Abstract
Background
Degenerative cervical myelopathy (DCM) is a common, chronic neurological condition that severely affects individuals by causing a range of disabling symptoms, frequently at a time around the peak of their careers. Subsequently, individuals with DCM often become dependent on informal care arrangements. The significant economic contribution of informal care and its burden on care providers are becoming increasingly recognized.
Objective
This study aimed to measure the quality of life of DCM informal caregivers and provide preliminary insight into possible contributing factors.
Methods
Carers of individuals with DCM completed a Web-based survey hosted by Myelopathy.org, an international DCM charity. Carer quality of life was assessed in the form of caregiver happiness and 7 dimensions of carer burden using the Care-Related Quality of Life (CarerQol) instrument. The relationships between patient disease severity, patient pain, and carer quality of life were investigated. Differences in carer quality of life were assessed across patient and carer demographic groups, including between UK and US carers.
Results
DCM caregivers experienced substantial burden as a result of their caregiving (mean CarerQol-7D=64.1; 95% CI 58.8-69.5) and low happiness (mean CarerQol-VAS [Visual Analog Scale]=6.3; 95% CI 5.7-6.9). Burden was high and happiness was low in DCM carers when compared with a large, mixed-disease study of adult informal carers where CarerQol-7D was 79.1 and CarerQol-VAS was 7.1. No significant relationship was found between DCM carer quality of life and patient disease severity and pain scores. DCM carer quality of life appeared uniform across all patient and carer demographic groups.
Conclusions
Caring for individuals with DCM is associated with reduced quality of life in the form of significant burden and reduced happiness. Reductions appear greater in DCM than in other diseases investigated. However, no simple relationship was identified between individual patient or carer factors and carer quality of life.
Keywords: spinal cord diseases, spondylosis, spinal osteophytosis, surveys and questionnaires, quality of life, chronic disease
Introduction
Background
Degenerative cervical myelopathy (DCM) is a neurological condition of symptomatic cervical spinal cord compression, secondary to a range of degenerative changes in the cervical spine [1]. The causative pathology includes osteophyte formation, disc herniation and ligament hypertrophy, calcification, and ossification [2].
DCM is the most common spinal cord disorder [2], with evidence from imaging studies estimating prevalence as high as 5% in the over 40s [3]. At present, treatment is limited to surgical decompression, which is able to halt disease progression, but existing damage is often permanent [4,5]. Consequently, most patients retain lifelong disabilities, including reduced quality of life. In fact, a recent study demonstrated that DCM patients have one of the most impaired quality of life scores of all chronic diseases—lower than diabetes, cancer, chronic obstructive pulmonary disease (COPD), and depression according to 36-Item Short Form Heath Survey (SF-36) scores [6].
Informal care refers to care provided by family and friends [7]. Historically, informal care received little attention. However, it is clear that providing informal care brings substantial burdens to informal care providers. One study found a 63% higher mortality risk among carers experiencing strain compared with noncaregiving controls [8], whereas another study reported a significant association between carer depression and the likelihood and amount of time missed at work [9]. Informal carers of patients suffering from a range of chronic conditions, including spinal cord injuries [10], dementia [11], eating disorders [12], and Pompe disease [13], among others, have now been studied. Regardless of the disease, these studies consistently describe increased levels of burden, stress, depression, physical health problems, and a range of psychosocial problems in carers. Moreover, in a national survey of 2000 carers in the United Kingdom, 77% reported health deterioration because of the strain of providing care [14]. Unfortunately, despite these substantial burdens for carers, informal care has a minor influence on health care decisions [7].
Despite this, recent work continues to demonstrate that informal care frequently forms a significant proportion of total care, particularly in chronic conditions [7] such as DCM. For example, in the United Kingdom there are an estimated 6 million informal carers [15], and in the United States, estimates suggest that there may be as many as 66 million informal carers [16]. The total economic contribution of UK carers is estimated at £132 billion per year [17], whereas in the United States the total opportunity costs of informal elder-care amounts to US $522 billion annually [18].
Methods have been developed to measure informal care and facilitate its incorporation into economic evaluations of health care [19]. Available methods are diverse, with a range of different instruments, measurements, and valuation techniques available. Both costs and effects of informal care can be measured with a range of monetary and nonmonetary methods. Nonmonetary methods focus on areas such as health-related quality of life, care-related quality of life, and well-being. Monetary methods include revealed preference-based methods and stated preference methods.
The Care-Related Quality of Life (CarerQol) instrument was designed to measure and value the impact of providing informal care [20]. The instrument consists of 2 parts. The first part, CarerQol-7D, is a subjective burden measure assessing 2 positive and 5 negative dimensions of the impact of providing care (Figure 1). The 2 positive dimensions measure (1) fulfillment from caregiving and (2) support with caregiving. The 5 negative dimensions assess (1) relationship problems, (2) own mental health problems, (3) problems combining care tasks with daily activities, (4) financial problems, and (5) own physical health problems.
Figure 1.
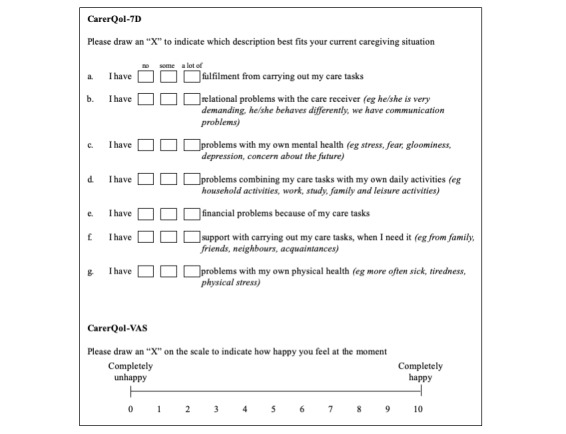
The Care-Related Quality of Life (CarerQoL-7D) instrument assesses carer quality of life in terms of burden and happiness (Visual Analog Scale [VAS]). For the 7D, carers choose from 3 responses to 7 different questions, their overall score aggregating to a total out of 100, with 100 representing the least carer burden. For the VAS, carers rate their happiness on a visual analog scale from 0 to 10, with 10 representing the greatest happiness.
The second part, CarerQol-Visual Analog Scale (VAS), consists of a subjective measure of carer well-being in the form of a general happiness rating on a VAS of 1 to 10. A particular benefit of the CarerQol is that it is generic, allowing for comparison between conditions.
Objectives
Given that DCM causes substantial reductions in the quality of life of patients [6], we hypothesized that there would also be reductions in the quality of life of DCM carers.
The objective was to measure the quality of life of DCM informal carers and provide preliminary insight into possible contributing factors.
Methods
The DCM carer quality of life survey was designed and is reported following the Checklist for Reporting Results of Internet E-Surveys [21].
Survey Design
A cross-sectional observational study was conducted utilizing a Web-based survey targeted at carers of patients with DCM.
The questionnaire included questions to assess the situation of DCM patients and carers. Patient situation questions captured demographics including age, gender, and education; Nurick score (a disease severity classification that utilizes the degree of walking impairment to score the severity of a patient’s cervical myelopathy) [22]; best, worst, and current neck and arm/hand pain scores; and patient dependence on a carer. Carer situation questions captured carer demographics including age, gender, education, employment, country of residence, and length of time as a carer.
Carer quality of life was assessed using the CarerQol instrument [20]. The instrument (Figure 1) comprises 2 parts: a CarerQol-7D and a CarerQol-VAS.
The CarerQol-7D is designed to provide a comprehensive description of the caregiving situation [23]. Each dimension is assessed using a 3-item scale. For example, the respondent rates the statement “I have fulfillment with carrying out my care tasks” by choosing from 3 responses: (1) no, (2) some, or (3) a lot of. The responses for each dimension are weighted with a tariff score. From these, an aggregate score between 0 and 100 can be calculated, with 0 corresponding to the most carer burden (worst informal care situation) and 100 to the least carer burden (best informal care situation). Tariffs for calculating these utility scores were derived using discrete choice experiments among the general population and are population-specific. At the time of study, tariffs were available for the Netherlands [24], Australia, Germany, Sweden, the United Kingdom, and the United States [25].
The CarerQol-VAS consists of a horizontal visual analog scale whereby the carer rates their happiness on a scale of 0 to 10, with 0 representing a situation in which the carer is completely unhappy and 10 representing a situation in which the carer is completely happy [20]. The CarerQol-VAS allows informal care to be considered from an economic perspective. Carer happiness assessed using the CarerQol-VAS is a broad measure, which allows capturing of the influences of the multitude of factors that contribute to carer happiness.
Numerous construct validation studies support the validity of the CarerQol instrument [26-29].
The survey was initially piloted on a small group of carers and found to be satisfactory without need for modification.
Ethics Approval and Informed Consent
The study was ethically approved by the University of Cambridge. All research was performed in accordance with relevant guidelines and regulations.
All carers completed the questionnaire voluntarily and were informed before doing so that their responses would be used anonymously for research purposes. Study objectives were outlined on the initial page, including details of the host organization. This acted as the electronic consent, with continuation into the survey taken as agreement. Respondents were also presented with a description of DCM, including relevant symptoms, and were required to confirm they cared for someone who suffered from this condition
No respondent-identifiable information was stored.
Participants
All DCM carers from countries for which CarerQol tariffs were available at the time of study were included. Carers from countries without available CarerQol tariffs were excluded.
Recruitment
The recruitment strategy has been described previously [30]. An open survey design was employed. Carers of patients with DCM were recruited to an Web-based questionnaire, administered by SurveyMonkey. Social media posts (Facebook and Twitter), supported by Myelopathy.org, were utilized to recruit participants. No contact was made with participants outside the survey.
Administration
The questionnaire was hosted on a designated landing page on Myelopathy.org, a UK registered charity, with a large online, international patient community. The website provides a range of educational materials, support groups, and details of current research studies. The survey was not administered via email. Completion of the survey was voluntary, and no incentives were offered. Responses were collected for 12 months from November 1, 2015. A total of 25 survey items were distributed over 7 survey pages. Only responses that were complete for all carer quality of life domains were included in the final data analysis. A missing data analysis showed complete and incomplete responses were otherwise comparable, providing reassurance that excluding incomplete responses did not introduce additional bias. Respondents were able to click back though and review their answers to previous questions before submission of the survey.
Response Rates
Google Analytics, a Web-based analytics service that enables tracking of visits to a website, was utilized in this study to measure the number of visitors to Myelopathy.org. Survey view rate for total visits to the Myelopathy.org home page was 2.37% (421/17,737), participation rate was 32.3% (136/421), and completion rate was 37.0% (136/368).
Preventing Multiple Entries From the Same Individual
Internet protocol addresses were recorded and used to prevent users submitting multiple responses.
Statistical Methods
Data were checked for the presence of outliers and normality of distribution. First, as CarerQol, Nurick, and pain scores were not monotonically related, Kendall tau-b was utilized to assess for a relationship, using 2-tailed tests. Second, differences in CarerQol-7D and VAS scores between demographic groups were assessed using 1-way analysis of variances (ANOVAs). In 1 case the assumption of homogeneity of variance was violated; a Welch ANOVA was performed to assess for difference in CarerQol-VAS as a function of duration of time as a carer. Third, an independent-samples t test was run to determine if there was a difference in CarerQol-7D score between UK and US carers. Fourth, as CarerQol-VAS violated the assumption of normality, a Mann-Whitney U test was run to determine if there were differences in CarerQol-VAS between UK and US carers. Distributions of UK and US CarerQol-VAS scores were similar, as assessed by visual inspection. Analyses were conducted using SPSS Version 22 (IBM Corp). Significance was set at P<.05. We report mean (SD) unless otherwise specified.
Results
Participants
A total of 136 responses were received (Figure 2). A total of 49 responses were inadvertently completed by DCM patients and were thus excluded. Of the remaining 87 responses, 31 were excluded: 3 were completed by Canadian carers for whom CarerQol tariffs were not available at the time of study, and 28 responses had partial (6) or completely (22) missing CarerQol data. In a missing data analysis, scores for each CarerQol component between the 56 complete and 6 partially incomplete responses were comparable, providing reassurance that excluding the partially incomplete responses was unlikely to introduce bias. Patient and carer characteristics were >95% complete for each variable, permitting meaningful analysis.
Figure 2.
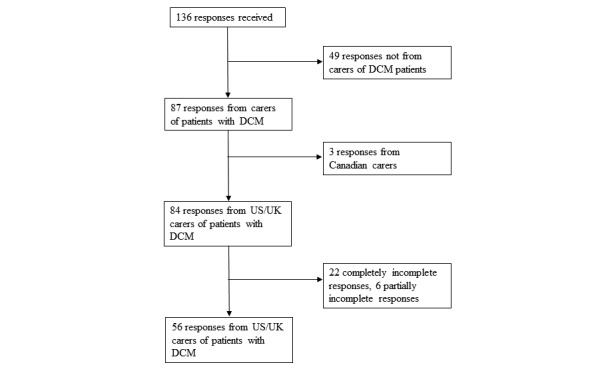
Flowchart of response selection. A total of 136 questionnaire responses were received, 56 of which were included in the final analysis. DCM: degenerative cervical myelopathy.
Patient and Carer Situation
As summarized in Table 1 (n [%]), the majority of carers were female (32/53, 60%), white (51/52, 98%), and from the United Kingdom (45/56, 80%). Duration of time as a carer was varied, ranging from less than 1 year to 25 years. Most (49/54, 91%) carers were over the age of 40 years, and most (31/53, 59%) combined their caring responsibilities with either full-time (21/53, 40%) or part-time (10/53, 19%) work. The majority (19/34, 56%) felt their employment had been affected by the demands of their caregiving.
Table 1.
Patient and carer situation.
| Variable | Patient, n (%) | Carer, n (%) | |
| Gender | n=56 | n=53 | |
|
|
Male | 22 (39) | 21 (40) |
| Country of residence | n=56 | n=56 | |
|
|
United Kingdom | 45 (80) | 45 (80) |
|
|
United States | 11 (20) | 11 (20) |
| Age (years) | n=56 | n=54 | |
|
|
≤17 | 0 (0) | 2 (4) |
|
|
18-20 | 0 (0) | 0 (0) |
|
|
21-29 | 1 (2) | 0 (0) |
|
|
30-39 | 4 (7) | 3 (5) |
|
|
40-49 | 14 (25) | 13 (24) |
|
|
50-59 | 18 (32) | 20 (37) |
|
|
≥60 | 19 (34) | 16 (30) |
| Education | n=56 | n=53 | |
|
|
Less than high school | 14 (25) | 6 (11) |
|
|
High school degree or equivalent | 10 (18) | 14 (26) |
|
|
Some college but no degree | 15 (27) | 14 (26) |
|
|
Associate degree | 5 (9) | 5 (10) |
|
|
Bachelor’s degree | 10 (18) | 4 (8) |
|
|
Graduate degree | 2 (3) | 10 (19) |
| Ethnicity | —a | n=52 | |
|
|
White | — | 51 (98) |
|
|
African American | — | 1 (2) |
| Employment status | — | n=53 | |
|
|
Employed, working full time | — | 21 (40) |
|
|
Employed, working part time | — | 10 (19) |
|
|
Not employed, looking for work | — | 0 (0) |
|
|
Not employed, not looking for work | — | 6 (11) |
|
|
Retired | — | 14 (26) |
|
|
Disabled/unable to work | — | 2 (4) |
| Employment affected by caring | — | 19 (56) | |
| Length of time as carer (years) | — | n=56 | |
|
|
0-1 | — | 13 (23) |
|
|
1-3 | — | 15 (27) |
|
|
3-10 | — | 24 (43) |
|
|
10-25 | — | 4 (7) |
|
|
>25 | — | 0 (0) |
aData were not collected.
Carer Burden and Happiness
Mean carer burden measured by the CarerQol-7D was 64.1 (SD 20.4). Mean carer happiness assessed by the CarerQol-VAS was 6.3 (SD 2.2; Table 2).
Table 2.
Carer burden and happiness scores (n=56).
| Instrument | Mean (SD) | 95% CI | Range |
| Care-Related Quality of Life-7D | 64.1 (20.4) | 58.8-69.5 | 14.6-100 |
| Care-Related Quality of Life-Visual Analog Scale | 6.3 (2.2) | 5.7-6.9 | 1-10 |
The distribution of responses to individual CarerQol-7D dimensions, as a percentage of the overall responses to each dimension, is shown in Figure 3. Most DCM carers (47/56, 84%) experienced at least some (some or a lot of) fulfillment caring. Despite this, most carers experienced at least some mental health problems (43/56, 77%) and at least some physical health problems (41/56, 73%). In addition, around half reported at least some relationship problems with the care receiver (32/56, 57%) and at least some financial problems (28/56, 50%) because of their care responsibilities. Less than half (27/56, 48%) received at least some support with their care tasks, when needed. Most carers (44/56, 79%) experienced problems combining their care tasks with their everyday activities.
Figure 3.

Distribution of responses to Carer-Related Quality of Life (CarerQol)-7D dimensions for degenerative cervical myelopathy carers.
Influence of Carer and Patient Situation
No significant relationship was found between carer burden or happiness and patient disease severity (Nurick score) and pain scores (Multimedia Appendix 1). Moreover, no significant difference in carer burden or happiness was found between different groups for demographic characteristics studied: patient age, gender, education, dependency, carer age, gender, education, employment, and duration of time as a carer (Multimedia Appendix 2).
United States Versus United Kingdom
Mean DCM severity was similar for UK and US patients with Nurick scores of 2.93 (SD 1.03) and 2.91 (SD 0.94), respectively. Mean carer burden score was 58.2 in the United States compared with 65.6 in the United Kingdom (Table 3). Mean carer happiness score was 5.9 in the United States and 6.4 in the United Kingdom. These differences were not statistically significant.
Table 3.
Mean carer burden and happiness lower in US carers.
| Country and instrument | Mean (SD) | 95% CI | Range | |
| United Kingdom (n=45) | ||||
|
|
Care-Related Quality of Life-7D | 65.6 (19.2) | 60.5-70.6 | 22-100 |
|
|
Care-Related Quality of Life-VAS | 6.4 (2.3) | 5.8-7.0 | 1-10 |
| United States (n=11) | ||||
|
|
Care-Related Quality of Life-7D | 58.2 (24.9) | 51.7-64.7 | 14.6-95.5 |
|
|
Care-Related Quality of Life-VAS | 5.9 (1.9) | 5.4-6.4 | 3-9 |
Discussion
Key Findings
These data demonstrate that carer quality of life is markedly reduced in DCM. Most carers reported mental and physical health difficulties, adverse impacts on employment, and strained relationships with the patient. No significant relationships between carer quality of life and patient disease and pain scores were identified. Moreover, no significant difference in carer quality of life was identified between different patient and carer demographic groups.
Interpretation
These findings are significant because informal care plays a fundamentally important role in health care. In the United Kingdom, the value of informal care is estimated to be £132 billion per year [17], whereas according to the Institute for Fiscal Studies, in 2015/16 the UK government spent £140.6 billion on health and £29.9 billion on social care.
Increased strain on carers leads to increased carer illness, creating further demands on health care and negative economic consequences. As an age-related degenerative condition, the incidence and prevalence of DCM is expected to rise. In the context of an ageing population and accelerating health care innovations, health care costs are ever increasing. Therefore, supporting the providers of informal care, to prevent carer burnout and preserve carer health, is essential in ensuring sustainable and financially viable health care systems.
Carer Quality of Life Is Reduced in Degenerative Cervical Myelopathy Compared With Other Chronic Conditions
Considering DCM carer quality of life in context is currently limited by several issues. Comparisons with the general population are limited because the CarerQol instrument questions are specifically targeted at the burden associated with being a carer. In addition, because of the novelty of the CarerQol instrument, few comparable studies currently exist. Unfortunately, the total CarerQol-7D score is often not reported. Nonetheless, several comparisons can be made as follows:
A large study of 1244 adult carers in the Netherlands reported a mean CarerQol-7D score of 79.1 and a mean CarerQol-VAS of 7.1 [26]. The mean CarerQol-7D of 64.1 and CarerQol-VAS of 6.3 detected in this study suggests higher carer burden and lower happiness in DCM carers compared with carers in general.
Similarly, CarerQol-VAS scores indicated that mean happiness in carers of individuals with DCM was lower than those observed in carers of individuals suffering from other conditions. Reported scores were 7.5 in head and neck cancers [31], 7.4 in autism [29], 7.5 in craniofacial malformations [32], and 7.2 in Pompe disease [13]. Therefore, DCM may pose heavier burden on carers than other reported diseases.
Using a similar 0 to 10 scale as in the CarerQol-VAS, the average population happiness has been estimated at 7.1 for the United Kingdom, 7.3 for the United States, 7.6 for the Netherlands, and 7.5 for Ireland [33]. The reduction of happiness in carers of individuals with DCM is large compared with the average happiness of the study population country (12.5%) and compared with carers of people with Pompe disease (5.3%), craniofacial malformations (2.7%), and autism (1.4%).
Although these comparisons are not without limitation, including lack of formal statistical comparison, carer quality of life scores appear consistently lower in DCM than reported in other diseases and general population estimates, suggesting that quality of life may be particularly affected in DCM carers. Exactly why carers are more affected in DCM remains unclear.
In this study we did not identify any associated factors. This may have been masked by our sample size, as studies involving larger groups (eg, n=200), albeit using alternative quality of life instruments, have found that carer demographics such as age, gender, health status, and duration of caregiving influence carer quality of life [34]. However, the absence of any trends between our investigated factors and carer quality of life may suggest that instead, significant factors were not considered. For example, other studies have shown a link with increasing hours of required care and the patient’s quality of life [13].
Recent research indicates that patient quality of life in DCM is lower than many other severe chronic conditions, including diabetes, cancers, and COPD [6]. In addition, DCM patients have a high prevalence of affective disorders [35], which may provide a possible explanation for the high carer burden and warrants further investigation.
Generalizability
As CarerQol tariffs become available for several other countries [25], more nationalities should be included in future work. The comparison of diverse cultures and health care systems may provide novel insight into factors influencing carer quality of life. For example, it would be interesting to compare carer quality of life across cultures that place differing care expectations upon the family of those who are ill and between countries with more and less developed health and social care systems. This would help elucidate whether it is personal or wider societal factors that are most influential on carer quality of life.
Limitations and Future Directions
Internet recruitment to patient-specific health surveys can be effective and reach an international audience efficiently and inexpensively, with less missing data compared with postal questionnaires [36,37].
Despite promising and comparable completion rates, the number of carers recruited was lower than patients in a DCM patient study using the same recruitment methods. Given the levels of disability in DCM, having fewer carers than patients is unlikely. It is more likely the internet recruitment methods were more effective for patients than carers, perhaps with patients more likely to identify with their condition (DCM) than carers with their situation (caring for someone with DCM). Given the limited experience of internet recruitment and behavior among carers, we can only speculate at this time. However, to support further research in this field, this deserves further consideration.
Inclusion of only 56 of the 136 responses received in the final analysis was disappointing. In total, 64% (56/87) of all responses from carers were included. A large proportion of excluded responses were inadvertently completed by patients, which is understandable given that at present most Myelopathy.org website visitors are patients. Nonetheless, finding no substantial differences between complete and incomplete responses makes selection bias unlikely. Moreover, the exclusion of carers from countries for which CarerQol tariffs were not available will resolve as more tariffs become available. Plans for development of a designated carer section of Myelopathy.org may improve carer participation in future work.
The participation rate of 32% in this study was lower than the typical response rate of 50% to 70% in other CarerQol studies [29,31,32]. These studies utilized postal questionnaires rather than open electronic questionnaires, as utilized in this study. Although response and participation rates are not identical measures, the participation rate in this study is almost certainly a substantial underestimate because it was not possible to distinguish between patient and carer website visitors, meaning that a large number of patient visitors were included in the denominator of our participation rate calculation.
Finally, patient and carer factors considered in this study were not found to influence carer quality of life. Although it is possible any associations may have been concealed by the sample size, considering other factors including the number of hours spent caring per week and further assessing the emotional and psychological burden for patient and carer will form important future work [13,35,38]. The identification of such factors is important to target supportive interventions.
Conclusions
DCM carer quality of life is low. The magnitude of reduction in DCM carer quality of life appears greater than reductions in carer quality of life in other conditions studied. In this study, no single patient or carer factors were associated with carer quality of life. Identification of influencing factors is important to better understand the basis for impaired quality of life and to target support, which should form the basis of future work.
Acknowledgments
This report is independent research arising from a Clinician Scientist Award, CS-2015-15-023, supported by the National Institute for Health Research (NIHR). The views expressed in this publication are those of the authors and not necessarily those of the National Health Service, the NIHR, or the Department of Health and Social Care.
Research in the MRK’s laboratory is supported by a core support grant from the Wellcome Trust and Medical Research Council to the Wellcome Trust-Medical Research Council Cambridge Stem Cell Institute. MRK is supported by an NIHR Clinician Scientist Award.
Abbreviations
- ANOVA
analysis of variance
- CarerQol
Care-Related Quality of Life
- COPD
chronic obstructive pulmonary disease
- DCM
degenerative cervical myelopathy
- NIHR
National Institute for Health Research
- VAS
Visual Analog Scale
Kendall tau-b correlations between carer burden and happiness and patient disease severity and pain scores.
No significant difference in carer happiness was identified between the different groups of 9 demographic characteristics using 1-way analysis of variances.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Davies BM, Mowforth OD, Smith EK, Kotter MR. Degenerative cervical myelopathy. Br Med J. 2018 Feb 22;360:k186. doi: 10.1136/bmj.k186. http://www.bmj.com/cgi/pmidlookup?view=long&pmid=29472200 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine (Phila Pa 1976) 2015 Jun 15;40(12):E675–93. doi: 10.1097/BRS.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 3.Kovalova I, Kerkovsky M, Kadanka Z, Kadanka Z, Nemec M, Jurova B, Dusek L, Jarkovsky J, Bednarik J. Prevalence and imaging characteristics of nonmyelopathic and myelopathic spondylotic cervical cord compression. Spine (Phila Pa 1976) 2016 Dec 15;41(24):1908–16. doi: 10.1097/BRS.0000000000001842. [DOI] [PubMed] [Google Scholar]
- 4.Fehlings MG, Wilson JR, Kopjar B, Yoon ST, Arnold PM, Massicotte EM, Vaccaro AR, Brodke DS, Shaffrey CI, Smith JS, Woodard EJ, Banco RJ, Chapman JR, Janssen ME, Bono CM, Sasso RC, Dekutoski MB, Gokaslan ZL. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: results of the AOSpine North America prospective multi-center study. J Bone Joint Surg Am. 2013 Sep 18;95(18):1651–8. doi: 10.2106/JBJS.L.00589.1734760 [DOI] [PubMed] [Google Scholar]
- 5.Fehlings MG, Ibrahim A, Tetreault L, Albanese V, Alvarado M, Arnold P, Barbagallo G, Bartels R, Bolger C, Defino H, Kale S, Massicotte E, Moraes O, Scerrati M, Tan G, Tanaka M, Toyone T, Yukawa Y, Zhou Q, Zileli M, Kopjar B. A global perspective on the outcomes of surgical decompression in patients with cervical spondylotic myelopathy: results from the prospective multicenter AOSpine international study on 479 patients. Spine (Phila Pa 1976) 2015 Sep 1;40(17):1322–8. doi: 10.1097/BRS.0000000000000988. [DOI] [PubMed] [Google Scholar]
- 6.Oh T, Lafage R, Lafage V, Protopsaltis T, Challier V, Shaffrey C, Kim HJ, Arnold P, Chapman J, Schwab F, Massicotte E, Yoon T, Bess S, Fehlings M, Smith J, Ames C. Comparing quality of life in cervical spondylotic myelopathy with other chronic debilitating diseases using the short form survey 36-health survey. World Neurosurg. 2017 Oct;106:699–706. doi: 10.1016/j.wneu.2016.12.124.S1878-8750(16)31439-5 [DOI] [PubMed] [Google Scholar]
- 7.van Exel J, Bobinac A, Koopmanschap M, Brouwer W. The invisible hands made visible: recognizing the value of informal care in healthcare decision-making. Expert Rev Pharmacoecon Outcomes Res. 2008 Dec;8(6):557–61. doi: 10.1586/14737167.8.6.557. [DOI] [PubMed] [Google Scholar]
- 8.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the caregiver health effects study. J Am Med Assoc. 1999 Dec 15;282(23):2215–9. doi: 10.1001/jama.282.23.2215.joc91040 [DOI] [PubMed] [Google Scholar]
- 9.Wilson MR, Houtven CH, Stearns SC, Clipp EC. Depression and missed work among informal caregivers of older individuals with dementia. J Fam Econ Iss. 2007 Aug 24;28(4):684–98. doi: 10.1007/s10834-007-9081-8. [DOI] [Google Scholar]
- 10.Post MW, Bloemen J, de Witte LP. Burden of support for partners of persons with spinal cord injuries. Spinal Cord. 2005 May;43(5):311–9. doi: 10.1038/sj.sc.3101704.3101704 [DOI] [PubMed] [Google Scholar]
- 11.van Vliet D, de Vugt ME, Bakker C, Koopmans RT, Verhey FR. Impact of early onset dementia on caregivers: a review. Int J Geriatr Psychiatry. 2010 Nov;25(11):1091–100. doi: 10.1002/gps.2439. [DOI] [PubMed] [Google Scholar]
- 12.Martín J, Padierna A, Aguirre U, González N, Muñoz P, Quintana JM. Predictors of quality of life and caregiver burden among maternal and paternal caregivers of patients with eating disorders. Psychiatry Res. 2013 Dec 30;210(3):1107–15. doi: 10.1016/j.psychres.2013.07.039.S0165-1781(13)00439-3 [DOI] [PubMed] [Google Scholar]
- 13.Kanters TA, van der Ploeg AT, Brouwer WB, Hakkaart L. The impact of informal care for patients with Pompe disease: an application of the CarerQol instrument. Mol Genet Metab. 2013 Nov;110(3):281–6. doi: 10.1016/j.ymgme.2013.07.020.S1096-7192(13)00268-0 [DOI] [PubMed] [Google Scholar]
- 14.Carers UK. 2008. [2018-06-21]. Carers Can't Afford to Be Ill https://www.carersuk.org/news-and-campaigns/news/carers-cant-afford-to-be-ill .
- 15.National Audit Office . Supporting Carers to Care: Report by the Comptroller and Auditor General, Session 2008-2009. London: Stationery Office Books; 2009. [Google Scholar]
- 16.Schulz R, Tompkins CA. National Center for Biotechnology Information. 2010. [2019-06-03]. Informal Caregivers in the United States: Prevalence, Caregiver Characteristics, and Ability to Provide Care https://www.ncbi.nlm.nih.gov/books/NBK210048 .
- 17.Buckner L, Yeandle S. The University of Sheffield. 2015. [2018-06-21]. Valuing Carers 2015 - The Rising Value of Carers Support https://www.sheffield.ac.uk/polopoly_fs/1.546409!/file/Valuing-Carers-2015.pdf .
- 18.Chari AV, Engberg J, Ray KN, Mehrotra A. The opportunity costs of informal elder-care in the United States: new estimates from the American time use survey. Health Serv Res. 2015 Jun;50(3):871–82. doi: 10.1111/1475-6773.12238. http://europepmc.org/abstract/MED/25294306 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoefman RJ, van Exel J, Brouwer W. How to include informal care in economic evaluations. Pharmacoeconomics. 2013 Dec;31(12):1105–19. doi: 10.1007/s40273-013-0104-z. [DOI] [PubMed] [Google Scholar]
- 20.Brouwer WB, van Exel NJ, van Gorp B, Redekop WK. The CarerQol instrument: a new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Qual Life Res. 2006 Aug;15(6):1005–21. doi: 10.1007/s11136-005-5994-6. [DOI] [PubMed] [Google Scholar]
- 21.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet e-surveys (CHERRIES) J Med Internet Res. 2004 Sep 29;6(3):e34. doi: 10.2196/jmir.6.3.e34. https://www.jmir.org/2004/3/e34/ v6e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nurick S. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95(1):87–100. doi: 10.1093/brain/95.1.87. [DOI] [PubMed] [Google Scholar]
- 23.Hoefman R, van Exel NJ, Brouwer WB. Institute for Medical Technology Assessment. 2011. [2018-06-21]. iVICQ: iMTA Valuation of Informal Care Questionnaire https://www.imta.nl/assets/uploads/2018/01/iVICQ_UK_version_1.1.pdf .
- 24.Hoefman RJ, van Exel J, Rose JM, van de Wetering EJ, Brouwer WB. A discrete choice experiment to obtain a tariff for valuing informal care situations measured with the CarerQol instrument. Med Decis Making. 2014 Jan;34(1):84–96. doi: 10.1177/0272989X13492013.0272989X13492013 [DOI] [PubMed] [Google Scholar]
- 25.Hoefman RJ, van Exel J, Brouwer WB. Measuring care-related quality of life of caregivers for use in economic evaluations: CarerQol tariffs for Australia, Germany, Sweden, UK, and US. Pharmacoeconomics. 2017 Apr;35(4):469–78. doi: 10.1007/s40273-016-0477-x. http://europepmc.org/abstract/MED/28039617 .10.1007/s40273-016-0477-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoefman RJ, van Exel J, Brouwer WB. Measuring the impact of caregiving on informal carers: a construct validation study of the CarerQol instrument. Health Qual Life Outcomes. 2013 Oct 21;11:173. doi: 10.1186/1477-7525-11-173. https://hqlo.biomedcentral.com/articles/10.1186/1477-7525-11-173 .1477-7525-11-173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoefman R, Al-Janabi H, McCaffrey N, Currow D, Ratcliffe J. Measuring caregiver outcomes in palliative care: a construct validation study of two instruments for use in economic evaluations. Qual Life Res. 2015 May;24(5):1255–73. doi: 10.1007/s11136-014-0848-8. [DOI] [PubMed] [Google Scholar]
- 28.Lutomski JE, van Exel NJ, Kempen GI, van Charante EP, den Elzen WP, Jansen AP, Krabbe PF, Steunenberg B, Steyerberg EW, Rikkert MG, Melis RJ. Validation of the care-related quality of life instrument in different study settings: findings from the older persons and informal caregivers survey minimum dataset (topics-MDS) Qual Life Res. 2015 May;24(5):1281–93. doi: 10.1007/s11136-014-0841-2. [DOI] [PubMed] [Google Scholar]
- 29.Hoefman R, Payakachat N, van Exel J, Kuhlthau K, Kovacs E, Pyne J, Tilford JM. Caring for a child with autism spectrum disorder and parents' quality of life: application of the CarerQol. J Autism Dev Disord. 2014 Aug;44(8):1933–45. doi: 10.1007/s10803-014-2066-1. http://europepmc.org/abstract/MED/24577786 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davies B, Kotter MR. Lessons from recruitment to an internet-based survey for degenerative cervical myelopathy: comparison of free and fee-based methods. JMIR Res Protoc. 2018 Feb 5;7(2):e18. doi: 10.2196/resprot.6567. https://www.researchprotocols.org/2018/2/e18/ v7i2e18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hanly P, Maguire R, Balfe M, Hyland P, Timmons A, O'Sullivan E, Butow P, Sharp L. Burden and happiness in head and neck cancer carers: the role of supportive care needs. Support Care Cancer. 2016 Oct;24(10):4283–91. doi: 10.1007/s00520-016-3261-8.10.1007/s00520-016-3261-8 [DOI] [PubMed] [Google Scholar]
- 32.Payakachat N, Tilford JM, Brouwer WB, van Exel NJ, Grosse SD. Measuring health and well-being effects in family caregivers of children with craniofacial malformations. Qual Life Res. 2011 Nov;20(9):1487–95. doi: 10.1007/s11136-011-9870-2. [DOI] [PubMed] [Google Scholar]
- 33.Veenhooven R. World Database of Happiness. 2018. [2018-06-21]. Happiness in Nations http://worlddatabaseofhappiness.eur.nl/hap_nat/nat_fp.php?mode=1,
- 34.Morley D, Dummett S, Peters M, Kelly L, Hewitson P, Dawson J, Fitzpatrick R, Jenkinson C. Factors influencing quality of life in caregivers of people with Parkinson's disease and implications for clinical guidelines. Parkinsons Dis. 2012;2012:190901. doi: 10.1155/2012/190901. doi: 10.1155/2012/190901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stoffman MR, Roberts MS, King JT. Cervical spondylotic myelopathy, depression, and anxiety: a cohort analysis of 89 patients. Neurosurgery. 2005 Aug;57(2):307–13. doi: 10.1227/01.neu.0000166664.19662.43.00006123-200508000-00018 [DOI] [PubMed] [Google Scholar]
- 36.Zuidgeest M, Hendriks M, Koopman L, Spreeuwenberg P, Rademakers J. A comparison of a postal survey and mixed-mode survey using a questionnaire on patients' experiences with breast care. J Med Internet Res. 2011 Sep 27;13(3):e68. doi: 10.2196/jmir.1241. https://www.jmir.org/2011/3/e68/ v13i3e68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Callas PW, Solomon LJ, Hughes JR, Livingston AE. The influence of response mode on study results: offering cigarette smokers a choice of postal or online completion of a survey. J Med Internet Res. 2010 Oct 21;12(4):e46. doi: 10.2196/jmir.1414. https://www.jmir.org/2010/4/e46/ v12i4e46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Janda M, Neale RE, Klein K, O'Connell DL, Gooden H, Goldstein D, Merrett ND, Wyld DK, Rowlands IJ, Beesley VL. Anxiety, depression and quality of life in people with pancreatic cancer and their carers. Pancreatology. 2017;17(2):321–7. doi: 10.1016/j.pan.2017.01.008.S1424-3903(17)30020-0 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Kendall tau-b correlations between carer burden and happiness and patient disease severity and pain scores.
No significant difference in carer happiness was identified between the different groups of 9 demographic characteristics using 1-way analysis of variances.


