Abstract
The role and use of minimal residual disease (MRD) testing has changed significantly over the past few years as it has become part of the routine care for response assessment in multiple myeloma. The most widely used standardized methods to assess MRD in myeloma in the bone marrow are multicolor flow cytometry and next-generation sequencing. Importantly, the depth of MRD negativity in the bone marrow correlates with improved progression-free survival and overall survival in myeloma. Whole-body position emission tomography–computed tomography and magnetic resonance imaging are also used to evaluate patchy and extramedullary disease, which may not be readily visible through bone marrow assessment. This article reviews a clinical case in which MRD testing, both in bone marrow and in functional imaging, is part of the standard of care. It also reviews the different modalities of MRD testing and current practice guidelines. Finally, patients with myeloma may be tested for MRD after treatment because this is part of the routine response assessment according to International Myeloma Working Group criteria and correlates with clinical outcomes. Important questions such as when to stop therapy for sustained MRD-negative patients or whether to change treatments for patients who go from MRD negative to positive without other evidence of disease relapse are being evaluated in clinical trials and remain controversial.
Learning Objectives
Learn about available standardized MRD techniques in myeloma
Learn how to incorporate myeloma MRD assessments into routine clinical practice
Clinical case
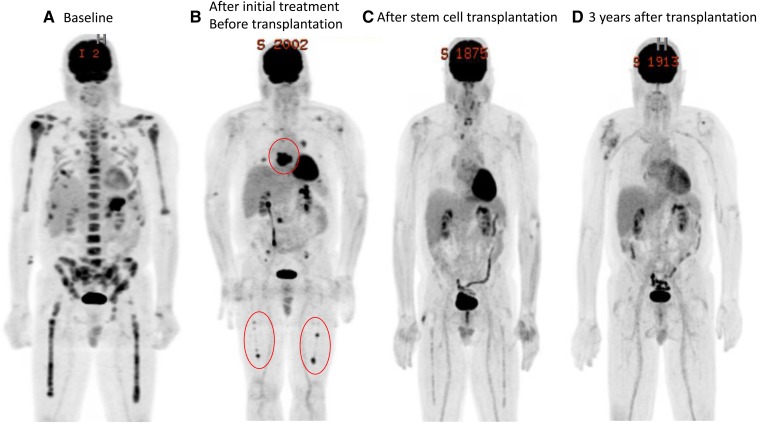
An otherwise healthy 64-year-old man was experiencing left-sided chest pain. He was taking aspirin to relieve his pain, and a few days later, he noticed dark stools, at which time he presented to a local emergency room, where he was found to be anemic with a hemoglobin level of 8.1 g/dL. Upper endoscopy with biopsy showed gastric ulceration with pathology positive for a high-grade neoplasm related to a plasma cell disorder. The patient was then referred to the hematology department for evaluation of potential multiple myeloma. His baseline results were as follows: white blood cell count 5 600/µL, platelets 257 000/µL, lactate dehydrogenase 312 IU/L, total protein 11 g/dL, albumin 3.2 g/dL, β2-microglobulin 6.4 mg/L, calcium 11.9 g/dL, creatinine 0.8 mg/dL, serum protein electrophoresis and immunofixation (SPEP/IFE) 6 g/dL immunoglobulin (Ig)A λ, 24-hour urine protein electrophoresis and immunofixation (UPEP/IFE) 116 mg Bence Jones protein λ, serum free light chain (sFLC) λ 494.96 mg/L, κ 5.16 mg/L, and involved/uninvolved sFLC ratio 96. A bone marrow biopsy showed 100% cellularity with massive infiltration by plasma cells in the core biopsy by CD138 immunohistochemistry. Flow cytometry of the bone marrow aspirate showed monoclonal plasma cells expressing CD38, CD138, CD45dim, CD20partial, CD28, and λ, as well as negative expression of CD19, CD56, and CD117. The result of fluorescence in situ hybridization was negative for usual myeloma genetic abnormalities, and the patient’s karyotype was 46,XY,t(1;4)12q-,18q-[8]/46,XY[2]. Whole-body positron emission tomography–computed tomography (WB-PET/CT) showed a gastric mass; T8 plasmacytoma; soft tissue left anterior second rib mass; lytic lesions throughout his skeleton; and increased fluorodeoxyglucose (FDG) avidity of his bilateral long bones, hip, and spine (Figure 1A). He was diagnosed with stage III multiple myeloma according to the Revised International Staging System. He was then started on treatment with carfilzomib, lenalidomide, and dexamethasone for four 28-day cycles with negative SPEP/IFE and 24-hour UPEP/IFE, normalization of involved/uninvolved sFLC ratio, and bone marrow biopsy showing normal plasma cells using a multicolor flow cytometry (MFC) minimal residual disease (MRD) assay with a sensitivity of 10−5 (2 million events analyzed). Follow-up WB-PET/CT showed a response to therapy in almost all areas of involvement but worsening FDG-avid abnormal soft tissue at T8-T9 and right pleura and scattered persistent areas of FDG avidity within the bones (Figure 1B). The patient then had stem cells collected and proceeded with high-dose melphalan 200 mg/m2 and stem cell rescue. Repeat bone marrow MFC MRD assessment and WB-PET/CT showed no residual disease (Figure 1C). At that time, the patient initiated treatment with lenalidomide after transplant with serial monitoring of MRD in bone marrow and WB-PET/CT every 12 months. The patient remained in complete remission (CR) as of his last assessment 3 years after transplant by both imaging and bone marrow MFC (Figure 1D).
Figure 1.
(A) Baseline. (B) After initial treatment before transplant. (C) After stem cell transplant. (D) Three years after transplant.
Introduction
Multiple myeloma is a cancer of the immune system that originates in plasma cells. Although multiple myeloma remains mostly without a cure, median overall survival (OS) for newly diagnosed patients has increased significantly from 2 to 3 years to closer to 10 years and beyond, with some patients being considered functionally cured.1-3 This is mostly due to the generalized use of proteasome inhibitors and immunomodulatory drugs for the initial treatment of multiple myeloma. In parallel, the response rates have also dramatically increased, with virtually all patients responding to therapy and up to 80% of those who respond achieving CR.4,5 The International Myeloma Working Group (IMWG) recognized in 2016 that MRD detection was an important endpoint in myeloma response assessment and updated the response criteria to include measurement of MRD as the deepest level of response that can be achieved.6 The IMWG defines the presence of MRD in myeloma as having one tumor cell in at least 105 normal cells in bone marrow (sensitivity of 10−5). Since then, MRD assessment in myeloma has been part of the standard of care and implemented at locations where MRD testing is available.
Goals of treatment and depth of response
In a meta-analysis of 15 flow cytometry MRD studies published between 1998 and 2016, 9 of these studies showed improved progression-free survival (PFS) and OS for patients who were MRD negative vs positive.7 In these studies, the sensitivity ranged from 10−4 to 10−5 with less than 2 million total acquired events. Moreover, the patients who achieved CR (MRD negative) had a much lower risk of progression or death than those who were MRD positive (decreased by 56% and 63% for progression and death, respectively). These results have also been confirmed in more recent studies using flow cytometry.8,9 Molecular techniques such as next-generation sequencing (NGS) have shown similar results with improved survival outcomes for patients who are MRD negative vs positive with higher sensitivity.10 Achievement of MRD negativity in myeloma should be the goal of therapy and a prerequisite to achieve a sustained remission and ultimately a cure.11 Thus, the goal of therapy for the 64-year-old man in the present clinical case should be to achieve CR (MRD negative) that is sustained over time.
Methods to quantify MRD used in routine care
Detection of myeloma MRD is most commonly done with the use of advanced flow cytometry (MFC) or NGS. Both are widely used for assessment of MRD in myeloma for clinical trials and standard of care.
Flow cytometry
Normal and abnormal plasma cells have different immunophenotypic profiles that can be detected using flow cytometry. This technique uses fluorochrome–antibody conjugation to antigens in the surface of the plasma cells for detection of MRD without requiring evaluation of cytoplasmic κ or λ light chain expression. Table 1 shows the differential phenotypic markers used for assessment by flow cytometry. Besides having restricted cytoplasmic immunoglobulin chain expression, myeloma cells usually show expression of at least two aberrant markers. Flow cytometry MRD assessments vary in technique among countries and institutions.12 Most centers use fluorochrome antibody panels using an 8- or 10-color approach with a sensitivity ranging from 10−5 to 10−6. An international effort led to development of the EuroFlow test, which captures up to 10 million events and uses 2 eight-color tubes with 10 different antigens and a detection limit of 2 myeloma cells in 1 million events.13 This method was standardized by using automated gating, and thus it is less expert dependent. Despite this, EuroFlow is labor intense with increased cost, which limits its applicability, at least in the United States, where additional reimbursement is not received. Because of this, several major U.S.-based centers use a 10-color single-tube technique with sensitivity that is similar to that of the EuroFlow test but is less labor intense and has improved applicability.14 At an institution that uses flow cytometry as a platform to measure MRD in myeloma, it is important to become familiar with the test’s sensitivity and the total number of events analyzed per sample. It is also important to try to make sure that these samples are taken as first pulls when drawing bone marrow aspirates, because hemodilution with sequenced aspirate pulls is well described and could lead to false-negative MRD results.15
Table 1.
Expression of surface markers that help differentiate between normal and aberrant plasma cells using flow cytometry
| CD38 | CD138 | CD81 | CD27 | CD45 | CD19 | CD20 | CD56 | CD117 | CD28 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Normal plasma cells | Strong | Strong | Strong | Strong | Variable | Variable | No expression | No expression | No expression | No expression |
| Abnormal plasma cells | Lower expression | Strong | Low or no expression | Low or no expression | Low or no expression | Low or no expression | Strong or variable | Strong or variable | Strong or variable | Strong or variable |
NGS
The most commonly used commercial molecular test to measure bone marrow myeloma MRD through NGS is the clonoSEQ Assay (Adaptive Biotechnologies, Seattle, WA). This platform has been cleared since 2018 by the FDA for use to determine MRD in myeloma. FDA approval was based on PFS and OS benefit from two large phase 3 studies: the ALCYONE and IFM/DCFI 2009 studies.10,16,17 In the IFM/DCFI study, in which newly diagnosed patients were treated with bortezomib-lenalidomide-dexamethasone with up-front or delayed autologous transplant, 269 patients who achieved at least a very good partial response to treatment were tested for MRD using clonoSEQ. Patients who did not achieve at least a very good partial response were considered MRD positive. At the clonoSEQ cutoff of 10−6 sensitivity, PFS and OS were significantly prolonged in the patients who achieved MRD negativity vs those who did not. (PFS was not reached in MRD-negative patients vs reached in 29 months in MRD-positive patients.) The ALCYONE study compared newly diagnosed patients who received bortezomib-melphalan-prednisone with or without daratumumab. In this study, the addition of daratumumab resulted in an improvement in the rate of MRD negativity (22% with and 6% without daratumumab; P < .001), and negative MRD status was associated with longer PFS than positive status, regardless of treatment. Two additional large, prospective, randomized studies in relapsed/refractory myeloma (CASTOR [bortezomib-dexamethasone with or without daratumumab] and POLLUX [lenalidomide-dexamethasone with or without daratumumab]) have shown similar results favoring MRD negativity as a treatment endpoint.18,19 clonoSEQ uses a polymerase chain reaction assay and NGS to quantify and identify rearranged VDJ, IgK, and IgL gene sequences from the patient’s bone marrow sample. With this method, clonotypes are identified. Once a clonotype has a frequency >5% in the baseline diagnostic sample, it is regarded as clonal. Through the identification and quantification of clonal gene rearrangements, MRD can be identified in follow-up samples after treatment and at relapse.
Another NGS method is used for detection of MRD. In the PETHEMA/GEM2010MAS65 study, 73 patients with myeloma older than 65 years of age were evaluated by a EuroClonality NGS group test, which showed high applicability (to 97% of patients) and sensitivity (10−5). In this study, the median OS was shorter for patients who were MRD positive than for those who were MRD negative (3-year OS, 50% vs 100%, respectively).20
The sensitivity, advantages, and disadvantages of using MFC vs NGS for determination and tracking of MRD in myeloma has been compared and reviewed extensively.21 Overall, NGS is more sensitive than conventional flow cytometry when measuring MRD for myeloma.22 However, MFC can achieve levels of sensitivity similar to those of NGS. Because of this, use of one method or another ultimately may depend on regional availability. NGS is fully automated and less expert dependent, and it has high sensitivity and applicability (>95%). It also allows for tracking and identification of clonotypes and subclones, which may provide information on the biology and evolution of myeloma for each patient with treatment. It does require a baseline sample to enable tracking of clones after treatment, whereas MFC does not.
In the present clinical case, the institution where the patient was being treated had availability of MFC, but not NGS, to measure bone marrow MRD in myeloma. For that reason, this patient had MRD tested this way. Use of MFC or molecular techniques for measurement of MRD assessment depends on institutional/geographical availability.
Functional imaging
Several studies have shown that skeletal survey is not adequate for the staging of patients with multiple myeloma, because it reports false-negative results in ∼30% of patients.23,24 Because of this, both WB-PET/CT and magnetic resonance imaging are used routinely in the care of patients with multiple myeloma. A major disadvantage of using bone marrow samples for assessment of MRD in myeloma is related to myeloma being a patchy disease. MRD bone marrow assessments may not capture spatial heterogeneity, and residual myeloma disease present in areas that are not being biopsied for MRD assessment can easily be missed. Functional imaging with WB-PET/CT or magnetic resonance imaging can detect residual myeloma disease that is not apparent in bone marrow MRD assessment, and it is useful to determine CR in patients after treatment as well as to assess possible relapse. The 2016 IMWG response criteria define “imaging plus MRD negative” as patients who have MRD negativity by either MFC or NGS and disappearance of any increased tracer uptake in baseline PET/CT. “Sustained MRD negative” is defined as MRD negativity in the bone marrow (MFC or NGS) and by imaging, confirmed with assessments a minimum of 1 year apart.6 In the present clinical case, the result of evaluation by only MFC bone marrow was consistent with MRD negativity; however, only when WB-PET/CT was performed was it revealed that the patient had significant residual disease in the spine and long bones (Figure 1B). Functional imaging of myeloma is required to assess residual disease after treatment. A combination of MRD bone marrow and imaging assessment is likely to yield the best prognosis in patients with negative results for both tests after treatment.
Prediction of clinical outcomes after MRD testing
A multitude of studies have shown that achievement of bone marrow MRD negativity in myeloma results in improved PFS and OS compared with MRD positivity.21 Thus, MRD negativity can be considered a surrogate marker of PFS and OS in most instances. Addition of whole-body functional imaging adds another layer of sensitivity. Once patients with myeloma are “imaging plus MRD negative” after treatment, it is unclear how often MRD bone marrow and functional imaging should be performed. Test cost (such as for WB-PET/CT) and discomfort (serial bone marrow biopsies) are limitations when considering MRD monitoring in patients with myeloma.
Limitations of serial monitoring could be overcome by performing liquid biopsies. Liquid biopsies use peripheral blood to detect and quantify myeloma disease. Several studies have evaluated the use of cell-free DNA and circulating tumor cells in myeloma. Overall, paired peripheral blood and bone marrow samples have shown that both cell-free DNA and circulating tumor cell levels correlate with the level of bone marrow involvement by myeloma and clinical outcomes, such as PFS and OS.25-27 Despite this, a consensus has not been reached regarding the use of liquid biopsies for clinical care in myeloma, and it remains largely investigational. As technology advances, it is possible that in the future a liquid biopsy may be available for patients with myeloma to assess response and monitor disease during treatment/relapse.
Depth of response
The current MRD sensitivity cutoff recommended by the IMWG is 10−5. Despite this, several studies have shown that the 10−6 cutoff may be better at predicting clinical outcomes, including the IFM2009 clinical trial, where the 10−6 cutoff was better than the 10−5 cutoff at discriminating PFS and OS.10,19 Ideally, MRD testing should reach a sensitivity level that is deep enough to predict absence of relapse (cure). To the author’s knowledge, the optimal level of sensitivity for myeloma MRD testing has not yet been established.
Timing of MRD and guidance during therapy
There is currently no consensus regarding the optimal time points for MRD and imaging assessment in myeloma after initial achievement of MRD-negative status. In the present clinical case, it was decided that this patient would be monitored while receiving maintenance lenalidomide with yearly MRD MFC bone marrow and WB-PET/CT. Initial data derived from clinical trials showed that MRD detection in patients who were previously MRD negative predated clinical relapse by a few months.28-30 Clinical trials are ongoing that address the question of how often to monitor for MRD and when to change therapy based on changes in MRD status.
In conclusion, MRD testing in myeloma is a powerful tool that predicts clinical outcomes. Response criteria in myeloma currently require MRD assessment using either MFC or NGS with a 10−5 cutoff. Both of these techniques are widely available. Use of one or the other may depend on local availability. Myeloma is a disease with spatial heterogeneity, and functional imaging is also required for response monitoring. After initial documentation of MRD-negative status, timing of serial monitoring and change in therapy are subjects of intense investigation in clinical trials and are controversial until more data are available. Liquid biopsies remain investigational in myeloma.
Acknowledgments
This work was supported by a grant from the International Myeloma Foundation Black Swan Research Initiative. This work was also supported in part by the MD Anderson Cancer Center Support Grant (P30 CA016672), a Leukemia and Lymphoma Society Specialized Center of Research program grant (SCOR-12206-17), the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation, the Multiple Myeloma Research Foundation, Chapman Perelman Foundation, and the University of Texas MD Anderson Cancer Center Moon Shot Program.
Correspondence
Elisabet E. Manasanch, Department of Lymphoma/Myeloma, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd, Unit 429, Houston, TX 77030; e-mail: eemanasanch@mdanderson.org.
References
- 1.Barlogie B, Mitchell A, van Rhee F, Epstein J, Morgan GJ, Crowley J. Curing myeloma at last: defining criteria and providing the evidence. Blood. 2014;124(20):3043-3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Usmani SZ, Hoering A, Cavo M, et al. Clinical predictors of long-term survival in newly diagnosed transplant eligible multiple myeloma—an IMWG Research Project. Blood Cancer J. 2018;8(12):123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thorsteinsdottir S, Dickman PW, Landgren O, et al. Dramatically improved survival in multiple myeloma patients in the recent decade: results from a Swedish population-based study. Haematologica. 2018;103(9):e412-e415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Landgren O, Rajkumar SV. New developments in diagnosis, prognosis, and assessment of response in multiple myeloma. Clin Cancer Res. 2016;22(22):5428-5433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaudhry M, Steiner R, Claussen C, et al. Carfilzomib-based combination regimens are highly effective frontline therapies for multiple myeloma and Waldenström’s macroglobulinemia. Leuk Lymphoma. 2019;60(4):964-970. [DOI] [PubMed] [Google Scholar]
- 6.Kumar S, Paiva B, Anderson KC, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17(8):e328-e346. [DOI] [PubMed] [Google Scholar]
- 7.Munshi NC, Avet-Loiseau H, Rawstron AC, et al. Association of minimal residual disease with superior survival outcomes in patients with multiple myeloma: a meta-analysis. JAMA Oncol. 2017;3(1):28-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu B, Thall P, Milton DR, et al. High-risk myeloma and minimal residual disease postautologous-HSCT predict worse outcomes. Leuk Lymphoma. 2019;60(2):442-452. [DOI] [PubMed] [Google Scholar]
- 9.Tageja N, Korde N, Kazandjian D, et al. Combination therapy with carfilzomib, lenalidomide and dexamethasone (KRd) results in an unprecedented purity of the stem cell graft in newly diagnosed patients with myeloma. Bone Marrow Transplant. 2018;53(11):1445-1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Avet-Loiseau H, Lauwers-Cances V, Corre J, Moreau P, Attal M, Munshi N. Minimal residual disease in multiple myeloma: final analysis of the IFM2009 Trial [abstract]. Blood. 2017;130(suppl 1):435. [Google Scholar]
- 11.Davies FE. Is molecular remission the goal of multiple myeloma therapy? Hematology Am Soc Hematol Educ Program. 2017;2017:205-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salem D, Stetler-Stevenson M, Yuan C, Landgren O. Myeloma minimal residual disease testing in the United States: evidence of improved standardization. Am J Hematol. 2016;91(12):E502-E503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flores-Montero J, Sanoja-Flores L, Paiva B, et al. Next generation flow for highly sensitive and standardized detection of minimal residual disease in multiple myeloma. Leukemia. 2017;31(10):2094-2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roshal M, Flores-Montero JA, Gao Q, et al. MRD detection in multiple myeloma: comparison between MSKCC 10-color single-tube and EuroFlow 8-color 2-tube methods. Blood Adv. 2017;1(12):728-732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manasanch EE, Salem DA, Yuan CM, et al. Flow cytometric sensitivity and characteristics of plasma cells in patients with multiple myeloma or its precursor disease: influence of biopsy site and anticoagulation method. Leuk Lymphoma. 2015;56(5):1416-1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mateos MV, Dimopoulos MA, Cavo M, et al. ; ALCYONE Trial Investigators. Daratumumab plus bortezomib, melphalan, and prednisone for untreated myeloma. N Engl J Med. 2018;378(6):518-528. [DOI] [PubMed] [Google Scholar]
- 17.FDA authorizes first next generation sequencing-based test to detect very low levels of remaining cancer cells in patients with acute lymphoblastic leukemia or multiple myeloma [news release]. 2018. September 28. https://www.fda.gov/news-events/press-announcements/fda-authorizes-first-next-generation-sequencing-based-test-detect-very-low-levels-remaining-cancer. Accessed 22 July 2019.
- 18.Suzuki K, Dimopoulos MA, Takezako N, et al. Daratumumab, lenalidomide, and dexamethasone in East Asian patients with relapsed or refractory multiple myeloma: subgroup analyses of the phase 3 POLLUX study. Blood Cancer J. 2018;8(4):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spencer A, Lentzsch S, Weisel K, et al. Daratumumab plus bortezomib and dexamethasone versus bortezomib and dexamethasone in relapsed or refractory multiple myeloma: updated analysis of CASTOR. Haematologica. 2018;103(12):2079-2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martinez-Lopez J, Sanchez-Vega B, Barrio S, et al. Analytical and clinical validation of a novel in-house deep-sequencing method for minimal residual disease monitoring in a phase II trial for multiple myeloma. Leukemia. 2017;31(6):1446-1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kunacheewa C, Lin P, Manasanch EE. Minimal residual disease in multiple myeloma 2019. Adv Cell Gene Ther. 2019;e71. [Google Scholar]
- 22.Ladetto M, Brüggemann M, Monitillo L, et al. Next-generation sequencing and real-time quantitative PCR for minimal residual disease detection in B-cell disorders. Leukemia. 2014;28(6):1299-1307. [DOI] [PubMed] [Google Scholar]
- 23.Manasanch EE, Landgren O. Myeloma imaging: time to move on! Leuk Lymphoma. 2016;57(7):1499-1500. [DOI] [PubMed] [Google Scholar]
- 24.Mangiacavalli S, Pezzatti S, Rossini F, et al. Implemented myeloma management with whole-body low-dose CT scan: a real life experience. Leuk Lymphoma. 2016;57(7):1539-1545. [DOI] [PubMed] [Google Scholar]
- 25.Gonsalves WI, Rajkumar SV, Gupta V, et al. Quantification of clonal circulating plasma cells in newly diagnosed multiple myeloma: implications for redefining high-risk myeloma. Leukemia. 2014;28(10):2060-2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oberle A, Brandt A, Voigtlaender M, et al. Monitoring multiple myeloma by next-generation sequencing of V(D)J rearrangements from circulating myeloma cells and cell-free myeloma DNA. Haematologica. 2017;102(6):1105-1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kis O, Kaedbey R, Chow S, et al. Circulating tumour DNA sequence analysis as an alternative to multiple myeloma bone marrow aspirates. Nat Commun. 2017;8:15086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gu J, Liu J, Chen M, Huang B, Li J. Longitudinal flow cytometry identified “minimal residual disease” (MRD) evolution patterns for predicting the prognosis of patients with transplant-eligible multiple myeloma. Biol Blood Marrow Transplant. 2018;24(12):2568-2574. [DOI] [PubMed] [Google Scholar]
- 29.Ferrero S, Ladetto M, Drandi D, et al. Long-term results of the GIMEMA VEL-03-096 trial in MM patients receiving VTD consolidation after ASCT: MRD kinetics’ impact on survival. Leukemia. 2015;29(3):689-695. [DOI] [PubMed] [Google Scholar]
- 30.Oliva S, Gambella M, Gilestro M, et al. Minimal residual disease after transplantation or lenalidomide-based consolidation in myeloma patients: a prospective analysis. Oncotarget. 2017;8(4):5924-5935. [DOI] [PMC free article] [PubMed] [Google Scholar]