Abstract
Most children with sickle cell disease (SCD) today survive into adulthood. Among emerging adults, there is a marked increase in acute care utilization and a rise in mortality, which can be exacerbated by not establishing or remaining in adult care. Health care transition programs are therefore essential to prepare, transfer, and integrate emerging adults in the adult care setting. The Six Core Elements of Health Care Transition, created by the Center for Health Care Transition Improvement, define the basic components of health care transition support as follows: (1) transition policy, (2) tracking and monitoring progress, (3) assessing transition readiness, (4) planning for adult care, (5) transferring to adult care, and (6) integrating into adult care. Programs that implement the Six Core Elements have experienced significant declines in care abandonment during adolescence and young adulthood and higher early adult care engagement. Most of the core transition activities are not currently reimbursable, however, posing a challenge to sustain transition programs. Ongoing studies are investigating interventions in comparative effectiveness trials to improve health-related quality of life and reduce acute care utilization among emerging adults with SCD. Although these studies will identify best practices for health care transition, it is also important to define how the transition outcomes will be measured, as no consensus definition exists for successful health care transition in SCD. Future research is needed to define best practices for health care transition, systematically assess transition outcomes, and revise payment models to promote sustainability of health care transition programs.
Learning Objectives
Review the evidence of unfavorable health outcomes due to poor transition to the adult care process for individuals with sickle cell disease
Describe the current health care transition models and interventions for adolescents and young adults with sickle cell disease
Describe the components of a health care transition program for emerging adults with sickle cell disease
Clinical case
A 13-year-old girl with sickle cell anemia is seen for a hematology health-maintenance visit. She went lost to follow-up between the ages of 3 and 13 years, and now resumes longitudinal sickle cell care after being referred from an emergency department (ED). The urine dipstick has 3+ protein and the serum creatinine is 0.7 mg/dL. The 24-hour urine discloses proteinuria (5 g/24 hours) and the renal biopsy reveals focal segmental glomerulosclerosis. She initiates lisinopril but fails to refill the prescription when her home supply ends because she and her mother did not understand the directions to refill the medication. She is recommended hydroxyurea but only initiates it at age 14 years after an acute chest syndrome event with acute kidney injury (serum creatinine, 4 mg/dL). Her kidney function improves but she develops hypertension. She initiates chronic transfusions and hydroxyurea is discontinued. Over the subsequent 4 years, she receives monthly transfusions, albeit missing appointments and averaging transfusions once every 5 to 6 weeks. She initiates subcutaneous deferoxamine and labetalol and continues lisinopril, all with suboptimal adherence. At age 18 years, an appointment with an adult provider is made. Her laboratory results disclose: a microalbumin-to-creatinine ratio of 1684 mg/g of creatinine and a diethylenetriaminepentaacetic acid clearance estimated glomerular filtration rate of 70 mL/min/1.73 m2. She fails to attend the first adult visit and is lost to follow-up for 18 months during which time she did not receive her medication or monthly transfusions. At age 20 years, she presents to the ED with chronic pain, hyperkalemia, and an estimated glomerular filtration rate of 24 mL/min/1.73 m2. She receives urgent hemodialysis and continues monthly hemodialysis treatment.
Survival of sickle cell disease
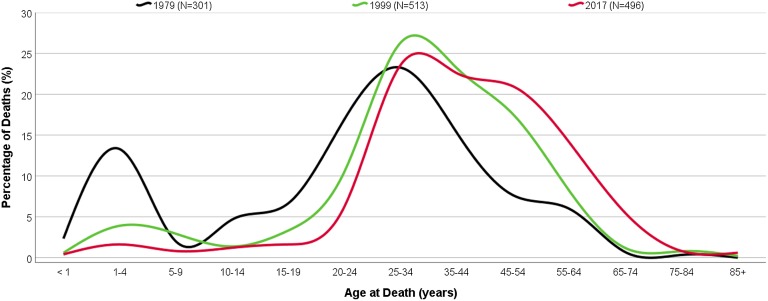
Survivorship into adulthood for children with sickle cell disease (SCD) has increased to >95% by age 18 years,1 and is attributed to newborn screening implementation, penicillin prophylaxis, primary stroke prevention, and disease-modifying therapies. This progress has resulted in a change in the pattern of mortality over the past almost 50 years. Age of death for individuals with SCD changed from a bimodal pattern in which a peak in early childhood, and again in adolescence, occurred (1979), to a unimodal one in which deaths in pediatrics became rare, but began to rise during young adulthood years (2017) (Figure 1). However, the peak in mortality among adults has not changed in the last 50 years (Figure 1) and, today, they continue to die an average of 20 years sooner than their race-matched counterparts.2
Figure 1.
Proportion of deaths among individuals with SCD by age group. Adapted from Hassell1 (source: wonder.cdc.gov) with permission.
The adolescence-to-adulthood gap
With increased survivorship, an important time for youth with SCD is the transition period from pediatric to adult life, when continued support is needed to ensure continuity of care. Health care transition is defined as “the purposeful, planned movement of adolescents and young adults with chronic physical and medical conditions from child-centered to adult-oriented health care systems.”3(p. 570) Health care transition comprises 3 phases: transition preparation, transfer, and adult care integration.4 Transfer comprises the act of changing from a pediatric to an adult-centered care model, whereas transition refers to the entire period of preparation, transfer, and integration into adult care.
Among individuals with SCD, a rise in mortality occurs in the early young adulthood years (ages 20 to 24 years) (Figure 1), coinciding with the period in which they leave pediatric care. During this period, acute care utilization rises, and a subset of patients demonstrates increased disease severity during the transfer period.5 Not only is the transfer period a high-risk time for poor health outcomes, but it is also costly to the health system. In 2011, up to $45 billion dollars were spent mitigating poor transition outcomes in the United States.6 Like SCD, increasing numbers of children and youth with special health care needs are surviving into adulthood. As of 2015, over one-half of individuals living with cystic fibrosis (CF) were adults, in contrast to <30% in 1986.7 However, contrasting with SCD, the Cystic Fibrosis Foundation mandates establishment of adult-centered care when a CF program has ≥40 patients aged ≥18 years. Additionally, a national registry of CF exists, allowing tracking of transition outcomes. According to the national CF registry, the mean age of transfer to adult care is 21 years, and there is a lesser decline in the forced expiratory volume in 1 second among those who transfer to an adult provider vs those remaining in pediatric care.8 Thus, it is imperative that more research and effort are focused on improving the health care transition resources for individuals with SCD, including better monitoring of the entire transition process.
Why does transition to adult care fail?
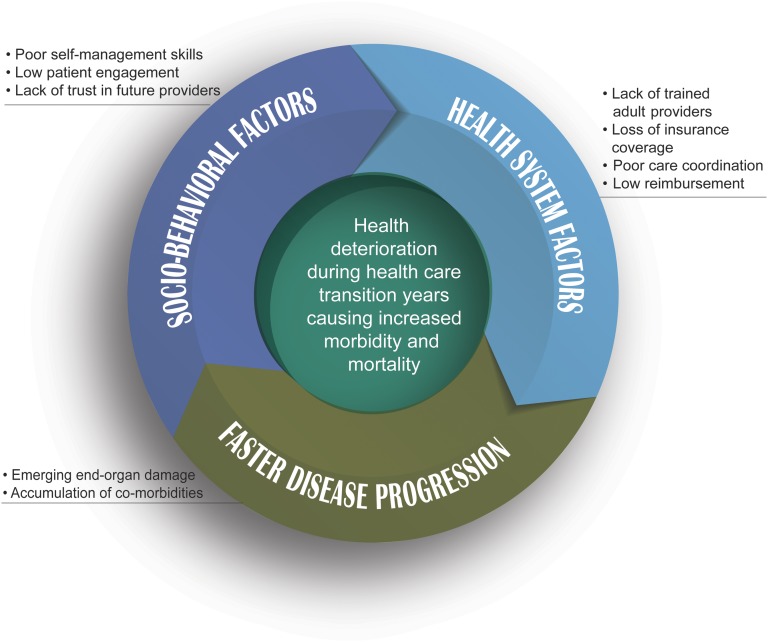
There are several barriers to health care transition. Health system barriers such as lack of specialized and interested providers, challenges in care coordination across pediatric and adult health systems, and losses in health coverage can all impact patients’ continuity of care and ultimately their management of the disease. Patient-level factors such as cognitive-functioning deficits, lack of preparedness, including disease knowledge and self-efficacy skills, and comorbidities (eg, depression, anxiety) are additional barriers that may affect patients’ ability to use self-management skills consistently and effectively.9 Studies have explored stakeholder perceptions about health care transition. Adolescents with SCD and caregivers have reported concerns about care delivered in the ED, appropriately communicating medical needs when in pain, need for transferring responsibility of disease management from caregiver to patient, and expectations about the differences between pediatric- and adult-centered care.10 Young adults with SCD have raised similar concerns, with a focus on negative experiences and stigma in adult care.11 Patients may be less likely to engage with the adult system due to poor experiences in the ED and unsatisfactory working relationships with adult providers, leading them to manage disease complications at home, thereby delaying receipt of necessary care. Collectively, these barriers result in poor transition outcomes, which in addition to disease progression, lead to health deterioration during the health care transitional years (Figure 2).
Figure 2.
Health deterioration multifactorial model during health care transition years for young adults with SCD.
The social-ecological model of adolescent and young adult readiness for transition (SMART) is a framework for understanding barriers as preexisting factors (eg, sociodemographic, medical status) and modifiable factors (eg, knowledge, skills, psychosocial functioning) that can impact the transition process and identifying targets for intervention.12 Other conceptual frameworks for transition suggested for SCD include the bioecological systems theory, which identifies the impact of environmental systems and SCD diagnosis, and the transtheoretical stages of change model, which identifies an individual’s level of readiness to engage in healthy behaviors.13
National standards and outcome measures for health care transition
Professional organizations have recognized the importance of health care transition. The American Academy of Pediatrics, American Academy of Family Physicians, and the American College of Physicians were the first to develop an expert opinion and consensus statement on effective transition.14 Later, a national initiative on health care transition, the National Alliance to Advance Adolescent Health, in partnership with the Maternal and Child Health Bureau, created the Got Transition/Center for Health Care Transition Improvement. Got Transition has defined the basic components of health care transition support through the development of the Six Core Elements of Health Care Transition. The Six Core Elements serve as a framework for transition programs and comprise: (1) creating a transition policy, (2) tracking and monitoring progress, (3) assessing transition readiness, (4) planning for adult care, (5) transferring to adult care, and (6) integrating into adult care (https://www.gottransition.org). The Six Core Elements have been tested in quality improvement projects and customized to different care settings, including subspecialties.15 An SCD transition policy statement has also been issued by the Association of Pediatric Hematology/Oncology Nurses and the American Society of Pediatric Hematology Oncology, and recommends: early discussion of transition; collaboration among patients, families, and providers to create the transition plan; annual transition readiness assessment; and communication between pediatric and adult providers during transfer of care.16 Additionally, the American Society of Hematology has developed a transition toolkit for SCD that provides disease-specific instruments that can be used during the transition process (https://www.hematology.org/clinicians/priorities/5573.aspx). Finally, increasing the proportion of youth with special health care needs whose health care provider has discussed transition planning from pediatric to adult health care is one of the Healthy People 2020 goals (https://www.healthypeople.gov/node/4153/data_details).
Currently, there is no established metric for successful health care transition. In the few studies attempting to address transition outcomes, outcomes were simplified, and have examined pre- and posttransition SCD knowledge,17 completion of an initial visit to an adult care provider,18 and satisfaction with the transition process.19 An SCD retrospective analysis found that during a 5-year time period, 32% of patients did not complete the adult transfer, and those at highest risk were patients with HbSC (compound heterozygous sickle and C hemoglobin) or HbSβ+ (compound heterozygous sickle and β thalassemia plus) thalassemia not on chronic transfusions and who lived >20 miles from the adult center.20 Studies have not examined psychosocial factors such as emotional and behavioral functioning, resilience, and health-related quality of life (HRQOL), all aspects that may impact transition. Providers have examined which transition outcomes were most meaningful, including health care utilization, HRQOL, and stable disease trajectory, providing guidance on possible outcome measures for health care transition.21
Health care transition interventions
There is limited evidence on the efficacy of health care transition interventions. Best practices, using care guidelines and evidence-based interventions, should drive the development and implementation of health care transition strategies. Additionally, the triple-aim framework should guide the development and outcome measurement for these interventions, whereby population health (eg, reduction of ED reliance), consumer experience (eg, satisfaction with the transition process), and cost of care should all be considered.22 In general, health care transition interventions and models can be divided into those focusing on individual Six Core Elements of Health Care Transition (single Element Core–based interventions) or multiple Core Elements, comprising a comprehensive health care transition model of care.4 In other chronic diseases, most of the interventions in health care transition have focused on the transfer period, rather than the entire range of the transition years.23 By contrast, in SCD, most interventions have focused on transition readiness assessment and transition planning (Table 1). Furthermore, health care transition interventions have incorporated technology and have used mobile Health (mHealth) to increase self-management, including medication adherence and increase access to personal medical history.24-26 To date, only 1 transition to adult care program for SCD has reported its results utilizing all Six Core Elements of Health Care Transition: the Transition Intervention Program from Virginia Commonwealth University.27 Although only a small sample of patients was reported to have completed this program (N = 37), all patients completed a first visit with the adult provider (an improvement from 50% preprogram), and 78% of them have remained in adult care, although the time frame for adult care retention was not provided.
Table 1.
Health care transition interventions for SCD according to the Six Core Elements of Health Care Transition
| Six Core Elements of Health Care Transition with intervention description |
|---|
| 1. Transition policy (informs youth of timing and upcoming process for transition) |
| 2. Tracking and monitoring transition progress |
| 3. Transition readiness/self-care assessment |
| Non–disease-specific instruments |
| Successful Transition to Adulthood with Therapeutics (STARx; parent and child forms)35 |
| Adolescent autonomy checklist36 |
| Newest vital sign37 (measures health literacy) |
| Transition Readiness Assessment Questionnaire (TRAQ)30 |
| Disease-specific instruments |
| Disease knowledge and self-management (adapted to SCD from the National Hemophilia Foundation Transition guidelines)38 |
| Transition Intervention Program (TIP)–Readiness for Transition (TIP-RFT)39 |
| Self-administered Sickle Cell Transition Intervention Program skills checklists40 |
| American Society of Hematology (ASH) transition toolkit* |
| 4. Transition planning (develop individualized transition plans, prepare individual, identify provider) |
| Problem-solving education (cognitive-behavioral intervention that teaches problem-solving skills as a way to cope with life stressors): acceptability demonstrated through focus groups41 |
| Skill-based educational handout (educational handouts provided in clinic and informed by items flagged in the readiness assessment as “needs practice”)42 |
| Music therapy (music therapy–based intervention to increase disease knowledge, self-efficacy, clinic attendance, and reduce ED visits): disease knowledge improved, and patients reported satisfaction with intervention43 |
| Education in clinic using hand-held device (general disease education, healthy living, general career and vocation guidance): found to improve disease knowledge17 |
| SCD-Plane (individualized transition plan informed by neuropsychological testing): used to inform academic planning and local services44 |
| SCD-specific web-based portal (designed to improve communication with providers, improve decision-making, facilitate access to laboratory results and scheduling): shown to be feasible, acceptable, and improve patient-provider communication, but not decision-making45 |
| iManage, a prototype app designed to promote self-management skills: rated as feasible and beneficial by SCD users26 |
| Chronic Disease Self-Management Program (a 6-week group-based intervention led by lay leaders with a chronic health condition): increased self-efficacy, but not disease-specific self-efficacy46 |
| Education about sickle cell heredity (in-clinic sessions by a health educator): feasibility and increased knowledge demonstrated28 |
| Personal health record education (tool used to increase knowledge of personal medical history given in clinic by social workers): shown to be feasible and able to identify areas of gap in medical history knowledge29 |
| 5. Transfer of care/initial adult provider visit (schedule of first adult visit, transfer of medical records, care for patient until first adult visit completed, confirm adult visit completed) |
| Visit of adult provider facilities prior to leaving pediatric care: shown to increase rate of fulfillment of first visit with adult provider18,47 |
| Transition sickle cell clinic with early introduction to adult provider: lower levels of negative affect (fear and sadness) and higher levels of positive affect (serenity and joviality) among youth who participated in the transition clinic compared with adults who did not48 |
| 6. Transition completion/ongoing care/consumer feedback |
| Young adult perspectives of the most important topics to include in transition programming: help in selecting adult provider, seeking emergency care, medication knowledge and medication adherence support, disease education, and being aware of the impact of health behaviors on one’s health11,49 |
| All Six Core Elements of transition described in 1 single program |
| Virginia Commonwealth University’s TIP: a multidisciplinary comprehensive program that begins transition programing and preparation at age 15 years using a curriculum developed by the program members; it measures readiness using the TIP-RFT survey, transfers patients after high school graduation, mostly within the same health system, and tracks patients during integration into adult care27 |
American Society of Hematology pediatric to adult hematologic care transition (https://www.hematology.org/clinicians/priorities/5573.aspx).
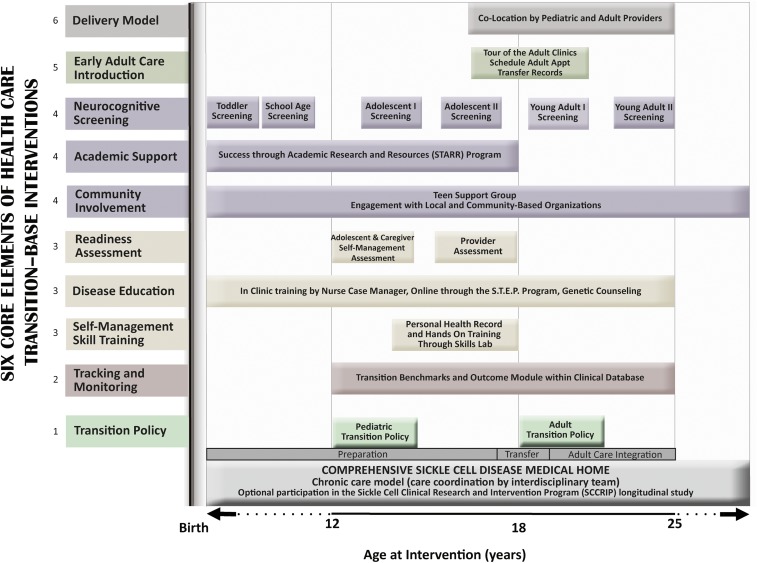
How we approach transition
Since 2007, St. Jude Children’s Research Hospital (St. Jude) has progressively developed and implemented a transitional health care program designed for youth with SCD that is embedded within a medical home and spans the ages of 12 to 25 years (Figure 3). The development and implementation of the program components were informed by suggestions from patients and families during evaluation of the program.10 The program components are presented according to the Six Core Elements of Health Care Transition (Figure 3).
Figure 3.
Map of the St. Jude Transition to Adult Care Program for SCD. Interventions within the program follow the Six Core Elements of Health Care Transition and occur according to age. Numbers next to the interventions correspond to one of the Six Core Elements of transition as follows: (1) transition policy, (2) tracking and monitoring progress, (3) assessing transition readiness, (4) planning for adult care, (5) adult care transfer, and (6) integration into adult care.
Transition policy: age 12 years
A hematology nurse case manager discusses the transition policy with the patient and family at age 12 years. This policy is written at a third-grade reading level and states that preparation for transition will occur from age 12 years until transfer to adult care at age 18 years and is a collaborative effort among the patient, family, and staff (https://www.stjude.org/content/dam/en_US/shared/www/patient-support/hematology-literature/pediatric-transition-policy.pdf).
Transition tracking and monitoring: ages 12 to 25 years
A transition module within our clinical database tracks: (1) transition outcomes, (2) disease-specific knowledge and transition readiness assessment scores, (3) dates of participation in self-management training and early introduction to adult care, (4) dates of last visit in pediatrics, (5) information about the adult provider to whom patient was transferred, (6) dates of first adult visit, and (7) retention in adult care. This database is used to monitor the patients’ progress as they are exposed to the sequential interventions of our program and their outcomes.
Transition readiness: ages 12 to 17 years
To increase transition readiness, semiannual 10- to 15-minute in-clinic disease educational sessions by the adolescent nurse case manager take place using resources developed by our program (https://www.stjude.org/treatment/disease/sickle-cell-disease/educational-resources.html). In-clinic education is supplemented by a web-based learning tool, the Sickle Cell Transition E-Learning Program (STEP) (https://www.stjude.org/treatment/disease/sickle-cell-disease/step-program.html). Topics covered by both education methods include disease manifestations (ie, signs and symptoms of end-organ dysfunction), disease pathophysiology, proper nutrition, exercise, growth and development, and treatment options. Pre- and posteducational test assessments evaluate knowledge retention. A health educator teaches SCD inheritance pattern and the implications of having trait or disease. This counseling session promotes high knowledge-retention rates among adolescents.28 Starting at age 13 years, part of the visit takes place without the parent in the room. Communication skills are further emphasized starting at age 15 years using the personal health record tool. This tool has identified gaps in knowledge, in that adolescents could report their correct sickle genotype and major disease complications (eg, stroke), but had limited knowledge about treatment information (eg, hydroxyurea dosing).29 Role-play skill training is offered during the Skills Laboratory, an activity that models medically necessary habits for transition.10 During the Skills Laboratory, adolescents receive practice training on insurance benefits, pharmacy readiness, and appointment scheduling. All educational activities are operationalized through age-based care plans (https://www.stjude.org/content/dam/en_US/shared/www/patient-support/hematology-literature/plan-of-care-visits.pdf).
To assess readiness, at ages 15 and 17 years, patients and caregivers complete the Self-Management Skills Checklist, a transition readiness assessment adapted from the Transition Readiness Assessment Questionnaire30 that assesses perceived adolescent SCD knowledge and self-management skills. Additionally, at age 17 years, transition readiness is assessed by the transition team using a new instrument that measures readiness in 4 domains: medical, academic, psychosocial, and emotional.31
Transition preparation and planning: ages 12 to 17 years
Cognitive deficits may occur as potential complications from ischemic brain damage in SCD.32 A 2-hour assessment of neurobehavioral skills is therefore completed at age 12 years by a pediatric neuropsychologist, and again repeated at ages 16, 19, and 25 years. Testing assesses intellectual ability, attention, executive functioning, processing speed, verbal memory, and visual motor integration, all areas in which youth with SCD may experience deficits. The results of these screening tests are used to identify those who require additional psychological assessment, to assist with academic planning, and to tailor future disease transition planning. Between the ages of 12 and 14 years, the social worker introduces the concept of self-advocacy and discusses insurance coverage. As additional support, all adolescents are invited to participate in monthly support groups to discuss personal, medical, and social concerns.
Academic planning.
The academic coordinator (a certified school educator) provides school advocacy and guides parents in federal educational plan enrollment (eg, 504 plan), which provides classroom accommodations and school awareness. Individualized academic management is informed by the neurocognitive assessments and may result in the development of an individualized education plan that includes other interventions, such as a special learning plan, occupational therapy, and speech/language therapy. Finally, an academic interest inventory is administered to gauge academic interests and career goals. In subsequent visits, the academic coordinator utilizes the results of the interest inventory, neurocognitive assessments, and academic performance to plan postsecondary life (eg, Job Corps, college enrollment, vocational programs).
Review and update of transition plan and preparation for adult care.
At age 17 years, care coordination switches from the adolescent nurse case manager to the transition nurse case manager, who coordinates care until age 25 years. Informed by the readiness assessments and neurocognitive testing, individualized action plans are put in place between ages 17 and 25 years.
Transfer of care: ages 17 to 18 years
At age 17 years, patients are introduced to adult medical homes through participation in the Transition Tour Program. Pilot data have shown significantly higher rates of matriculation into adult care among Tour Program participants vs nonparticipants.18 Health care is transferred to the adult care setting of choice at age 18 years. Patients who are socially or medically unstable are kept in pediatric care until stable enough to transfer. During the last pediatric visit, patients receive a packet that contains a transition certificate, medical summary, thermometer, information about SCD community-based organizations, and the date and address of their first adult appointment. After scheduling the first adult appointment, usually within 3 to 4 weeks from the last pediatric visit, the transition nurse manager sends the patient’s medical summary to the future adult provider. The summary contains information in 4 areas: (1) medical: list of previous and ongoing medical issues, end-organ assessment (eg, brain-imaging studies, pulmonary function tests), schedule of treatment, and evaluations (eg, vaccinations, iron overload and end-organ function assessment); (2) social: description of home life, conservatorship; (3) academic: past performance, plans for postsecondary education, and information about resources; and (4) emotional: mental health and cognitive assessment results and treatment. The transition nurse case manager is present at their first adult visit if the patient choses to receive care at the adult partner program, the Methodist Comprehensive Sickle Cell Center (MCSCC).
Transition completion and integration into adult care
Once transferred to MCSCC, youth are seen in the young adult transition clinic once every 4 months in the first year, and once every 6 months from ages 19 to 25 years. As in the pediatric program, a care plan details the education provided in clinic (https://www.stjude.org/content/dam/en_US/shared/www/patient-support/hematology-literature/plan-of-care-visits.pdf) and progress with gaining disease-specific knowledge is measured through pre- and postassessment tests. During their first visit, the transition policy is provided, and depression screening using Patient Health Questionnaire 9 (PHQ-9) is administered. Every 6 months, the adult social worker discusses insurance benefits, transportation needs, and advance directives. The pediatric and the adult programs colocate care. The psychologist and the transition nurse case manager’s efforts are allocated to both the pediatric and adult programs (∼50% in each). Additionally, from ages 18 to 25 years, patients receive comanaged care by both the new adult provider and the pediatric hematologist. In this colocated model, acute care utilization does not rise during the transition years and greater disease-specific knowledge associates with greater compliance with health-maintenance visits.33 At age 26 years, patients leave the young adult transition clinic and join the pool of older adults. Transition is now considered complete.
Outcomes of the St. Jude Transition to Adult Care Program
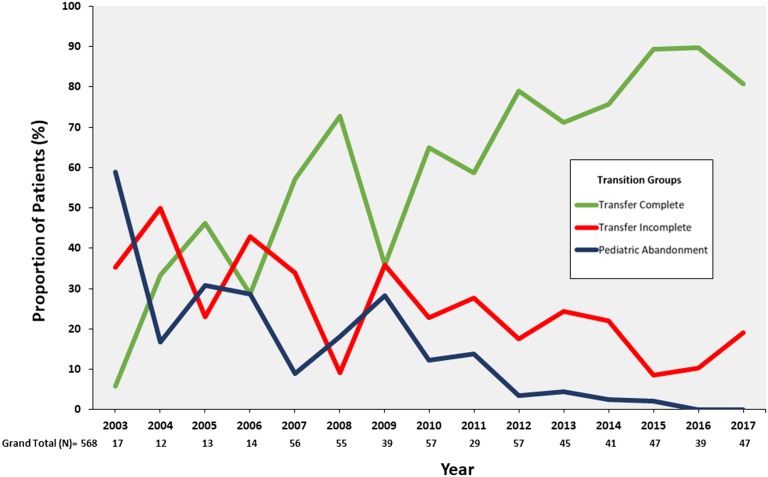
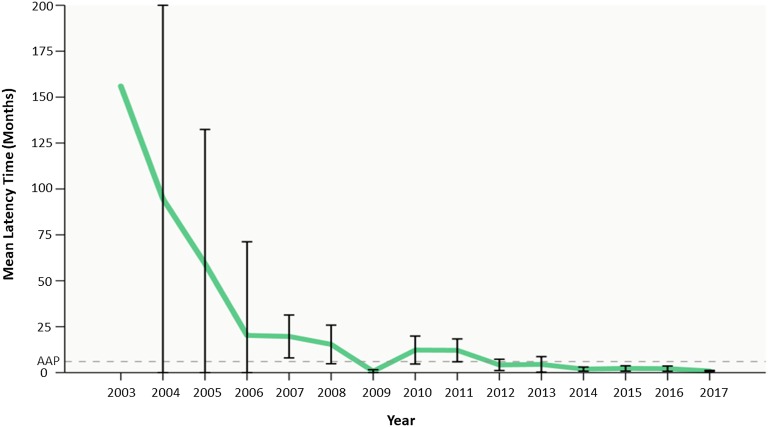
In our program, we track our patients’ transition of outcomes and study them through a lifetime longitudinal cohort study for SCD, the Sickle Cell Clinical Research and Intervention Program (SCCRIP).34 Trends in transition outcomes from program initiation (2007) to data censoring (2017) were analyzed, and transition outcomes from the preprogram period (2003-2006) were compared with those following program implementation (2007-2017). Three trends were analyzed from 2003 to 2017: (1) pediatric care abandonment (discontinuation of pediatric care between ages 12 and 18 years), (2) matriculation to adult care (completion of a first visit with the adult provider after pediatric care), and (3) adult care abandonment (discontinuation of adult care within 12 months from first adult visit). The rates of matriculation to adult care, as well as pediatric and adult care abandonment during and postpediatric care, were compared using linear regression. The frequencies of transition outcomes pre- and posttransition program initiation (2003-2006 vs 2007-2017) were compared with χ2 tests. Latency from pediatric to adult care (the interval between pediatric and adult care) was compared between years with the Mann-Whitney U test. Since the program inception in January 2007, 568 youth (307 boys and 261 girls) with SCD have participated. From 2003 to 2017, there has been a significant decrease in pediatric (β = −2.91; P = .002) and adult care abandonment (β = −1.91; P = .004) (Figure 4). The rate of matriculation to adult care has increased from year to year since the transition program start (β = 4.82; P < .001) (Figure 4). When 469 transition program patients were compared with the 36 pretransition program patients, there was a significant difference in the proportion of patients who matriculated to adult care (78% vs 42%) and those who abandoned care after completion of pediatric care (22% vs 58%; P < .01). Additionally, the median latency between pediatric and adult care decreased from 64 months (range, 0-162 months) pretransition program to 1 month (range, 0-111 months) posttransition program (P < .001; Figure 5).
Figure 4.
Adult care engagement and care abandonment. Since program implementation in 2007, there has been a decrease in the number of patients who have abandoned pediatric care (β = −2.91; P = .002) (blue line), an increase in completion of transition (green line), and an increase in completion of the first visit with the adult provider after leaving pediatric care (β = 4.82; P ≤ .001). A gradual decline in care abandonment (red line) after transfer to adult care is shown from 2003 to 2017 (β = −1.91; P = .004).
Figure 5.
Transfer latency time from pediatric to adult care. With the implementation of the St. Jude Transition to Adult Care Program in 2007, mean latency time to the adult provider after the last visit at St. Jude has significantly decreased, from 64 months (range, 1-162 months) pretransition program to 1 month (range, 0-111 months) posttransition program (P < .001).
Clinical case: transition reimagined
This 13-year-old girl with sickle cell anemia failed to transfer care within the recommended 6-month interval between the pediatric and the adult center care. Additionally, she did not receive adequate preparation during the pediatric years nor did she receive any special support during the transfer and adult care integration phases. Consequently, she disengaged in her care, likely contributing to her poor self-management skills and the faster progression of sickle nephropathy. Ideally, the following should have occurred: (1) enrollment in a transition to adult care program at the age of 13 years when she resumed longitudinal sickle cell care; (2) receipt of sickle cell education and self-management skill-building sessions tailored to her health literacy level (additionally, use of smart phone apps that motivate, send daily reminders, and allow an accountability partner [eg, her mother] to track daily medication intake, could have ensured better medication adherence); (3) during the transfer phase, she could have benefited from the services of a transition coordinator, who helps identify adult providers, remind them of upcoming appointments, and transfers records to the future adult provider (after missing her first adult appointment, having a peer mentor or a community health worker visit her house, reschedule, and accompany her to the appointment could have ensured care continuity); and (4) finally, continued transition services by a transition coordinator during young adulthood years who offered self-management skill-building sessions could have benefited this patient. Regular communications among adult providers (hematologist and nephrologist) through the electronic health record facilitate comanagement, in addition to making their notes visible to the patient through the patient portal, increasing the patient knowledge of her medical history. A structured comprehensive transition program could have afforded this patient care continuity with improved self-efficacy skills and better health outcomes, and could have leveraged digital technology to improve patient care engagement and care coordination.
Conclusions and future directions
The increased survival of children with SCD presents both a challenge and an opportunity. Structured and standardized transition to adult care programs are now priorities. No formally tested evidenced-based comprehensive care delivery model has been reported in SCD, therefore defining the interventions that are efficacious and improve outcomes during transfer and integration into the adult care system is critical. Several individual interventions have been described (Table 1), but their impact on transition outcomes (eg, transfer rates, care engagement) has not been consistently reported, nor has their reproducibility been tested. Currently, 2 Patient-Centered Outcomes Research Institute–funded studies are investigating the effectiveness of different transition interventions: the Sickle Cell Trevor Thompson Transition Project (ST3P-UP; NCT03593395) and Community Health Worker and Mobile Health Programs to Help Young Adults with Sickle Cell Disease Transition to Using Adult Healthcare Services (COMETS; NCT03648710) studies. The ST3P-UP study will randomize 700 patients ages 16 to 25 years to receive standardized transition education and peer support vs standardized transition education alone across 14 sickle cell clinics in North America (https://www.pcori.org/research-results/2017/comparative-effectiveness-peer-mentoring-vs-structured-education-based). The COMETS study will randomize 450 youth with SCD ages ≥17 years to receive guidance form community health workers who have SCD vs the use of the iManage app vs usual care provided by their treating physicians (https://www.pcori.org/research-results/2017/community-health-worker-and-mobile-health-programs-help-young-adults-sickle).
As transition to adult care programs for individuals with SCD are conceptualized, financial support to develop and maintain these programs is imperative. Most of the activities pertaining to care coordination (eg, transfer of records to adult providers) and transition readiness (eg, disease education) are not reimbursable. A fee-for-service model is not designed to support these activities. Alternative models that value the care delivered (ie, value-based initiatives) are urgently needed to financially support all required components of health care transition.
Finally, there is a need for standardization of health care transition outcome measures. Measures of health care utilization, self-management, and HRQOL have all been used as transition outcomes. A consensus on transition outcome measures would facilitate comparison across different interventions and programs. Ideally, these measures should reflect the activities and interventions during the 3 phases of transition (preparation, transfer, and adult care integration) and have patient input.
Acknowledgments
The authors thank the members of the transition to adult care program for their endless commitment and dedication to our patients and their families: Yvonne Carroll, Paul Lavoie, Carrie McIvor, Artangela Henry, Curtis Owens, Kenneth Ataga, Patricia Barker, Timothy Jacobs, Jane Schreiber, Sheila Anderson, Audrey Cole, Shyranda Jones, ToMeisha Conard-Stafford, Latacha Hamilton, and Christy Matthews. The authors are in debt to Katie Stokes and Jason Hodges for preparing the figures and Vikki Nolan for statistical analysis. The authors also thank the administrators at both St. Jude and Methodist University Hospital for their support and trust in their work.
Correspondence
Jane S. Hankins, St. Jude Children’s Research Hospital, 332 Danny Thomas Pl, Mail Stop 800, Memphis, TN 38105; e-mail: jane.hankins@stjude.org.
References
- 1.Hassell KL. Population estimates of sickle cell disease in the U.S. Am J Prev Med. 2010;38(suppl 4):S512-S521. [DOI] [PubMed] [Google Scholar]
- 2.DeBaun MR, Ghafuri DL, Rodeghier M, et al. Decreased median survival of adults with sickle cell disease after adjusting for left truncation bias: a pooled analysis. Blood. 2019;133(6):615-617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blum RW, Garell D, Hodgman CH, et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993;14(7):570-576. [DOI] [PubMed] [Google Scholar]
- 4.White PH, Cooley WC; Transitions Clinical Report Authoring Group; American Academy Of Pediatrics; American Academy Of Family Physicians; American College Of Physicians. Supporting the health care transition from adolescence to adulthood in the medical home [published correction appears in Pediatrics. 2019;143(2)]. Pediatrics. 2018;142(5). [DOI] [PubMed] [Google Scholar]
- 5.Kayle M, Docherty SL, Sloane R, et al. Transition to adult care in sickle cell disease: a longitudinal study of clinical characteristics and disease severity. Pediatr Blood Cancer. 2019;66(1):e27463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burton R. Improving care transitions. Health Affairs (https://www.healthaffairs.org/do/10.1377/hpb20120913.327236/full/). 13 September 2012. Accessed 28 July 2019.
- 7.Goralski JL, Nasr SZ, Uluer A. Overcoming barriers to a successful transition from pediatric to adult care. Pediatr Pulmonol. 2017;52(suppl 48):S52-S60. [DOI] [PubMed] [Google Scholar]
- 8.Tuchman L, Schwartz M. Health outcomes associated with transition from pediatric to adult cystic fibrosis care. Pediatrics. 2013;132(5):847-853. [DOI] [PubMed] [Google Scholar]
- 9.Bemrich-Stolz CJ, Halanych JH, Howard TH, Hilliard LM, Lebensburger JD. Exploring adult care experiences and barriers to transition in adult patients with sickle cell disease. Int J Hematol Ther. 2015;1(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Porter JS, Lopez AD, Wesley KM, et al. Using qualitative perspectives of adolescents with sickle cell disease and caregivers to develop healthcare transition programming. Clin Pract Pediatr Psychol. 2017;5(4):319-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sobota AE, Umeh E, Mack JW. Young adult perspectives on a successful transition from pediatric to adult care in sickle cell disease. J Hematol Res. 2015;2(1):17-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mulchan SS, Valenzuela JM, Crosby LE, Diaz Pow Sang C. Applicability of the SMART model of transition readiness for sickle-cell disease. J Pediatr Psychol. 2016;41(5):543-554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Treadwell M, Telfair J, Gibson RW, Johnson S, Osunkwo I. Transition from pediatric to adult care in sickle cell disease: establishing evidence-based practice and directions for research. Am J Hematol. 2011;86(1):116-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians; Transitions Clinical Report Authoring Group; Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128(1):182-200. [DOI] [PubMed] [Google Scholar]
- 15.Jones MR, Robbins BW, Augustine M, et al. Transfer from pediatric to adult endocrinology. Endocr Pract. 2017;23(7):822-830. [DOI] [PubMed] [Google Scholar]
- 16.Bryant R, Porter JS, Sobota A; Association of Pediatric Hematology/Oncology Nurses; American Society of Pediatric Hematology Oncology. APHON/ASPHO policy statement for the transition of patients with sickle cell disease from pediatric to adult health care. J Pediatr Oncol Nurs. 2015;32(6):355-359. [DOI] [PubMed] [Google Scholar]
- 17.Smith GM, Lewis VR, Whitworth E, Gold DT, Thornburg CD. Growing up with sickle cell disease: a pilot study of a transition program for adolescents with sickle cell disease. J Pediatr Hematol Oncol. 2011;33(5):379-382. [DOI] [PubMed] [Google Scholar]
- 18.Hankins JS, Osarogiagbon R, Adams-Graves P, et al. A transition pilot program for adolescents with sickle cell disease. J Pediatr Health Care. 2012;26(6):e45-e49. [DOI] [PubMed] [Google Scholar]
- 19.Griffin A, Gilleland J, Johnson A, et al. Applying a developmental-ecological framework to sickle cell disease transition. Clin Pract Pediatr Psychol. 2013;1(3):250-263. [Google Scholar]
- 20.Andemariam B, Owarish-Gross J, Grady J, Boruchov D, Thrall RS, Hagstrom JN. Identification of risk factors for an unsuccessful transition from pediatric to adult sickle cell disease care. Pediatr Blood Cancer. 2014;61(4):697-701. [DOI] [PubMed] [Google Scholar]
- 21.Stollon NB, Paine CW, Lucas MS, et al. Transitioning adolescents and young adults with sickle cell disease from pediatric to adult health care: provider perspectives. J Pediatr Hematol Oncol. 2015;37(8):577-583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759-769. [DOI] [PubMed] [Google Scholar]
- 23.Betz CL, O’Kane LS, Nehring WM, Lobo ML. Systematic review: health care transition practice service models. Nurs Outlook. 2016;64(3):229-243. [DOI] [PubMed] [Google Scholar]
- 24.Estepp JH, Winter B, Johnson M, Smeltzer MP, Howard SC, Hankins JS. Improved hydroxyurea effect with the use of text messaging in children with sickle cell anemia. Pediatr Blood Cancer. 2014;61(11):2031-2036. [DOI] [PubMed] [Google Scholar]
- 25.Creary SE, Gladwin MT, Byrne M, Hildesheim M, Krishnamurti L. A pilot study of electronic directly observed therapy to improve hydroxyurea adherence in pediatric patients with sickle-cell disease. Pediatr Blood Cancer. 2014;61(6):1068-1073. [DOI] [PubMed] [Google Scholar]
- 26.Crosby LE, Ware RE, Goldstein A, et al. Development and evaluation of iManage: a self-management app co-designed by adolescents with sickle cell disease. Pediatr Blood Cancer. 2017;64(1):139-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith WR, Sisler IY, Johnson S, et al. Lessons learned from building a pediatric-to-adult sickle cell transition program. South Med J. 2019;112(3):190-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Porter JS, Matthews CS, Carroll YM, Anderson SM, Smeltzer MP, Hankins JS. Genetic education and sickle cell disease: feasibility and efficacy of a program tailored to adolescents. J Pediatr Hematol Oncol. 2014;36(7):572-577. [DOI] [PubMed] [Google Scholar]
- 29.Zhao MS, Johnson M, Pullen A, et al. Assessment of personal medical history knowledge in adolescents with sickle cell disease: a pilot study. J Clin Outcomes Manag. 2016;23(6):251-257. [Google Scholar]
- 30.Sawicki GS, Lukens-Bull K, Yin X, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ–Transition Readiness Assessment Questionnaire. J Pediatr Psychol. 2011;36(2):160-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Porter JS, Carroll YM, Anderson S, et al. Transition readiness assessment for sickle cell patients: A quality improvement project. J Clin Outcomes Manag. 2014;21(6):263-269. [Google Scholar]
- 32.Kassim AA, Pruthi S, Day M, et al. Silent cerebral infarcts and cerebral aneurysms are prevalent in adults with sickle cell anemia. Blood. 2016;127(16):2038-2040. [DOI] [PubMed] [Google Scholar]
- 33.Nolan VG, Anderson SM, Smeltzer MP, et al. Pediatric to adult care co-location transitional model for youth with sickle cell disease. Am J Hematol. 2018;93(1):E30-E32. [DOI] [PubMed] [Google Scholar]
- 34.Hankins JS, Estepp JH, Hodges JR, et al. Sickle Cell Clinical Research and Intervention Program (SCCRIP): a lifespan cohort study for sickle cell disease progression from the pediatric stage into adulthood. Pediatr Blood Cancer. 2018;65(9):e27228. [DOI] [PubMed] [Google Scholar]
- 35.Nazareth M, Hart L, Ferris M, Rak E, Hooper S, van Tilburg MAL. A parental report of youth transition readiness: the Parent STARx Questionnaire (STARx-P) and re-evaluation of the STARx Child Report. J Pediatr Nurs. 2018;38:122-126. [DOI] [PubMed] [Google Scholar]
- 36.Abel RA, Cho E, Chadwick-Mansker KR, D'Souza N, Housten AJ, King AA. Transition needs of adolescents with sickle cell disease. Am J Occup Ther. 2015;69(2):6902350030p1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Perry EL, Carter PA, Becker HA, Garcia AA, Mackert M, Johnson KE. Health literacy in adolescents with sickle cell disease. J Pediatr Nurs. 2017;36:191-196. [DOI] [PubMed] [Google Scholar]
- 38.Speller-Brown B, Varty M, Thaniel L, Jacobs MB. Assessing disease knowledge and self-management in youth with sickle cell disease prior to transition [published online ahead of print 19 December 2018]. J Pediatr Oncol Nurs. doi:10.1177/1043454218819447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Treadwell M, Johnson S, Sisler I, et al. Development of a sickle cell disease readiness for transition assessment. Int J Adolesc Med Health. 2016;28(2):193-201. [DOI] [PubMed] [Google Scholar]
- 40.Sobota A, Akinlonu A, Champigny M, et al. Self-reported transition readiness among young adults with sickle cell disease. J Pediatr Hematol Oncol. 2014;36(5):389-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Melita N, Diaz-Linhart Y, Kavanagh PL, Sobota A. Developing a problem-solving intervention to improve self-management and transition readiness in adolescents with sickle cell disease. J Pediatr Nurs. 2019;46:26-32. [DOI] [PubMed] [Google Scholar]
- 42.Calhoun CL, Abel RA, Pham HA, Thompson S, King AA. Implementation of an educational intervention to optimize self-management and transition readiness in young adults with sickle cell disease. Pediatr Blood Cancer. 2019;66(7):e27722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rodgers-Melnick SN, Pell TJG, Lane D, et al. The effects of music therapy on transition outcomes in adolescents and young adults with sickle cell disease [published online ahead of print 5 August 2017]. Int J Adolesc Med Health. doi:10.1515/ijamh-2017-0004. [DOI] [PubMed] [Google Scholar]
- 44.Wills KE, Nelson SC, Hennessy J, et al. Transition planning for youth with sickle cell disease: embedding neuropsychological assessment into comprehensive care. Pediatrics. 2010;126(suppl 3):S151-S159. [DOI] [PubMed] [Google Scholar]
- 45.Kidwell KM, Peugh J, Westcott E, et al. Acceptability and feasibility of a disease-specific patient portal in adolescents with sickle cell disease [published online ahead of print 18 October 2018]. J Pediatr Hematol Oncol. doi:10.1097/MPH.0000000000001341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Crosby LE, Joffe NE, Peugh J, Ware RE, Britto MT. Pilot of the chronic disease self-management program for adolescents and young adults with sickle cell disease. J Adolesc Health. 2017;60(1):120-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cerns S, McCracken C, Rich C. Optimizing adolescent transition to adult care for sickle cell disease. Medsurg Nurs. 2013;22(4):255-257. [PubMed] [Google Scholar]
- 48.Latzman RD, Majumdar S, Bigelow C, et al. Transitioning to adult care among adolescents with sickle cell disease: a transitioning clinic based on patient and caregiver concerns and needs. Intl J Child Adolesc Health. 2010;3(4):537-545. [Google Scholar]
- 49.Porter J, Russell K, Rupff R, et al. Provider perspectives of necessary factors in sickle cell disease health care transition: results from an online survey [abstract]. Blood. 2017;130(suppl 1):2140. [Google Scholar]