Abstract
Young children with neurodevelopmental disorders such as autism spectrum disorders (ASD) and Rett syndrome often experience severe communication impairments. This study examined the efficacy of parent-implemented communication assessment and intervention with remote coaching via telehealth on the acquisition of early communication skills of three young children with ASD (2) and Rett syndrome (1). Efficacy of the intervention was evaluated using single-case experimental designs. First, functional assessment was used to identify idiosyncratic/potentially communicative responses and contexts for each child. Next, parents implemented functional communication training (FCT). All of the children acquired the targeted communication responses. The findings support the efficacy of telehealth as a service delivery model to coach parents on intervention strategies for their children’s early communication skills.
Keywords: Communication intervention, Telehealth, Idiosyncratic responses, FCT
Introduction
Early intervention targeting communication and other critical developmental domains is strongly recommended to promote optimal outcomes for children with autism spectrum disorder (ASD) and related neurodevelopmental disabilities (American Academy of Pediatrics 2007; Individuals with Disabilities Education ACT [IDEA] 2004; National Research Council 2001; Satcher 2000). Further, early and intensive intervention grounded in behavioral principles is linked to improvements in communication (Cohen et al. 2006; Sallows and Graupner 2005), IQ (Sheinkopf and Siegel 1998; Sallows and Graupner 2005; Cohen et al. 2006; Eldevik et al. 2006), challenging behavior (Wacker et al. 2013a, b), and related positive child and (Harris and Handleman 2000) family outcomes (Remington et al. 2007) for children with ASD.
Recommendations based on research findings indicate that early intervention should be delivered as an intensive, individualized, and specialized service (American Academy of Pediatrics 2007; Rogers 1998; National Research Council [NRC], 2001). The American Academy of Pediatrics; issued the following 2007 guidelines for children with ASD: (1) treatment should begin when ASD is a serious consideration, including before a formal diagnosis is given, if necessary, (2) a minimum of 25 h of intensive intervention per week for the full calendar year should occur, and (3) parent involvement, education, and training (retrieved from pediatrics.aappublications.org) need to be a part of treatment. Equally important is that services are delivered in family-centered settings natural to the child (AAP 2007; Horn et al. 2002; IDEA 2004; NRC 2001). The position statement of the American Speech-Language Hearing Association (ASHA 2011) states that early communication intervention should help to increase the child’s communication and functioning within their daily life. Taken together, optimal communication intervention for children with ASD and other neurodevelopmental disorders should be: (1) delivered early in life, (2) intensive, (3) delivered in natural settings, and (4) inclusive of families in education and training.
Barriers to Services
Despite the clear benefits of early intervention, many children and families of children with ASD or related developmental disabilities may experience difficulties with accessing intervention services in a timely or adequate manner. In a 2004 study regarding barriers to services for children with developmental disabilities, the majority of parents reported concerns regarding unmet communication and behavior management needs (Betz et al. 2004).
Prevalence and Waitlists
With the growing prevalence of ASD (Chasson et al. 2007), service providers have not been able to fulfill the increased demand for services. ASD impacts an estimated 1/68 children nationally (Christensen et al. 2016), and an estimated 1/72 children in Minnesota (Hewitt et al. 2013). Unfortunately, the increased prevalence and demand for services has resulted in a shortage of available evidence-based community services (Dingfelder and Mandell 2011; Kazdin 2008; Montes et al. 2009; Sperry et al. 1999; Stahmer and Gist 2001; Symon 2005). Increased demand for services compounded with limited capacity of service providers (i.e., shortage of high quality providers) likely results in many families being placed on a waitlist prior to service initiation. There are limited data available on the effects of waitlists or the effects a delay of service have for children with developmental disabilities. Keating et al. (1998), however, described the greatest concerns reported by stake-holders regarding time spent on waitlists as (1) concerns with the delay in the onset of services considering the clear benefits associated with early intervention, (2) lost time in the window of childhood development, and (3) prolonged or exacerbated stress and uncertainty put on families during the waiting process.
Personnel Shortage
Early intervention requires the knowledge and oversight of trained professionals, yet a high percentage of surveyed special education coordinators across the country report a shortage in ASD-related trained clinical providers, including behavioral therapists (reported from 89%) and SLPs (reported from 82%; Wise et al. 2010). Despite this shortage, demand for services continues to rise as a majority of coordinators also reported a marked increase since 2007 in requests for ASD evaluations and for early intervention services for ASD in their state (Wise et al. 2010).
Clinicians with a master’s or higher level of education and/or licensure, including Board Certified Behavior Analysts (BCBAs) and Speech-Language Pathologists (SLPs) often oversee clinical intervention. Nationally, many private insurance companies require a licensed mental health provider or BCBA to oversee the treatment planning and intervention for children receiving early intensive behavioral intervention. However, there is a very small number of BCBAs available to satisfy this requirement. For example, as of June 2015, there were only 120-registered and listed BCBAs in Minnesota (retrieved from http://www.bacb.com) to meet the needs of all the individuals with ASD in the state (a 2010 prevalence estimate of Minneapolis, MN indicated approximately 1 in 48 children between the ages of 7 and 9 with ASD; Hewitt et al. 2013). Compounding this problem is a shortage of licensed SLPs to guide and oversee communication interventions (ASHA 2005). The highest number of unfilled positions includes SLPs who work in children’s homes, where early intervention services are typically delivered (ASHA 2005). Furthermore, among practicing SLPs, there is a shortage of those who have training in augmentative and alternative communication (AAC) for children with severe disabilities (ASHA 2011).
Families Residing in Rural Areas
Children and families in rural areas are at a striking disadvantage in accessing needed services; they face limited service provider options and are less likely to access ASD treatment (Thomas et al. 2007). Taken together, the acceleration of the prevalence of ASD, waitlists for evaluations and services, and a lack of highly trained providers are barriers to adequate and/or timely services for children and families.
Costs of Delay in Service
In the short-term, delays or lack of access to services may worsen challenging behavior that often begins in early ages for children with developmental disabilities (Oliver et al. 2012; Rogers and Wallace 2011). Further, the delay or lack of access may result in the child requiring greater special education supports (Sallows and Graupner 2005). While waiting, families may experience prolonged stress and uncertainty (Keating et al. 1998). In the long-term, the failure to gain some form of communication by age 6 is closely related to poor outcomes for adults with ASD (Howlin et al. 2004) and puts children with severe disabilities at risk for an overall poorer quality of life than if they received early and effective intervention (Brown et al. 1998). Society also bears the costs of a lack of effective early intervention; a cost-analysis by Chasson et al. (2007) revealed that 3 years spent in early and intensive behavioral intervention for all children with ASD in the state of Texas would be associated with a projected 2.09 billion dollars of direct savings in the cost of special education services over the children’s school-age years. Thus, in both the short and the long-term, the benefits of early intervention far outweigh the costs.
Naturalistic Developmental Behavioral Interventions (NDBIs)
Operant-based models of applied behavior analytic (ABA) intervention have been effective at increasing communication for individuals with severe intellectual and developmental disabilities and communication impairments (Durand 1999; Johnston et al. 2004). Early behavioral interventions are backed by robust evidence for improvement in developmental domains such as language for children with ASD (e.g., Cohen et al. 2006; Eikeseth et al. 2002). Although these models are shifting to include more natural environment training arrangements, (Koegel et al. 1992; Sundberg and Partington 1999) many ‘traditional’ behavioral intervention models may rely on structured training in discrete trials arrangements, (a technique that minimizes distractions and includes initial teaching of a new skill through massed trials; e.g., Lovaas 1987).
NDBI models have emerged that are increasingly developmentally relevant while emphasizing highly effective ABA methodology for young learners (Ingersoll et al. 2016; Schreibman et al. 2015). NDBIs rely on ABA behavioral principles (e.g., three-term contingency, shaping and chaining, and socially important target behaviors) and methodologies (e.g., prompting and fading, and databased decision making; Schreibman et al. 2015). NDBIs are embedded with developmental principles and practices with an emphasis placed on naturalistic intervention elements (e.g., targeting skills within a developmentally appropriate sequence). In addition to adhering to recommended early intervention practices involving naturalized, routines-based, and family-centered interventions, as discussed by Schreibman et al. (2015), NDBIs may be easier for parents to implement and may promote child skill acquisition in a generalized and natural manner.
Functional Communication Training (FCT)
FCT is an empirical, behavioral, evidence- and reinforcement-based approach to replacing inappropriate or challenging behavior, such as aggression and self-injurious behavior, with an appropriate communicative response (Carr and Durand 1985). Functional analysis (FA; Iwata et al. 1982/94) informs intervention planning for FCT by identifying the maintaining functional reinforcers of challenging behavior. FA + FCT is well documented as an intervention approach for effectively reducing challenging behavior with individuals with severe disabilities (Tiger et al. 2008) because it provides differential functional reinforcement for an appropriate communicative behavior and can be individualized for people with even the most severe motor impairments (Horner and Carr 1997). FA + FCT has demonstrated effectiveness across a wide range of settings, including inpatient (Asmus et al. 2004) and outpatient clinics (Derby et al. 1992; Kurtz et al. 2003), residential (Bailey et al. 2002) and home settings (Derby et al. 1997; Wacker et al. 1998, 2005).
FA + FCT is also documented as an intervention package that parents of children with developmental disabilities and challenging behavior can effectively implement with coaching from behavior consultants (i.e., applied behavior analysts) both on-site (Derby et al. 1997; Wacker et al. 1998) and remotely via telehealth (Wacker et al. 2013a, b). In these studies, consultants described and demonstrated procedures as well as provided prompts and feedback to parents who implemented the procedures (Harding et al. 2009). These studies consistently demonstrated 90% or better reductions in challenging behavior and concomitant increases in appropriate responses such as communication and task completion (Wacker et al. 1998, 2005, 2011).
Although a majority of the FCT literature has focused on FCT as an intervention to reduce challenging behavior, there are also two studies that we know of that demonstrate the effectiveness of FCT for teaching appropriate communicative alternatives to replace idiosyncratic behavioral responses. These idiosyncratic responses are not identified as challenging behavior, but are topographies of responses that are difficult to interpret and expand upon, such as leading and reaching (Byiers et al. 2014; Keen et al. 2001). For children who do not have an easily recognizable method of communication, it is plausible that embedding social-communication intervention into natural daily activities and play routines would serve to maximize the effectiveness of the intervention (see Woods et al. 2004). Thus, FCT that is designed to shape idiosyncratic, potentially communicative responses into more recognizable communicative behavior may have potential significance as a model for initial communication intervention that takes advantage of contexts in which the child has been observed attempting to communicate.
FCT as a Routines-Embedded, Naturalistic Intervention
Moes and Frea (2002) examined parent-implemented intervention in both a traditional FCT model and a contextualized FCT on the disruptive and communicative behavior of three children with autism. The participants (2 boys and 1 girl) were between the ages of 3 and 5. Two children had only mild language delays, and 1 child had severe receptive and expressive language deficits. In the traditional FCT condition, FCT was conducted by the researchers who prompted and reinforced communicative alternative responses (verbalizations and manual signs) while the parent(s) observed. In the contextualized condition, FCT was embedded into routines in which the families had reported disruptive behavior problems; examples of routines included going for a walk and eating a meal at the table. Parents participated in the contextualized sessions by facilitating interaction between siblings, working on other skills within the routine (e.g., fine motor skills of holding a fork), and other goals that the family listed (e.g., both parents implementing the intervention) while the researchers taught the communicative alternative responses. Decreased disruptive behavior and increased communicative behavior were observed in both conditions and the results were maintained over 1 year. In a follow-up survey of the parents on “goodness of fit” of the two interventions, both mothers and fathers rated the contextualized intervention as the more sustainable intervention for their family.
FCT as an Early Communication Intervention
The extant literature primarily focuses on FCT as an intervention to reduce challenging behavior. However, there is emerging efficacy evidence for the use of FCT as a communication intervention (Byiers et al. 2014; Keen et al. 2001; Tait et al. 2004). As previously discussed, idiosyncratic responses can serve as ‘behavioral indicators’ of environmental events that serve as motivating for children without verbal or other established communication repertoires (Drasgow et al. 1996). If a child leads (i.e., takes an adult’s hand and pulls it towards an item or area) an adult towards the refrigerator to access juice, it would likely be advantageous to teach the child a more recognizable communicative response (i.e., AAC response) that will reliably produce access to the juice regardless of who the listener is and whether they know the child well enough to know that they are asking for juice and not milk or something else in the refrigerator.
Keen, Sigafoos, and Woodyatt (2001) demonstrated the utility of FCT to shape idiosyncratic responses into more recognizable communication with three participants with ASD who were nonverbal. Idiosyncratic responses were identified for each participant and an alternative behavior was targeted in the same context. For example, researchers shaped the idiosyncratic response of a participant whose eye gaze appeared to function as a response that produced attention into a communicative alternative that consisted of waving a hand to gain attention. Shaping potential communicative acts into formal communicative messages may be an important beginning communication intervention strategy for children with severe neurodevelopmental disabilities because the child has already demonstrated that they have some communicative means (Reichle and Wacker in press).
Byiers et al. (2014) experimentally analyzed the social function of varying idiosyncratic behavior forms of girls and women with RTT using functional analysis and subsequent FCT intervention; they found that all three participants engaged in differentially more idiosyncratic behavior during individualized conditions designed in which social reinforcers, (i.e., head massage, attention, and TV) were delivered contingent on the targeted idiosyncratic responses. Although limited, the available evidence suggests that idiosyncratic responses can be shaped into more recognizable communication through FCT as an initial communication intervention strategy.
The application of FCT may have potential significance as a model for initial communication intervention for children with severe neurodevelopmental disabilities who do not have an easily recognizable method of communication. FCT may be a feasible and efficient method to begin communication intervention that builds upon contexts of the child’s current motivation to attempt communication (Drasgow et al. 1996). The communicative alternative response can serve as an initial communication skill to later expand upon (Mace and Roberts 1993; Schieltz et al. 2011). Additionally, FCT that is aimed at shaping idiosyncratic responses into more recognizable communicative behaviors can be conducted within a child’s natural environment and can be easily tailored and embedded into natural routines and activities within their day. This intervention may have particular relevance as a feasible initial communication intervention for caregivers to implement in the home with their young children with severe neurodevelopmental disabilities.
Telehealth as a Service Delivery Mechanism
A potential solution to facilitate the cost-effective provision of services to more young children and their families lies in the use of telehealth technology. Previous research has demonstrated telehealth as a promising and efficacious service delivery method for remotely coaching parents through assessment and intervention for challenging behavior for children with ASD in their homes (Lindgren et al. 2016; Wacker et al. 2013a, b). These studies reported decreases in challenging behavior and replicated effects of the same procedures previously delivered in-person by interventionists in home and clinic settings. Parent participants who were coached remotely via telehealth implemented intervention procedures with a high level of procedural fidelity and they rated the procedures as highly acceptable (Suess et al. 2014; Wacker et al. 2013a, b).
Telehealth has been demonstrated as a promising method of intervention delivery for parent-implemented, social-communication interventions for young children with ASD (McDuffie et al. 2013; Vismara et al. 2012, 2013; Wainer and Ingersoll 2015). A parent-implemented version of Early Start Denver Model, a curriculum-based NDBI, has been demonstrated as efficacious at improving children’s social-communicative behaviors (Vismara et al. 2012) and child verbal utterances (Vismara et al. 2013) when parents were provided with video modules and coached on the procedures live via telehealth. Parents have also been able to serve as implementers with coaching via telehealth in interventions to teach imitation (Wainer and Ingersoll 2015) and natural language (McDuffie et al. 2013). Clearly, if interventions delivered via telehealth continue to produce favorable outcomes, telehealth for parent-coaching could revolutionize current models of service delivery by bridging the many barriers to intervention access.
Purpose of Study and Research Questions
The current study was designed to contribute to the evidence-base on communication interventions delivered via telehealth by conducting: (1) functional assessment to identify contexts in each child’s daily life and potentially communicative idiosyncratic responses the child engaged in (e.g., reaching for or leading an adult to desired items) within those contexts, (2) FCT intervention to provide differential reinforcement for an augmentative and alternative (AAC) request in the identified communicative context, and (3) intervention across three communicative contexts/routines. The overall purpose of the current study was to determine the effectiveness of parent-implemented communication assessment and FCT with coaching via telehealth on the acquisition of early communication skills for young children with severe neurodevelopmental disabilities.
Method
Participants and Settings
Three young girls with severe neurodevelopmental disabilities participated in this IRB-approved study. Children who met the following inclusion criteria were accepted into the study: (1) were between the ages of 3 and 5 years old, (2) had a clinical diagnosis of a severe neurodevelopmental disability (e.g., ASD, Rett syndrome), (3) experienced significant delay in verbal communication skills (i.e., fewer than 5 spoken words or word approximations demonstrated within communication contexts) as documented by parent report and pre-intervention communication assessment, (4) did not use an AAC system independently, consistently, or accurately (i.e., fewer than 5 independent and accurate AAC requests demonstrated within communication context). Due to the use of remote telehealth coaching, it was necessary that the participants’ parents, who implemented the intervention, understood English and had access to high speed internet in their homes.
Demographic information was collected pertaining to the participants’ gender, age, comorbid motor or sensory impairment, scores on the Vineland Adaptive Behavior Scale (VABS; Sparrow et al. 2005), and speech, educational, occupational therapy, or related services received within the past year. Parents were asked to refrain from instructing the service providers to implement the study procedures (specifically FCT, including prompting the specific AAC modality used with the participant during the study). However, service providers targeted the participants’ individualized treatment plan goals, which may have included communication goals but did not include FCT or the modality of AAC targeted in the research study. All participants were referred to the study from their diagnosing clinical service providers. Participants received a clinical diagnosis (of either ASD or Rett syndrome) prior to entering the study; researchers confirmed the diagnosis with the clinicians via written records review (all participants) and verbal reports (Ella and Lily).
Ella
Ella, 3.5-years old, was diagnosed with ASD by a clinical service provider, and she received three mornings per week of early childhood special education (ECSE). She received clinic-based SLP services for 1 year prior to the study; however, services were discontinued during the study due to parental concerns over her lack of progress with her SLP goals. She had been on a waitlist for early intensive behavioral intervention (EIBI) services for 12 months. Her EIBI services began 2 weeks prior to the study and consisted of 3–9 h of in-home services per week. Ella scored in the low adaptive range in the VABS, Vineland II parental interview (defined as between 20 and 70 on the VABS; Sparrow et al. 2005). Ella’s parents reported that she babbled infrequently with consonant and vowel sounds and made several word approximations (i.e., “bye–bye”). Word approximations did not often occur within context (e.g., saying “bye–bye” when someone was leaving) and did not occur consistently (i.e., parents reported approximately 0–5 occurrences per day). Ella had previous exposure to three modalities of AAC: (1) the Picture Exchange Communication System (PECS; Bondy and Frost 1994), which was discontinued due to lack of progress before the study began; (2) ASL signs (the sign for “more” and “all done”), and (3) a GoTalk speech-generating device with a 6-symbol array, which was used at her ECSE program throughout the study. Her parents reported that she did not use any of these systems independently or consistently and that she frequently threw the speech-generating device. She engaged in frequent tantrums, which consisted of yelling, throwing objects, dropping to the floor, elopement, and attempted biting and hitting of parents and siblings. Study procedures were conducted in Ella’s home at the table in the kitchen and in the living room areas, with either her mother or father serving as the interventionist. Ella’s younger sibling was present for the sessions. Parents reported Ella aggressed towards her sibling at times; therefore, during sessions the sibling either was placed in her high chair with an activity within sight of the parent, or was tended to by an older sibling or the other parent in a different room.
Lily
Lily, 4-years old, was diagnosed with ASD, and she received three mornings per week of ECSE for the first 2 weeks of the study. For the remainder of the study she was on summer break from ECSE. She received clinic-based private SLP, occupational, and physical therapy one morning per week for 1 h each. She had been on a waitlist for EIBI for 16 months and remained on the waitlist for the duration of the study. While on the waitlist, her family received 1-h per week in-home behavioral consultation. Her service providers did not target the study procedures or intervention (her SLP had previously targeted the phrase “all done” with signs). Lily scored in the low adaptive range in the VABS, Vineland II parental interview (Sparrow et al. 2005). Lily’s parents reported that Lily babbled frequently and used several word approximations (i.e., ‘go’ and ‘three, four’); however these words often were not used in contextually relevant situations (e.g., she often said them when looking in the mirror or when viewing television shows) and she did not vocally imitate them (e.g., did not respond consistently to the instruction “Say ‘go’”). During play she used the word ‘go’ within social games when her parent said, “Ready, set.” Lily had previous exposure to two AAC systems: (1) ASL signs (“more”, “all done”, and “help”), and could independently make an approximation of the sign for “more” by clapping her hands together, although she did not consistently use this sign without prompting, and (2) a 2D symbol system that consisted of picture cards. She did not use either system independently or accurately to indicate her wants or needs. Her parent reported that with the 2D symbol system, Lily either threw the cards on the floor or played with them by tapping them against surfaces. Study procedures were conducted in Lily’s home with her mother serving as the interventionist. Study sessions occurred at either the table in the kitchen or in the connected living room area. The family’s nanny attended to Lily’s older and younger siblings for the majority of the sessions.
Sidney
Sidney, 3.5 years old, was diagnosed with Rett Syndrome, and she received ESCE four mornings per week. She also received private clinic-based SLP, occupational, and physical therapies twice per week. She was ambulatory; her gross motor skills consisted of the ability to walk, step up and down to navigate stairs with supervision, and to bend down and pick up or briefly hold small items. Sidney’s hand function included the ability to self-feed small pieces of food, to pick up light-weight items (e.g., pacifier, small book), and to press buttons to activate musical toys. She engaged in frequent repetitive behaviors of bringing her hands clasped together at midline, mouthing her hands, and mouthing other objects such as her clothing or safe beaded jewelry. She often wore soft bands around her wrists to prevent tissue breakdown due to mouthing her wrists. Sidney scored in the low adaptive range on the VABS, Vineland II parental interview (Sparrow et al. 2005). Sidney occasionally babbled sounds of “ma-ma” or “ba-ba.” She had exposure to two forms of AAC: (1) a 2D symbol system in which caregivers held up several pictures of preferred items and Sidney reached for one of the pictures, and (2) a microswitch with voice-output that was placed at the bottom of the staircase for Sidney to press for someone to assist her to go upstairs. She had made some progress with these methods, but did not use either method consistently in an independent or accurate manner. Study procedures were conducted in Sidney’s home with both her mother and father serving as the interventionists. Study sessions occurred at either the table in the kitchen or in the living room area. Either the parent who was not serving as interventionist at the time, a grandparent, or a babysitter was present and tended to Sidney’s baby sibling during study sessions.
Response Definitions and Data Collection
Idiosyncratic responses were selected and defined individually based on the observed behavior of each participant during assessment. Idiosyncratic responses were then measured during baseline and intervention sessions. AAC requests were the targeted communicative response during baseline and intervention sessions. Based on observations and discussion with parents, the first author identified a form of AAC that the participant could produce reliably. Ella: Idiosyncratic responding included (1) leading, defined as pushing a parent’s hand or body towards or away from items or referents in the area (e.g., pulling her parent toward the refrigerator, or pushing a parent’s hand towards the iPad), and (2) yelling, defined as loud vocalizations made with an open mouth and without consonant sounds. Ella’s AAC response was touching a PECS card or making a verbal approximation of the word (e.g., saying “mo” for “more”). If Ella threw the card, put it in her mouth, or brushed it onto the floor, it was not counted as an AAC request. Lily: Idiosyncratic responding included (1) reaching, defined as extending one or both arms towards her parent or an item, not including if an item was being handed to her, (2) clapping (described by parents to be an approximation of the manual sign for ‘more’), and (3) tantrums which included one or more of the following: crying, yelling, screaming, dropping to the floor, and aggression in the form of pushing, hitting, or pulling hair. Lily’s AAC responses included touching a PECS card or picking up the PECS card and handing it to her parent as well as any verbal words or approximations related to the item (e.g., “drink” or an approximation such as “swink” or a different but related word such as “juice”). Sidney: Idiosyncratic responding included (1) hitting the tray of her high chair: making physical contact with the high chair tray with one or both palms or fists, (2) reaching: extending one or both hands towards her parent or an item, not including if an item was being handed to her, and (3) approaching: walking towards parent within an arm’s length. Sidney’s AAC response was touching a Bigmack™ microswitch with enough force to activate voice output.
During the structured descriptive assessment for all participants, frequency data were collected on idiosyncratic responses and the responses per min were computed by dividing the number of idiosyncratic responses by session length (number of min). During the functional analysis and FCT with Ella, frequency (occurrence) was selected as the dependent measure for tantrums and for idiosyncratic and AAC responses because all sessions were exactly the same length (5 min). During Lily’s functional analysis, partial interval data on crying and whining were collected and are reported as percentage of 6 s intervals. Lily’s responses during baseline and FCT are presented as percentage of trials with an independent response due to varied session length. Specifically, Lily often slowly consumed the foods during the food condition (even with foods in small pieces, her consumption could take upwards 3 min during a single trial), therefore sessions consisted of a certain number of trials. During FCT with Sidney, frequency of her idiosyncratic and AAC responses was selected (occurrence) was selected as the dependent measure because all sessions were exactly the same length (5 min).
Trained observers collected direct observation data on the dependent measures throughout the study. Observers used event coding of the dependent variables from video recordings of baseline and intervention sessions, with the exception of crying and whining behavior with Lily, which was coded using 6 s partial intervals during sessions that lasted between 4.5 and 7 min. For all AAC requests, a request was counted if (a) the participant made the request spontaneously and independently, or (b) a parent made a verbal prompt towards the AAC card or switch (e.g., “you have to tell me what you want”) or delivered a gestural prompt (such as pointing at or tapping on the card or microswitch). A request was not counted if partial or full physical assistance was used to prompt the request. The authors trained the observers during practice sessions using videotaped sessions with the participants until inter-observer agreement on the dependent measures reached a minimum of 90% agreement.
Interobserver Agreement
Interobserver agreement (IOA) was coded for a minimum of 25% of randomly selected videotaped sessions. Interobserver agreement on the idiosyncratic and AAC responses was calculated as a trial-by-trial agreement in event recording between two independent observers. IOA for all participants on idiosyncratic and AAC responses was collected across a total of 30% of sessions (Ella and Sidney) and 25% of sessions (Lily). A breakdown of interobserver agreement across participants was as follows: (1) Ella: idiosyncratic responses had an average 91% agreement (range 78–100) and AAC responses had an average 93% agreement (range 84–100). (2) Lily: idiosyncratic responses had an average 89% agreement (range 67–100) and AAC responses had an average 91% agreement (range 67–100), and (3) Sidney: idiosyncratic responses had an average 94% agreement (range 85–100) and AAC responses had an average 97% agreement (range 92–100).
Study Sequence, Experimental Design, and Data Analysis
Before the study began, a functional assessment interview (FAI; O’Neill et al. 1997) and preliminary observations of free play sessions were conducted. Next, a structured descriptive assessment (SDA; Anderson and Long 2002; Freeman et al. 2000) was conducted using a multi-element design. The purpose of the SDA was to identify idiosyncratic responses and potential contexts/routines (e.g., snack time, activities of daily living such as hair brushing) to embed the functional communication training intervention.
If challenging behavior was observed during the SDA, a consequent-based functional analysis (FA) was conducted using a multi-element design (Iwata et al. 1982/1994) to provide evidence of functional relations between the challenging behavior and one or more social reinforcers. This was the case for Ella and Lily. The FA involved manipulating analog conditions in a counterbalanced manner with replication to demonstrate experimental control based on visual analysis of differentiated trend, level, and variability of the challenging behavior.
The effects of communication intervention (FC) were examined using an adapted multiple-probe design (Gast and Ledford 2014) across contexts/requests. The multiple probe design (MPD) involved collecting baseline data (i.e., differential reinforcement of the idiosyncratic response) across three communicative contexts that were identified during the SDA, FA, or both. The first context (e.g. snack time) was represented in the top panel of the graph, the second context (e.g., dinner time) was displayed in the middle panel, and the third context (e.g., access to TV) was displayed in the bottom panel. After a minimum of five baseline data points were collected in the first context (top panel), FCT intervention (i.e., differential reinforcement of the AAC response) was introduced in that context. When the intervention data met criterion (3 consecutive data points with the AAC request occurring at a higher level than the idiosyncratic request without data overlap), FCT intervention was introduced in the next context (middle panel). This was repeated for the third context. During the first session of FCT, on the first trial, a signaled cue was provided in the form of a prompt (i.e., physically placing the participant’s hand on the switch or picture card) to indicate that the AAC response was now required for reinforcement. After this initial cue, a 10 s time delay with a most-to-least prompt hierarchy was used, if needed, throughout the remainder of FCT intervention sessions.
In addition, an ABAB (Birnbrauer et al. 1974) design was embedded in the first context (panel) of the multiple probe design for all participants. The purpose of the ABAB design was to strengthen the internal validity of the design by alternately replicating the effect of contingent reinforcement on the idiosyncratic and AAC responses. In the (‘A’) conditions, baseline procedures were implemented. Specifically, the reinforcer hypothesized from the SDA or identified in the FA was delivered contingent on idiosyncratic behavior. The AAC stimuli (e.g., PECS cards) were present during the (‘A’) sessions, but did not produce reinforcement. For Sidney, the microswitch was present but the vocal output was turned off. The (‘A’) sessions served as a baseline comparison for the FCT intervention (‘B’) sessions. During the (‘B’) sessions, FCT, or differential reinforcement of the AAC response was implemented. Specifically, the same functional reinforcer was delivered contingent only on activation of the AAC response and the idiosyncratic response was placed on extinction. A minimum of three sessions were conducted in each condition of the ABAB design to allow for established patterns of responding to be observed.
The authors conducted a visual analysis of the data in order to draw conclusions during assessment with the SDA, FA, and during intervention with the adapted MPD. SDA data were analyzed through the number of different idiosyncratic responses occurring across contexts and changes in level of occurrence of idiosyncratic response across contexts. FA data were examined for differences in level, trend, and variability across analog conditions. Intervention data were visually analyzed for changes in trend, level, and variability in idiosyncratic and AAC responses between DRA of the idiosyncratic response (A) and DRA of the AAC response (B) phases of the study.
Materials
Telehealth equipment was used in the University based lab (the research team’s equipment for delivering coaching, videotaping sessions, and data collection purposes) and on the user end (the families’ and participants equipment to receive the coaching and implement the procedures). AAC equipment and materials were used throughout the study.
Tele Lab Equipment
The telehealth coaching sessions occurred in the Telepresence Behavior Lab (TBL) to connect the coach with the family and the participants via video conferencing equipment. The following equipment was used: screen-recording software (Debut) on a dedicated computer (Dell OptiPlex 3010 Desktop) with Dell 24in monitor, Logitech HD Pro Webcam C920, Logitech ClearChat Comfort/USB Headset H390, Polaroid 8″ Heavy Duty Mini Tripod, secure Internet connection through the University server, and secure storing of data and files on the University system. The video conferencing software used was Google Hangout, a free, secure, web-based application. The coach used a timer to monitor session duration, and occasionally used examples of the picture cards (Ella and Lily) or a microswitch (Sidney) to demonstrate prompting techniques to the parent. The data coders used a Sper Scientific 6 s interval-recording timer for measures requiring partial interval recording.
Telehealth User-End Equipment
The University of Minnesota Telepresence lab retained a lending library of telehealth equipment kits to provide when families needed equipment for the duration of the study. Due to the video quality and the broad view required to capture the participants, all of the participants used the Logitech HD Pro Webcam C920 instead of the internal webcameras on the computers. Ella’s family used the webcamera with a tripod connected to their personal computer (a Macintosh desktop computer). Lily’s family used the webcamera with a tripod connected to their personal computer (a Macintosh desktop computer). Sidney’s family used a full telehealth kit, which included a Dell Latitude E6430 premier laptop, Logitech HD Pro Webcam C920, 1090p, and a Polaroid 8in Heavy Duty Mini Tripod. Therapists provided caregivers with a University of Minnesota Telepresence Lab Manual that contained a task analyses with computer screen shot images for parents to reference for technology set-up and for technology trouble-shooting. The following training formats were given to parents: (1) a paper-copy of the manual, (2) an electronic copy of the written manual, and (3) an electronic copy of a video training module demonstrating connecting equipment (e.g., plugging in the webcam), answering video conferencing calls, and changing settings for connectivity bandwidth, audio, and video.
Coaches also provided each participant with AAC equipment in modalities that matched her motor repertoire. Ella and Lily were provided with 2D PECS cards. Ella used two cards; the cards were colored with white backgrounds and were approximately 3.5″ × 2.5″. The “more” card had hands making a “more” sign and the “all done” card showed a person’s body and hands making the sign for “all done”. Lily used four cards; all were similar sizes (approximately 3″ × 2.5″), colored with white backgrounds and outlines. Four of the cards had photographs as symbols (“food”, “drink”, “playdoh™,” and “bubbles”) and one of the cards contained a line drawing for “all done” with the same symbol as Ella’s. Sidney used a BigMack™ microswitch (5″ × 6″) without an icon displayed. The microswitch produced the voice output “more” when activated.
Procedures
Pre-intervention Assessment
The coach conducted a functional assessment interview with one of the parents during a phone call to identify idiosyncratic or challenging behaviors and to identify environmental contexts in which they occurred (O’Neill et al. 1997). The expanded interview form of the Vineland Adaptive Behavior Scales (VABS; Sparrow et al. 2005) was used to gather information about the participant’s communication, functional, and motor skills; the VABS provides detailed information about communication, functional, and motor skills for individuals with severe disabilities.
Structured Descriptive Assessment (SDA)
Beginning in the second telehealth session, the coach provided instruction remotely via telehealth to the parent to conduct the sessions of a SDA (Anderson and Long 2002; English and Anderson 2006; Freeman et al. 2000). The goal of the SDA was to document the occurrence of idiosyncratic responses, challenging behavior, or both, across contexts. Each participant was exposed to 5 min sessions each of a variety of antecedent conditions or routines, designed to reflect parent report during the FAI. The interventionist coached the parent to set up the condition (i.e., snacks, activities of daily living such as hair brushing) and instructed the parent to “respond how you normally would” to any challenging behavior. The interventionist did not coach any programmed consequences. The conditions were presented in a counterbalanced sequence.
For Ella, restricted access to Playdoh™ and to snack and drink were examined, as well as a diverted attention condition in which her parents attended to a younger sibling and a task demand to place the pieces of a 3D puzzle. For Lily, restricted access to Playdoh™ or other toys and restricted access to food were examined as well as diverted attention, during which her mother turned away from Lily to attend to others in the room, and a task demand to complete a sorting task. For Sidney, restricted access to food in the high chair and in the living room were examined as well as diverted attention, during which Sidney’s parents engaged with her younger sibling or looked at a book.
Functional Analysis Procedures (FA)
An FA was conducted with Ella and Lily after challenging behavior was observed during the SDA. The observed parental responses to the challenging behavior during the SDA conditions were integrated into the programmed consequences of the FA in order to create conditions that were analogous to and representative of the naturally occurring interactions. The coach instructed the parents remotely from the lab to conduct the FA. The FA involved exposing the participant to up to 5 sessions each of a series of conditions designed to test specific social functions (e.g., access to social interaction/attention, removal of task/escape). All FA sessions lasted 5 min with no more than 10 sessions (50 min) conducted in a single day. Coaching instructions were delivered verbally and via email before the beginning of the session. The coach provided live feedback and instructions during the FA sessions and provided the parent with more specific instructions than during the SDA. The majority of instructions pertained to the parent: (1) presenting the establishing operation (e.g., withholding a preferred item), (2) providing immediate contingent access to the programmed consequence for challenging behavior, (3) withholding the programmed consequence in response to other forms of responding from the participant (e.g., withholding the programmed consequence for appropriate responding, such as the participant making the sign for “more”), and (4) the parent reinstating the establishing operation by restricting access or placing demands. An elevation in the challenging behavior across sessions within a particular condition was indicative of a functional relation, specifically, a social reinforcer for the specified challenging behavior. The FA continued until one or more social functions of challenging behavior was identified.
Parent-Implemented Functional Communication Training (FCT)
The purpose of the intervention phase was to examine the extent to which the three participants acquired the aided AAC requests during parent-implemented FCT that was embedded into three routines and coached via telehealth. The AAC requests were identified for each participant across three contexts (see Table 1 for a detailed description of contexts and AAC requests). Up to 7 sessions were conducted per day and sessions lasted 5 min (Ella and Sidney) and for 3 trial blocks (Lily). Sessions were terminated early if the child refused the reinforcing item (e.g., food) for 1 min or longer following parent attempts to re-engage the child in the reinforcing item (e.g., holding the item closer to the participant, taking the lid off of the bubbles).
Table 1.
Contexts, requests, camera placement
| Participant and request | AAC request | Context | Camera placement |
|---|---|---|---|
| Ella ‘snack’ | Touch PECS card “more” color | At kitchen table, in chair with parent in chair on her side | Camera on tripod on desk approximately 6 feet away |
| Ella ‘video’ | Touch PECS card “more,” color | At kitchen table, in chair, with parent in chair on her side | Camera on tripod on desk approximately 6 feet away |
| Ella ‘break’ | Touch PECS card “bye-bye”, color | At kitchen table in chair, with parent in chair on her side | Camera on tripod on desk approximately 6 feet away |
| Lily ‘food/drink’ | Touch PECS card from field of 2, “food” or “drink” or verbal approximation of either word | At kitchen table, in high chair, with parent seated next to her | Camera on tripod on desk, approximately 5 feet away |
| Lily ‘playdoh’ | Touch PECS card from field of 1, “playdoh” or verbal approximation of “playdoh”, “open,” “more,” “more playdoh” | Parent holding Playdoh and interacting with Lily, mirror placed at back of couch, Lily walking around or standing at table | Camera on tripod on desk, turned to follow her when needed, between 5 and 10 feet away |
| Lily ‘break’ | Touch PECS card from field of 1, “all done” or verbal approximation of “all done” | Parent bringing Lily to table with task placed on it (sorting game, blocks to stack, beads to string) | Camera on tripod on desk approximately 5 feet away |
| Sidney ‘food/drink’ | Press BigMack microswitch with voice output “more” | Sidney seated in high chair with parent seated across from her. Sibling seated with grandparent or babysitter | Laptop on kitchen table with camera on tripod in front of Sidney, camera approximately 2–3 feet away |
| Sidney ‘snack’ | Press BigMack microswitch with voice output “more” | Sidney in living room, parent seated on floor next to her, microswitch placed on couch, sibling in living room or other room with other caretaker | Laptop on opposing couch, tripod on coffee table across from parent and Sidney, approximately 6 feet away |
| Sidney ‘parent attention’ | Press BigMack microswitch with voice output “more” | Sidney in living room, parent seated on floor microswitch placed on couch, sibling in living room or other room with other caretaker | Laptop on opposing couch, tripod on coffee table across from parent and Sidney, approximately 6 feet away |
Baseline (Differential Reinforcement of the Idiosyncratic Response)
In the baseline phase for each routine, each occurrence of the identified idiosyncratic response(s) was reinforced. The AAC stimulus (card(s) or switch) was present in the baseline sessions but the participant was not prompted to engage in the AAC request, nor did occurrences of the AAC request produce access to the reinforcer (extinction). For Sidney, the vocal output on the microswitch was turned off during all baseline sessions.
Baseline arrangements were designed to: (1) serve as an analog to how parents responded to the idiosyncratic responses prior to introduction of the AAC response, and (2) to isolate the effects of differential reinforcement (the active ingredient of FCT) on the idiosyncratic and AAC responses. Sidney’s switch was turned in the ‘off’ mode for baseline to serve as an analog to natural conditions which may occur in which the switch would not receive reinforcement (e.g., the switch is turned off or batteries are dead).
Functional Communication Training (FCT)
Following baseline, the FCT intervention (differential reinforcement of the AAC response) was embedded into the three routines identified for each participant. The interventionist coached the parent via telehealth to implement the routine and to deliver reinforcement contingent on each occurrence of the AAC request and extinction for the idiosyncratic response(s). During the FCT sessions, the communicative context related to the social function was used in the intervention setting; therefore, the antecedent stimulus was presented (e.g., the participant was seated in her high chair and the parent held snack out of participant’s reach) and the maintaining social consequence was provided contingent on each AAC request (e.g., the parent gave the participant a bite of a snack). Parents were coached to use a most-to-least prompting hierarchy (Berkowitz 1990; MacDuff et al. 2001) combined with a time delay (Char-lop et al. 1985) were used as necessary to teach the AAC request.
Parent-Coaching Strategies.
Prior to sessions that contained changes to procedures (e.g., moving from FA to intervention) the coach emailed the parent a brief summary of the steps that would be executed during the upcoming session. During the sessions, coaches primarily provided verbal instructions and feedback to the parent, combined with some demonstrating how to physically prompt the AAC response using AAC stimuli in the telehealth laboratory.
Fidelity
Fidelity to study procedures was measured during 20% of baseline and intervention sessions for each participant as a percentage of the critical steps of baseline and intervention sessions that were implemented. Despite slight variations across individualized protocols for the participants, broadly defined steps were listed in the task analysis of baseline (6 steps) and intervention (7 steps, with the inclusion of the prompting procedures) sessions for use with all three participants. The task analyses contained steps related to: (1) session set-up, (2) pre-session access to the preferred item/activity, (3) onset procedure to begin a trial, (4) execution of the prompting procedure (intervention only), (5) immediate delivery of the reinforcer contingent on either the idiosyncratic response (baseline) or the AAC response (intervention), and (6) extinction of either idiosyncratic response (intervention) or the AAC response (baseline), and (7) adherence to early session termination criteria (participant refusing reinforcer for longer than 1 min). The steps could be scored as correct if either the coach prompted the parent to execute the step or the parent independently implemented the step. If any steps were skipped or a fidelity error occurred, the coach provided corrective feedback to the parent. Overall fidelity averages were as follows: Ella 96% (range 83–100), Lily 93% (range 71–100), and Sidney 94% (range 83–100).
Parent Ratings of Treatment Acceptability
Parent rating of treatment acceptability was measured and analyzed through descriptive methods. A modified version of the Treatment Acceptability Rating Form-Revised (TARF-R; Reimers and Wacker 1988; Reimers et al. 1991) was administered in a similar method to Suess et al. (2014). The TARF-R is a questionnaire that consists of 21 items in a 7-point Likert-type rating scale; 17 items are related to measures of parent’s perception of acceptability and 3 items are related to parent’s perception of the severity of the problem. In the current study, the TARF-R was slightly modified to align the TARF-R with the communication aspect of the primary research question of the study; items 4, 7, 10, 18, and 21 were modified to include the terms and/or communication.
Results
Ella
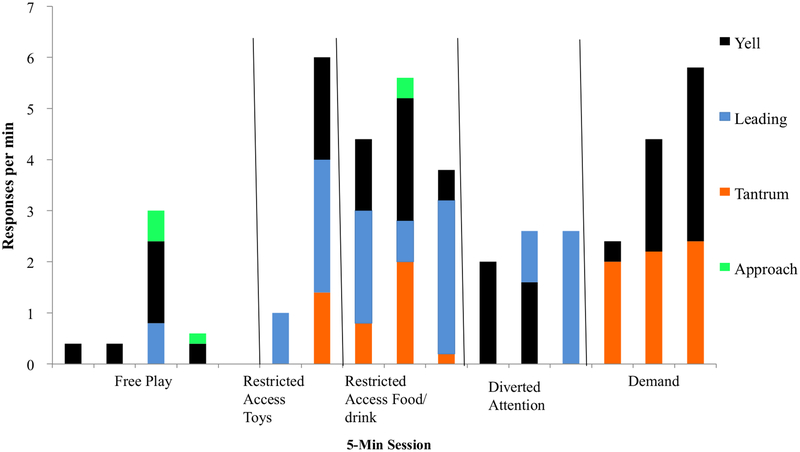
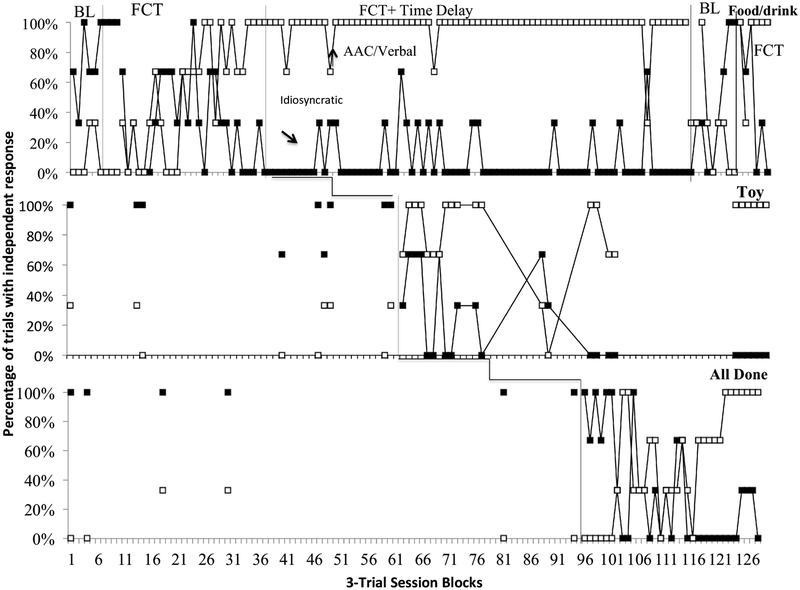
Ella’s pre-intervention assessment data are shown in Fig. 1 (SDA), 2 (FA), and intervention data are shown in Fig. 3.
Fig. 1.
Results of Ella’s structured descriptive assessment (SDA) of idiosyncratic response topographies across contexts of free play, restricted access to tangibles (Food/drink and videos), diverted parental attention, and demands (completing puzzle at the table with parent). Data are depicted in non-sequential order, by context, to aid in visual analysis of response topographies occurring in each context
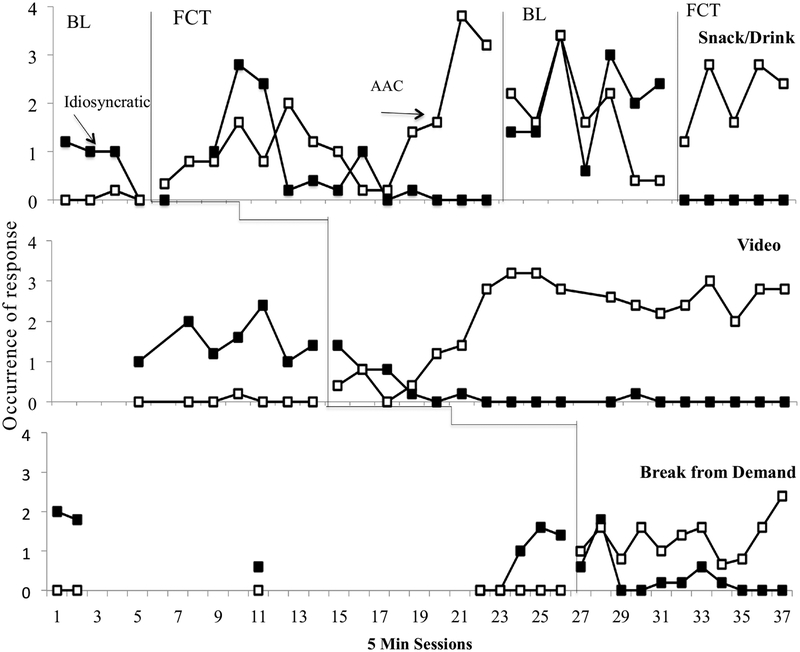
Fig. 3.
Ella MPD. Occurrences of responses of idiosyncratic responses (leading or tantrums) and AAC (touching or handing a PECS card and/or verbal approximation) across three contexts: snack/drink: (panel 1; idiosyncratic = leading parent: AAC = PECS “more”), video (panel 2; idiosyncratic = leading parent: AAC = PECS “more”), and demand/break (panel 3; idiosyncratic = yelling: AAC = PECS “all done”). Baseline (BL) = differential reinforcement of alternative response (idiosyncratic response) in baseline and FCT = differential reinforcement of alternative response (AAC and/or verbal response)
Ella SDA (Fig. 1)
Ella’s father (days 1 and 2) and mother (days 2, 3, 4) conducted the SDA, which lasted for a total of 4 session days and consisted of 17 total sessions and 5 conditions (see Fig. 1). Ella engaged in multiple topographies of idiosyncratic and potentially communicative responses across contexts. The three contexts with the highest level of overall responding were: (1) restricted access to food (M = 4.8 responses/min), (2) restricted access to toys (M = 6 responses/min), and (3) demands (M = 2.2 responses/min). The most frequently observed topography for both restricted access to food (M = 2.0 responses/min) and restricted access to toys (M = 2.6) was lead parent. Yell and tantrum were the only idiosyncratic topographies observed in the demand context occurred at the same level (M = 2.2 responses/min), with yell proceeding tantrums in most occurrences. It was noted that yell preceded tantrum in most occurrences. Lower levels of overall idiosyncratic topographies were observed in both free play (M = 0.5 responses/min) and diverted attention (M = 1.85 responses/min).
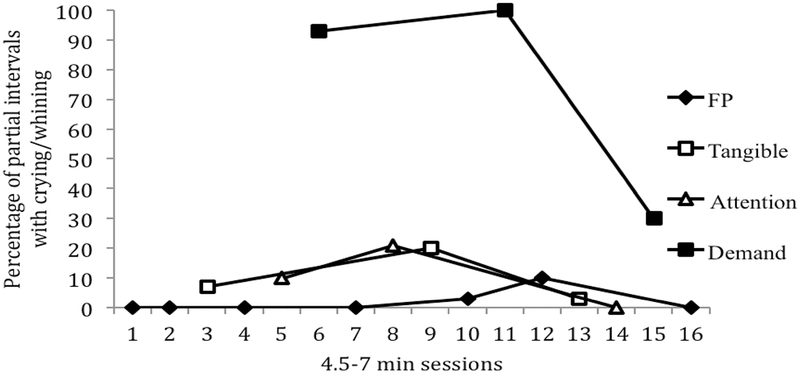
Ella FA (Fig. 2)
Fig. 2.
Functional analysis (FA) results for Ella’s tantrum responses
Due to the presence of challenging behavior in the form of tantrums during the SDA for Ella, an analog FA was conducted. Ella’s father (day 1) and mother (days 2, 3, 4) conducted the FA, which lasted for a total of 4 days, 14 sessions, and 4 conditions (see Fig. 2). In the FA, contingent reinforcement was arranged for tantrum behavior across analog conditions of free play, escape, tangible, and attention conditions. A high level of differentiation in tantrums occurred in the escape condition (M = 6.7). An elevated level of tantrums was also observed in the tangible condition (M = 2.3). Low and stable levels of tantrums were observed in the attention condition (M = 0.7) and free play (M = 0.1). Based on the results of the FA, escape and tangible functions were identified for Ella’s tantrums.
Ella Parent-Implemented FCT Across Contexts (Fig. 3)
For Ella, the three communicative contexts selected based on behavior observed during the SDA and FA were (1) access to snack/drink (Fig. 3, top panel), (2) access to video (Fig. 3, middle panel), and (3) escape from demands (Fig. 3, bottom panel). Ella’s requests consisted of “more” during both access to food/drink (Fig. 3, top panel) and access to a video (Fig. 3, middle panel), and “bye–bye” (i.e., break) during a demand condition (Fig. 3, bottom panel).
In baseline sessions across the contexts, there was low and stable occurrence of the AAC request (M = 0.01 across all baseline sessions). The level of idiosyncratic responding in baseline was differentiated from AAC requests in all but 2 of 18 sessions (both idiosyncratic behavior and AAC requests occurred 0 times in 1 baseline session of snack/drink and 2 baseline sessions of break).
Snack/Drink.
Upon introduction of FCT with differential reinforcement for the AAC response “more” to the snack/drink context, there was a small, immediate change in level of AAC requests for “more” (up from, M = 0–0.33) with an increasing trend across sessions. Following introduction of the intervention, an increasing trend in the idiosyncratic response was observed (range 0–2.8) until session 5.
A reversal to baseline was introduced beginning in session 19. There was an immediate change in level of both the idiosyncratic response (up from, M = 0–1.4) and the AAC request (down from, M = 3.2–2.2), and a high degree of variability and overlap between the two responses during the first 4 sessions (sessions 19–23) of the reversal. Following session 23, improved stability and differentiated rates (higher level of idiosyncratic responses and lower level of AAC responses) were observed and remained in the same pattern for the remainder of the reversal phase. Upon reinstatement of differential reinforcement of the AAC response, there was an immediate change in level of occurrence of both the idiosyncratic (down from, M = 2.4–0) and the AAC request (up from, M = 0.4–1.2). An overall level change with stable and differentiated responding was observed in all sessions of the final phase with idiosyncratic responses not occurring (M = 0: range, 0), and AAC requests elevated (M = 2.2: range 1.2–2.8).
Video.
Baseline occurrence of AAC (M = 0.1) and idiosyncratic responses (M = 1.5) remained stable in the video context (middle panel) during baseline sessions. In the first four sessions of intervention in the video context, AAC requests for “more” remained low and variable and idiosyncratic responses did not immediately change in level. However, beginning in session 5 and throughout the remainder of the intervention phase, AAC requests increased and idiosyncratic responses decreased.
All Done.
Idiosyncratic and AAC responses were probed across baseline sessions in the all done context (bottom panel). AAC responses of “bye–bye” never occurred during baseline and idiosyncratic responses were somewhat variable (M = 1.1; range 0–2). Upon introduction of the intervention in the all done context, AAC requests immediately increased in level and idiosyncratic requests quickly dropped to zero and rarely occurred in the remaining sessions.
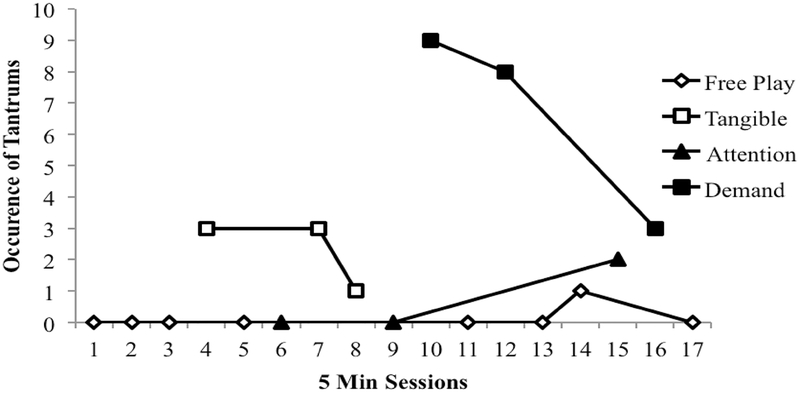
Lily
Lily’s pre-intervention assessment data are shown in Fig. 4 (SDA), 5 (FA), and intervention data are shown in Fig. 6.
Fig. 4.
Results of Lily’s structured descriptive assessment (SDA) of idiosyncratic response topographies across contexts of free play, restricted access to tangibles (food/drink, bubbles, and Playdoh™ items), demands (completing sorting task at the table with parent), and diverted parental attention. Data are depicted in non-sequential order, by context, to aid in visual analysis of response topographies occurring in each condition type
Fig. 6.
Lily MPD. Percentage of trials of idiosyncratic and potentially communicative response (reach, clap, and tantrums) and AAC response with (touching a PECS card or verbal approximations) across three contexts: food/drink context [panel 1: idiosyncratic = leading: AAC = PECS “food” and “drink” and verbal approximations of either word or a related word (e.g., “juice”)] toy context [panel 2: idiosyncratic = leading: AAC = PECS “playdoh” and “bubbles” and verbal approximations of either word or related word (e.g., “blow”)], and demand/break context (panel 3: idiosyncratic = tantrums: AAC = PECS “all done” or verbal approximation of word)
Lily SDA
Lily’s mother conducted all of the SDA. The SDA was conducted across 3 days, 14 sessions and 5 conditions (see Fig. 4). Lily engaged in multiple topographies of idiosyncratic and potentially communicative responses across contexts. The three contexts with the highest rate of overall responding per min were: (1) demand (M = 5.5), (2) restricted access to food (M = 3.1), and (3) restricted access to toys (M = 0.84). Cry/tantrum were the most frequently observed topographies in the demand context (M = 5.1). Reach (M = 1.6) and clap (M = 1) occurred at the highest rate in the restricted access to food context. Lower rates of overall idiosyncratic topographies were observed in diverted attention, (M = 1.6), restricted access to drink (M = 1.2), and free play (M = 0.34).
Lily FA
Due to the presence of challenging behavior in the forms of crying and whining during the SDA, an analog FA was conducted for Lily. Lily’s mother conducted all of the FA with assistance from her father for sessions on the 3rd day. The FA was conducted across 3 days, 14 sessions, and 4 conditions (see Fig. 5). Contingent reinforcement was arranged for cry/whine behavior across analog conditions of free play, escape, tangible, and attention conditions during the FA. Cry/whine was elevated most during the escape condition (M = 74%). Low and stable levels of cry/whine were observed across the other conditions as follows: (1) attention and tangible conditions both at (M = 10%), and (2) free play (M = 2%). Based on the results of the FA, an escape function was identified for cry/whine.
Fig. 5.
Functional analysis (FA) for Lily’s crying and whining responses
Lily Parent-Implemented FCT Across Contexts (Fig. 6)
The three communicative contexts selected from the SDA for Lily were (1) access to food/drink (Fig. 6, top panel), (2) access to toys (Fig. 6, middle panel), and (3) break from demands (Fig. 6, bottom panel). Lily’s requests consisted of “food” and “drink” during access to food and drink (Fig. 6, top panel), “playdoh” during access to toys (Fig. 6, middle panel), and “all done” during the demand condition (Fig. 6, bottom panel).
Food/Drink.
During baseline, Lily rarely used the AAC request and engaged in idiosyncratic responses in 70% or more of the trials in all but one session. Upon initial introduction of differential reinforcement for AAC and verbal requests for “food” and “drink” in the food/drink context, the data for both AAC requests and idiosyncratic responses were highly variable. After session 11, AAC responses increased to 70% or more of the trials with independent AAC responses in all but one session, and idiosyncratic responding occurred in 30% or less of the trials in the majority of sessions. The overall mean for AAC responses during the first intervention phase was 87% whereas the overall mean for idiosyncratic responses was 14%.
A reversal to differential reinforcement of the idiosyncratic response occurred beginning in session 113 and lasted until session 121. There was immediately decrease in the AAC request to a lower percent (down from 100 to 33%), followed by an overall low level throughout the reversal phase (M = 29%). Idiosyncratic responding did not have an immediate level change (remained flat, 0–0%); however, an increasing trend began on the 6th session of the reversal phase and continued until it stabilized at a higher percentage throughout the remainder of the phase (M = 41%). There was a moderate degree of overlap between AAC and idiosyncratic responding; overlap occurred for 3 out of the 9 reversal sessions. Upon reinstatement of the intervention in the final phase, an immediate increase in AAC requests was observed (up from 0 to 100%). The AAC request remained high and stable for all sessions of the phase. In the final intervention phase, the percentage of idiosyncratic responses initially remained unchanged and then decreased and remained low.
Toys.
Probes of idiosyncratic and AAC responses were conducted in the toys context. Prior to intervention in the toys context, idiosyncratic responses consistently occurred more than AAC responses occurred. Upon introduction of reinforcement for AAC in the toy context (middle panel), the AAC request for “playdough” immediately increased in occurrence and despite some variability, remained elevated throughout the phase. Idiosyncratic responses immediately decreased in level and despite some variability, remained low throughout the intervention phase.
All Done.
Probes of idiosyncratic and AAC responses were conducted in the all done context (bottom panel). During the first several sessions of reinforcement for the AAC response “all done”, idiosyncratic responding remained elevated and AAC responses did not occur. After 7 sessions of extinction of the idiosyncratic response and programmed reinforcement for the AAC response, AAC responses began to occur and idiosyncratic responses began to decrease. After a period of variability and overlap between the two responses, AAC responses increased to 100% and idiosyncratic responses decreased to lower levels (range 0–30% of trials).
Sidney
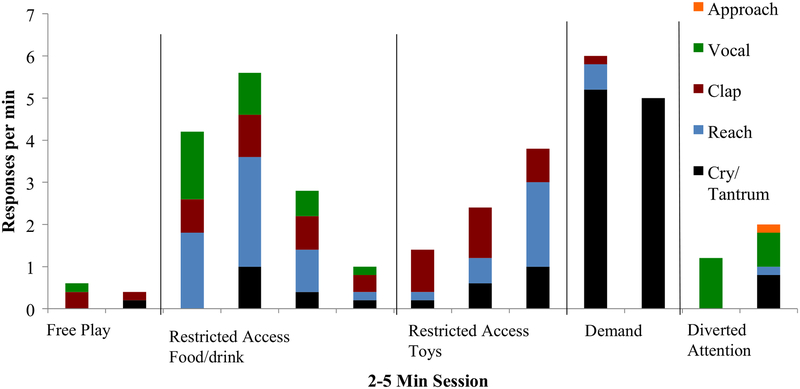
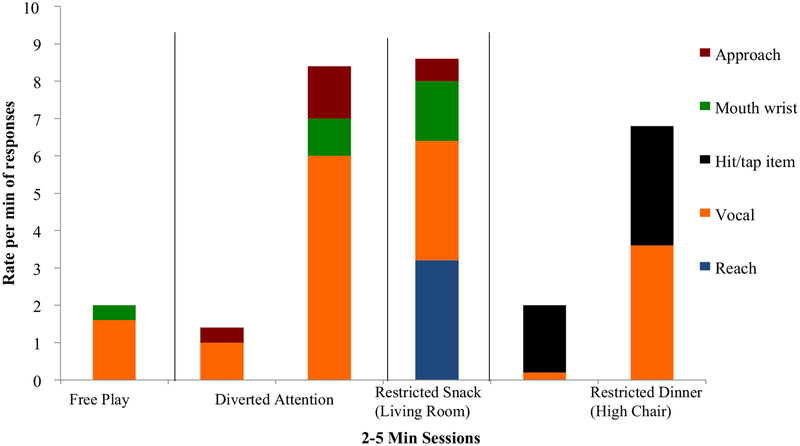
Sidney’s pre-intervention assessment data are shown in Fig. 7 (SDA) and intervention data are shown in Fig. 8.
Fig. 7.
Results of Sidney’s structured descriptive assessment (SDA) across idiosyncratic responses and contexts
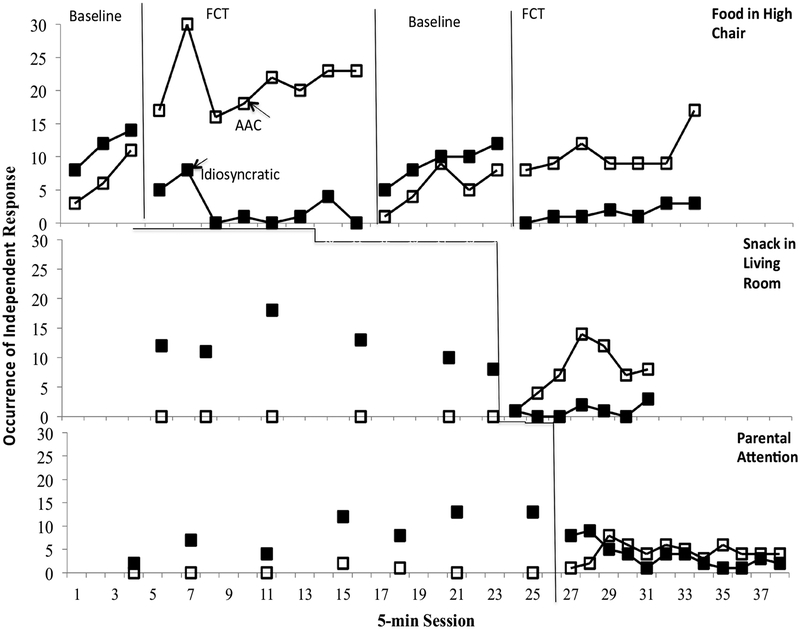
Fig. 8.
Sidney MPD. Occurrences of idiosyncratic and potentially communicative response (hit hand on high chair tray, reach, and approach) and AAC response (press a microswitch) across three contexts: food in high chair context (panel 1: idiosyncratic = hit high chair tray: AAC = microswitch “more”) snack in living room context (panel 2: idiosyncratic = reach: AAC = microswitch “more”), and parental attention context (panel 3: idiosyncratic = approach parent: AAC = microswitch “more”)
Sidney SDA (Fig. 7)
Sidney SDA. Sidney’s father (day 1) and mother (day 2) conducted the SDA, which lasted for a total of 2 days, 11 sessions, and 4 conditions (see Fig. 7). Sidney demonstrated multiple topographies of idiosyncratic and potentially communicative responses across all contexts. The contexts with the highest rate per min of overall idiosyncratic responding were: (1) restricted access to snack in living room (snack in LR: M = 8.6), (2) restricted access to food in the high chair (food in HC: M = 4.4), (3) free play (M = 2), and (4) diverted parental attention (parental attention: M = 1.9). Vocalizations were observed across all contexts at a high rate per min (M = 2.6 per context). Therefore, due to the likelihood that vocalizations may not have been socially mediated, the data were re-examined with the removal of vocalizations from the total. Without vocalizations, the rate of idiosyncratic responding were as follows across contexts: (1) snack in living room (M = 5.4), (2) food in high chair (M = 2), (3) parental attention (M = 1.4), and (4) free play (M = 0.4). Reaching was the most common idiosyncratic topography in snack in the living room (LR) (M = 1.6 responses per min). Hit/tap items (the high chair tray) was the most common idiosyncratic response during restricted access to food in the high chair (HC) (M = 2.5 responses per min). Approach parent was the most common idiosyncratic response in the parental attention context (M = 1.4 responses per min).
Sidney Parent-Implemented FCT Across Contexts (Fig. 8)
The three communicative contexts selected from the SDA for Sidney were (1) access to food in HC (Fig. 8, top panel), (2) snack in the living room (Fig. 8, middle panel), and (3) parental attention (Fig. 8, bottom panel). Sidney’s requests across contexts consisted of “more” during access to food/drink in her high chair (Fig. 8, top panel), access to a snack in the living room (Fig. 8, middle panel), and access to parental attention (Fig. 8, bottom panel).
Food in HC.
During baseline, both idiosyncratic and AAC responses occurred, but idiosyncratic responses consistently occurred more than AAC responses. When reinforcement for the AAC request for “more” was introduced in the food in high chair context, there was an immediate and consistent elevation of AAC requests above the baseline level and there was an immediate and sustained decrease in the occurrence of idiosyncratic responding. No overlap occurred between AAC and idiosyncratic responding for any of the 8 intervention sessions.
A reversal to differential reinforcement of the idiosyncratic response was implemented in sessions 12 through 16. AAC requests immediately dropped and consistently occurred less than idiosyncratic responses occurred. No overlap occurred between the AAC and idiosyncratic responses for any of the 5 reversal sessions. Upon reinstatement of differential reinforcement for AAC responses in the final phase, the idiosyncratic response immediately decreased in level of occurrences (from 12 to 0) while AAC responses remained elevated with no overlap between the two responses.
Snack in LR.
Idiosyncratic behavior consistently occurred more than AAC responses during baseline probes in the snack in living room context (middle panel). Upon introduction of reinforcement for AAC the response “more”, idiosyncratic responses dropped to zero or near zero for the remainder of the sessions while AAC responses consistently occurred more than five times per session after the first session.
Parental Attention.
During baseline probes in the parental attention context (bottom panel), AAC responses almost never occurred, whereas the occurrence of idiosyncratic responses was elevated and variable across probes. Upon introduction of reinforcement for the AAC response “more” in the parental attention context, idiosyncratic responding dropped and AAC responses occurred slightly more than idiosyncratic responses. Given the variability in both responses, there was little separation between the responses in the final phase.
Parent Ratings of Treatment Acceptability
For all participants, parents’ rated overall treatment acceptability as ‘highly acceptable’ on the Treatment Acceptability Rating Form-Revised items (TARF-R; Reimers and Wacker 1988; Suess et al. 2014; Wacker et al. 2013a, b) with an average score of 6.91 (range 6.88–6.95). Parents’ ratings of acceptability on items directly related to improvement in challenging behavior and/or communication (items 4, 7, 10, 18, 21) was an average of 7 or ‘highly acceptable.’
Discussion
The current study examined the extent to which three young children with severe neurodevelopmental disabilities acquired AAC responses during parent implemented FCT embedded across three contexts in which the children were previously displaying idiosyncratic and potentially communicative responses. Telehealth technology was used to coach parents to conduct the assessment and intervention procedures. During baseline conditions, the identified idiosyncratic response was differentially reinforced and occurred more than the AAC response. In subsequent intervention phases, when reinforcement was delivered contingent on an AAC response and withheld for the idiosyncratic responses, AAC responses were established or strengthened for all participants in all contexts. These findings are among the first to demonstrate a functional relation between the idiosyncratic responses and maintaining reinforcers. Specifically, the AAC response increased and the idiosyncratic response decreased when differential reinforcement was applied to the AAC response and this effect was replicated for all three participants. These results build upon previous findings that idiosyncratic responses may serve as behavioral indicators for where to begin communication intervention that is focused on requesting skills (Drasgow et al. 1996; Keen et al. 2001).
The results of the current investigation are promising. Two participants acquired multiple AAC responses across three contexts (Ella and Lily) and one participant acquired an AAC response across three contexts (Sidney); whereas, during naturally occurring routines and daily activities prior to intervention, none of the participants engaged in neither reliable nor easily recognizable communication forms. When AAC requests were taught and differentially reinforced, decreases in idiosyncratic responding was observed. For Ella and Lily, there was often overlap between the idiosyncratic and AAC responses at the beginning of the first phase of differential reinforcement of the AAC response. Several potential reasons for this pattern may be related to the functional equivalence of the effort of the responses. First, the participants were physically capable of producing the AAC response but required initial prompting to engage in the AAC response correctly at the trial onset. Second, intermittent reinforcement schedules can cause the idiosyncratic response to persist. In the current investigation, although the idiosyncratic responses did not produce reinforcement during experimental sessions, those responses did produce reinforcement in the same contexts outside of experimental sessions. In addition, for some participants, while some idiosyncratic response forms were on extinction in one context (e.g., intervention in the first context), they were reinforced in another context (e.g., baseline in the second context), possibly making it difficult to immediately discriminate the change in contingencies at the onset of a new phase. Third, functional equivalence is a fundamental principle of FCT intervention. For an alternative behavior (e.g., AAC response) to effectively compete with a response (e.g., idiosyncratic response) the responses should be similar in response effort (Horner and Day 1991). In cases where it took several sessions before the idiosyncratic response decreased, it may have been less effortful than the AAC response or it may have become chained with the AAC response (e.g., the participant first attempted the idiosyncratic response prior to the AAC response). Clearly, the idiosyncratic responses had a longer reinforcement history than the AAC responses, therefore one might expect them to persist longer. These speculations point to the need to further examine the findings of the current investigation and whether this approach would be effective for more subtle and more or less effortful response forms (e.g., eye gaze).
FCT as Early Communication Intervention
Despite much of the existing literature focused on FCT as an intervention with the primary purpose of decreasing challenging behavior, the current study provides support for FCT as an initial or early communication intervention strategy to establish AAC communication in contexts where idiosyncratic responses may have been functioning as communicative. The success of the current investigation builds on the work of Drasgow et al. (1996) who suggested focusing on contexts with idiosyncratic response forms as behavioral indicators. They noted that the idiosyncratic responses served as potential markers of motivating reinforcers and therefore should serve as the focus of initial communication intervention. The findings of the current investigation are consistent with previous work (Byiers et al. 2014; Drasgow et al. 1996; Keen et al. 2001) and demonstrated similar findings across several factors. Contexts with idiosyncratic communicative responses in the participant’s routine were assessed and selected for intervention. Additionally, functional communication training was used as intervention to replace the idiosyncratic responses with an AAC response. Finally, all of the participants acquired the AAC response.
Consistent with Moes and Frea (2002), the current findings contribute to the literature on parent-implemented NDBIs through ‘loosening’ and embedding FCT into natural, contextualized and family-centered routines. Collecting comprehensive descriptive functional assessment information (through the FAI and SDA) served as an important first step to construct FCT in a NDBI intervention framework to select and embed FCT into relevant contexts to the child and family.
There were novel findings from the current investigation. First, idiosyncratic and AAC responses were observed as dependent measures to investigate the functional relation between the two under reinforcement and extinction arrangements, and when a new response was introduced to the participant’s repertoire. Second, parents were successful at implementing both the assessment and intervention procedures. Third, telehealth was successfully used as the platform for coaching parents during the study.
Functional equivalence (Carr 1988) is an important underlying principle of FCT intervention (Drasgow et al. 1996). An important implication to consider is the functional equivalence required for functional communication training. FCT is most successful when the response effort is less for the competing response (the AAC response in the current investigation) than the target response (the idiosyncratic response in the current investigation). In the current study, the AAC response was acquired and the idiosyncratic responses decreased during differential reinforcement of the AAC request phases, demonstrating that the AAC response successfully competed with the idiosyncratic response. However, an important implication discussed by Drasgow and colleagues is that challenging behavior may be effortful (e.g., tantrums) whereas certain idiosyncratic responses (e.g., eye pointing) may be less effortful, and therefore more difficult to demonstrate functional equivalence with a competing behavior (e.g., handing a PECS card). In the current investigation, consideration was given to response effort during selection of the targeted AAC response for each participant, and each response selected was estimated to be of somewhat equal effort to the idiosyncratic response in the participant’s repertoire. For example, Ella’s leading and tantrums were replaced by first touching, and then giving her parent a picture card; she was not required to travel any distance to retrieve the card or to exchange with her parent. Neither Ella nor Sidney were required to discriminate icons; Lily was, but only after she independently demonstrated speaking the multiple words involved in the contexts (e.g., she spontaneously began to say “drink” and “food,” although initially only “food” was targeted on the picture cards). Interventionists should take care to match AAC effort to that of the responses with which they wish to compete. Future research may investigate the effects of more complex AAC responses under the FCT to replace idiosyncratic responses paradigm.
Telehealth Coached Interventions
The current investigation extends the pioneering work on FA + FCT intervention via telehealth by Wacker et al. (2013a, b) to early communication interventions. Consistent with the literature telehealth as a mechanism to deliver NDBI interventions (Wainer and Ingersoll 2015), parents were able to implement successfully and rated the treatment as acceptable. The novel contributions of the current investigation include the use of a SDA to assess potential idiosyncratic responses and contexts to embed communication intervention. Most importantly, the current investigation demonstrated evidence of increasing of multiple communication responses across multiple contexts in the child’s day during parent-implemented intervention delivered with coaching via telehealth.
Potential implications for future research for telehealth as a service delivery mechanism in early communication interventions may be a reduction in cost and resources. Wacker et al. (2013b) found a significant cost reduction when delivering FA via telehealth versus a clinician traveling to the family’s home. For example, in their study the average cost per week for delivering the FA via telehealth compared to an interventionist driving to the home was $57.95 (telehealth) compared to $335.09 (clinician traveling to home). Future research should examine whether these findings extend to early communication intervention. In addition, although the intervention investigated in the current study would not likely take the place of a comprehensive intervention package for young children with neurodevelopmental disabilities, it may serve as a supplement to interventions and it might represent an important starting place while parents are in the process of finding service providers. Finally, future research should examine the conditions under which telehealth can be an effective service delivery mechanism to train and support service providers in rural areas and to provide intervention and support for children with low incidence disorders (such as RTT).
Limitations to the current investigation are related to limited control of outside service delivery for two of the participants, generalizability, the high level of participant involvement required, and the lack of maintenance data. First, Ella and Lily had influence from outside service providers, though we asked the parents to have providers not implement FCT or the AAC modality targeted in the study. Although it is possible that during other communication programming influenced the intervention, the single-subject experimental design across contexts data did not suggest the influence of other communication programming. Second, it is reasonable to expect that a child or adult with more severe motor impairments (e.g., further into or more affected by regression in RTT) may have experienced greater difficulty with the AAC responses. Third, there was a high level of involvement required of the parents in this study. All of the participating children lived in two-parent households. During interventions, one parent served as the interventionist as the other parent or another caregiver assisted with siblings. If the parent had to serve as an interventionist without assistance it would have likely made implementing the procedures more challenging. Fourth, the lasting effects of the intervention are unknown, as there were no maintenance data collected. When the AAC response was placed on extinction and reinforcement was provided for the idiosyncratic responses during the reversal phase of the study, the AAC responses persisted for a limited number of sessions for Lily and Ella (7 and 4 sessions, respectively) and did not persist for Sidney (0 sessions). Although this response pattern would be predicted by the differential reinforcement schedule, it might be suggestive of how important fidelity to the differential reinforcement schedule would be following intervention. It also highlights the need for investigation of intervention fading strategies to promote maintenance.
It should be noted that extinction was implemented in the differential reinforcement arrangement in order to (a) teach the AAC response and (b) examine the functional relation between the idiosyncratic response and the AAC response. It was not necessarily our intent to extinguish the idiosyncratic responses, but rather, to (a) provide the participants with a more formal, easily recognizable response that might be more likely to produce reinforcement with unfamiliar caregivers such as babysitters or teachers, (b) provide an alternative response to undesirable behavior (in this case, tantrums and crying/whining) that often produce reinforcement and occasionally occur in the absence of formal, recognizable forms of communication, and (c) to expand the participants’ social communication repertoire rather than narrow it to a single response that may not always be available (e.g., when the battery in the microswitch does not work or the PECs card gets left behind when the family goes on an outing). Future research should examine response persistence, resurgence, and reinstatement of various response forms that have produced the same functional reinforcer under various conditions.
Acknowledgments
This research was funded in part by a grant from NIH/NICHD, Grant No. 44763. We wish to thank Dr. Dave Wacker, John Lee, and colleagues at the University of Iowa for their guidance in the development of the UMN telehealth laboratory and procedures. We also wish to thank Marianne Elmquist, Brittany Pennington, and Stephanie Snidarich for their efforts with data collection. We wish to express our deepest gratitude to the children and their families for their participation in this research.
Footnotes
Conflict of interest This research was completed in partial fulfillment of the requirements for a PhD in Educational Psychology at the University of Minnesota for the first author. The second and third authors have received research funding through NIH/NICHD Grant No. 44763. The authors have no conflicts of interest to disclose.
Ethical Approval All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants (parents) included in the study, which was approved by the University of Minnesota Internal Review Board.
References
- American Academy of Pediatrics [AAP], (2007). Management of children with autism spectrum disorder. Pediatrics, 120, 1162–1182. doi: 10.1542/peds.2007-2362. [DOI] [PubMed] [Google Scholar]
- American Speech Language Hearing Association. (2005). SLP Health Care Survey. http://www.asha.org/Research/memberdata/Health-careSurvey/. Accessed 27 Dec 2016.
- American Speech-Language Hearing Association. (2011) Autism. Retrieved June 1, 2015 from http://www.asha.org/PRPSpecific-Topic.aspx?folderid=8589935303§ion=Treatment.
- Anderson C, & Long E (2002). Use of a structured descriptive assessment methodology to identify variables affecting problem behavior. Journal of Applied Behavioral Analysis, 35, 137–154. doi: 10.1901/jaba.2002.35-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmus JM, Ringdahl JE, Sellers JA, Call NA, Andelman MS, & Wacker DP (2004). Use of a short-term inpatient model to evaluate aberrant behavior: Outcome data summaries from 1996 to 2001. Journal of Applied Behavior Analysis, 37, 283–304. doi: 10.1901/jaba.2004.37-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey J, McComas JJ, Benavides C, & Lovascz C (2002). Functional assessment in a residential setting: Identifying effective communication replacement response for aggressive behavior. Journal of Developmental and Physical Disabilities, 14, 353–369. doi: 10.1023/A:1020382819146. [DOI] [Google Scholar]
- Behavior Analyst Certification Board [BCBA] Certificant registry. (2012). Retrieved June 1, 2015, from http://www.bacb.com/index.php?page=100155&by=state.
- Berkowitz S (1990). A comparison of two methods of prompting in training discrimination of communication book pictures by autistic students. Journal of Autism and Developmental Disorders, 20, 255–262. doi: 10.1007/BF02284722. [DOI] [PubMed] [Google Scholar]
- Betz CL, Baer MT, Poulsen M, Vahanvaty U, Bare M, Haddad Y, & Nwachuken G (2004). Secondary analysis of primary and preventative services accessed and perceived service barriers by children with developmental disabilities and their families. Issues in Comprehensive Pediatric Nursing, 27, 83–106. doi: 10.1080/01460860490451813. [DOI] [PubMed] [Google Scholar]
- Birnbrauer JS, Peterson CR, & Solnick JV (1974). Design and interpretation of studies of single subjects. American Journal of Mental Deficiency, 79(2), 191–203. [PubMed] [Google Scholar]
- Bondy AS, & Frost LA (1994). The picture exchange communication system. Focus on Autistic Behavior, 9, 1–19. doi: 10.1177/108835769400900301. [DOI] [Google Scholar]
- Brown F, Gothelf CR, Guess D, & Lehr D (1998). Self-determination for individuals with the most severe disabilities: Moving beyond chimera. Journal of the Association for Persons with Severe Handicaps, 23, 17–26. doi: 10.2511/rpsd.23.1.17. [DOI] [Google Scholar]
- Byiers BJ, Dimian A, & Symons FJ (2014). Functional communication training in Rett syndrome: A preliminary study. American Journal on Intellectual and Developmental Disabilities, 119(4), 340–350. doi: 10.1352/1944-7558-119.4.340. [DOI] [PubMed] [Google Scholar]
- Carr EG (1988). Functional equivalence as a mechanism of response generalization In Horner RH, Dunlap G, & Koegel RL (Eds.), Generalization and maintenance: Lifestyle changes in applied settings (pp. 221–241). Baltimore, MD, US: Paul H Brookes Publishing. [Google Scholar]
- Carr EG, & Durand VM (1985). Reducing behavior problems through functional communication training. Journal of Applied Behavior Analysis, 18, 111–126. doi: 10.1901/jaba.1985.18-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlop MH, Schreibman L, & Thibodeau MG (1985). Increasing spontaneous verbal responding in autistic children using a time delay procedure. Journal of Applied Behavior Analysis, 18, 155–166. doi: 10.1901/jaba.1985.18-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chasson GS, Harris GE, & Neely WJ (2007). Cost comparison of early intensive behavioral intervention and special education for children with autism. Journal of Child and Family Studies, 16(3), 401–413. doi: 10.1007/s10826-006-9094-1. [DOI] [Google Scholar]
- Christensen DL, Baio J, Braun KV, et al. (2016). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, united states, 2012. MMWR Surveillance Summaries, 65, 1–23. doi: 10.15585/mmwr.ss6503a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen H, Amerine-Dickens M, & Smith T (2006). Early intensive behavioral treatment: Replication of the ucla model in a community setting. Journal of Developmental & Behavioral Pediatrics, 27(2), 145–155. [DOI] [PubMed] [Google Scholar]
- Derby KM, Wacker DP, Berg W, DeRaad A, Ulrich S, Asmus J, & Stoner EA (1997). The long-term effects of functional communication training in home settings. Journal of Applied Behavior Analysis, 30, 507–531. doi: 10.1901/jaba.1997.30-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derby KM, Wacker DP, Sasso G, Steege M, Northup J, Cigrand K, & Asmus J (1992). Brief functional assessment techniques to evaluate aberrant behavior in an outpatient setting: A summary of 79 cases. Journal of Applied Behavior Analysis, 25(3), 713–721. doi: 10.1901/jaba.1992.25-713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingfelder HE, & Mandell DS (2011). Bridging the research to practice gap in autism intervention: An application of diffusion of innovation theory. Journal of Autism & Developmental Disorders, 41, 597–609. doi: 10.1007/s10803-010-1081-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drasgow E, Halle JW, Ostrosky MM, & Harbers HM (1996). Using behavioral indication and functional communication training to establish an initial sign repertoire with a young child with severe disabilities. Topics in Early Childhood Special Education, 16, 500–521. doi: 10.1177/027112149601600408. [DOI] [Google Scholar]
- Durand VM (1999). Functional communication training using assistive devices: Recruiting natural communities of reinforcement. Journal of Applied Behavior Analysis, 32, 247–267. doi: 10.1901/jaba.1999.32-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eikeseth S, Smith T, Jahr E, & Eldevik S (2002). Intensive behavioral treatment at school for 4-to 7-year-old children with autism a 1-year comparison controlled study. Behavior modification, 26, 49–68. doi: 10.1177/0145445502026001004. [DOI] [PubMed] [Google Scholar]
- Eldevik S, Eikeseth S, Jahr E, & Smith T (2006). Effects of low-intensity behavioral treatment for children with autism and mental retardation. Journal of Autism and Developmental Disorder, 36, 211–224. doi: 10.1007/s10803-005-0058-x. [DOI] [PubMed] [Google Scholar]
- English CL, & Anderson CM (2006). Evaluation of the treatment utility of the analog functional analysis and the structured descriptive assessment. Journal of Positive Behavior Interventions, 8, 212–229. doi: 10.1177/10983007060080040401. [DOI] [Google Scholar]
- Freeman KA, Anderson CM, & Scotti JR (2000). A structured descriptive methodology: Increasing agreement between descriptive and experimental analyses. Education and Training in Mental Retardation and Developmental Disabilities, 35, 55–66. [Google Scholar]
- Gast DL, & Ledford JR (Eds.). (2014). Single case research methodology: Applications in special education and behavioral sciences. New York: Taylor & Francis. [Google Scholar]
- Harding JW, Wacker DP, Berg WK, Lee JF, & Dolezal D (2009). Conducting functional communication training in home settings: A case study and recommendations for practitioners. Behavior Analysis in Practice, 2, 21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris SL, & Handleman JS (2000). Age and IQ at intake as predictors of placement for young children with autism: A four- to six-year follow-up. Journal of Autism & Developmental Disorders, 30, 137–142. doi: 10.1023/A:1005459606120. [DOI] [PubMed] [Google Scholar]
- Hewitt A, Gulaid A, Hamre K, Esler A, Punyko J, Reichle J, & Reiff M (2013). Minneapolis Somali autism spectrum disorder prevalence project: Community report 2013. Minneapolis, MN: University of Minnesota, Institute on Community Integration, Research and Training Center on Community Living. [Google Scholar]
- Horn E, Lieber J, Sandall S, Schwartz I, & Worley R (2002). Supporting young children’s IEP goals in inclusive settings through embedded learning opportunities. Topics in Early Childhood Special Education, 20, 208–223. doi: 10.1177/027112140002000402. [DOI] [Google Scholar]
- Horner RH, & Carr E (1997). Behavioral support for students with severe disabilities: Functional assessment and comprehensive intervention. Journal of Special Education, 31, 84–104. doi: 10.1177/002246699703100108. [DOI] [Google Scholar]
- Horner RH, & Day HM (1991). The effects of response efficiency on functionally equivalent competing behaviors. Journal of Applied Behavior Analysis, 24(4), 719–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin P, Goode S, Hutton J, & Rutter M (2004). Adult outcome for children with autism. Journal of Child Psychology and Psychiatry, 45, 212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Individuals with Disabilities Education Act of 2004. 20 U. S. C. § 1400 et seq. (2004).
- Ingersoll B, Wainer AL, Berger NI, Pickard KE, & Bonter N (2016). Comparison of a self-directed and therapist-assisted telehealth parent-mediated intervention for children with ASD: A pilot RCT. Journal of Autism and Developmental Disorders. doi: 10.1007/s10803-016-2755-z. [DOI] [PubMed] [Google Scholar]
- Iwata BA, Dorsey MF, Slifer KJ, Bauman KE, & Richman GS (1982/1994). Toward a functional analysis of self-injury. Journal of Applied Behavior Analysis, 27, 197–209. doi: 10.1901/jaba.1994.27-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston SS, Reichle J, & Evans J (2004). Supporting augmentative and alternative communication use by beginning communicators with severe disabilities. American Journal of Speech Language Pathology, 13(1), 20–30. doi: 10.1044/1058-0360(2004/004). [DOI] [PubMed] [Google Scholar]
- Kazdin AE (2008). Evidence-based treatments and delivery of psychological services: Shifting our emphases to increase impact. Psychological Services, 5, 201–215. doi: 10.1037/a0012573. [DOI] [Google Scholar]
- Keating D, Syrmis M, Hamilton L, & McMahon S (1998). Paediatricians: Referral rates and speech pathology waiting lists. Journal of Paediatrics & Child Health, 34, 451–455. doi: 10.1046/j.1440-1754.1998.00273.x. [DOI] [PubMed] [Google Scholar]
- Keen D, Sigafoos J, & Woodyatt G (2001). Replacing prelinguistic behaviors with functional communication. Journal of Autism and Developmental Disorders, 31, 298–385. doi: 10.1023/A:1010612618969. [DOI] [PubMed] [Google Scholar]
- Koegel RL, Koegel LK, & Surratt A (1992). Language intervention and disruptive behavior in preschool children with autism. Journal of autism and developmental disorders, 22, 141–153. doi: 10.1007/BF01058147. [DOI] [PubMed] [Google Scholar]
- Kurtz PF, Chin MD, Huete JM, Tarbox RSF, O’Connor JT, Paclawskyj TR, & Rush KS (2003). Functional analysis and treatment of self-injurious behavior in young children: A summary of 30 cases. Journal of Applied Behavior Analysis, 36, 205–219. doi: 10.1901/jaba.2003.36-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindgren S, Wacker D, Suess A, Schieltz K, & Pelzel K (2016). Telehealth and autism: Treating challenging behavior at lower cost. Pediatrics, 137, 168–175. doi: 10.1542/peds.2015-2851O. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovaas OI (1987). Behavioral treatment and normal educational and intellectual functioning in young autistic children. Journal of Consulting and Clinical Psychology, 55, 3–9. doi: 10.1037/0022-006X.55.1.3. [DOI] [PubMed] [Google Scholar]
- MacDuff GS, Krantz PJ, & McClannahan LE (2001). Prompts and prompt-fading strategies for people with autism In Maurice C, Green G & Foxx RM (Eds.), Making a difference: Behavioral intervention for autism (pp. 37–50). Austin, TX: Pro-Ed. [Google Scholar]
- Mace FC, & Roberts ML (1993). Factors affecting selection of behavioral interventions In Reichle J, & Wacker DP (Eds.) Communicative alternatives to challenging behavior: Integrating functional assessment and intervention strategies (pp. 113–133). Baltimore, MD: Paul H Brookes Publishing. [Google Scholar]
- McDuffie A, Machalicek W, Oakes A, Haebig E, Weismer SE, & Abbeduto L (2013). Distance video-teleconferencing in early intervention: Pilot study of a naturalistic parent-implemented language intervention. Topics in Early Childhood Special Education, 33, 172–185. doi: 10.1177/0271121413476348. [DOI] [Google Scholar]
- Moes DR, & Frea WD (2002). Contextualized behavioral support in early intervention for children with autism and their families. Journal of Autism and Developmental Disabilities, 32, 519–533. doi: 10.1023/A:1021298729297. [DOI] [PubMed] [Google Scholar]
- Montes G, Halterman JS, & Magyar CI (2009). Access to and satisfaction with school and community health services for us children with asd. Pediatrics, 124, S407–S413. doi: 10.1542/peds.2009-1255L. [DOI] [PubMed] [Google Scholar]
- National Research Council (2001). Educating Children with Autism. Committee on Educational Interventions for Children with Autism. Lord Catherine and McGee James P., eds. Division of Behavioral and Social Sciences and Education; Washington, DC: National Academy Press. [Google Scholar]
- O’Neill RE, Horner RH, Albin RW, Storey K, Sprague JR, & Newton JS (1997). Functional assessment of problem behavior: A practical assessment guide. Pacific Grove, CA: Brooks/Cole. [Google Scholar]
- Oliver C, Petty J, Ruddick L, & Bacarese-Hamilton M (2012). The association between repetitive, self-injurious and aggressive behavior in children with severe intellectual disabilities. Journal of Autism and Developmental Disorders, 42, 910–919. doi: 10.1007/s10803-011-1320-z. [DOI] [PubMed] [Google Scholar]
- Reichle J, & Wacker DP (in press). Functional communication training for problem behavior. New York: Guilford Press. [Google Scholar]
- Reimers TM, & Wacker DP (1988). Parents’ ratings of the acceptability of behavioral treatment recommendations made in an outpatient clinic: A preliminary analysis of the influence of treatment effectiveness. Behavioral Disorders, 14, 7–15. http://www.jstor.org/stable/23886135. [Google Scholar]
- Reimers TM, Wacker DP, & Cooper LJ (1991). Evaluation of the acceptability of treatments for children’s behavioral difficulties: Ratings by parents receiving services in an outpatient clinic. Child & Family Behavior Therapy, 13, 53–71. [Google Scholar]
- Remington B, Hastings RP, Kovshoff H, degli Espinosa F, Jahr E, Brown T, et al. (2007). Early intensive behavioral intervention: Outcomes for children with autism and their parents after two years. American Journal on Mental Retardation, 112, 418–438. doi: 10.1352/0895-8017(2007)112[418:EIBIOF]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Rogers S & Wallace K (2011). Intervention for infants and toddlers with autism spectrum disorders In Amaral D, Dawson G & Geschwind D (Eds.), Autism spectrum disorders (pp. 1081–1094). Oxford, UK: Oxford University Press. [Google Scholar]
- Rogers SJ (1998). Empirically supported comprehensive treatments for young children with autism. Journal of Clinical Child Psychology, 27, 168–179. doi: 10.1207/s15374424jccp2702_4. [DOI] [PubMed] [Google Scholar]
- Sallows GO, & Graupner TD (2005). Intensive behavioral treatment for children with autism: Four-year outcome and predictors. American Journal on Mental Retardation, 110, 417–438. doi: 10.1352/0895-8017(2005)110[417:IBTFCW]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Satcher DS (2000). Executive summary: A report of the Surgeon General on mental health. Public Health Reports, 115, 89–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schieltz KM, Wacker DP, Harding JW, Berg WK, Lee JF, Dalmau YCP, … & Ibrahimović M (2011). Indirect effects of functional communication training on non-targeted disruptive behavior. Journal of Behavioral Education, 20, 15–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreibman L, Dawson G, Stahmer AC, Landa R, Rogers SJ, McGee GG, … & McNerney E (2015). Naturalistic developmental behavioral interventions: Empirically validated treatments for autism spectrum disorder. Journal of Autism and Developmental Disorders, 45, 2411–2428. doi: 10.1007/s10803-015-2407-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suess AN, Romani PW, Wacker DP, Dyson SM, Kuhle JL, Lee JF, Lindgren SD, Kopelman TG, Pelzel KE, & Waldron DB (2014). Evaluating the treatment fidelity of parents who conduct in-home functional communication training with coaching via telehealth. Journal of Behavioral Education, 23, 34–59. doi: 10.1007/s10864-013-9183-3. [DOI] [Google Scholar]
- Sheinkopf SJ, & Siegel B (1998). Home based behavioral treatment of young children with autism. Journal of Autism & Developmental Disorders, 28(1), 15–23. doi: 10.1023/A:1026054701472. [DOI] [PubMed] [Google Scholar]
- Sparrow SS, Cicchetti DV, & Balla DA (2005). Vineland adaptive behavior scales (2nd ed.). Bloomington, MN: Pearson Assessments. [Google Scholar]
- Sperry L, Whaley K, Shaw E, & Brame K (1999). Services for young children with autism spectrum disorder: Voices of parents and providers. Infants and Young Children, 11(4), 17–33. [Google Scholar]
- Stahmer AC & Gist K (2001). The effects of an accelerated parent education program on technique mastery and child outcome. Journal of Positive Behavior Interventions, 3(2), 75–82. doi: 10.1177/109830070100300203. [DOI] [Google Scholar]
- Sundberg ML, & Partington JW (1999). The need for both discrete trial and natural environment language training for children with autism In Ghezzi PM, Williams WL, & Carr JE (Eds.), Autism: Behavior analytic perspectives (pp. 139–156). Reno, NV: Context Press. [Google Scholar]
- Symon J (2005). Expanding interventions for children with autism: Parents as trainers. Journal of Positive Behavior Interventions, 7, 159–173. doi: 10.1177/10983007050070030501. [DOI] [Google Scholar]
- Tait K, Sigafoos J, Woodyatt G, O’Reilly M, & Lancioni G (2004). Evaluating parent use of functional communication training to replace and enhance prelinguistic behaviours in six children with developmental and physical disabilities. Disability and Rehabilitation, 26, 1241–1254. [DOI] [PubMed] [Google Scholar]
- Thomas KC, Ellis AR, McLaurin C, Daniels J, & Morrissey JP (2007). Access to care for autism related services. Journal of Autism and Developmental Disorders, 37, 1902–1912. doi: 10.1007/s10803-006-0323-7. [DOI] [PubMed] [Google Scholar]
- Tiger JH, Hanley GP, & Bruzek J (2008). Functional communication training: A review and practical guide. Behavior Analysis in Practice, 1, 16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vismara LA, McCormick C, Young GS, Nadhan A, & Monlux K (2013). Preliminary findings of a telehealth approach to parent training in Autism. Journal of Autism and Developmental Disorders, 43(12), 2953–2969. doi: 10.1007/s10803-013-1841-8. [DOI] [PubMed] [Google Scholar]
- Vismara LA, Young GS, & Rogers SJ (2012). Telehealth for expanding the reach of early autism training to parents. Autism Research and Treatment, 2012. doi: 10.1155/2012/121878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker DP, Berg WK, Harding JW, Barretto A, Rankin B, & Ganzer J (2005). Treatment effectiveness, stimulus generalization, and acceptability to parents of functional communication training. Educational Psychology, 25(2–3), 233–256. doi: 10.1080/0144341042000301184. [DOI] [Google Scholar]
- Wacker DP, Berg WK, Harding JW, Derby KM, Asmus JM, & Healy A (1998). Evaluation and long-term treatment of aberrant behavior displayed by young children with disabilities. Journal of Developmental and Behavioral Pediatrics, 19, 260–266. doi: 10.1097/00004703-199808000-00004. [DOI] [PubMed] [Google Scholar]
- Wacker DP, Harding JW, Berg WK, Lee JF, Schieltz KM, Padilla YC, Nevin JA, & Shahan TA (2011). An evaluation of persistence of treatment effects during long-term treatment of destructive behavior. Journal of the Experimental Analysis of Behavior, 96, 261–282. doi: 10.1901/jeab.2011.96-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker DP, Lee JF, Padilla Dalmau YC, Kopelman TG, Lindgren SD, Kuhle J, … & Waldron DB (2013a). Conducting functional communication training via telehealth to reduce the problem behavior of young children with autism. Journal of Developmental and Physical Disabilities, 25, 35–48. doi: 10.1007/s10882-012-9314-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker DP, Lee JF, Padilla Dalmau YC, Kopelman TG, Lindgren SD, Kuhle J, … & Waldron DB (2013b). Conducting functional analyses of problem behavior via telehealth. Journal of Applied Behavior Analysis, 46, 1–16. doi: 10.1002/jaba.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wainer AL, & Ingersoll BR (2015). Increasing access to an ASD imitation intervention via a telehealth parent training program. Journal of Autism and Developmental Disorders, 45, 3877–3890. [DOI] [PubMed] [Google Scholar]
- Wise MD, Little A, Holliman JB, Wise PD, & Wang CJ (2010). Can state early intervention programs meet the increased demand of children suspected of having autism spectrum disorders? Journal of Developmental and Behavioral Pediatrics, 31(6), 469–476. doi: 10.1097/DBP.0b013e3181e56db2. [DOI] [PubMed] [Google Scholar]
- Woods J, Kashinath S, & Goldstein H (2004). Effects of embedding caregiver-implemented teaching strategies in daily routines on children’s communication outcomes. Journal of Early Intervention, 26, 175–193. doi: 10.1177/105381510402600302. [DOI] [Google Scholar]