Abstract
Background:
Infant consumption of formula reconstituted with fluoridated water can lead to excessive fluoride intake. We examined the association between fluoride exposure in infancy and intellectual ability in children who lived in fluoridated or non-fluoridated cities in Canada.
Methods:
We examined 398 mother-child dyads in the Maternal-Infant Research on Environmental Chemicals cohort who reported drinking tap water. We estimated water fluoride concentration using municipal water reports. We used linear regression to analyze the association between fluoride exposure and IQ scores, measured by the Wechsler Primary and Preschool Scale of Intelligence-III at 3 to 4 years. We examined whether feeding status (breast-fed versus formula-fed) modified the impact of water fluoride and if fluoride exposure during fetal development attenuated this effect. A second model estimated the association between fluoride intake from formula and child IQ.
Results:
Thirty-eight percent of mother-child dyads lived in fluoridated communities. An increase of 0.5 mg/L in water fluoride concentration (approximately equaling the difference between fluoridated and non-fluoridated regions) corresponded to a 9.3- and 6.2-point decrement in Performance IQ among formula-fed (95% CI: −13.77, −4.76) and breast-fed children (95% CI: −10.45, −1.94). The association between water fluoride concentration and Performance IQ remained significant after controlling for fetal fluoride exposure among formula-fed (B = −7.93, 95% CI: −12.84, −3.01) and breastfed children (B = −6.30, 95% CI: −10.92, −1.68). A 0.5 mg increase in fluoride intake from infant formula corresponded to an 8.8-point decrement in Performance IQ (95% CI: −14.18, −3.34) and this association remained significant after controlling for fetal fluoride exposure (B = −7.62, 95% CI: −13.64, −1.60).
Conclusions:
Exposure to increasing levels of fluoride in tap water was associated with diminished non-verbal intellectual abilities; the effect was more pronounced among formula-fed children.
Keywords: Fluoride, Infants, Formula, Water fluoridation, Intellectual function
1. Introduction
Fluoride can occur naturally in water and, in some communities, is added to water supplies to reach the recommended concentration of 0.7 mg/L for the prevention of tooth decay1. About 74% of Americans and 38% of Canadians on municipal water are supplied with fluoridated drinking water. Water fluoridation has been reported to reduce the prevalence of tooth decay by 26% to 44%2,3 in youth and by 26%2 to 27%3 in adults. Infants who are fed formula reconstituted with fluoridated water have approximately three to four times greater exposure to fluoride than adults4 on a per body-weight basis. Formula-fed infants residing in fluoridated areas have an approximate 70-fold higher fluoride intake than exclusively breastfed infants5–8
The prevalence of enamel fluorosis, a discoloration of enamel resulting from chronic, excessive ingestion of fluoride during tooth development9–11, is higher among formula-fed infants than breastfed infants9,10,12–15. While enamel fluorosis develops from excess fluoride exposure during the first four years of life,16 the first 12 months are the most vulnerable period10,15. The risk of fluorosis increases with higher levels of fluoride in the water supply for formula-fed infants17.
Breastmilk contains extremely low concentrations of fluoride (0.005–0.01 mg/L) due to the limited transfer of fluoride in plasma into breastmilk6–8,18–21. Exclusive breastfeeding for six months, which is recommended by current practice guidelines22,23, is reported by 25% of mothers in the United States24 and Canada25. Ninety percent of bottle-fed infants are fed powdered formula26 and 75% of mothers report using tap water to reconstitute formula10. Thus, reconstituted formula is the major source of nutrition for many infants in the United States and Canada.
Despite growing concerns about excessive exposure to fluoride during infancy and the vulnerability of the developing brain27,28, no studies have tested the potential neurotoxicity of using optimally fluoridated drinking water to reconstitute formula during infancy29. Increased fluoride exposure during fetal brain development was associated with diminished IQ scores in two birth cohort studies30–32, among a number of recent studies conducted in endemic fluorosis areas33–35, as well as a 2012 meta-analysis of 27 ecologic studies36. Increased fluoride exposure has also been linked with ADHD-related behaviors in children37–39.
We investigated the association between water fluoride concentration and intellectual abilities of Canadian children who were formula-fed or breastfed. In addition, we tested whether postnatal effects of fluoride exposure on child IQ remained after controlling for fetal exposure.
2. Materials and Methods
2.1. Study population
Between 2008 and 2011, the Maternal-Infant Research on Environmental Chemicals (MIREC) program recruited 2,001 pregnant women from ten Canadian cities to participate in a longitudinal pregnancy cohort study. Women who could communicate in English or French, were >17 years, and were <14 weeks gestation were recruited from prenatal clinics. Participants were excluded if there was a known fetal abnormality, if they had any medical complications, or if there was known illicit drug use during pregnancy. Additional details are in the cohort profile description40.
Of the 610 children who were recruited to participate in the developmental follow-up phase of the study (MIREC-Child Development Plus), 601 completed all testing. Children were recruited from six of the cities in the original cohort (Vancouver, Toronto, Hamilton, Halifax, Kingston, Montreal); approximately half of the children lived in non-fluoridated cities and half lived in fluoridated cities.
This study received ethics approval from Health Canada and York University.
2.1. Infant Feeding Assessment
When children were between 30 and 48 months of age, mothers completed an infant feeding questionnaire asking, “How old was your baby when you ceased breastfeeding exclusively? At what age did you introduce other type of milk or food to your baby?”. Women who breastfed exclusively for six months or longer were included in the breastfeeding (BF) group; those who reported introducing formula within the first six months (never breastfed or partial breastfeeding) were included in the formula-feeding (FF) group.
To explore the possibility of recall or response bias of mothers completing the questionnaire, we compared information reported by mothers when their children were between 30 and 48 months of age (i.e. time when the questionnaire was completed for classifying the BF and FF groups) with information reported by a subset of women at an earlier visit when their children were between 6 and 8 months of age. Information about infant feeding was only available for 11% of the sample at the infant visit. Among women who provided information at both occasions, the median difference for when breastfeeding was reported to be ceased was 0 months; responses were within 1.5 months of each other for two-thirds of this subsample.
We dichotomized feeding status at six months because the Canadian Pediatric Society and American Academy of Pediatrics both recommend exclusive breastfeeding for six months22,23. Moreover, formula-fed infants who are younger than six-months derive most of their nutrition from formula, placing this group at highest risk of exceeding the recommended upper limit (0.7 mg/d) for fluoride4,29,41. Finally, fluoride intake differences become less evident when other dietary sources of fluoride are introduced at around six months6.
2.2. Infant Fluoride Exposure
We estimated fluoride concentrations in drinking water by accessing daily or monthly reports provided by water treatment plants. Water reports were first linked with mothers’ postal codes and the daily or weekly amounts were averaged over the first six-months of the child’s life. We only included participants whose postal codes could be linked to a water treatment plant that provided water fluoride measurements. We also excluded participants who reported that their primary drinking source was from a well or ‘other’ (e.g. bottled water) (Table S1). Further details can be found in our previous report42.
To obtain a continuous fluoride exposure estimate collapsed across the BF and FF groups, we estimated fluoride intake from formula (in mg F/day) by multiplying water fluoride concentration by the amount of time that the infant was not exclusively breastfed in the first year using the following equation:
where water_F mg/L refers to the average water fluoride concentration and 1-#mo_excl_BF/11.99 represents the proportion over the 12-month period the infant was not exclusively breastfed. A value near one indicates that an infant was primarily formula-fed over the 12 months whereas a value near zero indicates an infant primarily breastfed. We estimated fluoride intake based on an average of 0.80 L of water used to reconstitute powdered formula as suggested by an infant food diary completed for infants in a prior study43; the average milk intake at 3 months of age is 0.812 L per day, ranging from 0.523 to 1.124 L44. Because we did not know the type of formula used (i.e. soy- or milk-based), we did not add fluoride derived from formula to our fluoride intake estimate. Previous studies have indicated that fluoride from water used in formula is a greater source of fluoride than fluoride found in formula45.
2.3. Fetal Fluoride Exposure
We used maternal urinary fluoride (MUF) adjusted for specific gravity as a proxy of fetal fluoride exposure. MUF, which was derived by averaging three spot samples collected across all three trimesters of pregnancy, was considered our most reliable measure of exposure42. Urinary fluoride concentrations were analyzed at the Indiana University School of Dentistry using a modification46 of the hexamethyldisiloxane (Sigma Chemical Co., USA) micro-diffusion procedure previously described31.
2.4. Intelligence Assessment
We assessed children’s intellectual abilities between ages 3.0 and 4.0 years with the Wechsler Preschool and Primary Scale of Intelligence-III47 using United States population-based normative data (mean = 100, SD = 15). Outcomes included Full Scale IQ (FSIQ), a measure of global intellectual functioning, Verbal IQ (VIQ), a measure of verbal reasoning, and Performance IQ (PIQ), a measure of non-verbal reasoning and visual-motor coordination skills.
2.5. Covariates
We adjusted for potential confounding by selecting covariates a priori that have been associated with fluoride, breastfeeding, and children’s intellectual abilities. Final covariates included child’s sex and age at testing, maternal education (dichotomized as either a bachelor’s degree or higher versus trade school diploma or lower), maternal race (white or not), second-hand smoke in the home (yes, no), and quality of the child’s home environment (measured at time of testing using the Home Observation for Measurement of the Environment (HOME) - Revised Edition48). For each analysis, a covariate was retained in the final model if its p-value was <.20 or its inclusion changed the regression coefficient of water fluoride concentration or fluoride intake from formula by more than 10%49.
2.6. Statistical analyses
We used linear regression to model differences in child IQ by water fluoride concentration while controlling for covariates. In our first model, we examined whether feeding status (BF or FF) modified the impact of water fluoride. In our second model, we estimated the association between fluoride intake from formula and child IQ. We controlled potential confounders by including them simultaneously with predictors.
In secondary analyses, we controlled for MUF during pregnancy in both models to account for fetal exposure. We also tested for sex-specific effects because we previously found that MUF concentration was only associated with diminished FSIQ in males31.
Regression diagnostics indicated no assumption violations pertaining to linearity, normality, or homogeneity of variance. Specifically, QQ-plots of residuals were consistent with a normal distribution and plots of residuals against fitted values did not suggest any assumption violations. Two observations were investigated based on a plot of Cook’s D that suggested they may be influential; these cases had extremely low IQ scores that were more than 2.5 standard deviations from the sample mean. In a sensitivity analyses, we re-estimated the models after removing these two observations. Finally, variance inflation factors indicated no concerns with excessive multicollinearity.
To aid interpretation, we divided all regression coefficients by 2 so that they represent the predicted IQ difference per 0.5 mg/L of fluoride in tap water or 0.5 mg fluoride from formula; 0.5 mg/L corresponds to the approximate difference between mean water fluoride level in fluoridated versus non-fluoridated regions in our sample.
3. Results
Of the 601 children who completed neurodevelopmental testing, 591 (99%) mother-child pairs completed the infant feeding questionnaire and IQ testing (BF: n = 296; FF: n = 295). Of these, 398 (67.3%) pairs reported drinking tap water, had water fluoride data and complete covariate data (BF: n = 200; FF: n = 198). The demographic characteristics of women included in the current analyses (n = 398) were not substantially different from the original MIREC cohort (N = 1945) or the subset without complete water fluoride and covariate data (n = 203) (Table S2).
Among the BF group, more women who lived in a fluoridated region had a bachelor’s degree or higher compared with those in a non-fluoridated region (86 vs. 74%, p = .001) (Table 1). Compared with the FF group, women in the BF group were more educated, more likely to be married or common law, and had higher HOME scores (all ps < .05). The BF group had significantly higher FSIQ and VIQ scores relative to the FF group (Table 1; Figure S1). Children living in a fluoridated region had a significantly lower PIQ score, but higher VIQ score, relative to children living in a non-fluoridated region (Table 1; Figure S1).
Table 1.
Demographic characteristics and exposure outcomes for mother-child pairs by infant feeding status.
| Breastfed ≥6 mo. (n = 200) | Formula-fed (n = 198) | ||||
|---|---|---|---|---|---|
| Characteristic | Fluoridated | Non-fluoridated | Fluoridated | Non-fluoridated | p value comparing BF and FF groups |
| (n = 83) | (n = 117) | (n = 68) | (n = 130) | ||
| Mean (SD) / % | Mean (SD) / % | Mean (SD) / % | Mean (SD) / % | ||
| Maternal Characteristics | |||||
| Years of age at delivery | 32.54 (3.64) | 32.86 (4.79) | 32.91 (4.42) | 32.39 (5.11) | .73 |
| Net household income >$70K | 70.3 | 72.9 | 79.7 | 68 | .88 |
| Caucasian | 88 | 93 | 88 | 84 | .11 |
| Maternal education | |||||
| Trade school diploma/high school | 14 | 26* | 28 | 42* | <.001 |
| Bachelor’s degree or higher | 86 | 74* | 72 | 58* | <.001 |
| Employed at time of pregnancy | 92 | 90 | 94 | 84* | .40 |
| Married/common-law (at time of testing) | 100 | 99 | 96 | 92 | .001 |
| Smoked in trimester 1 | 0 | 1.7 | 2.9 | 3.8 | .17 |
| Parity (first birth) | 45 | 51 | 43 | 47 | .61 |
| Number of months exclusively breastfeeding | 7.54 (2.95) | 7.45 (2.46) | 2.63 (2.08) | 2.37 (2.13) | < .001 |
| Child characteristics | |||||
| Years of age at IQ testing | 3.48 (0.29) | 3.34 (0.31)* | 3.53 (0.28) | 3.37 (0.3)* | .32 |
| Female sex | 51 | 53 | 54 | 47 | .32 |
| HOME total score | 48.71 (3.42) | 48.09 (3.86) | 47.59 (4.33) | 46.55 (4.76) | < .001 |
| Second hand smoke in home | 2.5 | 3.4 | 4.4 | 5.4 | .43 |
| Gestational age in weeks | 39.22 (1.55) | 39.17 (1.52) | 38.68 (2.48) | 39.15 (1.53) | .24 |
| Birth weight (kg) | 3.42 (0.50) | 3.49 (0.46) | 3.43 (0.62) | 3.46 (0.52) | .75 |
| Full Scale IQ | 109.9 (12.4) | 108.9 (13.6) | 106.1 (15.8) | 106.8 (13.5) | .03a |
| Verbal IQb | 115.1 (11.3) | 110.4 (12.4)* | 110.9 (14.9) | 107.1 (13.3) | .00a |
| Performance IQb | 102.0 (15.2) | 105.6 (15.8) | 99.7 (15.1) | 105.6 (13.4)* | .69 |
| Exposure Variables | |||||
| Water fluoride concentration (mg/L) | 0.58 (0.08) | 0.13 (0.06)* | 0.59 (0.07) | 0.13 (0.05)* | .18 |
| % living in fluoridated region | 41.5 | 34.3 | .14 | ||
| Infant fluoride intake (mg F/day) | 0.12 (0.07) | 0.02 (0.02)* | 0.34 (0.12) | 0.08 (0.04)* | < .001 |
| MUF concentration (mg/L) | 0.70 (0.39) | 0.42 (0.28)* | 0.64 (0.37) | 0.38 (0.27)* | .07 |
Abbreviations: HOME = Home Observation for Measurement of the Environment; MUF = Maternal urinary fluoride, adjusted for specific gravity; SD = standard deviation.
p <.05 for comparing participants in the breastfed or formula-fed group living in a fluoridated versus non-fluoridated region.
p-value reported for main effect of feeding status from 2×2 ANCOVA, adjusting for maternal education (binary), maternal race (binary), child’s age at IQ testing (continuous), child’s sex, HOME total score (continuous), second-hand smoke status in the child’s house (yes, no), and water fluoridation status (fluoridated versus non-fluoridated).
Main effect of fluoridation status, adjusting for maternal education (binary), maternal race (binary), child’s age at IQ testing (continuous), child’s sex, HOME total score (continuous), second-hand smoke status in the child’s house (yes, no), and feeding status (BF vs. FF); VIQ: p=.02; PIQ: p<.001.
Water fluoride concentration was correlated with MUF (r = .37, p < .001) and estimated fluoride intake from formula (r = .79, p < .001); MUF was correlated with fluoride intake from formula (r = .55, p < .001).
3.1. Feeding status
The mean duration of exclusive breastfeeding was 4.98 months (SD = 3.48); 54 (13.6%) women reported never breastfeeding, 32 (8%) reported discontinuing breastfeeding after the first three months, and 200 (50.2%) reported continuing to breastfeed at six months or longer. Water fluoride concentration did not significantly differ between the BF (M = 0.32 mg/L) and FF groups (M = 0.29 mg/L; p = .18).
3.2. Model 1: IQ scores and water fluoride concentration by feeding status
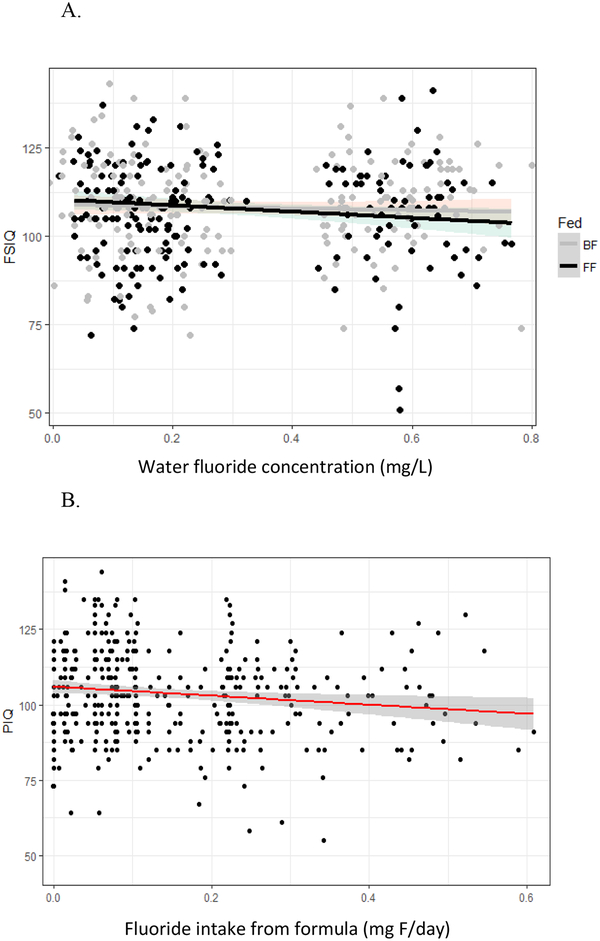
A 0.5 mg/L increase in water fluoride concentration was associated with a decrease of 4.4 FSIQ points (95% CI: −8.34, −0.46, p = .03) in the FF group, but it was not significantly associated with FSIQ in the BF group (B = −1.34, 95% CI: −5.04, 2.38, p = .48) (Table 2; Figure 1A); the interaction between water fluoride and feeding status was not statistically significant (p = .26). Controlling for fetal exposure by adding MUF to the model resulted in non-significant associations between water fluoride concentration and FSIQ in both the FF (B = −3.58, 95% CI: −7.83, 0.66, p = .098) and BF groups (B = −1.69, 95% CI: −5.66, 2.27, p = .40). Removing two cases with extreme IQ scores from the models resulted in non-significant associations between water fluoride concentration and FSIQ in both groups (Table S3).
Table 2.
Adjusted difference in IQ scores at 3–4 years of age per 0.5 mg/L water fluoride concentration and 0.5 mg infant fluoride intake from formula per day, with and without adjusting for maternal urinary fluoride (MUF).
| Exposure variable | N | FSIQ | N | PIQ | N | VIQ |
|---|---|---|---|---|---|---|
| B (95% CI) | B (95% CI) | B (95% CI) | ||||
| Model 1 | ||||||
| Water Fl (mg/L) | 398 | 393 | 397 | |||
| Formula-fed | −4.40 (−8.34, −0.46)* | −9.26 (−13.77, −4.76)* | 0.89 (−2.87, 4.65) | |||
| Breastfed | −1.34 (−5.04, 2.38) | −6.19 (−10.45, −1.94)* | 3.06 (−0.49, 6.61) | |||
| Water Fl (mg/L) adjusted for MUFa | 350 | 345 | 349 | |||
| Formula-fed | −3.58 (−7.83, 0.66) | −7.93 (−12.84, −3.01)* | 2.60 (−1.98, 7.16) | |||
| Breastfed | −1.69 (−5.66, 2.27) | −6.30 (−10.92, −1.68)* | 4.20 (−0.06, 8.45) | |||
| Model 2 | ||||||
| Fluoride intake from formula | 398 | −2.69 (−7.38, 2.01) | 393 | −8.76 (−14.18, −3.34)* | 397 | 3.08 (−1.40, 7.55) |
| Fluoride intake from formula adjusted for MUFb | 350 | −1.94 (−7.09, 3.21) | 345 | −7.62 (−13.64, −1.60)* | 349 | 3.05 (−1.89, 7.98) |
p <.05
Abbreviations: Fl = fluoride; MUF = maternal urinary fluoride; Regression model adjusted for maternal education (binary), maternal race (binary), child’s age at IQ testing (continuous), child’s sex, HOME total score (continuous), and second-hand smoke status in the child’s house (yes, no)
MUF was not significantly associated with FSIQ score (B = −1.08, 95% CI: −1.54, 0.47, p = .29), PIQ score (B = −1.31, 95% CI: −3.63, 1.03, p = .27), or VIQ score (B = −0.34, 95%CI: −2.21, 1.59, p=.73). Note: regression coefficients represent the predicted IQ difference per 0.5 mg/L MUF; effect for both sexes is reported. Variance inflation factor (VIF) for water Fl is 2.41 for FSIQ, 2.41 for PIQ, and 2.40 for VIQ when MUF is entered in the model.
MUF is significantly associated with PIQ score (B = −2.38, 95% CI: −4.62, −0.27, p = .04), but not FSIQ score (B = −1.50, 95% CI: −3.41, 0.43, p = .13) or VIQ score (B = −0.11, 95% CI: −1.94, 1.74, p = .91); Note: regression coefficients represent the predicted IQ difference per 0.5 mg/L MUF; effect for both sexes is reported. Variance inflation factor (VIF) for infant fluoride intake is 1.10 for FSIQ, 1.12 for PIQ, and 1.10 for VIQ when MUF is entered in the model.
Figure 1.
A. Water fluoride concentration as a predictor of Full Scale IQ with an interaction by formula-fed (FF) vs. breastfed (BF) group. Black data points represent the FF group and grey data points represent the BF group. B. Fluoride intake from formula (mg F/day) as a predictor of Performance IQ score.
Water fluoride concentration was significantly associated with lower PIQ in the FF (B = −9.26, 95% CI: −13.77, −4.76, p < .001) and the BF groups (B = −6.19, 95% CI: −10.45, −1.94, p = .004) (Table 2); the interaction was not significant (p = .26). Controlling for MUF, water fluoride concentration remained significantly associated with PIQ in the FF (B = −7.93 95% CI: −12.84, −3.01, p = .002) and BF groups (B = −6.30, 95% CI: −10.92,−1.68, p = .008). Likewise, the associations between water fluoride concentration and PIQ remained significant for both groups after removing two cases with extreme IQ scores (Table S3).
In contrast, water fluoride concentration was not associated with VIQ in the FF (B = 0.89, 95% CI: −2.87, 4.65, p = .64) or BF group (B = 3.06, 95% CI: −0.49, 6.61, p = .09); these associations remained non-significant after controlling for MUF (Table 2) and removing two cases with extreme IQ scores (Table S3).
3.3. Model 2: IQ scores and fluoride intake from formula
Fluoride intake from formula was not significantly associated with FSIQ (B = −2.69, 95% CI: −7.38, 2.01, p = .26) or VIQ (B = 3.08, 95% CI: −1.40, 7.55, p = .18) (Table 2). In contrast, a 0.5 mg increase in fluoride intake predicted an 8.76-point decrement in PIQ score (95% CI: −14.18, −3.34, p = .002; Figure 1B). Adding MUF to the PIQ model slightly attenuated the association between fluoride intake and PIQ (B = −7.62, 95% CI: −13.64, −1.60, p = .01) (Table 2). Removing two cases with extreme IQ scores did not appreciably alter the association between fluoride intake and PIQ score, with and without adjustment for MUF (Table S3).
4. Discussion
We found a decrease of 4.4 FSIQ points among preschool children who were formula-fed in the first six months of life for each 0.5 mg/L increase in water fluoride concentration, which is the approximate difference in mean water fluoride level between fluoridated (0.59 mg/L) and non-fluoridated (0.13 mg/L) regions. In contrast, we did not find a significant association between water fluoride concentration and FSIQ among exclusively breastfed children. The association between water fluoride concentration and FSIQ must be interpreted with caution, however, because the association became non-significant when two outliers were removed. We observed an even stronger association between water fluoride and PIQ (non-verbal intelligence). A 0.5 mg/L increase in water fluoride level predicted a decrement in PIQ in both the formula-fed (9.3-points) and the breastfed groups (6.2-points). Adjusting for fetal exposure or removing two extreme scores did not appreciably alter these results.
We observed converging results using fluoride intake from formula, which is a continuous, time-weighted exposure estimate. For each 0.5 mg/day of fluoride intake, we found an 8.8-point decrement in PIQ; adjusting for fetal exposure using MUF attenuated the association only slightly (7.6-point decrement in PIQ). MUF was also negatively associated with PIQ (2.4-point decrement for each 0.5 mg/L increase in MUF). The fluoride intake estimate may reflect a more refined measure of exposure in infancy because it captures differences in both water fluoride level and the proportion of time each child was given formula over the first year of life. Yet, our binary classification of whether a child was exclusively breastfed for 6 months may better capture children who are most vulnerable to neurotoxic effects of fluoride because it subsets those exposed to fluoride during the early infancy period when the brain undergoes significant development50,51. Taken together, these findings suggest that using optimally fluoridated water (0.7 mg/L) to reconstitute infant formula may diminish the development of intellectual abilities in young children, particularly for non-verbal abilities. The findings also suggest that both prenatal and postnatal fluoride exposure affect the development of non-verbal intelligence to a greater extent than verbal intelligence. Prior studies examining prenatal exposure to fluoride and IQ showed a similar pattern30,31.
Consistent with prior studies showing a positive effect of breastfeeding on cognition52, children in the breastfed group had higher FSIQ and VIQ scores relative to the formula-fed group, regardless of fluoridation status; higher education and income levels in the breastfed group likely accounts for part of this association53. In contrast, the breastfed group did not differ significantly from the formula-fed group with respect to PIQ score. Children who lived in non-fluoridated regions showed higher PIQ scores than children who lived in fluoridated regions, though this difference was significant only for the formula-fed group, perhaps reflecting a higher vulnerability of nonverbal abilities to fluoride exposure in infancy.
Most studies of fluoride exposure from infant formula consumption have focused on risk for later development of dental enamel fluorosis11,15,54. Beyond fluorosis, the safety of fluoride exposure from infant formula has not been rigorously tested, despite warnings of overexposure55. A recent study showed that up to 59% of infants younger than four months exceed the upper limit (0.1 mg/kg/day)41 when optimally fluoridated water is used to reconstitute infant formula29; 33% and 14.3% of six- and nine-month old infants exceeded the upper limit threshold, respectively. Conversely, breastfed infants receive very low fluoride intake (generally less than 0.01 mg/L), even in communities with fluoridated water7,8,19. Our estimate of fluoride intake (0.34 mg F/day) among formula-fed infants who live in a fluoridated region is an underestimate of actual fluoride intake because we did not include fluoride from other sources, such as the fluoride found in the formula or foods; thus, the association between fluoride intake and IQ scores among formula-fed infants may be stronger than the association obtained in our analysis.
Our results, which showed that higher fluoride exposure in infancy was associated with diminished IQ scores in young children, are consistent with two longitudinal birth cohort studies. In one study involving 299 mother-child pairs living in Mexico City, there was a decrement of 3.2 IQ points in preschool aged children for every 0.5 mg/L of MUF level during pregnancy30. In the other study, which we conducted using the same Canadian cohort, we reported a decrement of 2.2 IQ points among preschool aged boys for every 0.5 mg/L of MUF level during pregnancy31. When MUF was included as a covariate in the current study, the association between MUF and FSIQ was not significant (see Table 2, note a). This discrepancy arises because (1) Green et al.31 did not include fluoride exposure in infancy as a covariate and (2) Green et al.31 estimated sex-specific MUF effects whereas the current study estimated an overall MUF effect.
The beneficial effects of fluoride predominantly occur at the tooth surface, after teeth have erupted56. Fluoride contributes to the prevention of dental caries primarily when it is topically applied to teeth, such as brushing with fluoridated toothpaste4,56–59. Because fluoride is not essential for growth and development60, there is no recommended intake level of fluoride during fetal development or in the first six months of life before teeth have erupted. Accordingly, the Canadian Pediatric Society recommends administering supplemental fluoride (i.e. systemic exposure) only when primary teeth begin to erupt61 (at approximately 6 months) and only if the child is susceptible to high caries activity and is not exposed to other fluoride-based interventions, such as toothbrushing or water fluoridation62.
The American Dental Association54,63 advises parents to use optimally fluoridated drinking water to reconstitute concentrate infant formulas, while being cognizant of the potential risk of mild enamel fluorosis development. This recommendation is echoed by the Centers for Disease Control and Prevention64 as well as the U.S. Department of Health and Human Services65. The Canadian Dental Association66 recommends using water with low fluoride concentration (or ready-to-feed formula) when the fluoride level in drinking water is above the optimal level. In addition to tap water, which is reportedly used by 93% of caregivers who feed formula to infants11, “nursery” water (which may contain up to 0.7 mg F/L) is marketed for reconstituting formula and sold in Canada and the United States. The availability of fluoridated nursery water gives the false impression that fluoride exposure during early infancy is beneficial prior to teeth eruption.
Formula-fed infants who reside in fluoridated areas have a 70-fold higher intake of fluoride than exclusively breastfed infants5–8. Formula-fed infants also retain more fluoride than breastfed infants6,18 because infants have a limited capacity to excrete fluoride before renal function reaches its full capacity at about two years of age4,6. Fluoride absorption also depends on the presence of other nutrients1; when fluoride intake is exclusively from reconstituted formula, the bioavailability of fluoride is 65%, whereas a varied diet reduces fluoride absorption in tissues and bone to about 47%67. These factors place formula-fed infants at an even higher risk of fluoride toxicity.
Our study has some limitations. First, infant formulas vary in fluoride content. Ready-to-use formulas typically have less fluoride than powdered formula7,68; information about formula type was only available for 100 of 198 (50.5%) participants in the formula group; of those, 75% reported using powdered formula, which is the most common type of formula used by the general population26,69. Variability in fluoride content is also seen across different types of powdered formula5,29,70. Additionally, soy-based formula reconstituted with distilled water has more fluoride (0.24–0.30 mg/L depending on whether it is ready-to-feed or concentrated) than milk-based powdered formulas (0.12–0.17 mg/L)10,29,71. Although we lacked data on brand of formula, we have no reason to expect that use of powdered versus ready-to-feed or soy- versus milk-based formula would differ by fluoridation status. Moreover, our effects were primarily based on water fluoride content, which is the major source of fluoride9. Second, we did not have specific information on the type of water (bottled versus tap) used to reconstitute formula. However, mothers typically report using tap water for reconstituting formula10 and we only included children of women who reported drinking tap water in our analyses. Third, there is potential for non-differential misclassification of the feeding status variable because mothers may have been confused by the definition of exclusive breastfeeding on the questionnaire or the responses may have been affected by recall or response bias. As with any survey, women could be confused by the question, but given the demographic of the sample – highly educated, English speaking, and non-teenage mothers – confusion seems less likely. Fourth, our method of estimating infant fluoride intake has not been validated. Finally, children were tested between 3 and 4 years of age and we have no information regarding other possible sources of fluoride that occurred between post-weaning and the age of testing. Thus, other sources of fluoride (e.g. dental products) or more frequent brushing, might differ between participants who lived in fluoridated versus non-fluoridated communities or among those in the breastfeeding versus formula-feeding group. To control for these potential differences, we included maternal education in all models. In addition, the design of our study compares water fluoride level and IQ scores in the formula-fed children using the breast-fed children as a control.
In summary, fluoride intake among infants younger than 6 months may exceed the tolerable upper limits if they are fed exclusively with formula reconstitued with fluoridated tap water. After adjusting for fetal exposure, we found that fluoride exposure during infancy predicts diminished non-verbal intelligence in children. In the absence of any benefit from fluoride consumption in the first six months, it is prudent to limit fluoride exposure by using non-fluoridated water or water with lower fluoride content as a formula diluent.
Supplementary Material
Highlights:
Consumption of formula reconstituted with fluoridated water can lead to excessive fluoride intake.
Breastfed infants receive very low intake of fluoride.
We compared IQ scores in 398 children who were formula-fed versus breastfed during infancy.
IQ scores were lower with higher levels of fluoride in tap water.
The effect was more pronounced among formula-fed children, especially for nonverbal skills.
Acknowledgements
The authors gratefully acknowledge: Nicole Lupien, Stéphanie Bastien, and Romy-Leigh McMaster and the MIREC Study Coordinating Staff for their administrative support, as well as the MIREC study group of investigators and site investigators; the INSPQ for measuring the urinary creatinine; Christine Buckley, Dr. Frank Lippert and Prithvi Chandrappa for their analysis of urinary fluoride at the Indiana University School of Dentistry; and Dr. John Minnery for his valuable engineering advice regarding water fluoridation. The authors are also grateful to the staff affiliated with community water treatment plants who helped to provide water fluoride data for this study.
Funding Source: This study was funded by a grant from the National Institute of Environmental Health Science (NIEHS) (grant #R21ES027044). The MIREC Study was supported by the Chemicals Management Plan at Health Canada, the Ontario Ministry of the Environment, and the Canadian Institutes for Health Research (grant # MOP-81285).
Financial Disclosure: The authors have no financial disclosures.
Abbreviations:
- BF
breastfed
- FF
formula fed
- CI
confidence intervals
- HOME
Home Observation for Measurement of the Environment
- IQ
intelligence quotient
- FSIQ
Full Scale IQ
- PIQ
Performance IQ
- VIQ
Verbal IQ
- MIREC
Maternal-Infant Research on Environmental Chemicals
- MUF
maternal urinary fluoride
- SD
standard deviation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors have no conflicts of interest relevant to this article to disclose.
References
- 1.Health Canada. Guidelines for Canadian Drinking Water Quality: Guideline Technical Document —Fluoride. Ottawa, Ontario, Air and Climate Change Bureau, Healthy Environments and Consumer Safety Branch, Health Canada, Ottawa, Ontario; 2010. doi:Catalogue No. H128-1/11-647E-PDF. [Google Scholar]
- 2.Iheozor-Ejiofor Z, Worthington HV, Walsh T, O’Malley L, Clarkson JE, Macey R, Alam R, Tugwell P, Welch VG AM Water fluoridation for the prevention of dental caries. Cochrane Database Syst Rev. 2015;(6):CD010856. doi:DOI: 10.1002/14651858.CD010856.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Health and Medical Research Council (NHMRC). Public Statement 2017 Water Fluoridation and Human Health in Australia. 2017. [Google Scholar]
- 4.National Research Council (NRC). Fluoride in Drinking Water: A Scientific Review of EPA’s Standards. Washington, DC: National Academies Press; 2006. doi:http://www.nap.edu. [Google Scholar]
- 5.United States Environmental Protection Agency. Fluoride: Relative Source Contribution Analysis. Vol 820-R-10-0; 2010. [Google Scholar]
- 6.Zohoori FV, Omid N, Sanderson RA, Valentine RA, Maguire A. Fluoride retention in infants living in fl uoridated and non- fl uoridated areas : effects of weaning. 2018:1–8. doi: 10.1017/S0007114518003008. [DOI] [PubMed] [Google Scholar]
- 7.Fomon SJ, Ekstrand J, Ziegler EE. Fluoride intake and prevalence of dental fluorosis: trends in fluoride intake with special attention to infants. J Public Health Dent. 2000;60(3):131–139. doi: 10.1111/j.1752-7325.2000.tb03318.x. [DOI] [PubMed] [Google Scholar]
- 8.Ekstrand J No evidence of transfer of fluoride from plasma to breast milk. Br Med J. 1981;283:761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buzalaf MAR., Granjeiro JM., Damante CA. Fluoride content of infant formulas prepared with deionized, bottled mineral and fluoridated drinking water. ASDC J Dent Child. 2001;68(1):10–37. [PubMed] [Google Scholar]
- 10.Van Winkle S, Levy SM, Kiritsy MC, Heilman JR, Wefel JS, Marshall T. Water and formula fluoride concentrations: significance for infants fed formula. Pediatr Dent. 1995;17(4):305–310. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=7567636. [PubMed] [Google Scholar]
- 11.Brothwell D, Limeback H. Breastfeeding is protective against dental fluorosis in a nonfluoridated rural area of Ontario, Canada. J Hum Lact. 2003;19(4):386–390. doi: 10.1177/0890334403257935. [DOI] [PubMed] [Google Scholar]
- 12.Walton JL, Messer LB. Dental caries and fluorosis in breast-fed and bottle-fed children. Caries Res. 1981. 15:124–137. [DOI] [PubMed] [Google Scholar]
- 13.Fv Z, Pj M, Omid N, Abuhaloob L, Impact MA. Impact of water fluoride concentration on the fluoride content of infant foods and drinks requiring preparation with liquids before feeding. 2012;(1):432–440. doi: 10.1111/j.1600-0528.2012.00688.x. [DOI] [PubMed] [Google Scholar]
- 14.Do LG, Levy SM, Spencer AJ. Association between infant formula feeding and dental fluorosis and caries in Australian children. J Public Health Dent. 2012;72(2):112–121. doi: 10.1111/j.1752-7325.2011.00290.x. [DOI] [PubMed] [Google Scholar]
- 15.Hong L, Sm L, Broffitt B, et al. Timing of fluoride intake in relation to development of fluorosis on maxillary central incisors. Community Dent Oral Epidemiol. 2006:299–309. [DOI] [PubMed] [Google Scholar]
- 16.Levy SM, Broffitt B, Marshall TA, Eichenberger-Gilmore JM, Warren JJ. Associations between fluorosis of permanent incisors and fluoride intake from infant formula, other dietary sources and dentifrice during early childhood. J Am Dent Assoc. 2010;141(10):1190–1201. doi: 10.14219/jada.archive.2010.0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hujoel P, Zina L, Moimaz S, Cunha-cruz J. Infant Formula and Enamel Fluorosis: A Systematic Review. JADA. 2009;140(7):841–854. doi: 10.14219/jada.archive.2009.0278. [DOI] [PubMed] [Google Scholar]
- 18.Ekstrand J, Hardell LI SC. Fluoride balance studies on infants in a 1-ppm-water-fluoride area. Caries Res. 1984;18:87–92. [DOI] [PubMed] [Google Scholar]
- 19.Dabeka RW, Karpinski KF, McKenzie AD, Bajdik CD. Survey of lead, cadmium and fluoride in human milk and correlation of levels with environmental and food factors. Food Chem Toxicol. 1986;24(9):913–921. doi: 10.1016/0278-6915(86)90318-2. [DOI] [PubMed] [Google Scholar]
- 20.Esala S; Vuori E; Helle A. Effect of maternal fluorine intake on breast milk fluorine content. Br J Nutr. 1982;48(2):201–204. [DOI] [PubMed] [Google Scholar]
- 21.Faraji H, Mohammadi AA, Akbari-adergani B, Saatloo V, Lashkarboloki G, Mahvi AH. Correlation between Fluoride in Drinking Water and Its Levels in Breast Milk in Golestan Province , Northern Iran. 2014;43(12):1664–1668. [PMC free article] [PubMed] [Google Scholar]
- 22.Critch JCPS. Nutrition for healthy term infants, birth to six months: An overview. Paediatr Child Heal. 2013;18(4):206–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eidelman AISR. Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–e841. [DOI] [PubMed] [Google Scholar]
- 24.Breastfeeding Report Card. United States, 2018. Centers for Disease Control and Prevention. https://www.cdc.gov/breastfeeding/data/reportcard.htm. Published 2018. [Google Scholar]
- 25.Health Canada. Trends in Breastfeeding Practices in Canada (2001 to 2009–2010). http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/prenatal/trends-tendances-eng.php#a2. Accessed February 21, 2016. [Google Scholar]
- 26.Infant Feeding Practices Survey II. Web Table 3.16. Percent of babies who were fed each type of formula in the past 7 days by infant age among formula fed babies. Centers for Disease Control and Prevention. www.cdc.gov/ifps/res. Accessed March 4, 2019. [Google Scholar]
- 27.Rice D, Barone S Jr. Critical periods of vulnerability for the developing nervous system: evidence from humans and animal models. Env Heal Perspect. 2000;108 Suppl:511–533. http://ehpnet1.niehs.nih.gov/members/2000/suppl-3/511-533rice/rice-full.htmlhttp://ehpnet1.niehs.nih.gov/docs/2000/suppl-3/511-533rice/abstract.htmlhttp://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=10852851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grandjean P; Landrigan P Developmental neurotoxicity of industrial chemicals. Lancet. 2006;368(9553):2167–2178. doi: 10.1016/S0140-6736(06)69665-7. [DOI] [PubMed] [Google Scholar]
- 29.Harriehausen CX; Dosani FZ; Chiquet BT; Barratt MS; Quock RL Fluoride Intake of Infants from Formula. 2019;43(1):8–11. doi: 10.17796/1053-4625-43.1.7. [DOI] [PubMed] [Google Scholar]
- 30.Bashash M, Thomas D, Hu H, et al. Prenatal fluoride exposure and cognitive outcomes in children at 4 and 6 – 12 Years of age in Mexico. Enviromental Heal Perspect. 2017;125(9):097017. doi: 10.1289/EHP655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Green R; Lanphear B; Hornung R; Flora D; Martinez-Mier EA; Neufeld R; Ayotte P; Muckle G; Till C Fluoride Exposure during Fetal Development and Intellectual Abilities in a Canadian Birth Cohort. accepted. 2019. [Google Scholar]
- 32.Valdez Jiménez L, López Guzmán OD, Cervantes Flores M, et al. In utero exposure to fluoride and cognitive development delay in infants. Neurotoxicology. 2017;59:65–70. doi: 10.1016/j.neuro.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 33.Karimzade S, Aghaei M, Mahvi AH. Investigation of intelligence quotient in 9–12-year-old children exposed to high- and low-drinking water fluoride in West Azerbaijan Province, Iran. Fluoride. 2014;47(1):9–14. [Google Scholar]
- 34.Dong L; Yao P; Chen W; Li P; Shi X Investigation of dental fluorosis and intelligence levels of children in drinking water-related endemic fluorosis areas of Xi’an. Chinese J Epidemiol. 2018;37(1):45–48. [Google Scholar]
- 35.Zhang S, Zhang X, Liu H, et al. Modifying effect of COMT gene polymorphism and a predictive role for proteomics analysis in children’s intelligence in endemic fluorosis area in Tianjin, China. Toxicol Sci. 2015;144(2):238–245. doi: 10.1093/toxsci/kfu311. [DOI] [PubMed] [Google Scholar]
- 36.Choi AL, Sun G, Zhang Y, Grandjean P. Developmental fluoride neurotoxicity: A systematic review and meta-analysis. Environ Health Perspect. 2012;120(10):1362–1368. doi: 10.1289/ehp.1104912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Malin AJ, Till C. Exposure to fluoridated water and attention deficit hyperactivity disorder prevalence among children and adolescents in the United States: an ecological association. Environ Heal. 2015;14(1):1–10. doi: 10.1186/s12940-015-0003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bashash M, Marchand M, Hu H, et al. Prenatal fluoride exposure and attention deficit hyperactivity disorder (ADHD) symptoms in children at 6–12 years of age in Mexico City. Environ Int. 2018;121:658–666. doi: 10.1016/j.envint.2018.09.017. [DOI] [PubMed] [Google Scholar]
- 39.Riddell J; Malin AJ; Flora D; McCague H; Till C Association of water fluoride and urinary fluoride concentrations with Attention Deficit Hyperactivity Disorder in Canadian Youth. Environ Int. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arbuckle TE, Fraser WD, Fisher M, et al. Cohort profile: The maternal-infant research on environmental chemicals research platform. Paediatr Perinat Epidemiol. 2013;27(4):415–425. doi: 10.1111/ppe.12061. [DOI] [PubMed] [Google Scholar]
- 41.(IOM) I of M. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine; http://www.nap.edu/catalog/5776.html. Published 1997. [Google Scholar]
- 42.Till C; Green R; Grundy J; Hornung R; Neufeld R; Martinez-Mier A; Ayotte P; Muckle G; Lanphear B Community Water Fluoridation and Urinary Fluoride Concentrations in a National Sample of Pregnant Women in Canada. Enviromental Heal Perspect. 2018;126(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carignan CC, Cottingham KL, Jackson BP, Farzan SF, Gandolfi AJ. Research | Children ‘s Health Estimated Exposure to Arsenic in Breastfed and Formula-Fed Infants in a United States Cohort. Enviromental Heal Perspect. 2015;500(5):500–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dewey G, Heinig MJ, Nommsen LA, Lonnerdal B. Maternal versus infant facors related to breast milk intake and residual milk volume: The DARLING Study. Pediatrics. 1991;87(6):829–837. [PubMed] [Google Scholar]
- 45.Buzalaf MAR, Damante CA, Trevizani LMM, Granjeiro JM. Risk of fluorosis associated with infant formulas prepared with bottled water. J Dent Child (Chic). 2004;71(2):110–113. [PubMed] [Google Scholar]
- 46.Martínez-Mier EA, Cury JA, Heilman JR, et al. Development of gold standard ion-selective electrode-based methods for fluoride analysis. Caries Res. 2011;45(1):3–12. doi: 10.1159/000321657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wechsler D Wechsler Preschool and Primary Scale of Intelligence – Third Edition: Canadian. Toronto, ON, Canada, ON, Canada: Pearson Clinical Assessment; 2002. [Google Scholar]
- 48.Caldwell B, Bradley R. Home Observation for Measurement of the Environment (HOME) - Revised Edition. University of Arkansas, Little Rock., Little Rock; 1984. [Google Scholar]
- 49.Kleinbaum DG, Kupper LL, Morgenstern H. Epidemiologic Research: Principles and Quantitative Methods. Lifetime Learning Publications; 1982. [Google Scholar]
- 50.Huttenlocher PR, Dabholkar AS. Regional Differences in Synaptogenesis in Human Cerebral Cortex. J Comp Neurol. 1997;178(May):167–178. [DOI] [PubMed] [Google Scholar]
- 51.Kostovic I The development of cerebral connections during the first 20 e 45 weeks ‘ gestation. Semin Fetal Neonatal Med. 2006;11(6):415–422. doi: 10.1016/j.siny.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 52.Horta BL, Mola CL De, Victora CG. Breastfeeding and intelligence : a systematic review and meta-analysis. Acta Pediatr. 2015;104(467):14–19. doi: 10.1111/apa.13139. [DOI] [PubMed] [Google Scholar]
- 53.Walfisch A, Sermer C, Cressman A, Koren G. Breast milk and cognitive development — the role of confounders : a systematic review. BMJ Open. 2013;3(8):e003259. doi: 10.1136/bmjopen-2013-003259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Berg J, Gerweck C, Hujoel PP, et al. Evidence-based clinical recommendations regarding fluoride intake from reconstituted infant formula and enamel fluorosis. J Am Dent Assoc. 2011;142(1):79–87. doi: 10.14219/jada.archive.2011.0032. [DOI] [PubMed] [Google Scholar]
- 55.Diesendorf M, Diesendorf A. Supression by Medical Journals of a Warning about Overdosing Formula-Fed Infants with Fluoride. Account Res. 1997;5(1979):225–237. doi: 10.1080/08989629708573911. [DOI] [PubMed] [Google Scholar]
- 56.Limeback H A re-examination of the pre-eruptive and post-eruptive mechanism of the anti-caries effects of fluoride: is there any anti-caries benefit from swallowing fluoride? Community Dent Oral Epidemiol. 1999;27(August):62–71. doi: 10.1111/j.1600-0528.1999.tb01993.x. [DOI] [PubMed] [Google Scholar]
- 57.Pizzo G, Piscopo MR, Pizzo I. Community water fluoridation and caries prevention : a critical review. Clin Oral Invest. 2007;11(January 2001):189–193. doi: 10.1007/s00784-007-0111-6. [DOI] [PubMed] [Google Scholar]
- 58.Warren JJ; Levy SM. Current and future role of fluoride in nutrition. Dent Clin North Am. 2003;47(2):225–243. [DOI] [PubMed] [Google Scholar]
- 59.Featherstone J The science and practice of caries prevention. J Am Dent Assoc. 2001;131(7):887–899. doi: 10.14219/jada.archive.2000.0307. [DOI] [PubMed] [Google Scholar]
- 60.European Commission SC on H and ER (SCHER). Critical Review of Any New Evidence on the Hazard Profile, Health Effects, and Human Exposure to Fluoride and the Fluoridating Agents of Drinking Water.; 2011. [Google Scholar]
- 61.American Dental Association. Eruption Charts. https://www.mouthhealthy.org/en/az-topics/e/eruption-charts. [Google Scholar]
- 62.Society CP. The use of fluoride in infants and children. www.cps.ca/en/documents/position/fluoride-use. [Google Scholar]
- 63.American Dental Association. Fluoridation Facts.; 2018. [Google Scholar]
- 64.Division of Oral Health NC for CDP and HP. Community Water Fluoridation. Infant Formula. https://www.cdc.gov/fluoridation/faqs/infant-formula.html. [Google Scholar]
- 65.U.S. Department of Health and Human Services Federal Panel on Community Water Fluoridation. U.S. public health service recommendation for fluoride concentration in drinking water for the prevention of dental caries. Public Health Rep. 2015;130(1):1–14. doi: 10.1177/003335491513000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Association CD. Use of Fluorides in Caries Prevention. www.cda-adc.ca/_files/position_statements/fluoride.pdf. Accessed March 4, 2019. [Google Scholar]
- 67.Ekstrand J; Ehrnebo M Influence of milk products on fluoride bioavailability in man. Eur J Clin Pharmacol. 1979;16:211–215. [DOI] [PubMed] [Google Scholar]
- 68.Dabeka RW; McKenzie AD Lead, cadmium, and fluoride levels in market milk and infant formulas in Canada. J Assoc Off Anal Chem. 1987;70(4):754–757. [PubMed] [Google Scholar]
- 69.Fomon SJ, Ekstrand J, Ziegler EE. Fluoride intake and prevalence of dental fluorosis: trends in fluoride intake with special attention to infants. J Public Health Dent. 2000;60(3):131–139. doi: 10.1111/j.1752-7325.2000.tb03318.x. [DOI] [PubMed] [Google Scholar]
- 70.Mahvi AH, Ghanbarian M, Ghanbarian M, Khosravi A, Ghanbarian M. Determination of fluoride concentration in powdered milk in Iran 2010. 2012:1077–1079. doi: 10.1017/S0007114511003941. [DOI] [PubMed] [Google Scholar]
- 71.Van Winkle S, Levy SM, Kiritsy MC, Heilman JR, Wefel JS, Marshall T. Water and formula fluoride concentrations: significance for infants fed formula. Pediatr Dent. 1995;17(4):305–310. [PubMed] [Google Scholar]
- 72.Mcknight-hanes MC, Leverett DMDDH, Adair SM, Shields MSCP. Fluoride content of infant formulas: Soy-based formulas as a potential factor in dental fluorosis. Pediatr Dent. 1988;10(3):189–194. [PubMed] [Google Scholar]
- 73.Cohen J Statistical Power Analysis for the Behavioral Sciences. Second Edi (Lawrence Erlbaum Associates Inc., ed.). Hillsdale, NJ; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.