments interact to predict depression symptoms in young adolescents with ADHD. A sample of 342 adolescents (71% male, mean age = 13 years old) with DSM-IV-TR diagnosed ADHD completed baseline clinical assessments upon entry to a psychosocial treatment study for ADHD. Ratings of ADHD and sluggish cognitive tempo (SCT) symptoms, and social and academic impairment were obtained from parents, while ratings of depressive symptoms and conflict with parents were obtained from youth. Among adolescents with ADHD, elevated depressive symptoms were associated with higher SCT symptom severity, lower hyperactive/impulsive (HI) symptom severity, higher social impairments, higher conflict with parents, and lower academic problems. Interaction effects indicated that clinically significant depressive symptoms were most likely to occur when high levels of parent–youth conflict were present along with high inattentive (IN) symptoms, high SCT, and/or low HI. Among children and adolescents with ADHD, depression prevention efforts might target IN/SCT symptom management, as well as improving interpersonal relationships with parents and peers. Future work is needed to verify these findings longitudinally.
Keywords: ADHD, Depression, Adolescence, Peer relationships, Sluggish cognitive tempo
Introduction
Adolescents with attention-deficit/hyperactivity disorder (ADHD) are at significant risk of developing depression and related problems compared to typically developing peers (Angold and Costello 1993; Biederman et al. 2006; Meinzer et al. 2014). This comorbid presentation is associated with increased functional impairment, psychiatric hospitalization, and a threefold increase in risk for suicidality (Chronis-Tuscano et al. 2010; Biederman et al. 2008). According to recent epidemiological findings, 14% of children and adolescents with ADHD were reported to have a diagnosis of depression compared to 1% of non-ADHD youth (Larson et al. 2011). Longitudinal findings show that children with ADHD have a fourfold risk for developing major depression or dysthymia in adolescence (Chronis-Tuscano et al. 2010). Furthermore, depressive symptoms in individuals with ADHD may be more chronic than among non-ADHD youth. A recent longitudinal study indicated that children with ADHD exhibit elevated depressive symptoms by age 18 compared to non-ADHD children, and those youth with a history of ADHD continued to experience elevated depressive symptoms relative to same-age peers from ages 18–25 years (Meinzer et al. 2016).
Among youth with and without ADHD, adolescence appears to be the peak period for the onset of major depression (Biederman et al. 1995; Costello et al. 2003; Hankin et al. 1998). Among youth without ADHD, extant findings point to important risk factors for developing depression including academic problems (Reinherz et al. 1999; Verboom et al. 2014), family conflict (Sheeber et al. 1997), and social difficulties (Prinstein et al. 2005; Verboom et al., 2014). Notably, these same domains are among the most common areas of impairment for youth with ADHD (APA 2000).
Several explanations for the co-occurrence of ADHD and depression have been proposed. The first suggests that “ADHD with depression” results from a unique underlying etiology that is distinct from either ADHD or depression alone (Mick et al. 2003). In line with this theory, symptoms of ADHD in childhood predict depressive symptoms when controlling for other comorbidities (Biederman et al. 2006) and psychosocial impairments (Meinzer et al. 2013). This suggests a direct link between ADHD and depressive symptoms independent of allostatic factors. Within this model, depressive symptoms appear to be more commonly linked with inattention (IN) than hyperactive/impulsive (HI) symptoms (Hartman et al. 2001; Willcutt et al. 2012). Furthermore, family members of youth with comorbid ADHD and depression have greater risk for depression than families of youth with ADHD alone, suggesting a heritable etiology (Biederman et al. 1991; Mick et al. 2003). However, it is not certain whether these family associations are due to shared environmental effects.
A second explanation is that sluggish cognitive tempo (SCT) may contribute to the link between ADHD and depression. SCT is a behavioral dimension characterized by frequent daydreaming, confusion, and lack of energy that is highly correlated with, but reliably distinct from, inattentive symptoms (Barkley 2013; Becker et al. 2016a; Lee et al. 2014). SCT is robustly correlated with depressive symptoms (Barkley 2013; Becker et al. 2014, 2016a, b; del Mar Bernad et al. 2016; Camprodon-Rosanas et al. 2017; Carlson and Mann 2002; Khadka et al. 2016) and appears to account for much of the covariance between ADHD and depressive symptoms (independent of IN symptoms and externalizing psychopathology; Becker et al. 2016a). Several studies indicate that the relationship between IN symptoms and depression is no longer significant when SCT is accounted for, though SCT remains associated with depression when controlling for IN (Barkley 2013; del Mar Bernad et al. 2016; Penny et al. 2009; Lee et al. 2014). Therefore, SCT appears to constitute an important risk factor that should be integrated into investigations on risk for depression among ADHD youth.
A final explanation for the high rates of depression seen among adolescents with ADHD posits that depression may emerge in adolescents with ADHD due to high levels of impairment and, therefore, stress and demoralization secondary to ADHD (Biederman et al. 1998; Yeguez et al. 2018). For example, parents of adolescents with ADHD report greater parenting stress and conflict with their children compared with parents of non-ADHD youth (Edwards et al. 2001). Youth with ADHD experience more frequent and enduring rejection by peers than typically developing youth (Erhardt and Hinshaw 1994; Hoza et al. 2005; Nijmeijer et al. 2008), and both peer and parent–child relational problems are found to mediate the onset of depressive symptoms (Humphreys et al. 2013; Ostrander et al. 2006). Likewise, academic underperformance is another prominent impairment of adolescents with ADHD (Barbaresi et al. 2007; Kent et al. 2011) and is linked to co-occurring depression in youth with ADHD (Herman et al. 2007; Herman and Ostrander 2007).
Thus, the association between ADHD and depression may emerge from a distinct clinical etiology (i.e., ADHD with depression), a shared association with SCT, or the effects of functional impairment on self-worth. These hypotheses are not orthogonal; all three may contribute to the development of adolescent depression in children with ADHD. To better understand the interplay of factors proposed in these theories, the present study evaluates the relationship between ADHD symptoms, SCT, and environmental impairments in predicting depressive symptoms among adolescents with ADHD. Consistent with multiple pathways between ADHD and depression, it was hypothesized that: (1) IN and SCT, but not HI, would be uniquely associated with comorbid depressive symptoms and (2) peer relationship problems, academic problems, and parent–teen conflict would also be associated with elevated depressive symptoms, above the contribution of symptom-level variables. To develop hypotheses for future research, we also explored interactions between significant predictors to detect potential interplay amongst hypotheses for the ADHD-depression link.
Methods
Participants
Participants were 342 adolescents with ADHD, aged 11–16 years old (M = 13.09, SD= 1.62), who completed a standard intake battery (see Sibley et al. 2014, 2016) as part of recruitment into one of two psychosocial treatment trials between 2010 and 2013. Participants were referred by their parents and schools, and data were collected from parents, adolescents, and teachers at initial presentation to the research clinic (Table 1).
Table 1.
Sample characteristics (N = 342)
| Age M (SD) | 13.09 (1.62) |
| Estimated full-scale IQ—M (SD) | 97.00 (12.72) |
| Male (%) | 71.0 |
| Race/ethnicity (%) | |
| White non-hispanic | 7.6 |
| Black non-hispanic | 14.6 |
| Hispanic any race | 73.7 |
| Other | 4.1 |
| Parent highest education level (%) | |
| High school or less | 19.7 |
| Some college/specialized training | 28.5 |
| Bachelor’s degree | 32.9 |
| Master’s degree or higher | 18.8 |
| ADHD subtype (%) | |
| ADHD-Predominantly inattentive | 39.3 |
| ADHD-Combined | 60.7 |
| ODD diagnosis (%) | 36.4 |
| CD diagnosis (%) | 8.5 |
| Withdrawn/depressed t-score M (SD) | 57.1 (7.7) |
| T-score>65 (%) | 17.5 |
| Anxious/depressed t-score M (SD) | 57.0 (8.7) |
| T-score>65(%) | 19.0 |
| Current ADHD medication (%) | 43.7 |
| Current antidepressant/mood stabilizer (%) | 2.0 |
Estimated full-scale IQ from WASI-II; ADHD subtype, ODD, and CD diagnoses made by dual clinician review; withdrawn/depressed and Anxious t-scores from youth self-report form (Achenbach and Rescorla 2001)
Prior to participation, a brief phone screen with the primary caretaker ascertained previous diagnosis of ADHD, current symptoms of ADHD, and associated impairment. Families were invited to an intake assessment to determine study eligibility if the parent endorsed: (1) a previous diagnosis of ADHD OR four or more symptoms of either inattention or hyperactivity/impulsivity (APA 2000) AND (2) clinically significant problems in daily functioning (at least a “3” on a “0–6” impairment scale; Fabiano et al. 2006). Participants were required to (a) meet Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV-TR) diagnostic criteria for ADHD at an intake assessment, (b) be enrolled in school, (c) have an estimated IQ > 75, and (d) have no history of an autism spectrum disorder.
Procedures
All procedures were approved by the university institutional review board. Parental informed consent and adolescent assent were obtained. DSM-IV-TR ADHD diagnosis was assessed using structured clinical interview (C-DISC; Shaffer et al. 2000) administered to parents, as well as parent and teacher symptom and impairment ratings (Disruptive Behavior Disorder Rating Scale and Impairment Rating Scale; Pelham et al. 1992; Fabiano et al. 2006) per recommended best practices (Pelham et al. 2005). Brief tests of adolescent intellectual (Wechsler Abbreviated Scale of Intelligence, First or Second Edition; Wechsler 1999, 2011) and academic functioning (Wechsler Individual Achievement Test-III: Word Reading, Numerical Operations, and Spelling subtests; Wechsler 2009) were administered. Eligibility and diagnosis were determined through dual review of the resulting data by two Ph.D.-level clinicians. A third clinician was consulted to resolve disagreement, which occurred on six occasions.
Measures
Unless otherwise noted, parent-report measures were used given findings that adolescents with ADHD may underreport externalizing symptoms and functional impairments in clinical assessment (Fischer et al. 1993; Sibley et al. 2012a, b, 2014).
Depressive symptoms
Adolescents completed the Youth Self-Report (YSR), a widely used, well-validated measure of psychosocial adjustment problems in youth ages 11–18 years (Achenbach and Rescorla 2001). For internalizing problems in children and adolescents, youth self-report data are shown to be more sensitive than parent report alone (Jensen et al. 1999), and widely cited best practices emphasize the importance of self-report for assessing mood problems in adolescents (Klein et al. 2005). The Withdrawn/Depressed subscale is used to index depressive symptoms, but was modified to omit the item “Underactive, slow-moving, or lacks energy” which also appears in the parent-reported CBCL Sluggish Cognitive Tempo scale (described below). This subscale was calculated as the mean of the raw scores for remaining seven items and includes items that characterize social withdrawal, sadness, and anhedonia. This modified seven-item scale was highly correlated with the original (r = .95) and yielded internal consistency of α = .65 (somewhat lower than that obtained for the original sample norms, α = .71; Achenbach and Rescorla 2001).
ADHD and SCT symptoms
ADHD symptoms
The Disruptive Behavior Disorders Rating Scale (parent-report; Pelham et al. 1992) was used to measure symptoms of ADHD. The DBD has demonstrated excellent psychometric properties for child and adolescent samples, with evidence of distinct IN and HI factors (Pillow et al. 1998; Sibley et al. 2012a, b) and subscales with high internal consistency (α = .90 and .89, respectively, for the current sample).
SCT symptoms
The Child Behavior Checklist (CBCL; Achenbach and Rescorla 2001, 2007) was used to assess SCT. The CBCL is a well-validated parent-report broadband assessment tool used to screen for various problems. SCT has traditionally been measured by parent or teacher report, and well-validated self-report measures do not exist currently. The SCT subscale of the CBCL was used given its extensive use in previous research (e.g., Carlson and Mann 2002; Hartman et al. 2004); the SCT scale consists of the following items: Confused or seems to be in a fog; Day-dreams or gets lost in thoughts; Stares blankly; Underactive, slow-moving, or lacks energy with internal consistency of α = .66, which exceeds the internal consistency originally reported in the CBCL manual (Achenbach and Rescorla 2007).
Functioning and impairment
Social problems
The Social Problems subscale from the parent-report CBCL was used as an index of social functioning. The Social Problems subscale consists of items that index behaviors that indicate rejection by peers or difficulty socializing (such as being teased, not getting along with others, and socializing primarily with younger children). The social problems scale demonstrated acceptable internal consistency, α = .75.
Academic problems
The parent version of the Adolescent Academic Problems Checklist (Sibley et al. 2014) consists of 24 items that assess academic problems common to adolescents with ADHD during secondary school, particularly those that are associated with school failure. The psychometric properties of this measure are strong (Sibley et al. 2014), and previous research indicates that parents provide more valid reports of academic functioning than self-reports for adolescents with ADHD (Sibley et al. 2012a, b). Respondents rate each item as not at all (0), just a little (1), pretty much (2), or very much (3). Items are averaged for a single factor score. Internal consistency was excellent for the current sample (α = .92).
Parent–teen conflict
To assess parent–teen conflict, the youth-report Conflict Behavior Questionnaire-20 was used (CBQ-20; Robin and Foster 1989). The CBQ-20 is a 20-item scale adapted from the 73-item CBQ. The items used in the CBQ-20 best discriminated distressed from non-distressed families and is correlated very highly with the CBQ (r = .96; Robin and Foster 1989). In recent studies, parent-completed ratings of conflict interactions yielded greater severity than youth report of the same interactions (De Los Reyes et al. 2012). Thus, the more conservative index of parent–youth conflict (youth report) was selected to minimize confounding effect with oppositional symptoms. The 20 items on the CBQ-20 consist of statements about the parent–adolescent relationship, such as “My mom/dad screams a lot”; the adolescent rated the primary caretaker on the relevance of each on a 1–5 Likert scale. In the current study, alpha for the adolescent version was excellent (α = .91).
Data analysis plan
Hierarchical linear regression examined the mutual contributions of symptom-level (IN, HI, and SCT) and impairment-level features (parent–child conflict, academic problems, social skills deficits) to adolescent depressive symptoms. All predictors were mean-centered. All assumptions of multiple regression were examined to ensure appropriateness of analytic approach. The outcome variable in the model was depressive symptoms. At step 1, IN, HI, and SCT symptom severity were entered into the model. At step 2, academic problems, social problems, and parent–teen conflict were entered.
In an exploratory third step, interactions among the symptom-level and impairment-level predictors were separately probed. To do so, we specified individual two-way interactions between each symptom-level variable (IN, HI, and SCT) with each domain of impairment (social problems, parent–youth conflict, and academic problems) resulting in nine separate models. In each of these models, the interaction in question was included as a third step. According to recommended practices (Hayes and Matthes 2009), significant interactions were probed by graphing the moderator at ± 1 SD and examining Johnson–Neyman effects (Aiken and West 1991; Johnson and Neyman 1936; Bauer and Curran 2005).
Results
Pearson’s bivariate correlations among the included variables are shown in Table 2. There were no indications of multicollinearity. At step 1, the model reached significance (R2 = .05, F(3, 323) = 5.56, p = .001). SCT uniquely predicted depressive symptoms (b = 0.20, p < .01; Table 3). Step 2 predictors contributed incrementally to the model (ΔR2 = .07, F(6, 320) = 6.97, p < .001). Specifically, higher depression symptoms were predicted by higher SCT (b = 0.01, p < .01), lower HI symptoms (b = − 0.08; p < .05), higher social problems (b = 0.01, p < .05), lower academic problems (b = − 0.12, p < .05), and higher parent–teen conflict (b = 0.10, p < .001).1 Full results of the model are shown in Table 3.
Table 2.
Means and inter-correlations for variables of interest
| Variables | M (SD) | Age | IQ | IN | Hyp | ADHD | SCT | AAP | Soc | CBQ | YSR |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 13.09 (1.62) | 1.00 | −.17** | −.06 | −.15** | −.12* | .05 | .12* | −.06 | −19** | −.05 |
| IQ | 97 (12.72) | 1.00 | .13 | .01 | .08 | .07 | .17** | .02 | .12* | −.04 | |
| INa | 1.84 (0.72) | 1.00 | .55** | .88** | .42** | .67** | .34** | .15* | .07 | ||
| H/Ia | 1.10 (0.72) | 1.00 | .88** | .15* | .34** | .47** | .14* | −.05 | |||
| ADHD totala | 1.47 (0.64) | 1.00 | .33** | .58** | .40** | .16* | .02 | ||||
| SCTb | 61.84 (8.35) | 1.00 | .38** | .44** | .08 | .20** | |||||
| AAPC | 1.66 (0.57) | 1.00 | .29** | .11* | .01 | ||||||
| Social Probb | 61.53 (8.88) | 1.00 | .04 | .18* | |||||||
| CBQc | 2.41 (1.31) | 1.00 | .18* | ||||||||
| Withdrawnd | 57.12 (7.71) | 1.00 |
AAPC Adolescent academic problems checklist, NS not significant
p < .05;
p < .001
Mean parent rating from disruptive behavior disorders rating scale
Child behavior checklist (parent-report)
Conflict behavior questionnaire youth report
From the youth self-report form
Table 3.
Predictors of youth-report withdrawn/depressive scale
| R2Δ | F | b | SE | β | p | sr2 | |
|---|---|---|---|---|---|---|---|
| Step 1: symptoms | .05 | 5.56* | |||||
| IN symptoms | .03 | .04 | .05 | .45 | .00 | ||
| HI symptoms | −.06 | .03 | −.11 | .10 | .01 | ||
| SCT symptoms | .01 | < .01 | .20 | < .01 | .03 | ||
| Step 2: symptoms + impairment | .07 | 6.97** | |||||
| IN symptoms | .07 | .04 | .13 | .12 | .01 | ||
| HI symptoms | −.09 | .03 | −.18 | < .01 | .02 | ||
| SCT symptoms | .01 | < .01 | .15 | .02 | .01 | ||
| Social problems | .01 | < .01 | .17 | < .01 | .02 | ||
| Academic problems | −.10 | .05 | −.14 | < .05 | .01 | ||
| Parent-teen conflict | .05 | .03 | .19 | < .01 | .03 |
All predictors mean-centered prior to analysis. Exploratory interactions were examined individually.
p < .05,
p < .001;
significant increase in model R2; sr2= squared semi-partial correlation; IN, HI, and SCT = parent-rated inattentive, hyperactive/impulsive, and sluggish cognitive tempo, respectively; withdrawal/depressive symptoms reported by adolescent on
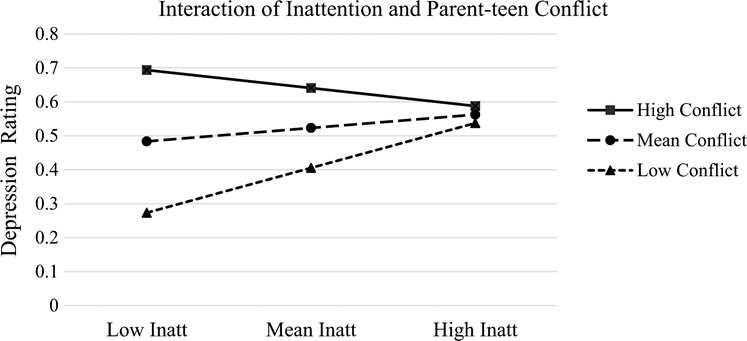
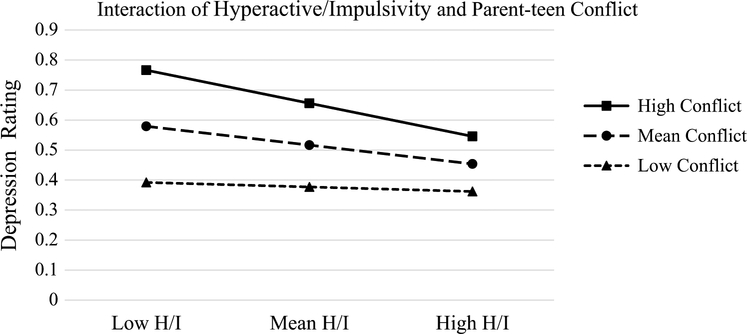
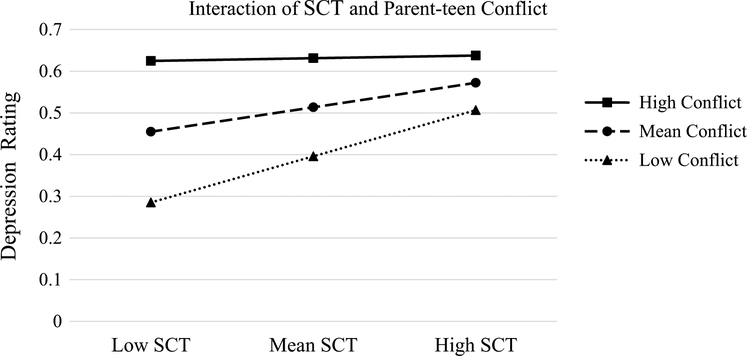
At step 3, the interaction of IN by parent–teen conflict contributed significantly to the model, ΔR2 = .02, F (7, 319) = 6.92, p < .001. Specifically, Johnson–Neyman statistics indicated that, on average, IN was a significant predictor of depressive symptoms for youth who fell below the sample 43rd percentile of parent–teen conflict, but not for those with higher reported parent–teen conflict. Additionally, parent–teen conflict was positively associated with depressive symptoms except for youth whose parent reported IN severity above the sample 73rd percentile (see also Fig. 1). In addition, the interaction between HI and parent–youth conflict also contributed significantly to the model, ΔR2 = .02, F (7, 319) = 6.63, p < .001. In particular, increased HI was associated with reduced depressive symptoms when parent–youth conflict was elevated above the sample 60th percentile, while HI was not associated with depression at mean or below-mean levels of parent–teen conflict (Fig. 2). Finally, the interaction of SCT by parent–youth conflict contributed significantly to the model, ΔR2 = .01, F (7, 319) = 6.45, p < .05 (Fig. 3, such that SCT significantly predicted depressive symptoms when parent–youth conflict was below the sample 72nd percentile. The following interactions were also tested and were not significant: IN × Social Problems (p = .22), HI × Social Problems (p = .84), SCT × Social Problems (p = .05), IN × Academic Problems (p = .75), HI × Academic Problems (p = .91), and SCT × Academic Problems (p = .51).
Fig. 1.
Interaction of inattention and parent–teen conflict predicting withdrawal/depression. Note High/low inattentive symptoms = ± 1 SD inattention, respectively, from disruptive behavior disorders rating scale; high/low conflict = ± 1 SD, respectively, from conflict behavior questionnaire; depression score = mean rating from youth self-report withdrawn/depressed score
Fig. 2.
Interaction of hyperactive/impulsive ratings and parent–teen conflict predicting withdrawal/depression. Note High/low HI symptoms = ± 1 SD, respectively, from disruptive behavior disorders rating scale; high/low conflict = ± 1 SD, respectively, from conflict behavior questionnaire; depression score = mean rating from youth self-report withdrawn/depressed scale
Fig. 3.
Interaction of SCT ratings and parent–teen conflict predicting withdrawal/depression. Note High/low SCT symptoms = ± 1 SD, respectively, from CBCL SCT scale; high/low conflict = ± 1 SD, respectively, from conflict behavior questionnaire; depression score = mean rating from youth self-report withdrawn/depressed scale
Discussion
The present study examines the contribution of symptom-level (IN, HI and SCT) and impairment-level (academic, social and parent–teen conflict) variables to the presence of comorbid depressive symptoms in adolescents with ADHD. Results indicate that adolescents with ADHD who have high levels of SCT symptoms and low levels of HI symptoms were more likely to experience co-occurring depression. Notably, HI symptoms emerged as a negative predictor of depressive symptoms. Furthermore, depression in adolescents with ADHD may have a distinct interpersonal component, with social problems and parent–teen conflict representing environmental links to depressive symptoms. Moderation analyses revealed that depressive symptoms were particularly associated with elevated IN or SCT symptoms combined with high levels of parent–youth conflict (Figs. 1 and 3).
Paradoxically, parent-reported academic problems emerged as a significant negative predictor of depression, which was counter to our hypothesis that academic struggles would be positively associated with depressive symptoms. In post hoc analyses, we explored the possibility that higher IQ may underlie this association, perhaps due to greater self-awareness of depressive symptoms and/or other ADHD-related impairments. However, IQ was not a significant predictor of depressive symptoms (p > .19) nor did IQ interact with academic problems to predict depressive symptoms (p > .60). More intriguing, academic problems did not correlate with depressive symptoms in a simple bivariate fashion, indicating the effect emerged only when controlling for other study variables. An alternate post hoc hypothesis that elevated anxiety might predict less academic problems but elevated depressive symptoms was also not supported (all p > .40).
In terms of symptoms, the current results corroborate previous findings indicating that SCT, more so than IN and HI, is uniquely tied to risk for depression problems (Barkley 2013; Milich et al. 2001). Notably, the effects obtained for SCT and HI symptoms were of similar size, yet, in opposite directions (see Table 3). This finding may suggest that HI symptoms are dampened by depressive symptoms, such as anhedonia or lethargy. On the other hand, it is possible that a particular ADHD symptom profile, characterized by prominent SCT in the absence of HI, is more commonly linked to risk for depression in ADHD youth. In fact, moderation analyses revealed that HI was associated with reduced depressive symptoms when parent–youth conflict was elevated (Fig. 2). Future longitudinal work will be informative for elucidating whether the onset of depression symptoms leads to subsequent reduction in HI for youth with ADHD relative to non-depressed ADHD youth. In addition, such research will be well-poised to address questions regarding potential biases in parent versus self-report of depressive symptoms in ADHD, which may vary from previously observed biases regarding self-report of ADHD symptoms (e.g., Fischer et al. 1993; Fraser et al. 2018; Sibley et al. 2012a, b).
Consistent with studies with non-ADHD adolescent samples (Prinstein et al. 2005; Sheeber et al. 1997), relational impairments were linked with depressive symptoms. For example, elevations in social problems predicted increased depression symptoms. Adolescence typically involves an increased desire for peer-acceptance and sensitivity to the effects of social exclusion (Larson and Richards 1991; Sebastian et al. 2010). Similarly, the association between greater parent–youth conflict and elevations in depression symptoms coincides with normative increase of conflicts with parents as adolescents strive for greater autonomy (Laursen et al. 1998). However, previously noted findings indicate increased parenting stress and parent–teen conflict for youth with ADHD relative to non-affected families (Edwards et al. 2001). These findings suggest that, in the critical period of adolescence, when depressive symptoms often first emerge (Hankin et al. 1998), targeting relational impairments in the treatment of ADHD may have an added benefit of preventing the onset of comorbid depression. Further, implementing a tailored depression prevention intervention for adolescents with ADHD that targets family support may be effective in reducing depressive symptoms (Meinzer et al. 2018).
While the current study did not investigate causal processes, these findings suggest support and future work toward both theories concerning the high comorbidity between ADHD and mood disorders, and the importance of accounting for SCT. The independent contributions of SCT and HI as positive and negative predictors, respectively, implicate a shared vulnerability for depression among ADHD youth. Additionally, the independent associations of impairment features with elevated depressive symptoms indicate an alternative mechanism of increased risk for depression related to environmental stressors. However, these levels of psychopathology interacted in informative ways which prompt hypotheses for future work. For example, high levels of SCT or, separately, parent–teen conflict may serve as independent correlates (Table 3) or act together in a cumulative fashion (see Figs. 1 and 3). Similarly, prevalent HI may act to prevent the onset of depressive symptoms, until parent–teen conflict reaches a certain threshold (Fig. 2).
The current findings may indicate that for adolescents with ADHD, the emergence of depressive symptoms is related to synergistic processes between SCT and relational impairments. However, effectively mapping the emergence (and outcome) of co-occurring mood problems in ADHD will require longitudinal designs which account for the trajectories of symptom-level and impairment-level variables, including associated features such as SCT.
Overall the current findings help to elucidate how features of ADHD and impairment can interact in their association with depression. However, these strengths need to be taken in light of the study’s limitations. First, the current study is cross-sectional, which limits conclusions concerning how the link between ADHD and depressive problems unfolds over time. For example, it may be the case that depressive symptoms cause the relational impairments noted in this paper or exacerbate pre-existing IN or SCT symptoms. Therefore, further longitudinal research is needed. A second potential limitation concerns the modified self-reported depression scale used; however, the modified scale was highly correlated with the original (r = .95) and, therefore, any risk to generalizability should be minimized. Furthermore, the current study utilized a sample of convenience; data were collected at baseline for a larger psychosocial treatment study for adolescents with ADHD, which constrained the measures available.
In addition, the sample was comprised primarily of youth in early to middle adolescence; these findings may not generalize to older adolescents. Furthermore, youth were referred by their parents as well as schools, which may have oversampled youth with academic problems. A strength of the current study is that it represents typically underrepresented ethnic minority research participants (Brown et al. 2014; Peterson 2001). However, the majority Hispanic and middle-class sample (see Table 1) may not generalize to all adolescents with ADHD. Finally, our measure of SCT was a unidimensional parent-reported measure; multi-dimensional measures of SCT were developed and rigorously tested subsequent to our data collection (e.g., Penny et al. 2009). Nascent findings have also begun to support the validity of self-report measures of SCT (Smith et al. 2018). Future research in this area would benefit from incorporating such instruments.
The current study informs the assessment and treatment of adolescents with ADHD, who frequently present with co-occurring disorders and a complex profile of functional impairments. Early intervention and treatment of ADHD may reduce symptom severity and associated impairment across the lifespan. Thus, a lifespan approach to preventing depression should be considered for youth with ADHD. These results also specifically suggest the importance of assessing for SCT and a range of interpersonal impairments, since these features may serve as risk markers for comorbid depressive symptoms and can inform conceptualization and treatment planning. In addition, the possibility should be explored that youth with high levels of SCT, low levels of HI, and elevated depressive symptoms may require novel treatments. For example, some treatment studies designed to treat ADHD predominantly inattentive type have shown promise for reducing SCT as well (Pfiffner et al. 2007). Developing similar interventions for adolescents, and potentially integrating depression prevention modules with cognitive, interpersonal, or tailored prevention components (e.g., Meinzer et al. 2018; Young and Mufson 2008), may be a promising approach to improving the functioning of youth with ADHD and comorbid depression.
Funding
This research was supported in part by Grants from the National Institute of Mental Health (R34 MH092466) and Institute of Education Sciences (R324A120169).
Footnotes
Conflict of interest The authors declare that they have no conflicts of interest.
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent Informed consent was obtained from all individual participants included in the study.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Given previous findings that externalizing problems are a primary risk for comorbid internalizing psychopathology in ADHD (e.g., Bagwell et al. 2006; Humphreys et al. 2013), follow-up analyses were completed with ODD symptoms included as a covariate. However, ODD was not a significant predictor and the overall findings were not altered. In addition, results with age, sex, and IQ included as covariates did not alter primary findings and are available upon request.
References
- Achenbach TM, Rescorla LA (2001) Manual for the ASEBA school-age forms and profiles. University of Vermont, Research Center for Children, Youth, and Families, Burlington [Google Scholar]
- Achenbach TM, Rescorla LA (2007) Multicultural supplement to the manual for the ASEBA school-age forms and profiles. University of Vermont, Research Center for Children, Youth, and Families, Burlington [Google Scholar]
- Aiken LS, West SG (1991) Multiple regression: testing and interpreting interactions. Sage Publications Inc, Thousand Oaks [Google Scholar]
- American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders fourth edition (text revision) American Psychiatric Association, Washington, DC [Google Scholar]
- Angold A, Costello EJ (1993) Depressive comorbidity in children and adolescents: empirical, theoretical, and methodological issues. Am J Psychiatry 150(12):1779–1791 [DOI] [PubMed] [Google Scholar]
- Bagwell CL, Molina BS, Kashdan TB, Pelham WE Jr, Hoza B (2006) Anxiety and mood disorders in adolescents with childhood attention-deficit/hyperactivity disorder. J Emot Behav Disord 14(3):178–187 [Google Scholar]
- Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ (2007) Long-term school outcomes for children with attention-deficit/hyperactivity disorder: a population-based perspective. J Dev Behav Pediatr 28(4):265–273 [DOI] [PubMed] [Google Scholar]
- Barkley RA (2013) Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: executive functioning, impairment, and comorbidity. J Clin Child Adolesc Psychol 42(2):161–173 [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Curran PJ (2005) Probing interactions in fixed and multilevel regression: inferential and graphical techniques. Multivar Behav Res 40:373–400 [DOI] [PubMed] [Google Scholar]
- Becker SP, Luebbe AM, Fite PJ, Stoppelbein L, Greening L (2014) Sluggish cognitive tempo in psychiatrically hospitalized children: factor structure and relations to internalizing symptoms, social problems, and observed behavioral dysregulation. J Abnorm Child Psychol 42(1):49–62 [DOI] [PubMed] [Google Scholar]
- Becker SP, Leopold DR, Burns GL, Jarrett MA, Langberg JM, Marshall SA, Willcutt EG (2016a) The internal, external, and diagnostic validity of sluggish cognitive tempo: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry 55(3):163–178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Withrow AR, Stoppelbein L, Luebbe AM, Fite PJ, Greening L (2016b) Sluggish cognitive tempo is associated with suicide risk in psychiatrically hospitalized children. J Child Psychol Psychiatry 57(12):1390–1399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Keenan K, Tsuang MT (1991) Evidence of familial association between attention deficit disorder and major affective disorders. Arch Gen Psychiatry 48(7):633–642 [DOI] [PubMed] [Google Scholar]
- Biederman J, Mick E, Faraone SV (1998) Depression in attention deficit hyperactivity disorder (ADHD) children:“true” depression or demoralization? J Affect Disord 47(1–3):113–122 [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone S, Mick E, Lelon E (1995) Psychiatric comorbidity among referred juveniles with major depression: fact or artifact? J Am Acad Child Adolesc Psychiatry 34(5):579–590 [DOI] [PubMed] [Google Scholar]
- Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens TE, Silva JM, Faraone SV (2006) Young adult outcome of attention deficit hyperactivity disorder: a controlled 10-year follow-up study. Psychol Med 36(02):167–179 [DOI] [PubMed] [Google Scholar]
- Biederman J, Ball SW, Monuteaux MC, Mick E, Spencer TJ, McCreary M, Faraone SV (2008) New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. J Am Acad Child Adolesc Psychiatry 47(4):426–434 [DOI] [PubMed] [Google Scholar]
- Brown G, Marshall M, Bower P, Woodham A, Waheed W (2014) Barriers to recruiting ethnic minorities to mental health research: a systematic review. Int J Methods Psychiatric Res 23(1):36–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camprodon-Rosanas E, Ribas-Fitó N, Batlle-Vila S, Persavento C, Alvarez-Pedrerol M, Sunyer J, Forns J (2017) Sluggish cognitive tempo: sociodemographic, behavioral, and clinical characteristics in a population of Catalan school children. J Atten Disord 21(8):632–641 [DOI] [PubMed] [Google Scholar]
- Carlson CL, Mann M (2002) Sluggish cognitive tempo predicts a different pattern of impairment in the attention deficit hyperactivity disorder, predominantly inattentive type. J Clin Child Adolesc Psychol 31(1):123–129 [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Molina BS, Pelham WE, Applegate B, Dahlke A, Overmyer M, Lahey BB (2010) Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 67(10):1044–1051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A (2003) Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 60(8):837–844 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Thomas SA, Swan AJ, Ehrlich KB, Reynolds EK, Suarez L, Pabón SC (2012) It depends on what you mean by ‘disagree’: differences between parent and child perceptions of parent–child conflict. J Psychopathol Behav Assess 34(3):293–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Mar Bernad M, Servera M, Becker SP, Burns GL (2016) Sluggish cognitive tempo and ADHD inattention as predictors of externalizing, internalizing, and impairment domains: a 2-year longitudinal study. J Abnorm Child Psychol 44(4):771–785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards G, Barkley RA, Laneri M, Fletcher K, Metevia L (2001) Parent–adolescent conflict in teenagers with ADHD and ODD. J Abnorm Child Psychol 29(6):557–572 [DOI] [PubMed] [Google Scholar]
- Erhardt D, Hinshaw SP (1994) Initial sociometric impressions of attention-deficit hyperactivity disorder and comparison boys: predictions from social behaviors and from nonbehavioral variables. J Consult Clin Psychol 62(4):833. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Pelham WE Jr, Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM, Burrows-MacLean L (2006) A practical measure of impairment: psychometric properties of the impairment rating scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. J Clin Child Adolesc Psychol 35(3):369–385 [DOI] [PubMed] [Google Scholar]
- Fischer M, Barkley RA, Fletcher KE, Smallish L (1993) The stability of dimensions of behavior in ADHD and normal children over an 8-year followup. J Abnorm Child Psychol 21(3):315–337 [DOI] [PubMed] [Google Scholar]
- Fraser A, Cooper M, Agha SS, Collishaw S, Rice F, Thapar A, Eyre O (2018) The presentation of depression symptoms in attention-deficit/hyperactivity disorder: comparing child and parent reports. Child Adolesc Mental Health 23(3):243–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE (1998) Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol 107(1):128. [DOI] [PubMed] [Google Scholar]
- Hartman CA, Hox J, Mellenbergh GJ, Boyle MH, Offord DR, Racine Y, Sergeant JA (2001) DSM-IV internal construct validity: when a taxonomy meets data. J Child Psychol Psychiatry 42:817–836 [DOI] [PubMed] [Google Scholar]
- Hartman CA, Willcutt EG, Rhee SH, Pennington BF (2004) The relation between sluggish cognitive tempo and DSM-IV ADHD. J Abnorm Child Psychol 32:491–503 [DOI] [PubMed] [Google Scholar]
- Hayes AF, Matthes J (2009) Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behav Res Methods 41(3):924–936 [DOI] [PubMed] [Google Scholar]
- Herman KC, Ostrander R (2007) The effects of attention problems on depression: developmental, academic, and cognitive pathways. School Psychol Quart 22(4):483 [Google Scholar]
- Herman KC, Lambert SF, Ialongo NS, Ostrander R (2007) Academic pathways between attention problems and depressive symptoms among urban African American children. J Abnorm Child Psychol 35(2):265–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoza B, Gerdes AC, Mrug S, Hinshaw SP, Bukowski WM, Gold JA, Greenhill LL (2005) Peer-assessed outcomes in the multimodal treatment study of children with attention deficit hyperactivity disorder. J Clin Child Adolesc Psychol 34(1):74–86 [DOI] [PubMed] [Google Scholar]
- Humphreys KL, Katz SJ, Lee SS, Hammen C, Brennan PA, Najman JM (2013) The association of ADHD and depression: mediation by peer problems and parent–child difficulties in two complementary samples. J Abnorm Psychol 122(3):854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen PS, Rubio-Stipec M, Canino G, Bird HR, Dulcan MK, Schwab-Stone ME, Lahey BB (1999). Parent and child contributions to diagnosis of mental disorder: are both informants always necessary? J Am Acad Child Adolesc Psychiatry 38(12):1569–1579 [DOI] [PubMed] [Google Scholar]
- Johnson PO, Neyman J (1936) Tests of certain linear hypotheses and their application to some educational problems. Stat Res Mem 1:57–93 [Google Scholar]
- Kent KM, Pelham WE Jr, Molina BS, Sibley MH, Waschbusch DA, Yu J, Karch KM (2011) The academic experience of male high school students with ADHD. J Abnorm Child Psychol 39(3):451–462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khadka G, Burns GL, Becker SP (2016) Internal and external validity of sluggish cognitive tempo and ADHD inattention dimensions with teacher ratings of Nepali children. J Psychopathol Behav Assess 38:433–442. 10.1007/s10862-015-9534-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Dougherty LR, Olino TM (2005) Toward guidelines for evidence-based assessment of depression in children and adolescents. J Clin Child Adolesc Psychol 34(3):412–432 [DOI] [PubMed] [Google Scholar]
- Larson R, Richards MH (1991) Daily companionship in late childhood and early adolescence: changing developmental contexts. Child Dev 62(2):284–300 [DOI] [PubMed] [Google Scholar]
- Larson K, Russ SA, Kahn RS, Halfon N (2011) Patterns of comorbidity, functioning, and service use for US children with ADHD, 2007. Pediatrics 127:462–470. 10.1542/peds.2010-0165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laursen B, Coy KC, Collins WA (1998) Reconsidering changes in parent–child conflict across adolescence: a meta-analysis. Child Dev 69(3):817–832 [PMC free article] [PubMed] [Google Scholar]
- Lee S, Burns GL, Snell J, McBurnett K (2014) Validity of the sluggish cognitive tempo symptom dimension in children: sluggish cognitive tempo and ADHD-inattention as distinct symptom dimensions. J Abnorm Child Psychol 42(1):7–19 [DOI] [PubMed] [Google Scholar]
- Meinzer MC, Lewinsohn PM, Pettit JW, Seeley JR, Gau JM, Chronis-Tuscano A, Waxmonsky JG (2013) Attention–deficit/hyperactivity disorder in adolescence predicts onset of major depressive disorder through early adulthood. Depress Anxiety 30(6):546–553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer MC, Pettit JW, Viswesvaran C (2014) The co-occurrence of attention-deficit/hyperactivity disorder and unipolar depression in children and adolescents: a meta-analytic review. Clin Psychol Rev 34(8):595–607 [DOI] [PubMed] [Google Scholar]
- Meinzer MC, Pettit JW, Waxmonsky JG, Gnagy E, Molina BS, Pelham WE (2016) Does childhood attention-deficit/hyperactivity disorder (ADHD) predict levels of depressive symptoms during emerging adulthood? J Abnorm Child Psychol 44(4):787–797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer MC, Hartley CM, Hoogesteyn K, Pettit JW (2018) Development and open trial of a depression preventive intervention for adolescents with ADHD. Cogn Behav Pract 25(2):225–239. 10.1016/j.cbpra.2017.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mick E, Biederman J, Santangelo S, Wypij D (2003) The influence of gender in the familial association between ADHD and major depression. J Nerv Ment Dis 191(11):699–705 [DOI] [PubMed] [Google Scholar]
- Milich R, Balentine AC, Lynam DR (2001) ADHD combined type and ADHD predominantly inattentive type are distinct and unrelated disorders. Clin Psychol Sci Pract 8(4):463–488 [Google Scholar]
- Nijmeijer JS, Minderaa RB, Buitelaar JK, Mulligan A, Hartman CA, Hoekstra PJ (2008) Attention-deficit/hyperactivity disorder and social dysfunctioning. Clin Psychol Rev 28(4):692–708 [DOI] [PubMed] [Google Scholar]
- Ostrander R, Crystal DS, August G (2006) Attention deficit-hyperactivity disorder, depression, and self-and other-assessments of social competence: a developmental study. J Abnorm Child Psychol 34(6):772–786 [DOI] [PubMed] [Google Scholar]
- Pelham WE Jr, Gnagy EM, Greenslade KE, Milich R (1992) Teacher ratings of DSM–III–R symptoms for the disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry 31:210–218. 10.1097/00004583-199203000-00006 [DOI] [PubMed] [Google Scholar]
- Pelham WE Jr, Fabiano GA, Massetti GM (2005) Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. J Clin Child Adolesc Psychol 34(3):449–476 [DOI] [PubMed] [Google Scholar]
- Penny AM, Waschbusch DA, Klein RM, Corkum P, Eskes G (2009) Developing a measure of sluggish cognitive tempo for children: content validity, factor structure, and reliability. Psychol Assess 21(3):380. [DOI] [PubMed] [Google Scholar]
- Peterson RA (2001) On the use of college students in social science research: insights from a second-order meta-analysis. J Consum Res 28:450–461 [Google Scholar]
- Pfiffner LJ, Mikami AY, Huang-Pollock C, Easterlin B, Zalecki C, McBurnett K (2007) A randomized, controlled trial of integrated home-school behavioral treatment for ADHD, predominantly inattentive type. J Am Acad Child Adolesc Psychiatry 46(8):1041–1050 [DOI] [PubMed] [Google Scholar]
- Pillow DR, Pelham WE, Hoza B, Molina BSG, Stultz CH (1998) Confirmatory factor analyses examining attention deficit hyperactivity disorder symptoms and other childhood disruptive behaviors. J Abnorm Child Psychol 26:293–309. 10.1023/A:1022658618368 [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Borelli JL, Cheah CS, Simon VA, Aikins JW (2005) Adolescent girls’ interpersonal vulnerability to depressive symptoms: a longitudinal examination of reassurance-seeking and peer relationships. J Abnorm Psychol 114(4):676. [DOI] [PubMed] [Google Scholar]
- Reinherz HZ, Giaconia RM, Hauf AMC, Wasserman MS, Silverman AB (1999) Major depression in the transition to adulthood: risks and impairments. J Abnorm Psychol 108(3):500. [DOI] [PubMed] [Google Scholar]
- Robin AL, Foster SL (1989) Negotiating parent–adolescent conflict: a behavioral-family systems approach. Guilford Press, New York [Google Scholar]
- Sebastian C, Viding E, Williams KD, Blakemore SJ (2010) Social brain development and the affective consequences of ostracism in adolescence. Brain Cogn 72(1):134–145 [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME (2000) NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry 39:28–38 [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Alpert A, Davis B, Andrews J (1997) Family support and conflict: prospective relations to adolescent depression. J Abnorm Child Psychol 25(4):333–344 [DOI] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Molina BSG, Gnagy EM, Waschbusch DA, Karch KM (2012a) Diagnosing ADHD in adolescence. J Consult Clin Psychol 80:139–150. 10.1037/a0026577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE Jr, Molina BS, Gnagy EM, Waxmonsky JG, Waschbusch DA, Kuriyan AB (2012b) When diagnosing ADHD in young adults emphasize informant reports, DSM items, and impairment. J Consult Clin Psychol 80(6):1052–1061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Altszuler AR, Morrow AS, Merrill BM (2014) Mapping the academic problem behaviors of adolescents with ADHD. School Psychol Quart 29(4):422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Campez M, Perez A, Morrow AS, Merrill BM, Altszuler AR, Yeguez CE (2016) Parent management of organization, time management, and planning deficits among adolescents with ADHD. J Psychopathol Behav Assess 38:216–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ZR, Eadeh HM, Breaux RP, Langberg JM (2018) Sleepy, sluggish, worried, or down? The distinction between self-reported sluggish cognitive tempo, daytime sleepiness, and internalizing symptoms in youth with attention-deficit/hyperactivity disorder. Psychol Assess 31(3):365–375 [DOI] [PubMed] [Google Scholar]
- Verboom CE, Sijtsema JJ, Verhulst FC, Penninx BW, Ormel J (2014) Longitudinal associations between depressive problems, academic performance, and social functioning in adolescent boys and girls. Dev Psychol 50(1):247. [DOI] [PubMed] [Google Scholar]
- Wechsler D (1999) Wechsler abbreviated scale of intelligence. Pearson, San Antonio [Google Scholar]
- Wechsler D (2009) Wechsler individual achievement test, 3rd edn Psychological Corporation, San Antonio [Google Scholar]
- Wechsler D (2011) WASI-II: wechsler abbreviated scale of intelligence, 2nd edn Pearson, San Antonio [Google Scholar]
- Willcutt EG, Nigg JT, Pennington BF, Solanto MV, Rohde LA, Tan-nock R, Lahey BB (2012) Validity of DSM-IV attention deficit/hyperactivity disorder symptom dimensions and subtypes. J Abnorm Psychol 121:991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeguez CE, Hill RM, Buitron V, Pettit JW (2018) Stress accounts for the association between ADHD symptoms and suicide ideation when stress-reactive rumination is high. Cognit Ther Res 42:461–467 [Google Scholar]
- Young JF, Mufson L (2008) Interpersonal psychotherapy for treatment and prevention of adolescent depression In: Abela JRZ, Hankin BL (eds) Handbook of depression in children and adolescents. Guilford Press, New York, pp 288–306 [Google Scholar]