Abstract
Patient: Male, 17-year-old
Final Diagnosis: Ganglioneuroma
Symptoms: Incidental
Medication: —
Clinical Procedure: CT scan
Specialty: Radiology
Objective:
Unusual clinical course
Background:
Ganglioneuroma is a rare benign sympathetic chain neoplasm which rarely arise from the adrenal gland in adults and exceedingly rare for ganglioneuroma to arise from different origins in the same patient. We present a rare case of retroperitoneal ganglioneuroma concurring with an adrenal ganglioneuroma in an adult patient.
Case Report:
A 17-year-old healthy male underwent computed tomography (CT) scan after road traffic accident where he was found to have a left adrenal homogeneous hypovascular lesion with another retroperitoneal lesion seen within the right para-colic gutter with similar radiological features. Successful surgical resection was obtained, and histological diagnosis of both lesions was benign ganglioneuroma.
Conclusions:
Adrenal and extra-adrenal ganglioneuroma can, although rare, concur together. Key findings are the similar radiological appearance of the lesions with typical hypovascular progressive pattern of enhancement. Appropriate pre-surgical diagnosis can aid to proper management since ganglioneuroma needs wide surgical resection due to its high chance of recurrence.
MeSH Keywords: Adrenal Glands, Ganglioneuroblastoma, Ganglioneuroma
Background
Ganglioneuroma is a rare benign neuro-endocrine neoplasm that composes of ganglion cells, neurites, Schwann cells, and fibrous tissues. It originates from the sympathetic neural crest which is found within the sympathetic ganglia and adrenal gland [1]. These neoplasms are usually non-functioning in contrast to their main differential diagnosis; ganglioneurblastoma and paraganglioma [2].
The most common location is the posterior mediastinum (41.5%) followed by the retroperitoneal space (37.5%) including the adrenal glands (21%), other less common locations are in the neck (8%) where few case reports of a retropharyngeal ganglioneuroma where reported [3,4].
Combined adrenal ganglioneuroma and extra adrenal ganglioneuroma is extremely rare where only 1 case has been reported in the literature [5].
We reported a case of combined adrenal and extra-adrenal retroperitoneal ganglioneuroma presenting as incidentalomas.
Case Report
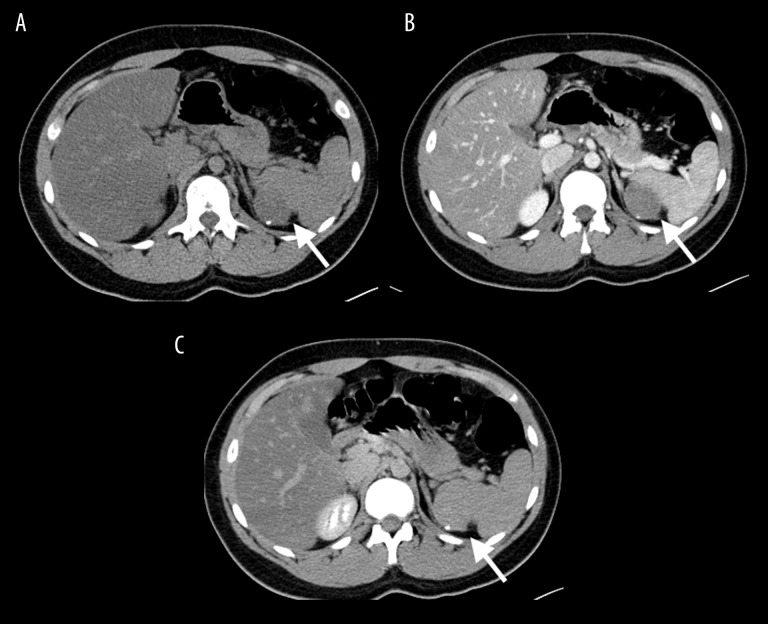
A 17-year-old healthy male underwent computed tomography (CT) scan of the abdomen and pelvis after a road traffic accident (RTA). Fortunately, the CT yielded no trauma related injuries. However, the patient was found to have a left adrenal lesion with another lesion seen in the retroperitoneal space adjacent to the cecum within the right paracolic gutter. Both lesions showed similar radiological features in which both were well defined, homogeneous and hypo-vascular with progressive pattern of enhancement. The larger lesion was located in the left adrenal gland and showed peripheral tiny calcifications. It was measuring 3.7×4 cm. The right retroperitoneal lesion measured 1.8×2.8 cm. The trauma protocol CT scan utilized in our hospital composes of 70 sec venous phase and 2 min delayed phase. The lesions were showing attenuation values of 46 and 64 HU on the venous and delayed phases for the adrenal lesion respectively (Figure 1). The left para-colic lesion showed 40 and 51 HU on the venous and delayed phases respectively (Figure 2).
Figure 1.
(A–C) Axial computed tomography (CT) scan at the level of the left adrenal obtained in (A) pre-contrast (B) venous phase and (C) excretory phase illustrating the left adrenal ganglioneuroma (arrow) which is homogeneous and shows progressive pattern of enhancement. Note the peripheral calcific nodule.
Figure 2.
(A–C) Axial computed tomography (CT) scan obtained in (A) pre contrast (B) venous phase and (C) excretory phase illustrating the right parabolic gutter ganglioneuroma (arrow). Note its homogeneous attenuation and progressive pattern of enhancement.
The initial differential diagnosis were neurogenic tumors such as ganglioneuroma because of the progressive enhancement pattern. Another differential diagnosis was granulomatous infection because of the presence of calcifications. A 3-month follow-up study was performed in pre-contrast, venous, and delayed phases. The lesions show interval stability in size and enhancement pattern. The only additional feature that was obtained from the follow-up scan was the pre-contrast HU attenuation values which were 26 and 28 HU for the adrenal and the retroperitoneal lesion respectively.
Both masses were laparoscopically excised utilizing 3 ports; left mid-clavicular, supra-umbilical and left anterior clavicular line for excision of the right parabolic gutter mass. The later was adjusted into a left lateral position port and the left adrenal mass was 360 degrees separated with vascular contents. Routine tissue closure was achieved, and surgery went uneventful. The patent was discharged on the 3rd day post-operation with no complications.
Gross pathology examination of both masses showed white tan firm nodules. Histopathological assessment revealed that both lesions showed Schwannian rich stroma containing ganglion cells in different maturation stages in keeping with ganglioneuromal neoplasm. No neoplastic component was found in either specimens.
Discussion
Ganglioneuroma is a benign neoplasm originating from ganglion cells of the sympathetic chain along with other tumors including neuroblastomas and ganglioneuroblastomas, where they compose of variable degrees of immaturity and malignant behavior [3].
The most common location of ganglioneuroma is the mediastinum followed by the aortocaval sympathetic ganglia within the retroperitoneal space. Less frequently, ganglioneuroma can arise in the adrenals, and affect primarily pediatric patients and young adults [3,6].
Combination of adrenal and extra-adrenal ganglioneuroma is extremely rare in which only one case was reported by Sucandy et al. describing a combination of adrenal and retroperitoneal ganglioneuroma arising from the retro-pancreatic space in a 50-year-old male [5]. Our case share comparable locations involving the adrenal and retroperitoneal space. However, in our case, ganglioneuroma was arising from the left adrenal gland and the other lesion was arising from the contra-lateral retroperitoneal space particularly within the para colic gutter while the aforementioned case report described a left adrenal ganglioneuroma with concurring midline retroperitoneal ganglioneuroma. Another slight incongruity was the hormonal inactivity that was presented in our case. Sucandy et al. addressed mildly elevated vanillyl mandelic acid (VMA) but a normal 24-hour catecholamine, metanephrine and cortisol levels.
Thorough review of the literature showed that most of ganglioneuromas are hormonally inactive. However, this feature could not be utilized as a differential tool between ganglioneuroma and their main differentials; ganglioneuroblastoma and neuroblastoma since ganglioneuroma had been reported to be hormonally active as well [5].
Adrenal ganglioneuromas are most commonly diagnosed indecently as showed by the largest study on adrenal ganglioneuroma carried by Xie et al. [7]. This study was done on 42 cases and showed incidental detection rate of 75%. Xie et al. concluded that 62.2% of ganglioneuromas were homogeneous [7]. Calcifications were present in 33.3% of cases [7], which are consistent finding with our study. Another important distinctive feature was the progressive enhancement nature of the tumor. Post contrast venous phase attenuation values in the Xie et al. study were 30–54 HU and 40–70 HU in the excretory phase [7]. We had comparable attenuation values: 46 versus 40 HU) and (50 versus 64 HU) in the venous phase and excretory phase respectively.
Malignant degeneration is rare but can present especially in tumors that are penetrating through the neural foramen into the spinal canal and being dumbbell in shape where the risk of transforming into malignant peripheral nerve sheath tumor is high [8].
Laparoscopic resection carries excellent prognosis. However, risk of recurrence after resection is still evident [9,10].
Conclusions
Ganglioneuroma arising from the adrenal gland in adult has been frequently described lately and concurrence with other ganglioneuromas from different origins is now possible as this is the second reported case in the literature. Homogeneous masses that show progressive enhancement and arise along the expected sympathetic chain are highly suggestive of ganglioneuroma even when multiple.
Footnotes
Conflict of interests
None.
References:
- 1.Georger B, Hero B, Harms D, et al. Metabolic activity and clinical features of primary ganglioneuroma. Cancer. 2001;91(10):1905–13. doi: 10.1002/1097-0142(20010515)91:10<1905::aid-cncr1213>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 2.Bove KE, McAdams AJ. Composite ganglioneuroblastoma. Arch Pathol Lab Med. 1981;105:325–30. [PubMed] [Google Scholar]
- 3.Linos D, Tsirlis T, Kapralou A, et al. Adrenal ganglioneuromas: Incidentalomas with misleading clinical and imaging features. Surgery. 2011;149(1):99–105. doi: 10.1016/j.surg.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 4.Yang A, Ozsvath J, Shukla P, Fatterpekar GM. Retropharyngeal ganglioneuroma: A case report. J Neuroimaging. 2013;23(4):537–39. doi: 10.1111/j.1552-6569.2012.00765.x. [DOI] [PubMed] [Google Scholar]
- 5.Sucandy I, Akmal YM, Sheldon DG. Ganglioneuroma of the adrenal gland and retroperitoneum: A case report. N Am J Med Sci. 2011;3:336–38. doi: 10.4297/najms.2011.3336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lonergan GJ, Schwab CM, Suarez ES, Carlson CL. Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: Radiologic-pathologic correlation. Radiographics. 2002;22:911–34. doi: 10.1148/radiographics.22.4.g02jl15911. [DOI] [PubMed] [Google Scholar]
- 7.Xie J, Dai J, Zhou WL, Sun FK. Adrenal ganglioneuroma: Features and outcomes of 42 cases in a Chinese population. World J Surg. 2018;42(8):2469–75. doi: 10.1007/s00268-018-4499-8. [DOI] [PubMed] [Google Scholar]
- 8.De Chadarevian JP, MaePascasio J, Halligan GE, et al. Malignant peripheral nerve sheath tutor arising from an adrenal ganglioneuroma in a 6-year-old boy. Pediatr Dev Pathol. 2004;7:277–84. doi: 10.1007/s10024-004-8084-9. [DOI] [PubMed] [Google Scholar]
- 9.Ruiz-Tovar J, Gamallo-Amat C. [Laparoscopic excision of retroperitoneal ganglioneuroma through anterior transperitoneal approach] Cir Cir. 2012;80:274–77. [in Spanish] [PubMed] [Google Scholar]
- 10.Retrosi G, Bishay M, Kiely EM, et al. Morbidity after ganglioneuroma excision: Is surgery necessary? Eur J Pediatr Surg. 2011;21:33–37. doi: 10.1055/s-0030-1263195. [DOI] [PubMed] [Google Scholar]