Food bolus impaction of the oesophagus (food bolus obstruction (FBO)), is a common gastroenterological emergency and has been increasingly recognised as a complication of eosinophilic oesophagitis (EoE).1 2 The initial management of FBO is to safely expedite relief of obstruction in order to prevent aspiration of gastric contents and oesophageal perforation and, second, to consider the underlying cause in order to inform future management.3 4 It is in this latter case where clinical practice is most divergent, and where consensus and future guidelines are also needed. Failure to identify and then to commence appropriate treatment of EoE not only may lead to recurrent FBO but also may increase the risk of a fibrostenosing form of EoE.2 4
The article by Ntuli et al published in this journal5 emphasises the variability of the clinical management of FBO and discusses the significant divergence from ‘ideal’ practice among various craft groups. With resolution of FBO, consideration of the underlying aetiology should inform commencement of treatment. In the era of increased EoE recognition, biopsies have been advocated at the time of food bolus removal.3 Of concern, excluding all repeat presentations and considering all patients at first presentation, is that some 276 individuals presented with FBO, yet only 25 (9.1%) were diagnosed with EoE; 4 (1.4%) had a known diagnosis of EoE, with a novel diagnosis of EoE made in 21 (7.6%) subjects.2 5 Given that EoE is now recognised as a major and common cause of FBO,6 it is likely that many cases were missed in this cohort of patients presenting with FBO. Specifically, nearly one-third (35%) of presentations were managed without an upper gastrointestinal endoscopy (OGD), and only 40% of those who underwent OGD had oesophageal biopsies taken, likely missing cases of EoE.
The methodology used by Ntuli et al has some limitations, most importantly being that data are retrospective, and management practices are variable, thus rendering estimation of disease frequency invalid. Nonetheless, this study adds to a significant body of contemporary data, likewise acquired retrospectively (audit), that tells a similar story and speaks to a need for coordinated action. Hiremath et al, in a survey of clinical practice, demonstrated significant variation in the approach to FBO among paediatric and adult gastroenterologists, where it was estimated that of the 69 150 adult and 4030 paediatric patients presenting to emergency departments with FBO annually in the USA, some 13 766 (20%) adult and 96 (2.5%) paediatric cases of EoE-attributable FBO could be missed per year as a resultant of management that is divergent from best practice (eg, that did not include endoscopy and biopsy).7
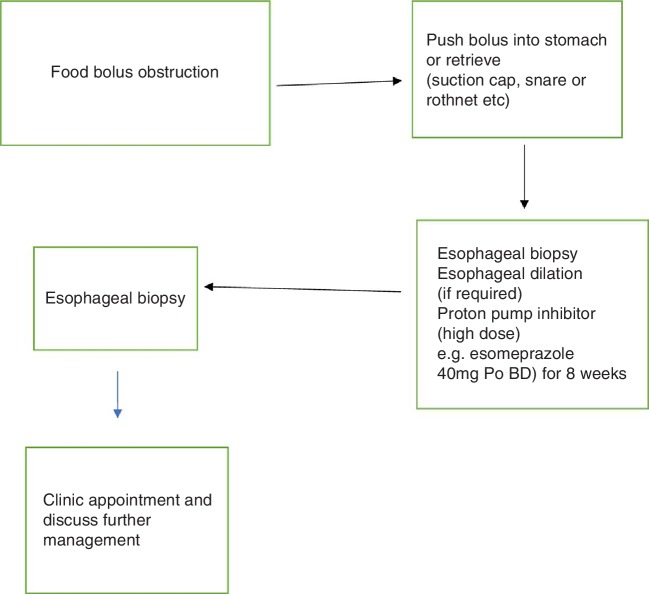
Ntuli et al quite reasonably, therefore, advocate for a formal FBO protocol that involves management by a single craft group (preferably gastroenterology), including flexible OGD and multiple oesophageal biopsies, ensuring that EoE is diagnosed and systematic follow-up in an outpatient clinic is arranged. Indeed, one could go further in suggesting that the technique of food bolus removal be standardised also, in line with recent guidelines. This may involve initial gentle attempts to ‘push’ the bolus in to the stomach, which should be abandoned in favour of bolus retrieval using a suction cap or a polyp snare if resistance to passage is encountered (see figure 1). Routine oesophageal biopsies from the proximal and distal oesophagus during initial assessment of FBO and attempting rebiopsies from the oesophagus during surveillance EGD after treatment should be advocated. A protocol that encompasses management of patients from admission to endoscopy, to treatment and outpatient follow-up is required. Such a protocol, perhaps made universal by formalised guidelines, should in future prevent unnecessary recurrent FBO events, which are uncomfortable and dangerous for the patient and costly to the healthcare system at large.
Figure 1.
Proposed ideal management of food bolus obstruction secondary to eosinophilic oesophagitis.
Footnotes
Contributors: Both authors contributed to the writing of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1. Sperry SLW, Crockett SD, Miller CB, et al. Esophageal foreign-body impactions: epidemiology, time trends, and the impact of the increasing prevalence of eosinophilic esophagitis. Gastrointest Endosc 2011;74:985–91. 10.1016/j.gie.2011.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Philpott HL, Nandurkar S, Thien F, et al. Seasonal recurrence of food bolus obstruction in eosinophilic esophagitis. Intern Med J 2015;45:939–43. 10.1111/imj.12790 [DOI] [PubMed] [Google Scholar]
- 3. ASoP C, Ikenberry SO, Jue TL, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc 2011;73:1085–91. [DOI] [PubMed] [Google Scholar]
- 4. Runge TM, Eluri S, Cotton CC, et al. Causes and outcomes of esophageal perforation in eosinophilic esophagitis. J Clin Gastroenterol 2016;111:206–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ntuli Y, Bough I, Wilson M. Recognising eosinophilic oesophagitis as a cause of food bolus obstruction. Frontline Gastroenterol 2019;11:11–15. 10.1136/flgastro-2019-101176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Heerasing N, Lee SY, Alexander S. Prevalence of eosinophilic oesophagitis in adults presenting with oesophageal food bolus obstruction. World J Gastrointest Pharmacol Ther 2015;6:244–7. 10.4292/wjgpt.v6.i4.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hiremath G, Vaezi MF, Gupta SK, et al. Management of esophageal food impaction varies among Gastroenterologists and affects identification of eosinophilic esophagitis. Dig Dis Sci 2018;63:1428–37. 10.1007/s10620-018-4972-0 [DOI] [PMC free article] [PubMed] [Google Scholar]