Abstract
The products used in nail care services contain toxic chemicals. This study aimed to characterize occupational health risk factors and chemical exposures among Asian nail salon workers on the East Coast of the U.S. for informing the development of more effective, culturally appropriate interventions. We conducted a community-based participatory research (CBPR) study to characterize occupational health risks. A face-to-face, self-reported survey was performed, and personal exposure to volatile organic compounds (VOCs) was evaluated. Three VOCs, acetone, methyl methacrylate (MMA), and toluene, were measured using 3M 3500 organic vapor monitors. We collected data on 112 workers with 100 personal chemical exposure measurements from 25 nail salons. Self-reported health problems that emerged or worsened after participants started working in the nail salon industry included headaches (8%); lightheadedness (9.8%); and irritation to the nose, eyes, throat, and skin (21.2%). Approximately 70% of participants reported that they had been pregnant, 11.7% of whom had at least one miscarriage. The mean concentrations of acetone, MMA, and toluene were 18.51 parts per million (ppm), 39.45 ppm, and 0.09 ppm, respectively. Mean concentrations of acetone and MMA measured from salons in New York City were significantly lower than those measured in Philadelphia and southern New Jersey. CBPR proved to be as an efficient approach for recruiting hard-to-reach Asian immigrant nail salon workers. Adverse health symptoms and problems associated with providing nail salon services were identified in these workers. Further studies are needed to better understand the long-term health effects of chronic chemical exposures in nail salon environments.
Keywords: Nail salon, Chemical exposure, Health risks, Health disparities
Introduction
Nail salons provide nail care mainly in the form of manicures and pedicures. Services include the use of nail polishes, polish removers, and artificial nail applications. While the nail salon industry has grown only modestly in recent years, with a reported revenue of $8.28 billion in 2013 and $8.53 billion in 2017, the U.S. Bureau of Labor and Statistics anticipates a faster-than-average rate of growth for the industry from 2016 to 2026. In 2017, there were more than 56,000 nail salons and 440,000 nail technicians in the US. Growth in the numbers of salons and workers in the coming years are expected to result in greater job opportunities [1, 2].
Immigrants have been particularly drawn to the nail salon industry due to the low barriers of entry, including a lack of educational and skill-related prerequisites, short-term training, flexible work schedule, limited financial pressure, and low need for English proficiency [3]. In addition, ethnic business networks promote the nail salon business among immigrants as a means of earning an income. Vietnamese immigrants traditionally hold the largest stake in the nail salon industry and dominate the salon business workforce, however, in recent years, increasing numbers of Chinese, Korean, and Hispanic immigrants have joined the industry as well [4, 5].
The products used to carry out nail care services contain many toxic and potentially hazardous chemical compounds, including acetone, toluene, formaldehyde, and acrylates. These chemical compounds, many of which are volatile organic compounds (VOCs), are largely unregulated in the United States. In fact, the vast majority of the 10,000 chemicals used in personal care products have never been assessed for safety [6]. Despite the increasing use of some green i.e., 3-free, eco-friendly products, which do not contain formaldehyde, toluene, and dibutyl phthalate (DBP), exposure to other chemicals in nail products has been associated with the development of adverse effects, including irritation to the eyes and nose, headaches, asthma, dizziness, disorders of the reproductive system, and even cancer [7–9]. Exposure over a long period of time increases the risk of these adverse effects. Frequent exposure to VOCs in high concentrations also poses health risks to nail salon customers [10–15].
Several recent survey studies have focused on occupational health risks in Vietnamese nail salon workers [10, 16–18]. One intervention study was conducted in California [19]. Given the fact that large numbers of Chinese and Korean immigrants are joining the nail salon industry on the East Coast of the United States, the purpose of this study was to characterize Asian nail salon workers’ occupational health risk status specifically in New York City (NYC), Philadelphia, and southern New Jersey. Our study was carried out by conducting a health risk survey and measuring personal VOC exposure in nail salon workers in these areas. Data collected from this study can be used as a reference to inform larger educational intervention studies in Asian and other ethnic groups aimed at reducing and eventually eradicating chemical exposure-induced health disparities among nail salon workers.
Methods
Study Population
This study, conducted between January 2017 and August 2017, was a community-based participatory research investigation in the eastern United States. The study protocol was reviewed and approved by the Temple University Institutional Review Board (IRB protocol titled: A pilot culturally appropriate intervention to reduce chemical exposures in Asian American nail salon workers). Nail salon owners and workers from three major Asian ethnic communities that dominate the nail salon business in the United States, Chinese, Korean, and Vietnamese, were recruited from NYC, Philadelphia, and southern New Jersey. Eligibility criteria included (1) being self-identified as part of the Asian ethnicity (Chinese, Korean, or Vietnamese immigrants); (2) being men and women age 18 years and above; (3) having worked in a nail salon continuously for at least 12 months; (4) being accessible by cell telephone; (5) being present in the same geographic study area for a period of one year (to minimize participant attrition); and (6) not being enrolled in any other interventions (to prevent a potential program impact). Informed consent forms were obtained from all participants.
Recruitment Strategy
We started our recruitment strategy by using community-based networks, as well as personal connections and relationships [17, 19]. Over the past decade, we have built a strong partnership network with numerous Asian community-based organization partners on the East Coast. Using this community-based recruitment strategy, we successfully built connection to establish collaborative partnerships with the nail salon owners. We thus explained to the owners, as well as the participating workers, the purpose of our study, our data collection procedures, and how chemical exposures would be measured. We recruited a total of 25 nail salons with 102 workers, including 11 Chinese-owned nail salons with 53 workers, 10 Vietnamese-owned nail salons with 35 workers, and 4 Korean-owned nail salons with 24 workers. Chinese nail salon owners and workers were recruited from NYC and Philadelphia, Korean nail salon owners and workers were recruited from Philadelphia, and Vietnamese nail salon owners and workers were recruited from Philadelphia and southern New Jersey.
Observation of Nail Salon Working Environment
In order to better describe the nail salon working environment in terms of chemical exposures, we collected information about the number of doors and windows, manicure stations, pedicure stations, and workers present at each salon. We further documented whether ventilation systems were turned on and whether personal protective gear was used at work. The amount of 3-free or 4-free (“n-free”) “green” products used in the nail salons was also recorded.
Assessment
Survey questions were designed to collect information about nail salon workers’ demographics, nail salon work history, nail salon work-related risk factors, self-reported general health problems, self-reported nail salon-related health problems, and the use of protective gear. We incorporated standardized and nail salon-specific health questions based on similar, previously validated surveys, from existing literature on nail salon studies, and related online nail salon reports [3, 15–22].
To validate survey questions, we conducted a pilot test of 7 nail salon workers from 3 salons in Philadelphia. Pilot testing showed good face validity of the instruments in the survey questionnaire. Based on initial feedback, the questionnaire was revised for clarity by deleting redundant questions, helping reduce the amount of time needed to complete the survey.
The survey questions and informed consent form were translated respectively to Chinese, Korean, and Vietnamese, and then translated back into English by bilingual professionals.
Personal VOC Chemical Exposure Monitoring
We measured VOC exposures in nail salon workers using 3M 3500 organic vapor monitors (3M, St. Paul, Minnesota). Each participating worker wore the device by clipping it onto his or her coat collar to absorb air samples close to his or her breathing zone and eyes. Workers wore the devices during the entire regular work shift, with a minimum sampling time of 4 h [3]. We then collected, timed, and sealed the monitors at the end of each sampling measurement. The number of manicure and pedicure services provided by each worker during the sampling period was recorded accordingly. The sealed monitors along with a non-exposed control monitor were stored at 4 °C within 2 weeks of the time the samples were collected before being sent out for laboratory (Pace Analytical Services, Minneapolis, Minnesota) analysis of time-weighted average (TWA) concentrations. We monitored VOC concentrations of acetone, methyl methacrylate (MMA), and toluene.
Data Analysis
Statistical analyses were performed using SPSS version 23.0 (SPSS, Chicago, IL). Descriptive statistics, specifically, absolute frequency and relative frequency (percentage) for categorical variables, and mean and range for continuous variables, are presented. For VOC monitoring measurements that were below the limit of detection (LOD), we used LOD. To compare the concentration of chemical compounds measured from nail salons across three ethnic communities and across three different geographic regions, we conducted t tests and presented the p-values to indicate whether the differences were statistically significant at the 0.05 level.
Results
Sociodemographic Characteristics of Nail Salon Workers
The sociodemographic characteristics of participating nail salon workers are shown in Table 1. We collected survey data from a total of 112 workers at 25 different nail salons. Of the 112 participating workers, 13 (100%) were salon owners, all born in the United States. Only five of the 99 remaining workers (5.1%) were also born in the United States. These data demonstrate that the majority of nail salon workers (94.9%) in the study were immigrants with a mean of 15.26 (range 1–47) years of U.S. residency. There were two males (15.4%) in the owner group and 15 males (15.2%) in the worker group. The mean owner age was 48.31 years, with a range of 39–63 years, while the mean worker age was 42.64 years, with a range of 17–65 years. In general, owners had stayed longer in the United States and had worked longer in the nail salon industry than the workers. More than one-third of workers (38.38%) had degrees above the level of a high school diploma. However, the majority of workers claimed only limited of English proficiency (67.68%). Among owners, 69.23% had an education level above a high school diploma and 53.85% claimed good English proficiency. A majority of owners (84.62%) and workers (94.85%) had at least one form of insurance coverage.
Table 1.
Sociodemographic characteristics of salon owners (n = 13) and salon employees (n = 99)
| Sociodemographic characteristics | Salon owners Mean (range) or n (%) | Salon employees Mean (range) or n (%) |
|---|---|---|
| Age | 48.31 (39.0–63.0) | 42.64 (17–65.0) |
| Gender | ||
| Male | 2 (15.4) | 15 (15.2) |
| Female | 11 (84.6) | 84 (84.8) |
| Marital status | ||
| Never married | 5 (38.46) | 45 (45.45) |
| Married/cohabitating | 6 (46.15) | 45 (45.45) |
| Divorced/separated/widowed | 2 (15.38) | 9 (9.09) |
| Birthplace | ||
| U.S. | 0 | 5 (5.1) |
| Outside the U.S. | 13 (100.0) | 94 (94.9) |
| Years lived in the U.S. | 15.26 (1–47) | |
| English proficiency | ||
| Poor/fair | 6 (46.15) | 67 (67.68) |
| Good/excellent | 7 (53.85) | 32 (32.32) |
| Highest education level | ||
| High school or lower | 4 (30.77) | 61 (61.62) |
| College or higher | 9 (69.23) | 38 (38.38) |
| Insurance coverage | ||
| None | 2 (15.38) | 5 (5.15) |
| Medicare/Medicaid | 2 (15.38) | 35 (36.08) |
| Affordable Care Act | 6 (46.15) | 38 (39.18) |
| Private insurance | 3 (23.08) | 19 (19.59) |
| Years in the nail salon industry | 9.62 (1–25) | 8.29 (0.50–30.00) |
| Age began working in the nail salon industry | 36.69 (26–54) | 33.03 (17.00–58.00) |
| Average work hours per week | 37.77 (9–84) | 34.42 (8–60) |
Nail Salon Work Environment
Among the 25 nail salons enrolled in this study, 11 were from Chinese communities, with 9 in NYC and 2 in Philadelphia; 10 were from Vietnamese communities, with 6 in Philadelphia and 4 in southern New Jersey; and 4 were from Korean communities, all located in Philadelphia. In total, we surveyed 9 salons in NYC, 12 salons in Philadelphia, and 4 salons in southern New Jersey.
The characteristics of these participating nail salons are summarized in Table 2. We observed that about one-fifth of salons had fewer than 5 stations for manicure and pedicure services, respectively. Only one salon did not have a ventilation system. There were 19 salons with front and back doors and 6 with only front doors. In addition, there were 19 salons with at least one window for ventilation and 6 with no windows for ventilation. In addition, 18 salons used some green products, while 7 salons did not use any green products. All salons except one had their own enclosed business spaces. One salon shared a large room with a hair care service. Several salons also had facial massage rooms, separate from manicure and pedicure services.
Table 2.
Characteristics of participating salons (n = 25) and work information of nail salon workers (n = 112)
| Salon characteristics | Mean (range) or n (%) |
|---|---|
| Manicure stations | |
| < 5 stations | 6 (24.0) |
| ≥ 5 stations | 19 (76.0) |
| Pedicure stations | |
| < 5 stations | 5 (20.0) |
| ≥ 5 stations | 20 (80.0) |
| Ventilation | |
| No | 1 (4.0) |
| Yes | 24 (96.0) |
| Doors | |
| 1 door | 6 (24.0) |
| ≥ 2 doors | 19 (76.0) |
| Windows | |
| 0 windows | 6 (24.0) |
| ≥ 1 window | 19 (76.0) |
| Green Products | |
| No | 7 (28.0) |
| Yes | 18 (72.0) |
| Worker characteristics | |
| Working hours per day | 8.0 (2–12) |
| Services performed per day | 6.9 (2–20) |
| Personal ventilation device at work desk | |
| Yes | 61 (55.5) |
| No | 38 (34.5) |
| Don’t Know | 11 (10.0) |
| Notice of any unpleasant odor in the salon | |
| Yes | 17 (15.2) |
| No | 42 (37.5) |
| Sometimes | 53 (47.3) |
| Use of only green, 3-free polishes | |
| Yes, always | 41 (37.6) |
| Yes, sometimes | 24 (22.0) |
| Not at all | 5 (4.6) |
| Not sure | 39 (35.8) |
| Protective gear worn while working | |
| Latex gloves | 91 (81.3) |
| Nylon gloves | 3 (2.7) |
| Infection control face masks | 28 (25.0) |
| Chemical safety face masks | 41 (36.6) |
| Other | 2 (1.8) |
| None of the above | 5 (4.5) |
| Meals typically eaten at work | |
| Breakfast | 10 (8.9) |
| Lunch | 109 (97.3) |
| Dinner | 4 (3.6) |
| Snack | 24 (21.4) |
| Storage for food and drinking water during work | |
| At work bench | 1 (0.9) |
| In designated lockers/cubbies | 17 (15.5) |
| In a separate lunch room/lounge area | 89 (80.9) |
| Other (fridge) | 3 (2.7) |
| Place typically where meals are eaten during work | |
| Don’t eat during work hours | 4 (3.6) |
| Eat at a designated kitchen or lunch room | 108 (96.4) |
| Wash hands with soap and water before eating, drinking, or smoking a cigarette | |
| Yes, always | 106 (94.6) |
| Yes, sometimes | 2 (1.8) |
| No | 3 (2.7) |
| Other | 1 (0.9) |
To further understand conditions associated with health risks in nail salon workers, we conducted a self-report survey among participating workers. As shown in Table 2, the average number of hours worked per day was 8, with a range of 2–12 h. In corresponding to amount of time worked, the average number of services performed by each worker was 6.9 per day. More than 55.5% of workers claimed to have a personal ventilation device at their work desk. Only 37.5% reported having no notice of any unpleasant odor in the salon. Almost 60% of workers reported using “3-free” green products either always or sometimes when performing services. With the exception of 4.5% of surveyed workers, all reported using personal protective equipment (PPE), such as gloves and masks. A majority of workers (94.6%) washed their hands before eating their lunch at a designated kitchen area in the salon (96.4%).
Health Problems and Risks Among Nail Salon Workers
When asked about cancer risk factors, more than 10% of workers had a family history of cancer, with lung cancer (4.5%), breast cancer (3.6%), and other cancer types (7.2%) reported. Approximately 90% of workers never drank alcohol or smoked. When asked about frequency of routine daily exercise lasting 30 min or more, workers responded with an average of 1.89 times per week. Approximately half of workers responded that they had not had any cancer screening within the past 5 years (Table 3).
Table 3.
Cancer risk factors and general health information associated with nail salon workers (n = 112)
| Risk factors | Mean (range) or n (%) |
|---|---|
| Which cancer screenings have you had within the past 5 years? | |
| Mammogram and/or MRI for breast cancer | 50 (45.5) |
| Colonoscopy or fecal test for colorectal cancer | 19 (17.1) |
| Pap test for cervical cancer | 33 (29.7) |
| Low-dose CT scan for lung cancer | 10 (9.0) |
| None of the above | 52 (46.8) |
| I don’t know | 6 (5.4) |
| Do you have any family history of cancer? | |
| No | 94 (87.9) |
| Lung cancer | 5 (4.5) |
| Breast cancer | 4 (3.6) |
| Nasopharyngeal cancer | 1 (0.90) |
| Other (skin, uterine, pancreatic, or cervical cancer) | 8 (7.2) |
| Have you ever drunk alcohol at least once per week for 6 months or longer? | |
| Yes | 10 (9.1) |
| If yes, how many years have you been drinking alcohol at least once per week? | 8.00 (1–20) |
| No | 100 (90.9) |
| What is your smoking status? | |
| Current smoker | 4 (3.8) |
| Previous smoker | 7 (6.7) |
| Never smoked | 94 (89.5) |
| Days per week doing moderate to vigorous intensity activity for at least 30 min as part of daily routine | 1.89 (0–7) |
| Have you ever been pregnant? | |
| Yes | 77 (81.0) |
| If yes, how many times? | 2.1 (1–4) |
| No | 33 (30.0) |
| Have you ever had a miscarriage? | |
| Yes | 12 (15.6) |
| No | 91 (88.3) |
| How often do you suffer from headaches? | |
| Very often (> 1 per day) | 2 (1.8) |
| Often (> 1 per week) | 3 (2.7) |
| Rarely (> 1 per month) | 33 (29.7) |
| Very rarely (< 1 per month) | 34 (30.6) |
| Never | 39 (35.1) |
| Have you been experiencing more headaches since you began working in the nail salon industry? | |
| Yes | 9 (8.0) |
| No | 73 (65.2) |
| Not sure | 30 (26.8) |
| Do you currently suffer from regular irritation of the following? | |
| Nose | 24 (21.4) |
| Throat | 13 (11.6) |
| Eyes | 19 (17.0) |
| Skin | 13 (11.6) |
| Other (hand or waist) | 4 (3.6) |
| None of the above | 54 (48.2) |
| Did your irritations begin when you started working in the nail salon industry? | |
| Yes | 18 (21.2) |
| No | 41 (48.2) |
| Do not know | 26 (30.6) |
| Did your irritations worsen when you started working in the nail salon industry? | |
| Yes | 17 (15.5) |
| No | 65 (59.1) |
| Do not know | 28 (25.5) |
| Have you ever been experiencing lightheadedness or confusion since you started working in the nail salon industry? | |
| Yes | 11 (9.8) |
| No | 87 (78.4) |
| Do not know | 13 (11.6) |
Table 3 also shows information on workers’ general health in association with performing nail salon services. The most common health complaints included irritation of the nose (21.4%), throat (11.6%), eyes (17%), and skin (11.6%). Some began experiencing headaches (8%) and lightheadedness (9.8%) when they started working in the nail salon industry. Furthermore, 15.5% of workers responded that their irritations began to worsen after they started working in the industry. Other symptoms workers experienced at least one day a week included chronic cough, breathing problems, nausea, shoulder pain, tendonitis, carpal tunnel, and arthritis.
Eighty-one percent (81%) of the workers reported that they had been pregnant, and 15.6% of them experienced at least one miscarriage (Table 3).
VOC Chemical Exposures in Nail Salon Workers
In Table 4, we summarized the means of chemical exposure results of VOCs at the nail salon level, with measurements of acetone, MMA, and toluene from at least three workers per salon. Only 12 Korean nail salon workers participated in personal chemical exposure monitoring, with three workers from each of the four participating Korean salons. Thus, the total measured workers was 100 out of the 112 workers surveyed. For acetone, the highest level was 58.47 parts per million (ppm), measured in salon 14, and the lowest level was 3.3 ppm, measured in salon 22. For MMA, the highest level was 941.25 ppm, measured in salon 21, and the lowest level was 0.049 ppm, measured in salon 15. With the exception of salon 1, with 18.95 ppm, and salon 19, with 21.52 ppm, most of the remaining salons had very low levels of MMA (less than 0.1 ppm). For toluene, the highest level was 0.24 ppm, measured in salon 2, and the lowest level was 0.06 ppm, measured in salon 16. All measurements for toluene were almost undetectable, indicating that this chemical compound was either very low or under strictly controlled use in nail salon products (in California, for example, the Environmental Protection Agency recommends ambient air levels of 0.08 ppm for toluene).
Table 4.
Arithmetic mean and standard deviation (SD) of personal chemical exposure for workers at the salon-level for toluene, methyl methacrylate (MMA), and acetone in parts per million (ppm)
| VOCs | Mean | SD | |
|---|---|---|---|
| Salon 1 (n = 3) | Acetone | 9.03 | 1.10 |
| MMA | 18.95 | 14.48 | |
| Toluene | 0.08 | 0.0038 | |
| Salon 2 (n = 3) | Acetone | 23.58 | 15.07 |
| MMA | 2.87 | 2.33 | |
| Toluene | 0.24 | 0.01 | |
| Salon 3 (n = 4) | Acetone | 19.1 | 5.23 |
| MMA | 0.08 | 0 | |
| Toluene | 0.08 | 0 | |
| Salon 4 (n = 3) | Acetone | 9.78 | 1.44 |
| MMA | 0.08 | 0 | |
| Toluene | 0.12 | 0.00 | |
| Salon 5 (n = 4) | Acetone | 10.24 | 0.39 |
| MMA | 0.098 | 0 | |
| Toluene | 0.14 | 0.0055 | |
| Salon 6 (n = 4) | Acetone | 35.36 | 34.01 |
| MMA | 5.08 | 4.15 | |
| Toluene | 0.08 | 0 | |
| Salon 7 (n = 7) | Acetone | 8.31 | 6.78 |
| MMA | 0.09 | 0.0061 | |
| Toluene | 0.10 | 0.0058 | |
| Salon 8 (n = 3) | Acetone | 28.43 | 4.21 |
| MMA | 0.06 | 0.00062 | |
| Toluene | 0.07 | 0.00067 | |
| Salon 9 (n = 6) | Acetone | 16.92 | 8.67 |
| MMA | 0.06 | 0.0023 | |
| Toluene | 0.07 | 0.0029 | |
| Salon 10 (n = 6) | Acetone | 10.10 | 3.26 |
| MMA | 0.08 | 0.0078 | |
| Toluene | 0.09 | 0.0107 | |
| Salon 11 (n = 6) | Acetone | 4.40 | 1.90 |
| MMA | 0.09 | 0.0055 | |
| Toluene | 0.09 | 0.0058 | |
| Salon 12 (n = 4) | Acetone | 35.43 | 4.40 |
| MMA | 0.18 | 0.15 | |
| Toluene | 0.10 | 0.0046 | |
| Salon 13 (n = 3) | Acetone | 14.73 | 1.80 |
| MMA | 0.05 | 0 | |
| Toluene | 0.10 | 0.01 | |
| Salon 14 (n = 3) | Acetone | 58.47 | 8.80 |
| MMA | 0.07 | 0 | |
| Toluene | 0.08 | 0.01 | |
| Salon 15 (n = 3) | Acetone | 40.3 | 2.92 |
| MMA | 0.049 | 0 | |
| Toluene | 0.06 | 0.02 | |
| Salon 16 (n = 3) | Acetone | 7.30 | 2.41 |
| MMA | 0.06 | 0 | |
| Toluene | 0.06 | 0 | |
| Salon 17 (n = 4) | Acetone | 24.85 | 7.37 |
| MMA | 1.82 | 0.24 | |
| Toluene | 0.10 | 0 | |
| Salon 18 (n = 4) | Acetone | 6.35 | 6.15 |
| MMA | 0.08 | 0.01 | |
| Toluene | 0.14 | 0.07 | |
| Salon 19 (n = 3) | Acetone | 47.1 | 34.09 |
| MMA | 21.52 | 12.76 | |
| Toluene | 0.09 | 0 | |
| Salon 20 (n = 3) | Acetone | 18 | 2.98 |
| MMA | 1.37 | 0.04 | |
| Toluene | 0.08 | 0 | |
| Salon 21 (n = 4) | Acetone | 14.59 | 15.26 |
| MMA | 941.25 | 589.37 | |
| Toluene | 0.11 | 0.06 | |
| Salon 22 (n = 3) | Acetone | 3.30 | 1.60 |
| MMA | 0.08 | 0.01 | |
| Toluene | 0.13 | 0.07 | |
| Salon 23 (n = 5) | Acetone | 12.02 | 4.98 |
| MMA | 0.09 | 0 | |
| Toluene | 0.09 | 0 | |
| Salon 24 (n = 5) | Acetone | 14.49 | 5.20 |
| MMA | 2.41 | 0.46 | |
| Toluene | 0.08 | 0.001 | |
| Salon 25 (n = 4) | Acetone | 27.03 | 27.03 |
| MMA | 0.08 | 0.01 | |
| Toluene | 0.10 | 0.03 | |
| Total (n = 100) | Acetone | 18.51 | 16.09 |
| MMA | 39.45 | 211.62 | |
| Toluene | 0.09 | 0.03 |
Salon 21 was determined to be an outlier for MMA
VOC Chemical Exposure Differences Among Nail Salon Workers
To better understand whether VOC exposure differs among nail salon workers in different ethnic populations and geographic regions, we compared the means of chemical exposure results for Chinese, Vietnamese, and Korean workers and for salons in Philadelphia, southern New Jersey, and NYC. We removed the MMA outlier from salon 21 for all comparisons, as indicated at the bottom of each table.
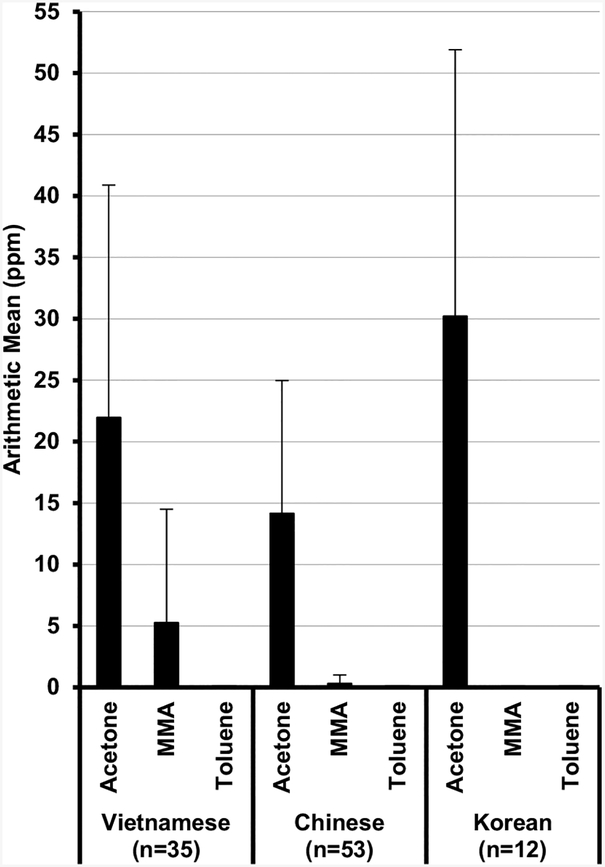
Figure 1 shows comparison results at the ethnicity level. For acetone, there was a significant difference between Vietnamese and Chinese workers (21.95 ppm vs. 14.15 ppm, p < 0.05), as well as between Chinese and Korean workers (14.15 ppm vs. 30.20 ppm, p < 0.01), with Korean workers having the highest exposures and Chinese workers the lowest exposures. For MMA, there was a significant difference between Vietnamese and Chinese workers (5.25 ppm vs. 0.31 ppm, p < 0.01). For toluene, there was a significant difference between Vietnamese and Korean workers (0.10 ppm vs. 0.08 ppm, p < 0.01).
Fig. 1.
Comparison of chemical exposures for workers from different ethnic populations. For acetone, levels between Vietnamese and Chinese (p ≤ 0.05) and Chinese and Korean (p < 0.01) both showed significant difference; for MMA, the level between Vietnamese and Chinese (p < 0.01) showed significant difference
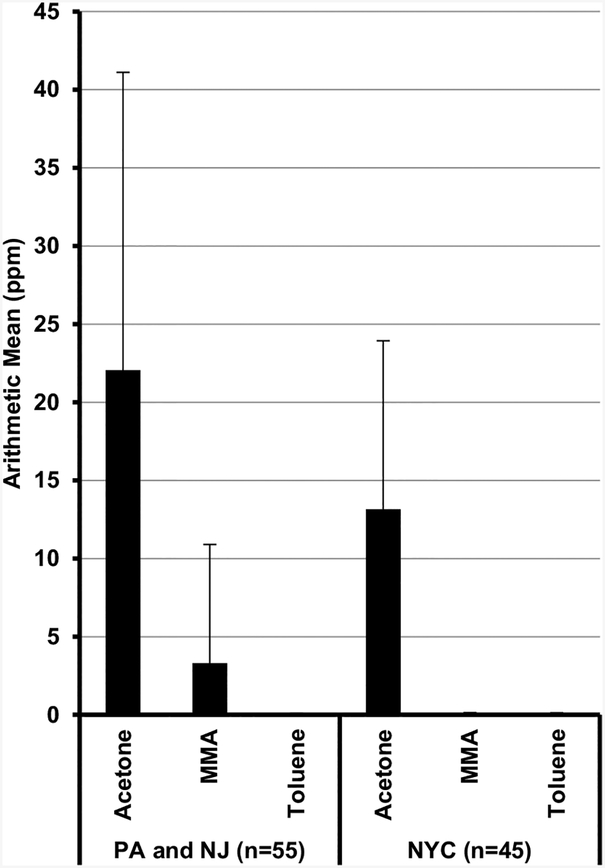
Figure 2 shows comparison results at the geographic level. For acetone and MMA, salons in Philadelphia and the southern New Jersey region (the greater Philadelphia metropolitan area) had significantly higher (p < 0.01) exposure levels than those in NYC, with 22.06 ppm vs. 13.15 ppm and 3.31 ppm vs. 0.09 ppm, respectively. There was no detectable significant difference for toluene exposure level between these two regions.
Fig. 2.
Comparison of chemical exposures for workers working at PA/NJ (the greater Philadelphia metropolitan area) and NYC. Levels of both acetone and MMA showed significant differences between these two regions (p < 0.01)
Overall, our results indicate that nail salon workers tested in both Philadelphia and southern New Jersey received significantly higher VOC exposures compared to those tested in NYC.
Discussion
Previous studies on occupational health risks in the nail salon industry have been conducted in single geographic regions and focused mainly on Vietnamese immigrants, the largest workforce population in the nail salon business in the United States [3, 10, 16–18, 23]. In this study, we focused on three major Asian ethnic immigrant populations, Chinese, Korean, and Vietnamese, which dominate the nail salon business on the East Coast of the United States. We conducted the study in three different metropolitan regions, NYC, Philadelphia, and southern New Jersey.
Our results indicate an association between chemical exposure to VOCs in nail salon workplace settings and self-reported adverse health effects, such as nose, throat, eye, and skin irritations; headaches; and breathing problems (Table 3). This finding is consistent with previously published data [3, 10, 17]. The miscarriage rate among surveyed nail salon female workers was 15.6%, higher than the reported average rate in Asian women [24]. The average age of entry into the nail salon industry among surveyed workers was 33 years, with an average duration in the business of about 9 years (Table 1). Due to the nature of the nail salon industry and the workers’ immigrant status (Table 1, > 94% born outside of U.S.), the workforce in nail salons has a relatively high turnover rate. Therefore, our surveyed adverse health effects and health problems are likely underestimated, especially since nail salon workers who have experienced severe health symptoms, such as miscarriage or cancer, may have already left the industry.
Our personal chemical exposure results measured the level of VOC exposures among 100 nail salon workers in our surveyed salons. Due to the limitations of this device’s chemical exposure capacity, we selected acetone, MMA, and toluene as target chemical compounds for measurement [11, 25–29]. It is well-known that MMA and toluene are hazardous compounds that can directly cause severe adverse health effects. These two VOCs were measured in previous research studies, which can be used for comparison to our results [3, 19].
The mean value of acetone in our surveyed salons was 18.51 ppm, much higher than the 3.10 ppm mean value obtained in a previous study for area monitoring [3]. This finding indicates that nail salon workers in our study were exposed to acetone during their regular working shifts.
Our measured mean values for personal exposure level of MMA was 39.45 ppm, which is between the measurements of 69.67 ppm and 19.70 ppm found in a previously published intervention study [19]. Since the 1970s, MMA has been considered a poisonous and deleterious substance by the FDA. Although no regulation specifically prohibits the use of MMA monomers in cosmetic products, it is important that these products should not be applied directly to the skin, since direct contact can result in an allergic reaction and may cause fingernail damage and deformity, as well as contact dermatitis [11, 12, 26, 30]. Nonetheless, MMA has been detected in the majority of surveyed salons, even in U.S. states that have banned its use [3, 21]. While the measured mean level of MMA in this study is lower than 50–100 ppm, the Threshold Limit Value–Time-Weighted Average (TLV–TWA) set by the American Conference of Governmental Industrial Hygienists (ACGIH) and the Occupational Safety and Health Administration (OSHA), it is still much higher than the U.S. Environmental Protection Agency’s (EPA) recommended ambient air level of 0.17 ppm [3]. The majority of the 25 nail salons surveyed had low MMA concentrations with a level equal to or lower than the EPA recommended ambient air level. To the contrary, one salon (salon 21, Table 4) had four workers with extremely high levels of MMA, with 1510 ppm, 1370 ppm, 579 ppm, and 306 ppm, respectively, the highest of all salon measurements. We double-checked the accuracy of the data by contacting the testing laboratory and received confirmation that the results were without technical problems. This finding suggests that at least two of the four workers mentioned above may perform services other than regular manicures and pedicures, which alone would not raise MMA levels so significantly. This was also reported by Quach et al. [19]. One of the job tasks performed on test day was the application of artificial nails. This service required the use of an acrylic liquid monomer, which contains MMA. The use of MMA for acrylic nail services began in the 1960s, as it was much less expensive than safer alternatives, such as ethyl methacrylate (EMA). MMA is hazardous only when it is in liquid form. Its presence is made known by its distinctive strong fruity odor. Our results indicate that MMA is still in use for nail services by some salons, which should attract more attention from regulatory agencies.
The level of toluene was the lowest of our three VOC measurements, with a mean value of 0.09 ppm, similar to results reported from previous studies [3, 19]. These combined results demonstrated that the use of toluene in nail products has been greatly reduced to a level that meets exposure limits, and that toluene has been replaced with safer alternatives, or that it has been totally removed from the products. Since toluene is widely known for its toxicity, its use in nail products has long been under strict and extensive scrutiny and has been banned in many states.
Interestingly, our data showed significant differences in mean chemical exposure levels between Chinese, Korean, and Vietnamese nail salon workers. Specifically, Chinese workers had the lowest levels of acetone exposure, while Vietnamese workers had the highest level of MMA exposure (Fig. 1). Levels of toluene were similar among the three ethnic populations, due to reasons explained above. We further compared geographic differences in chemical exposures. Our comparison indicated that both acetone and MMA levels measured in NYC were significantly lower than those measured in Philadelphia and in the southern New Jersey region (Fig. 2). A possible reason for this difference could be the stricter regulations implemented in New York state [22]. Our data revealed health risk disparities between regions and ethnic populations of Asian immigrant nail salon workers, despite the fact that nail salon workers, as a whole, experience health disparities with regard to occupational chemical exposures.
The adverse or detrimental health effects to nail salon workers can be attributed to the products used in the salon, the number of services provided, the salon size and ventilation, and the use of PPE by workers, especially nose masks and gloves.
The hazardous chemicals contained in nail care products are the fundamental source and risk for chemical exposures to nail salon workers. To reduce chemical exposure levels, some brands use safer alternatives in place of hazardous chemicals. These non-toxic green products either do not contain the three notoriously toxic compounds, toluene, formaldehyde, and DBP, or do not contain more harmful compounds. In this study, we found that salons in NYC mainly used green products, while the majority of salons in Philadelphia and southern New Jersey still used many traditional products. One of the obvious reasons for this difference is that New York state has some of the strictest regulations in the nail salon business in the United States. Our tested chemical exposure results also reflected these differences (Table 4, Fig. 2).
The nail salons in our study had an average of 5 manicure and pedicure stations, comparable to previously published data (Table 2) [19]. In addition, our survey revealed that the average number of workers present at work each day in a salon is about 5, consistent with previously published numbers, and the average number of services provided by each worker is 7 (Table 2) [10]. Combined with the products selected and the salon work environment, the number, type, and duration of services form a second critical risk factor for chemical exposure in a nail salon.
The consistent use of PPE by nail salon workers, as recommended by OSHA, including the use of masks and gloves, can greatly reduce the level of personal chemical exposure when providing services. Unfortunately, observations from real-world practice in salons are not always in line with OSHA PPE recommendations. A study conducted in NYC reported that only one-quarter of the 415 surveyed nail salon workers used protective gloves when they were providing services [22]. Another interview study conducted in Florida reported a similar situation, with only 30% of manicurists using masks when providing services [18]. While our self-reported data indicated that 55% and 75% of workers used gloves and masks, respectively, our observations did not support the results. We noticed that the majority of workers did not wear gloves and masks when they were providing services. Some wore masks but did not always cover their noses. Moreover, many workers complained that the use of gloves interfered with personal comfort and efficiency and performance quality when providing services. The low frequency of PPE use by nail salon workers could be largely due to a lack of knowledge about the health risks of chemical exposure from nail salon products. A previous intervention study demonstrated that educational training could improve knowledge, behavior, and health for nail salon workers, although further research is needed to demonstrate the long-term health benefits of educational intervention [19].
Currently there are no chemical exposure standards specifically tailored to nail salon products. Standards used as references are from other occupational settings, which usually are not suitable for the nail salon working environment, especially when long-term adverse health effects from low levels of VOC exposure are considered. While the use of PPE is important to reduce chemical exposures in nail salon workers, suitable chemical exposure standards for nail salon products are needed in order to reduce chemical exposures and adverse health risks. A potential strategy to develop such standards is to advocate for policy makers to fill gaps in current regulation by requiring manufacturers to conduct premarket testing and to provide full disclosure of product ingredients, especially ingredients that are potentially hazardous [31, 32].
Based on the current situation in the nail salon business, strategies to reduce chemical exposures and health risks among nail salon workers and customers should include knowledge improvement among workers. Wearing PPE and using safe practices would further help avoid regular and accidental exposures [33]. It has been shown that educational intervention can enhance these strategies for reducing chemical exposures and health risks [19]. Overall, gradually increasing regulation and enforcing policies represents a fundamental strategy for reducing chemical exposures and health risks in nail salon workers, owners, and customers.
While this study, for the first time, obtained valuable data regarding health risks and chemical exposures from Asian immigrant nail salon workers in NYC, Philadelphia, and southern New Jersey, it had some limitations. This was a pilot study, and therefore the sample size was relatively small. In addition, the recruited salons and workers were not proportional to the target ethnic populations and the three different locations. Nail salon workers are a special workforce that is difficult to reach for study recruitment [16, 17, 19]. Specifically, we had difficulties in recruiting owners and workers from the Korean community in this study. In addition, our survey questions about health risks and health symptoms were answered by workers without any medical examination confirmations. Furthermore, we noticed that there were workers who intentionally provided misleading answers, as they had concerns about releasing certain information, such as insurance and health history. These factors could reduce the accuracy of our data and explain discrepancies in answers to similar questions. In this study, we also measured only three VOCs because of technical limitations. However, a more realistic picture of chemical exposure in nail salons would be provided by monitoring a number of hazardous VOCs through one measurement. The major health risk to nail salon workers is actually the synergistic effect of chronic exposure to numerous VOCs from nail salon products.
Our monitoring of chemical exposures in nail salon workers in this study, as well as in several previously published studies, was cross-sectional. While these research studies provide valuable data on occupational health risks among nail salon workers, they could not provide a direct association between nail salon chemical exposures and chronic health effects or symptoms in nail salon workers. Longitudinal prospective studies are needed in order to better evaluate the effects of chemical exposure on health, particularly the synergistic effects of numerous VOCs from nail salon products. Overall, enhancing health literacy among nail salon workers and updating regulation policies to enforce stricter regulations are two important steps in lowering occupational chemical exposure and health risks in nail salon workers, especially for chronic exposure effects. In the meantime, it is crucial to encourage the use of safe alternative products by both nail salon owners and customers, which can potentially also encourage manufacturers to produce more green products for meeting market needs. This will lead to a fundamental solution for reducing or eliminating chemical exposure in nail salon workers and can be achieved through many years’ efforts of delivering effective, culturally appropriate educational interventions among nail salon owners, workers, and customers.
Acknowledgements
This research was supported by faculty research funds, Temple University (PI: Grace X. Ma, PhD). The authors wish to thank the nail salon partners, volunteers, and Asian community coordinators. We thank Dr. Yin Tan at Center for Asian Health, Lewis Katz School of Medicine, Temple University for help in data analysis and manuscript review. The project was also partially supported by TUFCCC/HC Regional Comprehensive Cancer Health Disparity Partnership, Award Number U54 CA221704(5) (Contact PIs: Grace X. Ma, PhD and Olorunseun O. Ogunwobi, MD, PhD) from the National Cancer Institute of National Institutes of Health (NCI/NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NCI/NIH.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nail salons: Spending U.S. 2017. | Statistic. (n.d.). Statista. Retrieved February 13, 2019, from https://www.statista.com/statistics/276605/revenue-nail-salon-services-united-states/ [Google Scholar]
- 2.Barbers, Hairstylists, and Cosmetologists : Occupational Outlook Handbook: U.S. Bureau of Labor Statistics. (n.d.). Retrieved February 13, 2019, from https://www.bls.gov/ooh/personal-care-and-service/barbers-hairstylists-and-cosmetologists.htm#tab-6
- 3.Quach T, Gunier R, Tran A, Von Behren J, Doan-Billings P-A, Nguyen K-D, et al. (2011). Characterizing workplace exposures in Vietnamese women working in California nail salons. American Journal of Public Health, 101(Suppl 1), S271–S276. 10.2105/AJPH.2010.300099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoang KK (2015). Nailing race and labor relations: Vietnamese nail salons in majority-minority neighborhoods. Journal of Asian American Studies, 18(2), 113–139. 10.1353/jaas.2015.0017. [DOI] [Google Scholar]
- 5.Nails Magzine, 2012–2013 The big book. (2013). Retrieved from https://files.nailsmag.com/Market-Research/NAILSbb12-13stats.pdf
- 6.We Need Safe Cosmetics Reform Now! (n.d.). EWG. Retrieved February 13, 2019, from https://www.ewg.org/enviroblog/2013/05/we-need-safe-cosmetics-reform-now [Google Scholar]
- 7.Pak VM, Powers M, & Liu J (2013). Occupational chemical exposures among cosmetologists: Risk of reproductive disorders. Workplace Health Safety, 61(12), 522–528. 10.1177/216507991306101204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin C-C, Huang C-N, Wang J-D, Hwang Y-H, Shie R-H, Chang Y-Y, et al. (2013). Exposure to multiple low-level chemicals in relation to reproductive hormones in premenopausal women involved in liquid crystal display manufacture. International Journal of Environmental Research and Public Health, 10(4), 1406–1417. 10.3390/ijerph10041406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peters C, Harling M, Dulon M, Schablon A, Torres Costa J, & Nienhaus A (2010). Fertility disorders and pregnancy complications in hairdressers—A systematic review. Journal of Occupational Medicine and Toxicology (London, England), 5, 24 10.1186/1745-6673-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White H, Khan K, Lau C, Leung H, Montgomery D, & Rohlman DS (2015). Identifying health and safety concerns in Southeast Asian immigrant Nail Salon workers. Archives of Environmental & Occupational Health, 70(4), 196–203. 10.1080/19338244.2013.853644. [DOI] [PubMed] [Google Scholar]
- 11.Henriks-Eckerman M-L, & Korva M (2012). Exposure to airborne methacrylates in nail salons. Journal of Occupational and Environmental Hygiene, 9(8), D146–D150. 10.1080/15459624.2012.696023. [DOI] [PubMed] [Google Scholar]
- 12.Moreira J, Gonçalves R, Coelho P, & Maio T (2017). Eyelid dermatitis caused by allergic contact to Acrylates in artificial nails. Dermatology Reports, 9(1), 7198 10.4081/dr.2017.7198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grešner P, Świercz R, Wąsowicz W, & Gromadzińska J (2017). Faster health deterioration among nail technicians occupationally exposed to low levels of volatile organic compounds. International Journal of Occupational Medicine and Environmental Health, 30(3), 469–483. 10.13075/ijomeh.1896.00854. [DOI] [PubMed] [Google Scholar]
- 14.LoSasso GL, Rapport LJ, Axelrod BN, & Whitman RD (2002). Neurocognitive sequelae of exposure to organic solvents and (meth)acrylates among nail-studio technicians. Neuropsychiatry, Neuropsychology, and Behavioral Neurology, 15(1), 44–55. [PubMed] [Google Scholar]
- 15.Harris-Roberts J, Bowen J, Sumner J, Stocks-Greaves M, Bradshaw L, Fishwick D, et al. (2011). Work-related symptoms in nail salon technicians. Occupational Medicine (Oxford, England), 61(5), 335–340. 10.1093/occmed/kqr096. [DOI] [PubMed] [Google Scholar]
- 16.Quach T, Nguyen K-D, Doan-Billings P-A, Okahara L, Fan C, & Reynolds P (2008). A preliminary survey of Vietnamese nail salon workers in Alameda County, California. Journal of Community Health, 33(5), 336–343. 10.1007/s10900-008-9107-7. [DOI] [PubMed] [Google Scholar]
- 17.Roelofs C, Azaroff LS, Holcroft C, Nguyen H, & Doan T (2008). Results from a community-based occupational health survey of Vietnamese-American nail salon workers. Journal of Immigrant and Minority Health, 10(4), 353–361. 10.1007/s10903-007-9084-4. [DOI] [PubMed] [Google Scholar]
- 18.Ho K, Perrin KM, & Thomas KB (2007). The use of protective equipment among Vietnamese manicurists: A pilot study. International Journal of Health Promotion and Education, 45(4), 104–106. 10.1080/14635240.2007.10708113. [DOI] [Google Scholar]
- 19.Quach T, Varshavsky J, Von Behren J, Garcia E, Tong M, Nguyen T, et al. (2013). Reducing chemical exposures in nail salons through owner and worker trainings: An exploratory intervention study. American Journal of Industrial Medicine, 56(7), 806–817. 10.1002/ajim.22146. [DOI] [PubMed] [Google Scholar]
- 20.Park S-A, Gwak S, & Choi S (2014). Assessment of occupational symptoms and chemical exposures for nail salon technicians in Daegu City, Korea. Journal of Preventive Medicine and Public Health, 47(3), 169–176. 10.3961/jpmph.2014.47.3.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alaves VM, Sleeth DK, Thiese MS, & Larson RR (2013). Characterization of indoor air contaminants in a randomly selected set of commercial nail salons in Salt Lake County, Utah, USA. International Journal of Environmental Health Research, 23(5), 419–433. 10.1080/09603123.2012.755152. [DOI] [PubMed] [Google Scholar]
- 22.Basch C, Yarborough C, Trusty S, & Basch C (2016). Use of protective gloves in nail salons in Manhattan, New York City. Journal of Preventive Medicine and Public Health, 49(4), 249–251. 10.3961/jpmph.16.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Federman MN, Harrington DE, & Krynski KJ (2006). Vietnamese manicurists: Are immigrants displacing natives or finding new nails to polish? Industrial and Labor Relations Review, 59(2), 302–318. [Google Scholar]
- 24.Harb HM, Al-rshoud F, Dhillon R, Harb M, & Coomarasamy A (2014). Ethnicity and miscarriage: A large prospective observational study and meta-analysis. Fertility and Sterility, 102(3), e81 10.1016/j.fertnstert.2014.07.276. [DOI] [Google Scholar]
- 25.Wysocki CJ, Dalton P, Brody MJ, & Lawley HJ (1997). Acetone odor and irritation thresholds obtained from acetone-exposed factory workers and from control (occupationally unexposed) subjects. American Industrial Hygiene Association Journal, 58(10), 704–712. 10.1080/15428119791012342. [DOI] [PubMed] [Google Scholar]
- 26.Raposo I, Lobo I, Amaro C, Lobo ML, Melo H, Parente J, et al. (2017). Allergic contact dermatitis caused by (meth) acrylates in nail cosmetic products in users and nail technicians—A 5-year study. Contact Dermatitis, 77(6), 356–359. 10.1111/cod.12817. [DOI] [PubMed] [Google Scholar]
- 27.Borak J, Fields C, Andrews LS, & Pemberton MA (2011). Methyl methacrylate and respiratory sensitization: A critical review. Critical Reviews in Toxicology, 41(3), 230–268. 10.3109/10408444.2010.532768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Donald JM, Hooper K, & Hopenhayn-Rich C (1991). Reproductive and developmental toxicity of toluene: A review. Environmental Health Perspectives, 94, 237–244. 10.1289/ehp.94-1567945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hannigan JH, & Bowen SE (2010). Reproductive toxicology and teratology of abused toluene. Systems Biology in Reproductive Medicine, 56(2), 184–200. 10.3109/19396360903377195. [DOI] [PubMed] [Google Scholar]
- 30.Nutrition, C. for F. S. and A. (n.d.). Products—Nail Care Products. WebContent. Retrieved February 13, 2019, from https://www.fda.gov/Cosmetics/ProductsIngredients/Products/ucm127068.htm
- 31.Quach T, Liou J, Fu L, Mendiratta A, Tong M, & Reynolds P (2012). Developing a proactive research agenda to advance nail salon worker health, safety, and rights. Progress in Community Health Partnerships: Research, Education, and Action, 6(1), 75–82. 10.1353/cpr.2012.0005. [DOI] [PubMed] [Google Scholar]
- 32.Quach T, Tsoh JY, Le G, Le M, Pham A, Fu L, et al. (2015). Identifying and understanding the role of key stakeholders in promoting worker health and safety in nail salons. Journal of Health Care for the Poor and Underserved, 26(2 Suppl), 104–115. 10.1353/hpu.2015.0060. [DOI] [PubMed] [Google Scholar]
- 33.Safety and Health Topics| Personal Protective Equipment| Occupational Safety and Health Administration. (n.d.). Retrieved February 13, 2019, from https://www.osha.gov/SLTC/personalprotectiveequipment/