1. Introduction
Poor health outcomes of chronically ill low-income adults are costly in both fiscal and human terms. One-third of Americans have hypertension and < 50% of those have their disease controlled, which costs the US $51 billion annually in medical care and productivity [13]. African American adults have the highest rates of hypertension in the world (> 43%) with high rates of exacerbations and complications [28, 10]. Low-income African American adults face life situations complicated by limited resources, high environmental and social risks, a high burden of stress and limited access to healthcare, all of which contribute to a substantial risk for multiple chronic conditions [10, 11, 19]. These factors may also contribute to a low sense of trust in the healthcare system, low self-efficacy regarding self-management behaviors to control hypertension, poor chronic disease management and costly sequelae [6, 19]. Thus, new intervention models and systems of care that are consumer-driven must be developed to improve outcomes. Client self-management of chronic diseases has emerged as a key factor in improved health outcomes [8]. We tested the effect of an innovative Ecological Nurse Case Management (ENCM) intervention on perceived stress, self-efficacy, self-management behaviors (SMB), and health status of low-income, chronically ill, African American adults. We hypothesized ENCM would reduce stress and increase self-efficacy and positively impact health status. We expected that that clients receiving this intervention would show decreased blood pressure (B/P), body mass index (BMI) and waist circumference (WC).
2. Methods
2.1. Design, setting and sample
This study was a two-group randomized clinical trial pilot study with repeated measures over six months. Potential participants were identified by health care providers in a free community medical clinic serving primarily low-income African Americans. With > 160 persons with hypertension seen per month across three locations, this clinic provided excellent access to the target population. It was operated by a local major health care system and run with a large cadre of interprofessional volunteer providers, medical Residents and health professions students. Three paid staff, a medical director, nurse clinic manager and pharmacist, provide leadership for clinic services. Services included primary care and some limited specialty medical service; individual health education; dental, vision and social worker services; and health promotion classes. The study primary investigator (PI) had participated in collaborative partnership activities with the clinic over the past 25 years. The clinic administrator supported and facilitated the study activities with the clinic staff.
Clients were eligible for enrollment if they were African American, aged 30–65 years, receiving treatment for hypertension with antihypertensive drugs, and spoke and wrote English. Exclusion criteria were clients with acute or terminal condition (e.g., Myocardial infarction, terminal cancer), psychiatric diagnosis (e.g., schizophrenia or cognitive impairment), or other conditions that would limit participation in the study. Eligibility was confirmed and written informed consent obtained from all participants at their baseline visit. The study was approved by the University Institutional Review Board (IRB) (#15.225) and registered at clinicaltrials.gov.
2.2. Procedure
Flyers about the study were posted at the three clinic sites with a contact number so clients could call the PI to ask about study enrollment. Clinic staff also screened clients and referred those meeting the study inclusion criteria to the PI. When further client interviews by the PI or Research Assistant (RA) confirmed that all inclusion criteria and no exclusion criteria were met, the study protocol was explained and clients were given the option to join the study. Following completion of informed consent, clients were randomized to either treatment group or control group (1:1 ratio). Randomization was carried out by a computer random-generator program. Clients in the treatment group received the ENCM intervention and those in the control group received usual clinic care. Usual clinic care was defined as medical care routinely received in the free clinic. The control group were offered six months of free ENCM services at the University nurse-managed health centers when the study was completed.
Immediately after enrollment, the PI or RA collected baseline study data. The PI or RA made follow-up appointments with each subject to repeat the same measurements at about 1, 3, and 6 months of the study, which are common intervals for return visits for hypertension management. Gift cards of $20 from a local discount store were provided for both groups at each measurement visit to improve client retention. The interventionist, a community health nurse prepared with a Bachelor’s degree; over 14 years of experience; and ENCM intervention training, contacted the subjects in the experimental group for ENCM intervention visits either at the time of their enrollment or via a later phone call. The intervention group participants were asked to visit with the intervention nurse at least once a month.
2.3. Intervention
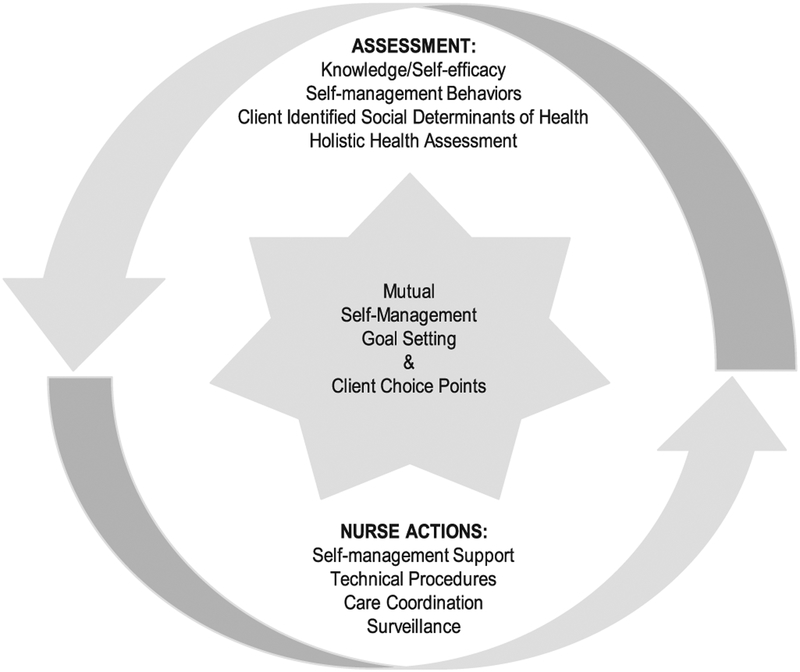
The Individual and Family Self-Management Theory (IFSMT) [20] provided the framework for this study which examined the impact of an innovative ENCM intervention for low-income African American adults on multiple variables related to the IFSMT ‘Context’ (gender and perceived stress) and ‘Process’ (self-efficacy), and ‘Proximal’ and ‘Distal’ ‘Outcomes’ components. The ‘Proximal Outcome’ was hypertension SMB and the ‘Distal Outcomes’ related to hypertension health status including, B/P, BMI and WC. The IFSMT ‘Intervention’ component was operationalized by the ENCM. A full description of the intervention is registered at clinicaltrials.gov. The ENCM (Fig. 1) intervention relies on an assumption that given the proper tools (i.e. knowledge, skills and support) individuals can learn to better self-manage their symptoms on a day to day basis and better utilize the health care resources available to them. ENCM is grounded in an acknowledgment of individual/family strengths and resilience. The intervention is individualized to each client. Clients are valued as managers of their own care and promoted to become experts in self-care. Mutual Self-Management Goal Setting, which is key to establishing trust and retaining clients, and Client Choice Points, such as self-management preferences and visit place and times, are the primary components of the ENCM intervention.
Fig. 1.
Components of the ecological nurse case management intervention. © 2014 Bev Zabler
The ENCM intervention is non-linear, though it follows a basic sequence through the course of the client visits. At the first visit in this study, the interventionist asked the client to identify three goals to improve her/his health in which she might be of assistance. Client-interventionist dialogue refined the goals to be achievable in 6 months. This practice was a key component of the ENCM intervention, termed ‘Mutual Self-Management Goal Setting’ (Fig. 1). The interventionist then initiated a holistic health assessment, inclusive of a health history encompassing information on SMB, support systems, stress management/coping skills, spiritual/cultural beliefs, and past experiences with the health care system. She followed each client’s lead regarding the depth of the discussion in the initial visit. Full holistic assessments were completed with each client in subsequent visits.
The interventionist nurse provided any or all of four primary nurse actions targeting specific problems identified by the client and nurse in the visit and individualized to the client. These actions included: self-management support, inclusive of both health education and behavior modification; technical procedures; care coordination; and/or surveillance. Multiple strategies and options were discussed at the visits and the nurse consistently elicited and respected client’s choices. At the end of each intervention visit, collaborative plans were made for subsequent appointments for which the client chose the venue and desired time. Monthly appointments for the next 6-months were agreed to for the minimal intervention dose. Clients could choose more frequent visits or phone calls. After the initial intervention training, the PI conducted weekly intervention fidelity checks with the interventionist nurse, who completed a ‘Branching Simulation’ [16], compliance checklist and either case reviews or documentation audits.
2.4. Measures
We used surveys to measure variables related to the IFSMT components of ‘Context’ (Stress) and ‘Process’ (Self-Efficacy), and the ‘Proximal Outcome’ of Hypertension SMB. The surveys for perceived stress [7, 21], self-efficacy [22], hypertension self-management [12] have each been validated for use in low-income African American populations. The reliability Alpha coefficients of these scales among our subjects were 0.81 for perceived stress, 0.89 for self-efficacy, and 0.92 for hypertension self-management. We measured the IFSMT Distal Outcome of Health Status by B/P [18], WC [29] and BMI from height and weight [17] based on standardized procedures. For example, we measured B/Ps three times on the left arm unless contraindicated, with the subject in a sitting position, after a 30-min rest. The PI or RA conducted the measurements at study enrollment (baseline) and at 1, 3, and 6 months.
2.5. Participants
We achieved 96.7% of our recruitment target goal, enrolling 59 (Table 1) of a targeted sample of 61 participants determined by a priori power analysis, and realized an 83.1% retention rate at the end of six months. At baseline, the 59 non-Hispanic Black participants in the study has an average age of 53.73 years (SD = 6.67) and 63% were women. About half of the participants were single (48%), 27% were married, 12% were separated, 12% were divorced and only 2% were widowed. Most participants were currently employed (73%), head of household (85%), and 85% were uninsured. The mean monthly income was $1167 (SD = 724.1). In the control group, the mean age was 53.60 (SD = 6.41) years and 70% were women. In ENCM intervention group, the mean age was 53.86 (SD = 7.04) years with 55% women. There were no significant differences in the demographic characteristics between the two groups.
Table 1.
Characteristics of study groups (n = 59).
| Control (n = 30) | ENCM (n = 29) | |
|---|---|---|
| Age in years (mean [SD]) | 53.60 [6.4] | 53.86 [7.0] |
| Gender (%) | ||
| Male | 30.0 | 44.8 |
| Female | 70.0 | 55.2 |
| Marital status (%) | ||
| Single | 50.0 | 44.8 |
| Separated | 10.0 | 13.8 |
| Divorced | 10.0 | 13.8 |
| Married | 26.7 | 27.6 |
| Widowed | 3.3 | 0.0 |
| Current employment (%) | ||
| Employed | 70.0 | 75.9 |
| Unemployed | 23.3 | 20.7 |
| Retired | 6.7 | 3.4 |
| Head of household (%) | 86.7 | 82.8 |
| Type of Insurance (%) | ||
| None | 83.3 | 86.2 |
| Medicare | 3.3 | 3.4 |
| Medicaid HMO | 6.7 | 3.4 |
| Medicaid Straight | 3.3 | 0.0 |
| Private | 0.0 | 6.9 |
| Other | 3.3 | 0.0 |
2.6. Data analysis
The data were analyzed using Stata SE 14 [23]. Descriptive statistics were used to summarize the characteristics of study groups and describe the measurement results. A mixed model analysis was used to estimate the differences between an ENCM intervention group and a control group related to changes in the identified IFSMT proximal and distal outcome variables. Over the four waves of observation time, there were 12% total missing values on outcome variables. To properly handle missing data and to make valid statistical inference with minimal bias, we employed multiple imputation (mi) methods [30]. All statistical analyses were conducted based on these multiply imputed data with the STATA multiple imputations (mi) estimate modules. To correctly specify our panel data, we used a STATA random-effects GLS regression model procedure for estimating the time effects on outcome variables controlling for the background characteristics measured at baseline.
3. Results
3.1. Baseline measurements
Means of systolic and diastolic B/Ps for both groups of participants (Table 2) were controlled within the prehypertension level [3] at the time of the baseline measurements. Most the participants in this study were obese with mean BMI scores ≥35 [4]. Means of the measures for perceived stress, self-efficacy, hypertension SMB, and WC were also similar across the groups at baseline.
Table 2.
Mean scores and p-values of time-group interactions for perceived stress, self-efficacy, and hypertension self-management behaviors and health status measurements (N = 59).
| Individual and Family Self-Management Theory (IFSMT) Component Variables | Control Group (n = 30) Mean (SE) | Intervention Group (n = 29) Mean (SE) | p-value Time-Group Interactions | Effect Size (Cohen’s d) |
|---|---|---|---|---|
| Context: Perceived Stress1a | ||||
| Baseline | 26.82 (1.22) | 26.99 (1.23) | −0.07 | |
| 1-month follow up | 24.86 (1.22) | 24.95 (1.30) | 0.962 | −0.07 |
| 3-month follow up | 25.30 (1.22) | 23.15 (1.28) | 0.149 | −0.39 |
| 6-month follow | 25.61 (1.27) | 22.47 (1.35) | 0.047* | −0.49 |
| Process: Self-efficacy2b | ||||
| Baseline | 38.53 (1.20) | 39.40 (1.22) | 0.22 | |
| 1-month follow up | 38.19 (1.21) | 39.69 (1.25) | 0.713 | 0.27 |
| 3-month follow up | 38.34 (1.21) | 39.67 (1.26) | 0.795 | 0.26 |
| 6-month follow | 36.54 (1.23) | 40.67 (1.33) | 0.066 | 0.62 |
| Proximal Outcome: Hypertension Self-Management Behaviors3b | ||||
| Baseline | 49.42 (1.58) | 46.73 (1.60) | −0.32 | |
| 1-month follow up | 52.16 (1.59) | 50.64 (1.64) | 0.542 | −0.15 |
| 3-month follow up | 52.29 (1.59) | 52.69 (1.71) | 0.119 | 0.05 |
| 6-month follow | 51.37 (1.59) | 54.27 (1.70) | 0.005* | 0.33 |
| Distal Outcomes: (Health Status Measurements) | ||||
| Systolic Blood Pressure (mmHg) | ||||
| Baseline | 130.46 (2.99) | 131.62 (3.04) | 0.05 | |
| 1-month follow up | 132.25 (3.03) | 124.73 (3.32) | 0.055 | −0.41 |
| 3-month follow up | 130.89 (3.03) | 126.66 (3.29) | 0.230 | −0.27 |
| 6-month follow | 134.88 (3.08) | 126.22 (3.47) | 0.037* | −0.54 |
| Diastolic Blood Pressure (mmHg) | ||||
| Baseline | 78.17 (1.47) | 79.99 (1.49) | 0.28 | |
| 1-month follow up | 78.03 (1.49) | 76.71 (1.56) | 0.157 | −0.12 |
| 3-month follow up | 78.73 (1.49) | 78.38 (1.69) | 0.345 | −0.01 |
| 6-month follow | 79.05 (1.51) | 77.69 (1.70) | 0.172 | −0.13 |
| Body Mass Index (BMI) Score | ||||
| Baseline | 36.46 (1.47) | 35.31 (1.49) | −0.23 | |
| 1-month follow up | 36.28 (1.49) | 34.32 (1.61) | 0.537 | −0.31 |
| 3-month follow up | 35.91 (1.52) | 33.93 (1.58) | 0.532 | −0.31 |
| 6-month follow | 36.74 (1.53) | 33.98 (1.76) | 0.292 | −0.37 |
| Waist Circumference (cm) | ||||
| Baseline | 114.27 (3.29) | 113.23 (3.35) | −0.12 | |
| 1-month follow up | 115.45 (3.37) | 109.98 (3.58) | 0.156 | −0.34 |
| 3-month follow up | 115.38 (3.36) | 109.35 (3.57) | 0.108 | −0.36 |
| 6-month follow | 118.58 (3.48) | 108.09 (4.02) | 0.017* | −0.52 |
Results showed improvements in perceived stress, hypertension SMBs, systolic B/P, and WC for the ENCM intervention group. In the following sections, we summarize the study results organized by their related IFSMT component of ‘Context’, ‘Process’ and ‘Proximal’ and ’Distal’ ‘Outcome’ variables. The p-values of the time-group interactions for all variables are shown in the Table 2. Small to medium effect sizes (Cohen’s d = 0.33 to 0.62) were found for all outcome variables (Table 2).
3.1.1. Context: perceived stress
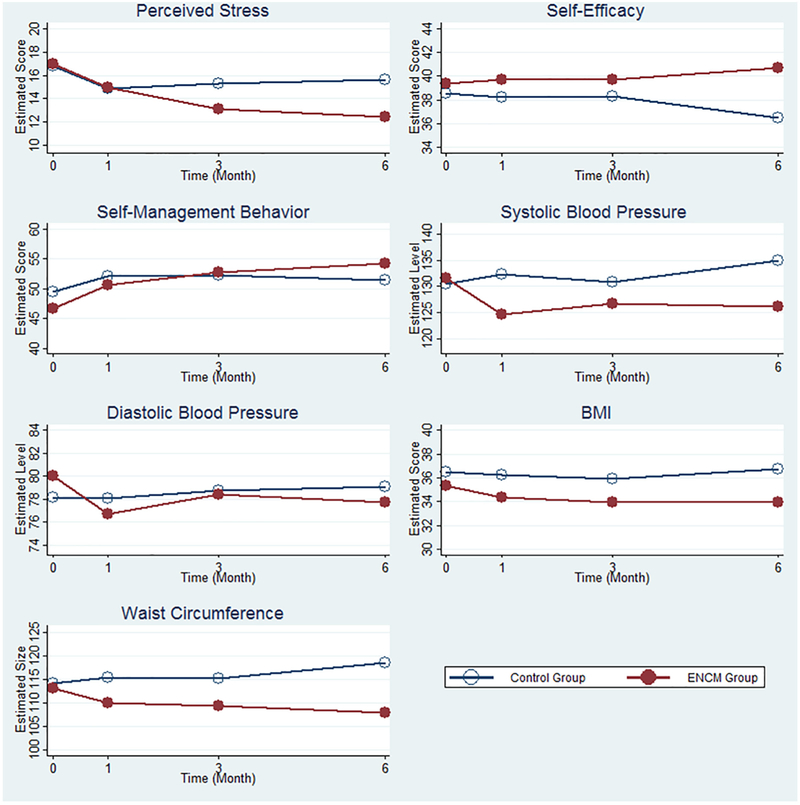
Perceived Stress survey results were comparable at baseline and 1-month for both the ENCM and control group (Fig. 2). Non-significant trends were seen at 3-months in the ENCM scores decreasing, which indicates lower perceived stress levels. In month 6, there were significantly (p = .047) lowered perceived stress scores for the ENCM group compared to the changes observed in the control group.
Fig. 2.
Estimated outcomes by time and group.
3.1.2. Process: self-efficacy
The Self-efficacy survey scores again were nearly the same at baseline, 1- and 3-months. In the 6-month measures, the Control group scores decreased and the ENCM group scores increased without a statistically significant difference.
3.1.3. Proximal outcome: self-management behaviors (SMB) for hypertension
As to the proximal outcome of SMB for hypertension, a significant difference was found at the 1-month follow-up compared to baseline measurements (β = 3.312, p = .001). The outcomes at subsequent months 3 and 6 were also significantly different from the baseline (p < .001). As indicated in Fig. 2, the estimated scores of SMB for control group was increased from baseline to 1-month follow-up, then started to decrease after 1-month follow-up. For ENCM group, the estimated score of SMB was 46.73 at baseline and significantly increased to 54.27 at 6-month follow-up.
3.1.4. Distal outcomes: systolic and diastolic blood pressure (B/P)
As shown in Fig. 2, there was no difference in mean systolic B/Ps at baseline between ENCM group and control group. The mean estimated values of systolic B/P for control group was 130.46 mmHg and 131.62 mmHg for the ENCM group. However, changes in systolic B/P between baseline and 6 months in the ENCM group were significantly greater than that of the control group. For mean diastolic B/Ps, no difference was found between the ENCM group and the control group at baseline. In addition, the time trajectories of diastolic B/P were no different between the ENCM group and the control group. The difference between baseline and 6-month follow-up diastolic B/P measurement in the ENCM group was not significantly different from the control group though it was in the direction of decreasing (Fig. 2).
3.1.5. Distal outcome: waist circumference (WC) and body mass index (BMI)
The results of the WC measures were like those of the systolic B/P. The time trajectories of WC were different between the ENCM group and the control group. The estimated value of WC at baseline for the control group was 114.27 cm and 113.23 cm for the ENCM group. Both ENCM group and control group had similar WC at baseline, but the difference between ENCM and control group in their changes of WC observed at month 6 since baseline was significant (see Fig. 2). Compared to baseline, the ENCM group had a significantly decreased WC at 6-month follow-up. The BMI measurements had no differences across analyses.
In summary, four of the seven variables framed by the IFSMT demonstrated significant changes over six months period of this pilot study (Table 2). While the ‘Process’ variable of self-efficacy only showed trends of changing in the hypothesized direction, the ‘Context’ variable, perceived stress, showed significant (p = .047) change during that time. The ‘Proximal Outcome’ of SMB had a significant group by time interaction effect at month 6 (p = .005). The four IFSMT related ‘Distal Outcomes’ related to the participants’ health status had mixed results. The SBP showed no group effect or time effect, but did demonstrate a significant group by time interaction effect at month 6 (p = .037). The diastolic BP and BMI showed no differences across analyses. Finally, the WC measures had a group by time interaction effect at month 6 (p = .017).
4. Discussion
We tested the effect of the ENCM intervention on self-management context, process and outcomes framed by the IFSMT for low-income, African American adults with hypertension. We hypothesized that ENCM would reduce stress and increase self-efficacy of the study participants and positively impact their health status, including decreased B/P, BMI and WC. The pilot study results showed improvements in perceived stress, hypertension SMB, systolic B/P, and WC for the ENCM intervention group along with small to medium effect sizes for all measured variables (Table 2). As an IFSMT Social Environment Context factor, reduction of perceived stress would be creating a more favorable context for an individual or family to achieve positive self-management. This was the case as the hypertension SMBs also demonstrated improvements in this pilot study.
Testing of other models of nurse case management (NCM) is reported in the literature [5, 9, 14, 25] with varied outcomes related to client self-management of chronic diseases, including hypertension. This may be attributable to two primary factors. First, there is a failure of many providers to meaningfully understand and work with clients to address client-defined social, cultural and economic factors that contribute to poor self-management. Second, variations in both the specific interventions and the dose of the NCM protocol used lead to inconsistent results of NCM outcomes. NCM that incorporates trust building, self-monitoring skills and social support, as well as low-cost/convenient opportunities for physical activity have shown the most efficacy in SMB change in low-income African American populations [15, 19]. There has been growing evidence that “comprehensive care” for underserved groups is cost effective [24].
We found some improvements in the IFSMT [20] ‘Proximal’ and ‘Distal’ ‘Outcomes’ over the six-months of this pilot study between the control and ENCM groups. These groups had comparable samples of predominately uninsured, low-income, employed, single, female head-of-households. The proximal outcome of hypertension SMBs showed significant increases from baseline at 1, 3 and 6 months. However, though trending in the direction of improvements, no statistically significant time effect differences were found between the control and ENCM treated groups over 6 months in follow-up measurements of the distal outcomes of B/Ps, BMI, or WC, or the ‘Process’ variable of self-efficacy. When considered through the lens of the IFSMT [20], these findings fit the theoretical expectations of proximal outcomes changing before the distal outcomes. Indeed, the group by time interaction results of this pilot study showed the intervention group had significantly greater decreases than the control group in systolic B/P at 1 and 6 months and for WC at 1 month. The time effect analysis result indicated that the participants had better SMB in controlling their hypertension when they stayed involved in the study longer. Indeed, even with the small pilot sample size, Cohen’s evaluation standards revealed a medium treatment effect on systolic B/P by the end of 6 months (Cohen’s d = 0.55) showing promise for future larger clinical trials of ENCM.
Surprisingly, both groups had mean BPs (Table 2) that were under control by standards in effect at baseline [3]. These controlled BPs may be due to convenience sampling and monthly, free, comprehensive care clinic appointments. First, both study groups were convenience samples of self- or clinic-referred patients. Clinic staff referred patients under treatment for hypertension who were interested to the study and a few patients self-referred in response to study flyers. All enrolled participants were concerned about their B/Ps enough to take time to enroll in the study and continue their participation for six months. In addition, we found that the usual care at the free clinics was much more comprehensive than anticipated in the study design. In the anticipated usual medical model, clients would have ten-minute appointments with their provider each month, until their B/Ps stabilized and then visits every three to six months. In contrast, at the free clinics, all clients on medication had monthly appointments. Providers addressed many client physical and social needs during appointments. Specialists were on-site and available during the appointment times, at least for a brief consultation or introduction, including mental health, social workers, dental, vision and assorted medical specialist providers. Group health education and support, such as yoga, aerobic workouts, and nutrition classes were often available at the same time. This comprehensive care model at the free clinic might also explain the controlled B/Ps in the baseline measurements. As primary care service delivery models are becoming more comprehensive [2,26,27] we need to assess study sites’ care delivery and practice models and clearly define ‘usual care’ in research designs. Despite the comparable baseline B/Ps, we found significant interactions on systolic BP; WC and SMBs in month 6, that were significantly lower for the ENMC group than the control group. The practice of ENCM allowed the intervention nurse to meaningfully understand and work with clients to address client-defined social, cultural and economic factors that contribute to poor self-management and to provide appropriate support. Provision of self-management support is a focus of the ENCM intervention. Little literature is found related to the IFSMT [20] on the ‘Process’ components.
4.1. Limitations
There were several limitations to this study. It was a pilot study with a small sample size. A larger sample size may yield more results of greater statistical significance. All p-values are presented without adjustments for multiple comparison. This is appropriate given that this was a pilot study designed for the purposes of informing a future study with more statistical power. This study compensated participants with $20 gift cards for their measurement visits, which may not be financially feasible for a larger study. Other methods to facilitate participant retention would need to be considered. The participants on average had hypertension controlled in the prehypertension range [3] which may have limited the changes in measurements over time. This was unusual as, in the US, < 50% of those living with hypertension have their disease controlled [13]. A sample with a more usual distribution of hypertension control may have demonstrated more change over time with the ENCM intervention. We believe the lower average B/Ps may be attributed to clients’ monthly visits to the free clinic with its comprehensive, interprofessional model of care. These pilot study results are limited to generalizability to other low-income African American adults attending clinics with other models of care. Lastly, this study took place in an urban setting and would not be generalizable to other settings.
5. Conclusions
This clinical trial pilot study provides preliminary support for an innovative, well-defined nurse case management intervention to improve hypertension self-management for low-income African Americans. This was true even though both the experimental and control group participants had controlled hypertension at baseline. The intervention was effective especially for hypertension SMB and for the IFSMT distal outcomes of systolic B/P and WC. The small to medium effect sizes for all outcome variables in this pilot study indicate that the ENCM intervention should be tested in a larger clinical trial. Further research needs more focus on SMB, larger samples, examination of distal outcomes over time, and closer examination of other aspects of ‘Process’ variables in the IFSMT, such as self-efficacy which is a skill that can be developed [1]. Should further research support the effectiveness of ENCM, clinic nurses could be trained in ENCM and nurse visits included with each hypertension follow-up appointment. Health care cost savings could be realized for this chronic disease which is affecting disproportionate amounts of African Americans when targeted interventions are fully tested.
Acknowledgments
Research reported in this publication was supported by the National Institute of Nursing Research (NINR) of the National Institutes of Health (NIH) under Award Number P20NR015339. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Additional support was provided by the Office of Research and the College of Nursing at the University of Wisconsin-Milwaukee.
References
- [1].Alicea-Planas J, Improving self-efficacy for Latinos through goal setting at a community health center, Hispanic Health Care International 11 (3) (2013) 119–130, 10.1891/1540-4153.11.3.119. [DOI] [PubMed] [Google Scholar]
- [2].American Academy of Family Physicians (AAFP), The Patient-Centered Medical Home (PCMH), Retrieved from, 2017. http://www.aafp.org/practice-management/transformation/pcmh.html,.
- [3].Centers for Disease Controls and Prevention (CDC), High blood presure: Measuring blood pressure, Retrieved from, 2017. https://www.cdc.gov/bloodpressure/measure.htm,.
- [4].Centers for Disease Controls and Prevention (CDC), Healthy weight: About adult BMI, Retrieved from, 2017. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html,.
- [5].Chang A, Fritschi C, Kim MJ, Nurse-led empowerment strategies for hypertensive clients with metabolic syndrome, Contemp. Nurse 42 (1) (2012) 118–128. [DOI] [PubMed] [Google Scholar]
- [6].Chen D, Yang T, The pathways from perceived discrimination to self-rated health: an investigation of the roles of distrust, social capital, and health behaviors, Soc. Sci. Med 104 (2012) 64–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Cohen S, Janicki-Deverts D, Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009, J. Appl. Soc. Psychol 42(6) (2012) 1320–1334. [Google Scholar]
- [8].Coleman MT, Newton KS, Supporting self-management in patients with chronic illness, Am. Fam. Physician 72 (8) (2005) 1503–1510. [PubMed] [Google Scholar]
- [9].Crowley MJ, Powers BJ, Olsen MK, Grubber JM, Koropchak C, Rose CM,Maciejewski ML, The cholesterol, hypertension, and glucose education (CHANGE) study: results from a randomized controlled trial in African Americans with diabetes, Am. Heart J. 166 (1) (2013) 179–186. [DOI] [PubMed] [Google Scholar]
- [10].Egan BM, Bland VJ, Brown AL, Ferdinand KC, Hernandez GT, Jamerson KA, … Reed JW, Hypertension in African Americans aged 60 to 79 years: statement from the international society of hypertension in blacks, The Journal of Clinical Hypertension 17(4) (2015) 252–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Beckie TM, A systematic review of allostatic load, health, and health disparities, Biological Research for Nursing 14 (4) (2012) 311–346, 10.1177/1099800412455688. [DOI] [PubMed] [Google Scholar]
- [12].Han H, Lee H, Commodore-Mensah Y, Kim M, Development and validation of the hypertension self-care profile: a practical tool to measure hypertension self-care, J. Cardiovasc. Nurs (2013) 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. , Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association, Circulation 123 (8) (2011) 933–944 Retrieved from: http://circ.ahajournals.org/content/early/2011/01/24/CIR.0b013e31820a55f5.full.pdf+html. [DOI] [PubMed] [Google Scholar]
- [14].Joo J, Huber D, An integrative review of nurse-led community-based case management effectiveness, Int. Nurs. Rev 61 (2014) 14–24. [DOI] [PubMed] [Google Scholar]
- [15].Kirkendoll K, Clark PC, Grossniklaus D, Igho-Pemu P, Mullis R, Dunbar SB, Metabolic syndrome in African Americans: views on making lifestyle changes, J. Transcultural Nursing 21 (2) (2010) 104–113, 10.1177/1043659609357636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Kovach CR, Rababa M, Using branching simulations in treatment fidelity plans, Res. Gerontol. Nurs 7 (5) (2014) 216–223. [DOI] [PubMed] [Google Scholar]
- [17].Ocker LB, Melrose DR, Examining the validity of body mass index cut-off score for obesity of different ethnicities, Journal of Multicultural Gender and Minority Studies 2 (1) (2008) 1–7 Retrieved from: http://www.scientificjournals.org/journals2008/articles/1390.pdf. [Google Scholar]
- [18].Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW,Kurtz T, Sheps SG, Roccella EJ, Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on high blood pressure research, Circulation 111 (2005) 697–716. [DOI] [PubMed] [Google Scholar]
- [19].Rimando M, Perceived barriers to and facilitators of hypertension management among underserved African American older adults, Ethnicity & Disease 25 (3) (2015) 329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Ryan P, Sawin K, The individual and family self-management theory: background and perspectives on context, process, and outcome, Nurs. Outlook 57 (2009) 217–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Slotkin J, Kallen M, Griffith J, Magasi S, Salsman J, Nowinski C, Gershon R, NIH toolbox: Perceived stress survey technical manual, Retrieved from: http://www.nihtoolbox.org/HowDoI/TechnicalManual/Technical%20Manual%20sections/Toolbox%20Perceived%20Stress%20Survey%20Technical%20Manual.pdf,.
- [22].Slotkin J, Kallen M, Griffith J, Magasi S, Salsman J, Nowinski C, Gershon R, NIH toolbox: Self-efficacy survey technical manual, Retrieved from: http://www.nihtoolbox.org/HowDoI/TechnicalManual/Technical%20Manual%20sections/Toolbox%20Self-Efficacy%20Survey%20Technical%20Manual.pdf,.
- [23].Stata, Data analysis and statistical software: New in Stata – 14 release, Retrieved from, 2017. http://www.stata.com/new-in-stata/,.
- [24].Tasosa J, Schuster R, McAlearney JS, Cost-effectiveness of treating hypertension, hyperglycemia, and hyperlipidemia in African Americans and the general population with type 2 diabetes, J. Health Care Poor Underserved 21 (1) (2010) 161–176. [DOI] [PubMed] [Google Scholar]
- [25].Trief PM, Izquierdo R, Eimicke JP, Teresi JA, Goland R, Palmas W, Weinstock RS, Adherence to diabetes self-care for White, African-American and Hispanic American telemedicine participants: 5 year results from the IDEATel project, Ethnicity & Health 18(1) (2013) 83–96. [DOI] [PubMed] [Google Scholar]
- [26].U.S. Centers for Medicare and Medicaid Services (CMS), Comprehensive Primary Care Initiative, Retrieved from, 2017. https://innovation.cms.gov/initiatives/Comprehensive-Primary-Care-Initiative/,.
- [27].U.S. Centers for Medicare and Medicaid Services (CMS), Transforming clinical practice initiative, Retrieved from, 2017. https://innovation.cms.gov/initiatives/Transforming-Clinical-Practices/,.
- [28].Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, Simone G, Ferguson TB,Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM,Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM,Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R,Sorlie P, Stafford R, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J, American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics – 2010 update: a report from the American Heart Association, Circulation 121 (2010) 948–954. [DOI] [PubMed] [Google Scholar]
- [29].Centers for Disease Control and Prevention, National Health and Nutrition Examination Survey. Anthropometry Procedures Manual, (2011) Available at http://www.cdc.gov/nchs/data/nhanes/nhanes_11_12/Anthropometry_Procedures_Manual.pdf.
- [30].Rubin DB, Multiple imputation after 18+ years, J. Am. Stat. Assoc 91 (434) (1996) 473–489. [Google Scholar]