Abstract
Purpose
Interest in mobile health applications (apps) for diabetes self-care is growing. Mobile health is a promising new treatment modality for diabetes, though few smartphone apps have been designed based on a proper study and prioritization. The aim of this study was to determine a minimum set of features for diabetes mobile apps.
Methods
This study was conducted in three steps: 1.A review of the literature to collect all available features, 2. Assessing the validity of suggested features by Content Validity Index (CVI) and Content Validity Ratio (CVR), 3. Examining the importance of features by Friedman test.
Results
We retrieved all features of available mobile apps for type 2 diabetes, which are suggested and discussed in literature and compiled as a single list comprising of 33 features. Then, a survey of expert’s opinion produced a set of 23 final minimum features which includes all types of tracking, mealtime tagging, food database, diet management, educational materials, healthy coping, reducing risks, problem solving, Email, color coding, alerts, reminder, target range setting, trend chart view, logbook view, numerical indicators view, customizable theme, preset notes, and custom notes. According to the mean rank which indicates the priority of each feature, the most important one was blood glucose tracking (with 16.71 mean rank) and the least important feature was the numerical indicators like such as standard deviation or average (with 6.50 mean rank).
Conclusions
The present study is the first step towards the development of our mobile apps for people with type II diabetes, and highest the essential features that are required for an optimal self-care comprehensively.
Keywords: Mobile health, mHealth, Smartphone apps, Type 2 diabetes, Features
Introduction
Diabetes is one of the major concerns in healthcare. Diabetes could be a cause of many disabling complications such as cardiovascular disease, kidney failure, blindness, and amputation. It also affects the quality of life and the ability of the patients to manage their life during the course of the illness [1]. Since 1980, the number of adults with diabetes has quadrupled. More than 400 million people worldwide are diagnosed with diabetes, and these growing numbers tend to rise to more than 600 million by 2040 [2]. However, less than half of those people receive standard care [3]. Almost 90% of these cases make up Diabetes type 2 (T2DM) which is defined as insufficient insulin secretion or resistance to it [4]. Although diabetes type 2 patients play important role to control the progression of their disorder [5], there is growing concern whether traditional methods for monitoring the patient’s self-care activities cover health care needs effectively. Therefore, modern methods are recommended. Also, the World Health Organization (WHO) emphasizes that no adequate coverage of global health without the support of electronically based interventions can be obtained [6]. mHealth is a subset of all types of electronic interventions in healthcare that refers to the use of smart phones for health care services [7]. It is also known as mobile health refers to the use of mobile computational technologies such as mobile phone in patient care that go beyond the traditional patient-physician communication [8].
Based on the data that patients import into mobile-based applications known as apps (whether manually or automatically, such as logging in via Bluetooth), these apps can provide appropriate feedback. These apps can enhance self-care skills through ease of communication with the healthcare providers and provide immediate monitoring and educational messages. It is proven that mobile apps may make clinical efficiency for T2DM control [9].
Here are some of the other advantages of this method, which increases the tendency to use it: (1) The ability to be present all over the place, (2) high scalability for provided services, (3) low cost and convenient for use by the end user, (4) usable in deprived and low-income areas, (5) provide two-way, close and comfortable patient and provider communication, and (6) can be personalized for patient’s self-care. Mobile phones are now used as a supporter of health care services because they are widely available and relatively affordable. Researchers and healthcare providers have introduced this tool with ubiquitous nature, as a guide to help patients [7].
Because of these benefits, statistics show 44 million health apps downloaded in 2012 exceeded to 142 million downloads by 2016. Many of these apps are dedicated to manage chronic and costly diseases like T2DM [10]. Therefore, there are numerous mobile apps with various features for managing T2DM. The understanding of the use of mobile health apps is growing too, while the creation and completion of the apps are developing [11]. However, to utilize available opportunities for these apps, several necessary considerations are required [12]. Self-care improvement approaches are effective if mobile apps are designed according to the patient’s status and complex condition. They need to consider a lot of necessary requirements for diabetes patients care such as continuous monitoring of blood glucose, physical activity, blood pressure, and medication simultaneously [13]. Unfortunately, such fertile opportunity is sometimes limited only to focus on using text messages [12]. or sometimes, patients are bewildered to use complicated diabetes mobile apps. Therefore selecting the appropriate one with adequate features, for satisfying the needs is so critical [14]. Many of these apps are designed without considering any scientific base and user requirement. Truly, many of the researchers offer a list of features merely considering expert’s opinions [15–18]. That is, many apps help patients to guide, implement, and control their own self-care behaviors, still, there is a need to provide the desired template for diabetes patients self-care mobile apps [19]. The present study attempts to point out the minimum features as a base which is required for T2DM self-care apps based on previous research results and expert’s point of view.
Methods
This study aims to offer a set of features for mobile apps designed for T2DM self-care. We used a mixed descriptive analytic method in which questionnaire tool was used to cover this objective. This research has been conducted following three steps.
The first step, the totality of available and suggested features were reviewed in the literature related to mobile based diabetes type II self-care. The articles in the databases of Web of Knowledge, Google Scholar, PubMed, Scopus, and Science Direct were retrieved using the keywords of “diabetes”, “glucose”, “blood sugar”, “insulin”, “mobile health”, “mobile apps”,” smartphone”, “mobile phone” and “mHealth”. All non-English articles were excluded. All articles older than 2012 were discarded. Articles that specifically did not deal with diabetes self-care straightly and were limited to topics such as physical activity, diet, or medication adherence, were removed in this step. Also, articles that did not directly mention the use of mobile devices in the field of T2DM self-care were also eliminated. We searched guidelines and standards related to self-care diabetes specially based on mobile apps too After that, all suggested features from remained studies were extracted. Then the duplicated features were removed. We tried to provide correct and uniform definition for each feature in order to make accurate understanding. Some features have well and complete definition, so we extracted that definitions from the literature; however, the definitions of some others have not any definitions or were vague, and we tried to provide acceptable definitions based on reviewed literature [20–25] and expert opinions.
In the second step, the validity of extracted features was analyzed. For this task, we examine both relevancy and necessity of features. We requested from six members of the interdisciplinary expert team including Iranian Board of Health Informatics, Health Information Management, Adult Endocrinologist, Health Education, and Promotion to comment to approve the most necessary and relevant features. Thus, for this purpose, the content validity ration (CVR) and content validity index (CVI) scales was calculated. The CVR is a useful statistical technique to determine the validity of individual questionnaire items related to necessity, as rated by a panel of content experts. The CVI provides a numeric value for the overall mean CVRs and related to relevancy of all items included in the questionnaire. To determine CVR scale, we used the formula shown in follow. According to Lawshe’s table [26], if CVR’s feature is higher than 0.99, that feature is accepted. The relevancy of the suggested features were examined based the predefined score of Lynn’s table, those items would be accepted that have at a level higher than 0.79 among these six experts [27]. We collected the views of experts proposed on the four-part of Likert for the CVI includes non-relevant, to some extent relevant and relevant calculated. Also, three parts of Likert for CVR include “necessary”, “useful but not necessary”, and “not necessary”. After calculating the CVR and CVI, some features were revised to be kept or deleted. Afterward, we made a questionnaire by verified features, in order to determine the final features list and analyses the level of importance of them, a Likert questionnaire was made to considered the five-part of scales from “totally agree” (highest score), “almost agree”, “indifferent”, “agree” and “not agree” (least score). The list of names and email addresses of specialists in various areas include Health Informatics, Health Information Management, Adult Endocrinologist, Health Education, and Promotion was collected separately from the website of the Ministry of Health Scientometrics and Publications. The requirements for faculty members to complete the questionnaire at all universities across the country were a higher academic degree, a minimum of 5 years’ experience and research experience in diabetes. Taking these criteria, we requested 34 specialists to comment suggested features; and 21 of them responded.
In third step, we used Friedman test to sort features importance with mean rank measure (P value <0.05). Non parametric Friedman test was used to sort out features in term of their importance based on their scores. we used this test, which is equivalent to analysis of variance to compare the mean of ratings among features. The Friedman test is used for one-way repeated measures analysis of variance by ranks. This measurement used when at least data in the ordinary scale. This test was exploited in SPSS 22.0.
Results
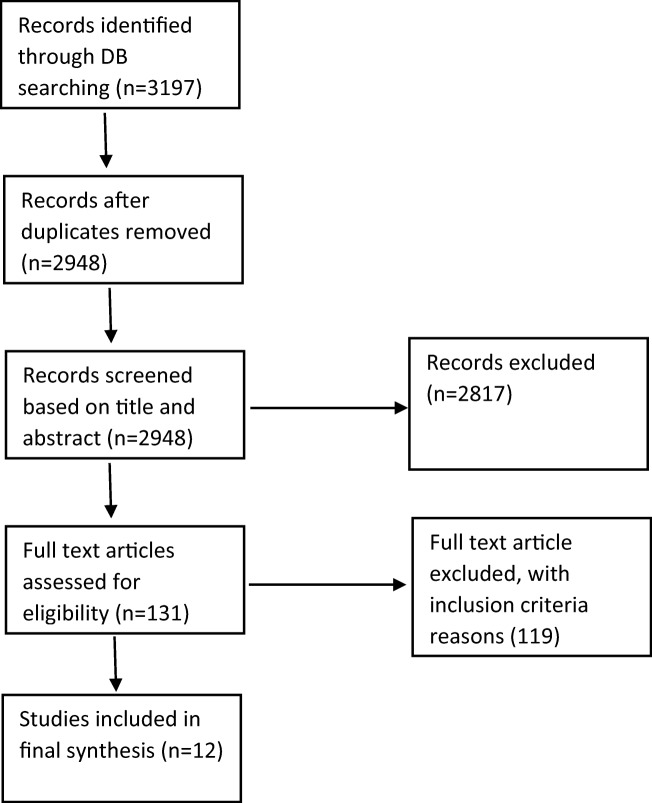
With respect to each step of the procedure, the results are reported. For the first step, the search process from online journal databases illustrated in Fig. 1 was done. Based on our inclusion and exclusion criteria, 12 relevant papers remained.
Fig. 1.
PRISMA flow diagram of selection process for papers
We needed to have a clear definition that experts would be able to grasp the function of each feature in a straightforward manner and that the same impression would occur. Some features were well-defined and we extracted their definitions from the literature [18, 22, 25]; however, the definition of some others was vague; therefore, we tried to provide acceptable definitions based on reviewed papers. The identified features from the first step and their definitions are listed in Table 1.
Table 1.
Features list of diabetes mobile apps and their definition based on literatures database search
| Record | Features | Definition |
|---|---|---|
| 1 | Blood Glucose Tracking | Comparison of BG test results entered in different sessions |
| 2 | Insulin and Medication Tracking | Comparison of insulin test results entered in different sessions |
| 3 | Physical Activity Tracking | Comparison of physical activity results entered in different sessions |
| 4 | Weight Tracking | Comparison of weight checking results entered in different sessions |
| 5 | Blood pressure Tracking | Comparison of blood pressure test results entered in different sessions |
| 6 | Diet Tracking | Comparison of calorie, fat or other nutritional information of consumed meal via barcode or selected from the list |
| 7 | Food database | The extent to which the user can choose consumed food in a list |
| 8 | Mealtime tagging | To tag, the time/s patients have had meal/s over a specific time |
| 9 | Education | To provide a specific tip for patients to better manage a condition |
| 10 | Messaging | To communicate healthcare to get a new update of app or events in the health center |
| 11 | Data export | To change entered data into other formats such as CSV or email |
| 12 | Synchronization to website | To keep the mobile app in coherence with the website in order to maintain data integrity between these two sources |
| 13 | Synchronization with PHR | To keep the mobile app in coherence with PHR in order to maintain data integrity between these two sources |
| 14 | Synchronization with social network | To keep the mobile app in coherence with the social network in order to maintain data integrity between these two sources |
| 15 | Color Coding | Categories are coded by different colors based on BG values including low, middle and high level |
| 16 | Alerts | To alert the user about the condition |
| 17 | Reminder | To remind patient about activities user must do for self-care |
| 18 | Prediction | To predict condition based on data entered into the system |
| 19 | Estimation | To estimate the value of the BG level based on user condition using entered related data |
| 20 | Detection | To detect specific condition based on the value of BG entered in the system |
| 21 | Trend Chart View | To show a graphical display of BG or others health-related measured values over time |
| 22 | Logbook View | To review important events related to BG management in an electronic page |
| 23 | Numerical Indicators | To calculate the measures of patient BG, BP and so on by Average, Standard Deviation |
| 24 | Customizable Theme | To change the display or layout of the app |
| 25 | Data Entry Automation | To upload the level of blood glucose into the app automatically due to the compatibility of the app and blood glucose meter reader or insulin pump |
| 26 | Preset Notes | To use a structured note by the user in order to remember something or a number |
| 27 | Custom Notes | To use unstructured note by the user in order to remember something or a number |
| 28 | Target range setting | To allow the user to establish what they want to achieve in terms of BG level or other important measurements |
| 29 | Security | The ability to put pin code or password for whole or database part of the app |
| 30 | Communication | The possibility of connecting patient to other patients, friends or family member via email, write a review or exchange their experiences |
| 31 | Problem Solving | The ability to figure out how to problem solve in general and for specific issues you may be facing. |
| 32 | Reducing Risks | The ability to find the best way to help reduce patients risks and avoid other health problems |
| 33 | Healthy Coping | The ability to find healthy ways to cope that work with patients’ lifestyle |
To better utilize the potential of mobile technologies for interventions, it is better to use theories and models to design and develop complex interventions that respond appropriately to different inputs [28]. One of the best references could be the American Association of Diabetes Educators (AADE) guidance, because of providing a collection of necessities for diabetes mobile apps. According to the American Association of Diabetes Educators, explicitly states that mobile apps for diabetic patients should improve or upgrade any of seven therapeutic elements. These seven elements include 1. healthy eating, 2. being active, 3. monitoring, 4. taking medications, 5. problem solving, 6. reducing risks, and 7. healthy coping [29].
For the second step based on expert’s opinions, 23 relevant features out of 33 were approved with CVI = 0.79 or more. CVI of each feature presented in Table 2. In addition, all features had CVR higher than 0.99. These features include: blood glucose tracking, insulin and medication tracking, physical activity tracking, weight and BMI tracking, blood pressure tracking, mealtime tagging, food database, diet tracking, educational materials, healthy coping, reducing risks, problem-solving, messaging, color coding, alerts, reminder, target range setting, trend chart view, logbook view, numerical indicators view, customizable theme, preset notes, custom notes.
Table 2.
The values of CVI of each feature of Diabetes type II mobile application
| Record | Features | CVI | Acceptable | Record | Features | CVI | Acceptable |
|---|---|---|---|---|---|---|---|
| 1 | Blood Glucose Tracking | 1 | √ | 18 | Alerts | 1 | √ |
| 2 | Insulin and Medication Tracking | 1 | √ | 19 | Reminder | 1 | √ |
| 3 | Physical Activity Tracking | 1 | √ | 20 | Prediction of insulin dosage | 0.66 | × |
| 4 | Weight and BMI Tracking | 1 | √ | 21 | Target range setting | 0.50 | √ |
| 5 | Blood pressure Tracking | 0.83 | √ | 22 | Trend Chart View | 1 | √ |
| 6 | Meal time tagging | 0.83 | √ | 23 | Logbook View | 0.83 | √ |
| 7 | Food (Diet) database | 1 | √ | 24 | Numerical indicators View | 1 | √ |
| 8 | Diet Tracking | 1 | √ | 25 | Customizable Theme | 0.83 | √ |
| 9 | Educational Materials | 1 | √ | 26 | Preset Notes | 0.83 | √ |
| 10 | Healthy Coping | 1 | √ | 27 | Custom Notes | 0.83 | √ |
| 11 | Reducing Risks | 0.83 | √ | 28 | Communication | 0.33 | × |
| 12 | Problem Solving | 1 | √ | 29 | Estimation | 0.50 | × |
| 13 | Data export | 0.66 | × | 30 | Detection | 0.50 | × |
| 14 | Portability with the website | 0.66 | × | 31 | Data entry automation | 0.16 | × |
| 15 | Portability with social network | 0.50 | × | 32 | Security | 0.50 | × |
| 16 | Messaging | 0.83 | √ | 33 | Portability with PHR | 0.50 | × |
| 17 | Color Coding | 1 | √ |
The next goal of this study in the last step was to evaluate the importance of features through the Friedman test. The results of the study are shown in Table 3. We can consider the cutting point to be 11.5. In other words, to select the best and appropriate features we assumed features which gain mean rank more than this point.
Table 3.
Descriptive analysis and ranking of final essential features
| Rank | Variable | Mean | SD | Min | Max | Mean rank |
|---|---|---|---|---|---|---|
| 1 | Blood Glucose Tracking | 4.90 | .30 | 4 | 5 | 16.71 |
| 2 | Educational material | 4.86 | .36 | 4 | 5 | 16.31 |
| 3 | Problem solving | 4.76 | .44 | 4 | 5 | 15.31 |
| 4 | Reminder | 4.71 | .46 | 4 | 5 | 15.24 |
| 5 | Alert | 4.71 | .46 | 4 | 5 | 15.00 |
| 6 | Weight and BMI Tracking | 4.62 | .50 | 4 | 5 | 14.14 |
| 7 | Reducing risk | 4.62 | .67 | 3 | 5 | 14.02 |
| 8 | Physical activity Tracking | 4.57 | .51 | 4 | 5 | 13.81 |
| 9 | Healthy coping | 4.57 | .60 | 3 | 5 | 13.64 |
| 10 | Blood pressure Tracking | 4.52 | .60 | 3 | 5 | 13.24 |
| 11 | Insulin and Medication Tracking | 4.52 | .60 | 3 | 5 | 13.14 |
| 12 | Trend chart view | 4.48 | .68 | 3 | 5 | 12.83 |
| 13 | Log book view | 4.40 | .75 | 3 | 5 | 11.50 |
| 14 | Diet Tracking | 4.41 | .96 | 1 | 5 | 11.02 |
| 15 | Meal time tagging | 4.19 | .68 | 3 | 5 | 10.43 |
| 16 | Target range setting | 4.24 | .63 | 3 | 5 | 10.50 |
| 17 | Messaging | 4.14 | .85 | 2 | 5 | 10.21 |
| 18 | Color coding | 3.95 | 1.16 | 1 | 5 | 9.69 |
| 19 | Custom note | 4.14 | .66 | 3 | 5 | 9.52 |
| 20 | Food database | 4.10 | .54 | 3 | 5 | 8.95 |
| 21 | Customizable theme | 3.90 | .83 | 2 | 5 | 8.33 |
| 22 | Preset note | 3.81 | .75 | 3 | 5 | 7.19 |
| 23 | Numerical indicator | 3.57 | 1.12 | 1 | 5 | 6.50 |
Among the features suggested by experts, the highest degree of importance was attributed to the blood glucose tracking feature with a mean score of 16.71, and the lowest grade of importance attributed to the display of numerical indicator with a mean score of 6.50. These results are also consistent with the results of the previous step, which is indicated by experts. Therefore, we have 23 final essential features with their rate of priority.
Discussion
Some experts have provided a brief list of features available in diabetes care apps in addition attention to language and platform of them, and apparent features [25]. Some others list different features based on some high rating of apps used for self-monitoring of blood glucose management [21, 22].
In our review focus was on the necessity, relevancy, and importance. In the suggested features set, the results are shown that blood glucose tracking is in the highest level of necessity and importance for diabetes type II self- care. This finding is also confirmed by previous studies. Many of the researches have reported that diabetes people could have a better self-care in case they control their blood glucose level [18, 25, 30].
Education that has been addressed as the second important feature might affect directly on self-efficacy which is a cornerstone element in self-care improvement [31]. Hence, this feature could be ranked in second. However, this feature is not sufficiently considered when diabetes app is being developed. Problem-solving was another feature which has been also emphasized by AADE [28]; This feature may lead to improve patient’s self-efficacy and therefore this improve self-care [31]. This feature is less common in diabetes apps, unfortunately. One of the best reason for high priority of this features is a relationship between education and blood glucose tracking as identifying the trends of blood glucose of patients could make a good plan or take educations more seriously to improve related self-care behaviors [9].
Other features that were recognized as the final and high score ones are related to the monitoring of the main elements of care for diabetes II, which are recognized as central and fundamental features for mobile apps like weight and BMI tracking or physical activity tracking [32].
Using communications means like reminders have been reported from other prominent and important features. Communication between patients and care providers plays a very important role in monitoring the disease and even patient education. For example, by sending reminders for taking medication or appointments or adhering to medical conditions and paying attention to educational tips, there are somethings that can be promoted to improve the self-care of diabetic patients [33].
Our results almost were in line with the results of the study of Chomutare et al. [18]. In their article, the analysis of apps in the market showed importance degrees similar to our results in Table 3. Perhaps one of the concerns of physicians about mobile apps has been the effectiveness of these apps. Another reason might be due to this fact that these apps have been delivered and marketed without clinical examinations without the presence of patients and experts’ opinion [34, 35]. While, these considerations explicitly mentioned in mobile apps developing [16, 17]. Thus, it is necessary that the number of considered features in apps to be set up as low as possible and matched with the apps desired goals. Therefore, the development of features in diabetes mobile apps requires to be more specific and user oriented. That is, mobile apps can be a useful tool for customized self-care for diabetic patients if they would be blended with evidence-based self-care behaviors [36]. although, usefulness of healthcare mobile apps depends on other factors besides mobile phone technologies, such as the healthcare context, social values, and culture. therefore more researches are needed [37].
Conclusion
There are many diabetes mobile apps which are not consistent with the recommendations of the guidelines. Therefore, the more design and development of diabetes mobile apps based on studies and guidelines, future plans will be beneficial. Therefore, partnerships between academics and apps developers may be an important component of future diabetes mobile apps approaches both in research and practice. It is hoped that the results of this paper could be used to set an appropriate framework of apps features and component for diabetes type II mobile apps in futures. In addition, this study could be a step for the path of designing the approved apps and presenting a set of features of the case.
Acknowledgments
This study is a part of a Ph.D. dissertation financially supported by Tehran University of Medical Sciences (Grant: # 37529-97-01-31). We appreciate the contributions of all members of the Board of Health Informatics, Adult Endocrinologist, Health Education and Promotion which commented on our questionnaire form.
Author’s contributions
Conception and design: Raheleh Salari, Sharareh R. Niakan Kalhori, Marjan Ghazisaeedi. Provision of study material or patients: Raheleh Salari, Sharareh R. Niakan Kalhori, Marjan Ghazisaeedi. Collection and assembly of data: Raheleh Salari, Sharareh R. Niakan Kalhori. Data analysis and interpretation: Raheleh Salari, Sharareh R. Niakan Kalhori. Manuscript writing: All authors. Final approval of manuscript: All authors.
Compliance with ethical standards
Conflict of interest
The authors have no conflicts of interest to declare.
Limitation
The number of specialists filling out the questionnaire was less than expected. Due to the widespread geographical dispersion, there was no possibility to deliver this form in paper in person for all of them. Therefore the questionnaire form emeiled in electronic form. Inaccessibility to the full text of some articles were another limitation in this study.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Breland JY, Yeh VM, Yu J. Adherence to evidence-based guidelines among diabetes self-management apps. Transl Behav Med. 2013;3(3):277–286. doi: 10.1007/s13142-013-0205-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation. Global report on diabetes. https://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf?sequence=1. Accessed 19 March 2019.
- 3.Torjesen I. More than half of diabetes patients are not getting standard health checks. British Medical Journal Publishing Group. 2012. [DOI] [PubMed]
- 4.Fatehi F, Menon A, Bird D. Diabetes care in the digital era: a synoptic overview. Curr Diab Rep. 2018;18(7):38. doi: 10.1007/s11892-018-1013-5. [DOI] [PubMed] [Google Scholar]
- 5.Group UPDS Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352(9131):837–853. doi: 10.1016/S0140-6736(98)07019-6. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organisation . The global diffusion of eHealth: making universal health coverage achievable: report of the third global survey on eHealth. Geneva: WHO; 2016. [Google Scholar]
- 7.Holtz B, Lauckner C. Diabetes management via mobile phones: a systematic review. Telemed J E Health. 2012;18(3):175–184. doi: 10.1089/tmj.2011.0119. [DOI] [PubMed] [Google Scholar]
- 8.Eng DS, Lee JM. The promise and peril of mobile health appss for diabetes and endocrinology. Pediatr Diabetes. 2013;14(4):231–238. doi: 10.1111/pedi.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu H, McMahon SK, Gross CR, et al. Usability and clinical efficacy of diabetes mobile applications for adults with type 2 diabetes: a systematic review. Diabetes Res Clin Pract. 2017;131:70–81. doi: 10.1016/j.diabres.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 10.Eng DS, Lee JM. The promise and peril of mobile health applications for diabetes and endocrinology. Pediatr Diabetes. 2013;14(4):231–238. doi: 10.1111/pedi.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ristau RA, Yang J, White JR. Evaluation and evolution of diabetes mobile appss: key factors for healthcare professionals seeking to guide patients. Diabetes Spectr. 2013;26(4):211–215. doi: 10.2337/diaspect.26.4.211. [DOI] [Google Scholar]
- 12.Goyal S, Lewis G, Yu C, Rotondi M, Seto E, Cafazzo JA. Evaluation of a behavioral mobile phone app intervention for the self-management of type 2 diabetes: randomized controlled trial protocol. JMIR Res Protoc. 2016;5(3):e174. doi: 10.2196/resprot.5959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garabedian LF, Ross-Degnan D, Wharam JF. Mobile phone and smartphone technologies for diabetes care and self-management. Curr Diab Rep. 2015;15(12):109. doi: 10.1007/s11892-015-0680-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Basilico A, Marceglia S, Bonacina S, Pinciroli F. Advising patients on selecting trustful apps for diabetes self-care. Comput Biol Med. 2016;71:86–96. doi: 10.1016/j.compbiomed.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 15.Strickland PAO, Hudson SV, Piasecki A, Hahn K, Cohen D, Orzano AJ, Parchman ML, Crabtree BF. Features of the Chronic Care Model (CCM) associated with behavioral counseling and diabetes care in community primary care. J Am Board Fam Med. 2010;23(3):295–305. doi: 10.3122/jabfm.2010.03.090141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sibal L, Home PD. Management of type 2 diabetes: NICE guidelines. Clin Med. 2009;9(4):353–357. doi: 10.7861/clinmedicine.9-4-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paulweber B, Valensi P, Lindström J, Lalic N, Greaves C, McKee M, Kissimova-Skarbek K, Liatis S, Cosson E, Szendroedi J, Sheppard K, Charlesworth K, Felton AM, Hall M, Rissanen A, Tuomilehto J, Schwarz P, Roden M, Paulweber M, Stadlmayr A, Kedenko L, Katsilambros N, Makrilakis K, Kamenov Z, Evans P, Gilis-Januszewska A, Lalic K, Jotic A, Djordevic P, Dimitrijevic-Sreckovic V, Hühmer U, Kulzer B, Puhl S, Lee-Barkey Y, AlKerwi A, Abraham C, Hardeman W, Acosta T, Adler M, AlKerwi A, Barengo N, Barengo R, Boavida J, Charlesworth K, Christov V, Claussen B, Cos X, Cosson E, Deceukelier S, Dimitrijevic-Sreckovic V, Djordjevic P, Evans P, Felton AM, Fischer M, Gabriel-Sanchez R, Gilis-Januszewska A, Goldfracht M, Gomez J, Greaves C, Hall M, Handke U, Hauner H, Herbst J, Hermanns N, Herrebrugh L, Huber C, Hühmer U, Huttunen J, Jotic A, Kamenov Z, Karadeniz S, Katsilambros N, Khalangot M, Kissimova-Skarbek K, Köhler D, Kopp V, Kronsbein P, Kulzer B, Kyne-Grzebalski D, Lalic K, Lalic N, Landgraf R, Lee-Barkey Y, Liatis S, Lindström J, Makrilakis K, McIntosh C, McKee M, Mesquita A, Misina D, Muylle F, Neumann A, Paiva A, Pajunen P, Paulweber B, Peltonen M, Perrenoud L, Pfeiffer A, Pölönen A, Puhl S, Raposo F, Reinehr T, Rissanen A, Robinson C, Roden M, Rothe U, Saaristo T, Scholl J, Schwarz P, Sheppard K, Spiers S, Stemper T, Stratmann B, Szendroedi J, Szybinski Z, Tankova T, Telle-Hjellset V, Terry G, Tolks D, Toti F, Tuomilehto J, Undeutsch A, Valadas C, Valensi P, Velickiene D, Vermunt P, Weiss R, Wens J, Yilmaz T. A European evidence-based guideline for the prevention of type 2 diabetes. Horm Metab Res. 2010;42(S 01):S3–S36. doi: 10.1055/s-0029-1240928. [DOI] [PubMed] [Google Scholar]
- 18.Chomutare T, Fernandez-Luque L, Årsand E, Hartvigsen G. Features of mobile diabetes appss: review of the literature and analysis of current appss compared against evidence-based guidelines. J Med Internet Res. 2011;13(3):e65. doi: 10.2196/jmir.1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gao J, Wang J, Zhu Y, Yu J. Validation of an information–motivation–behavioral skills model of self-care among Chinese adults with type 2 diabetes. BMC Public Health. 2013;13(1):100. doi: 10.1186/1471-2458-13-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williams JP, Schroeder D. Popular glucose tracking apps and use of mHealth by Latinos with diabetes. JMIR Mhealth Uhealth. 2015;3(3):e84. doi: 10.2196/mhealth.3986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rao A, Hou P, Golnik T, Flaherty J, Vu S. Evolution of data management tools for managing self-monitoring of blood glucose results: a survey of iPhone appss. J Diabetes Sci Technol. 2010;4(4):949–957. doi: 10.1177/193229681000400426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klonoff DC. The current status of mHealth for diabetes: will it be the next big thing? J Diabetes Sci Technol. 2013;7(3):749–758. doi: 10.1177/193229681300700321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Demidowich AP, Lu K, Tamler R, Bloomgarden Z. An evaluation of diabetes self-management appss for android smartphones. J Telemed Telecare. 2012;18(4):235–238. doi: 10.1258/jtt.2012.111002. [DOI] [PubMed] [Google Scholar]
- 24.Chen L, Chuang L-M, Chang C-H, Wang C-S, Wang I-C, Chung Y, Peng HY, Chen HC, Hsu YL, Lin YS, Chen HJ, Chang TC, Jiang YD, Lee HC, Tan CT, Chang HL, Lai F. Evaluating self-management behaviors of diabetic patients in a telehealthcare program: longitudinal study over 18 months. J Med Internet Res. 2013;15(12):e266. doi: 10.2196/jmir.2699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arnhold Madlen, Quade Mandy, Kirch Wilhelm. Mobile Applications for Diabetics: A Systematic Review and Expert-Based Usability Evaluation Considering the Special Requirements of Diabetes Patients Age 50 Years or Older. Journal of Medical Internet Research. 2014;16(4):e104. doi: 10.2196/jmir.2968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–575. doi: 10.1111/j.1744-6570.1975.tb01393.x. [DOI] [Google Scholar]
- 27.Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;3596:382–386. [PubMed] [Google Scholar]
- 28.Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med. 2011;1(1):53–71. doi: 10.1007/s13142-011-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peeples M, Tomky D, Mulcahy K, Peyrot M, Siminerio L, Project AO, et al. Evolution of the American Association of Diabetes Educators' diabetes education outcomes project. The Diabetes Educator. 2007;33(5):794–817. doi: 10.1177/0145721707307615. [DOI] [PubMed] [Google Scholar]
- 30.Wilkinson A, Whitehead L, Ritchie L. Factors influencing the ability to self-manage diabetes for adults living with type 1 or 2 diabetes. Int J Nurs Stud. 2014;51(1):111–122. doi: 10.1016/j.ijnurstu.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 31.Sigurðardóttir ÁK. Self-care in diabetes: model of factors affecting self-care. J Clin Nurs. 2005;14(3):301–314. doi: 10.1111/j.1365-2702.2004.01043.x. [DOI] [PubMed] [Google Scholar]
- 32.Issom D-Z, Woldaregay AZ, Chomutare T, Bradway M, Årsand E, Hartvigsen G. Mobile apps for people with diabetes published between 2010 and 2015. Diabetes Management (DMJ) 2015;5(6):539–550. doi: 10.2217/dmt.15.40. [DOI] [Google Scholar]
- 33.Shi C. Mobile phone messaging for facilitating self-management of long-term illnesses: summaries of nursing care-related systematic reviews from the Cochrane library. International Journal of Evidence-Based Healthcare. 2013;11(4):344–345. doi: 10.1111/1744-1609.12041. [DOI] [Google Scholar]
- 34.Fijacko N, Brzan PP, Stiglic G. Mobile applications for type 2 diabetes risk estimation: a systematic review. J Med Syst. 2015;39(10):124. doi: 10.1007/s10916-015-0319-y. [DOI] [PubMed] [Google Scholar]
- 35.Okazaki S, Castañeda JA, Sanz S, Henseler J. Factors affecting mobile diabetes monitoring adoption among physicians: questionnaire study and path model. J Med Internet Res. 2012;14(6):e183. doi: 10.2196/jmir.2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eyler AA. Are diabetes self-management apps based on evidence? Transl Behav Med. 2013;3(3):233. doi: 10.1007/s13142-013-0233-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beratarrechea Andrea, Lee Allison G., Willner Jonathan M., Jahangir Eiman, Ciapponi Agustín, Rubinstein Adolfo. The Impact of Mobile Health Interventions on Chronic Disease Outcomes in Developing Countries: A Systematic Review. Telemedicine and e-Health. 2014;20(1):75–82. doi: 10.1089/tmj.2012.0328. [DOI] [PMC free article] [PubMed] [Google Scholar]