Abstract
Purpose
Childhood overweight/ obesity is one of critical public health concern. It has been suggested that there is a link between breakfast skipping and obesity. However, results are conflicting. The aim of the present study was to summarize the association between breakfast skipping and overweight/obesity in children and adolescent.
Methods
We performed a literature search using Pubmed/Medline, Scopus, Web of Science and EMBASE electronic databases from 2000 through 28 February 2018 without language limitation. Observational studies in which risk measures were reported regarding the link between breakfast skipping and obesity in children and adolescent were included. Studies with at least the score of 5 from Newcastle-Ottawa Scale were considered as low risk of bias. Random effect model was used for data synthesis.
Results
Of 3276 publications, finally 16 studies (14 cross-sectional studies, 2 cohort studies) were included for meta-analysis. Based on cross-sectional studies, we found a positive association between breakfast skipping and obesity (Odd ratio (OR) trim & fill: 1.43; 95%CI: 1.32, 1.54), while cohort studies showed no significant link (OR:1.01, 95%CI: 0.93, 1.11; I2: 48%, p = 0.14). Subgroup analysis in cross-sectional studies showed that the association between breakfast skipping and the risk of obesity in boys was OR: 1.64; 95% CI: 1.38, 1.95; I2: 38.3%, p = 0.18, while it was 1.56 (95% CI: 1.38, 1.77, I2: 0.0%, p = 0.49) in girls.
Conclusion
The risk of obesity in children and adolescents who skipped breakfast was 43% greater than those who ate breakfast regularly in cross-sectional studies, while no significant link was found in cohort studies. However, due to high heterogeneity and limited cohort studies, findings should be interpreted by caution.
Keywords: Breakfast skipping, Child, Adolescent, Obesity
Introduction
Childhood overweight/ obesity is one of critical public health concern in the twenty-first century. The prevalence of obesity in children and adolescence have been rising at alarming level [1]. Based on the report by the World Health Organization (WHO), obesity rate increased markedly from 11 million in 1975 to 124 million in 2016 among subjects under 18 years olds across the world [2]. Childhood obesity is worrisome due to the evidence that obese children and adolescence are greater at risk for obesity and other chronic diseases including diabetes mellitus, cardiovascular diseases and dyslipidemia in adulthood [3].
Although certain mechanisms of obesity in children and adolescent have not been identified so far, it is well established that healthy dietary patterns play key roles in total energy intake and weight management [4–6]. One of the proposed dietary factors influencing body weight and energy intake is breakfast eating [7]. Based on earlier studies, breakfast eating is associated with healthy dietary patterns [8]. For instance, the consumption of whole grain, fruit and dairy products in children who skipped breakfast was less than breakfast eaters [9]. It has been suggested that there was a link between breakfast skipping and the consumption of larger meal portions and snacks in the rest of the day. Accordingly, breakfast is an important meal to regulate energy balance and probably is a preventing strategy to decrease the risk of adiposity.
Although several studies found positive association between breakfast skipping and obesity [10–15], some studies did not show any significant association [16–18]. Based on such discrepancies, we cannot make a certain decision whether breakfast skipping increases the risk of obesity in children and adolescent or not.
To the best of our knowledge, there is only one meta-analysis on skipping breakfast and obesity. In the study by Horikawa et al., it has been reported that the risk of overweight/ obesity in subjects in the lowest category was 75% greater than those in the highest one [7]. However, they did not report the association in children, separately. In this study, most included studies were on adult populations and the link remained unclear in subjects under 18 years old. In addition, they limited their study to Asian and Pacific regions. Due to differences in cultural, social and economic status among countries, we cannot generalize the findings by Horikawa et al., to all societies. Moreover in the previous meta-analysis, methodological quality of the included studies were not examined. All the aforementioned issues points to the necessity for doing a meta-analysis. The purpose of the present study was to summarize the association between breakfast skipping and overweight/obesity in children and adolescents in observational studies and do a meta-analysis, if possible.
Methods & materials
Search strategy
We performed a literature search using Pubmed/Medline, Scopus, Web of Science and EMBASE electronic databases from 2000 through 28 February 2018 without language limitation. To find publications examining the association between breakfast skipping and risk of overweight or obesity in children and adolescent the following free terms and the Medical Subject Headings (MeSH) were used: breakfast OR meal in combination with obesity OR obese OR adiposity OR weight OR “body mass index” OR “BMI” AND child OR adolescent OR boy OR girl and their synonyms. To avoid missing any relevant publications, we also searched the reference lists of the relevant articles manually.
The protocol of the study was registered in the international prospective register of systematic reviews (PROSPERO) database (http://www.crd.york.ac.uk/PROSPERO; registration number: CRD42019115665).
Selection criteria
The inclusion criteria for publications were as follows: i) observational (cross-sectional, cohort, case-control) studies, ii) studies on children and adolescent, iii) reporting breakfast as an exposure and overweight and/or obesity as an outcome, iv) reporting risk measures for overweight and/or obesity based on BMI criteria, iv) reporting relative risk (RR) or odd ratio (Odd ratio) and 95% confidence intervals (CIs). Studies were excluded if they were clinical trials, case reports, case series, animal studies, or other types of studies except observational studies, examined adult populations, report overall meal pattern or other meals skipping, and considered other criteria expect BMI for obesity, or report results by providing frequency or mean and standard deviations or other forms except RR/OR and 95% CI for obesity. It is notable that only studies that examine the association between breakfast skipping and overweight/obesity as their primary outcome was included. In addition, grey literatures including theses, conference papers, interviews, etc. were not included.
“Breakfast skipping group” is commonly defined as subjects who consumed breakfast at all or ate maximum two times per week in an individual study. Although the definition of overweight/ obesity varied among studies, we considered all studies that reported overweight and/or obesity as an outcome. When more than one paper was published from the same population, the newest one with the most complete data was included.
Three investigators independently examined the eligibly of each study (N.N, H.G, E.A) for qualitative and quantitative synthesis. In addition, studies that reported changes in BMI instead of BMI, was not included. In some studies, overweight/obesity was considered exposure and breakfast skipping as an outcome, such studies that their aims were different from the purpose of the current meta-analysis were not included.
Data extraction
Two reviewers (N.N, M.J, R.J) independently extracted the following data based on pre-defined standard form from each publication: the first author’s name, year of publication, location, sample size, participants’ characteristics (age, gender), method for anthropometric measurements, comparison groups, and controlled covariates. It is notable that if more than one measurement was conducted, the last measurement was extracted. In each step, when there was any discrepancy, it was resolved by principal investigators (L.A or B.L).
Quality assessment
The methodological quality of the included studies was evaluated with two independent investigators (E.A, M.Z) independently using the Newcastle-Ottawa Scale for cross-sectional and cohort studies [19]. Studies with at least the score of 5 were considered as high-quality. Any discrepancy was resolved by the third investigator (R.J).
Statistical analysis
To examine the association between skipping breakfast and the risk for obesity, pooled RR and 95% confidence intervals (CIs) for skippers vs. non-skippers were computed using a random-effect model. For meta-analysis, the most fully adjusted model was pooled with the DerSimonian and Laird method. Between-study heterogeneity was assessed using I2 index. I2 values greater than 50% were considered as substantial heterogeneity. To reduce heterogeneity, subgroup analysis was performed if there were at least two studies in each category. Complementary analyses including sensitivity analysis and full & trim were performed as well. To examine publication bias, Egger’s regression asymmetry test was performed. Statistical analyses were conducted using Stata, version 11.0 (Stata Corp, College Station, TX). P value <0.05 was considered statistically significant.
Results
Study characteristics
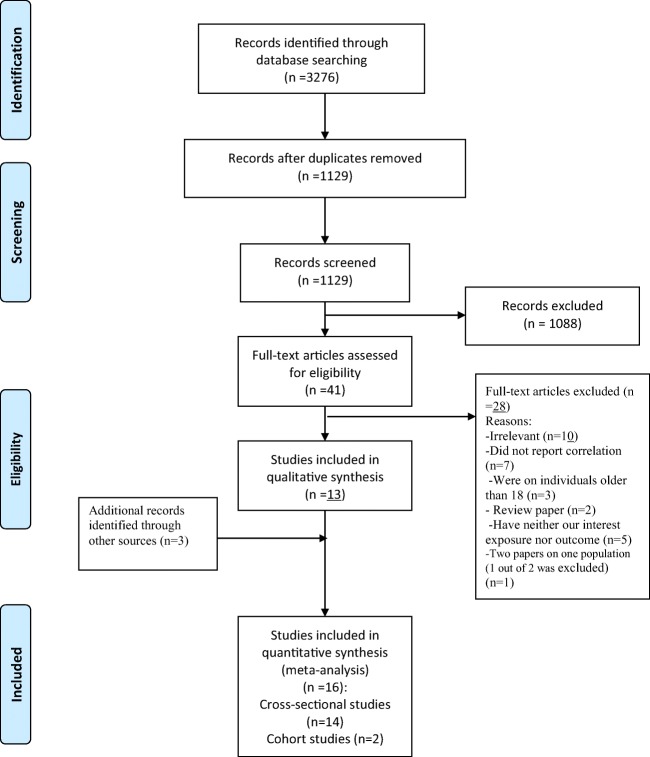
As it is illustrated in Fig. 1, the initial search of four electronic databases yielded 3276 (2147 duplicates) studies. After the evaluation of titles and abstracts (n = 1129), 1088 studies were excluded. In the next step, of 41 fulltexts, 28 studies did not meet our criteria were excluded due to the following reasons: irrelevant (n = 10), did not report correlation (n = 7), were on individuals older than 18 (n = 3), review paper (n = 2), and have neither our interest exposure nor outcome (n = 5). In addition, two studies were on same participants, therefore, only one [12] of them with greater sample size that its main purpose was the evaluation of the link between breakfast skipping and the risk of obesity was included. Three relevant papers were found from reference lists as well. Finally, 16 papers (14 cross-sectional studies, 2 cohort studies) that evaluated the association between breakfast skipping and the risk of overweight/obesity in children and adolescent were included (Fig. 1).
Fig. 1.
Selection processes of eligible papers
Main characteristics of studies are represented in Table 1. The 16 included studies [10–18, 20–26] in qualitative studies were published between 2005 and 2018. Sample size ranged from 523 [15] to 25,176 [10] individuals. The design of the most studies was cross-sectional (n = 14) [10–16, 20–26] and only two [17, 18] were cohort studies. In addition, all studies obtained minimum the half score of quality checklist and considered as high quality.
Table 1.
Main characteristics of studies examined the association between breakfast skipping and overweight/obesity in children and adolescents
| First Author (Year) | Study design | Location | Sample size | Characteristics of participants | Age range (years) | Anthropometric assessment | Comparison groups | Adjustment | Quality score |
|---|---|---|---|---|---|---|---|---|---|
| Anderson et al., 2005 [16] | Cross-section | Norway | 1432 | Both genders/ fourth & eighth graders | 11 | Self-reported | ≤ 2 vs. 6-7 times/weak eating breakfast | Age, gender, social class, watching TV, Energy | 7 |
| Harding et al., 2008 [13] | Cross-section | London | 6599 | Both sexes | 11-13 | Standard measurement | Skippers vs. eaters | Gender | 5 |
| Dialectakou et al., 2008 [11] | Cross-section | Piraeus | 811 | High school students | 16 | Standard measurement | Skipper s vs. regular eaters | sex, age, ethnicity, smoking, dieting, physical activity, and parental education | 5 |
| Dubios et al., 2008 [12] | Cross-section | Canada | 1549 | Both sexes, Healthy children | 4 | Standard measurement | Skippers (fewer than 7 days) vs. eaters | Gender, mother’s education | 5 |
| Crozen et al., 2009 [10] | Cross-section | Netherland | 25,176 | Both sexes Adolescents in grade 2 & 4 | 13-16 | Self-reported | Skipping >2 days vs. 0 days | Gender, family situation, ethnic background, education, smoking | 6 |
| Maddah et al., 2009 [14] | Cross-section | Iran | 6635 | Both genders at elementary schools | 6-11 | Standard measured | Skipping vs. non-skipping (no clear definition) | age, sex, maternal educational level, television viewing, birth rank, mother’s employment, parental overweight/obesity, walking, birth weight | 6 |
| Thompson et al., 2010 [15] | Cross-section | Fiji | 523 | Adolescent girls | 16.6 | Self-reported | Skippers vs. regular eaters | Not clear | 6 |
| Dupuy et al., 2011 [22] | Cross-section | France | 7154 | Both genders, WHO-collaborative Health behavior in schoo-aged children study (HBSC) study, | 11-15 | Self-reported | Not daily eating vs. daily eating | Age, sex, marital status, educational level, monthly income, cigarette smoking, alcohol consumption, betel quid chewing and exercise habit | 6 |
| Duncan et al., 2011 [21] | Cross-section | Brazil | 3397 | Children & adolescents, both genders | 7-18 | Standard measured | 5 days a week vs. never | Sex, age, father education, mother education | 7 |
| Kim et al., 2012 [17] | Cohort | Korea | 20,962 | Adolescents, both genders | 15 | Self-reported | 1-2 times/wks vs.6-7 times/wks | Age, frequency of smoking, frequency of drinking, the parents’ education level, economic status, frequency of vigorous physical activity (PA), frequency of moderate PA, frequency of muscular strength exercises, mental stress, and sleep duration | 6 |
| Shafiee et al., 2013 [24] | Cross-section | Iran | 5625 | Both genders, children and adolescents | 10-18 | Standard measurements | 0-2 days/wks vs. 6-7 days/wks | Age, sex, family history of chronic disease, educations of parents, physical activity, socioeconomic status | 6 |
| Bjonara et al., 2013 [26] | Cross-section | 8 European countries | 6512 | Both genders, students at final year of primary school | 10-12 | Self-reported | 7 days a weak vs. 0-6 days a weak | Sex, ethnicity, education level | 6 |
| Kuper et al., 2014 [18] | Cohort | Netherland | 1366 | Both genders, children | 5 | Standard measurement | Skippers (fewer than 7 days) vs. eaters | Age, gender, birth weight, maternal BMI, parental BMI, single parenting, maternal educational level | 5 |
| Ahadi et al., 2015 [20] | Cross-section | Iran | 13,486 | Children and adolescents, both genders | 6-18 | Standard measurement | 0-2 days/wks vs. 5-7 days/wks | Age, sex, family history of chronic diseases, screen time, physical activity, socio-economic status | 8 |
| Nilsen et al., 2017 [23] | Cross-section | Sweden | 2620 | Children | 7-9 | Standard measurement | Skipper vs. eaters | 5 | |
| Tee et al., 2018 [25] | Cross-section | Malaysia | 5332 | Children and adolescents | 6-17 | Standard measurement | Skippers vs. regular eaters | Age, sex, ethnicity, fathers education, income, physical activity | 6 |
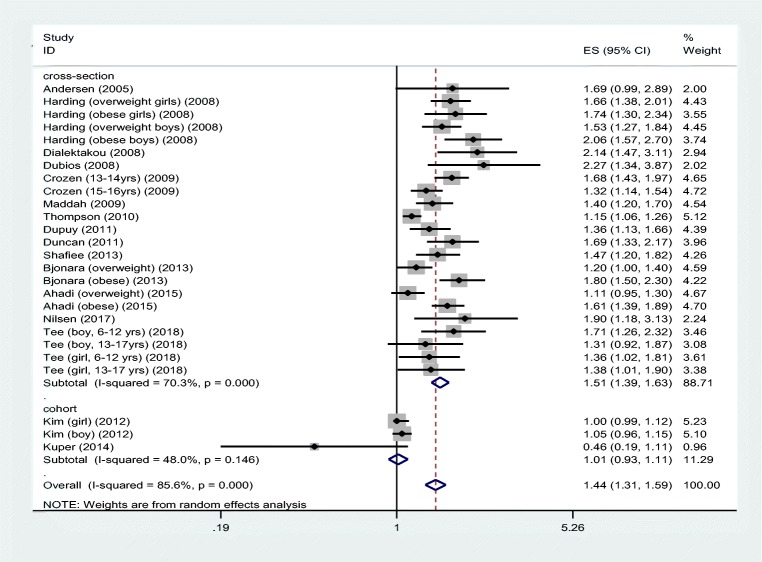
Findings from a meta-analysis
Based on the pooled 23 effect sizes extracted from 14 cross-sectional studies, we found that there was a positive association between breakfast skipping and the risk of overweight/obesity (Pooled OR: 1.51; 95% CI: 1.39, 1.63). However, the heterogeneity was high (I2: 70.3%, p = 0001) (Fig. 2). Meta-analysis of two cohort studies (three effect sizes) showed that the link between breakfast skipping and obesity is not significant (OR: 1.01; 95% CI: 0,93, 1.11; I2: 48%, p = 0.14) (Fig. 2).
Fig. 2.
The association between breakfast skipping and overweight/obesity in children and adolescents
In cross-sectional studies, subgroup analysis on sex revealed that the association between breakfast skipping and the risk of obesity in boys was 1.64; 95% CI: 1.38, 1.95; I2:38.3%, p = 0.18), while it was 1.56; 95% CI: 1.38, 1.77, I2:0.0%, p = 0.49) Besides, stratification by age showed that in individuals less than 12 years OR was 1.53; 95% CI: 1.33, 1.77, while the association was 1.49; 95% CI: 1.35, 1.65 in olders (Table 2). After excluding two studies adjusted for energy intake, the association did not change considerably (OR: 1.49, 95%CI: 1.37, 1.62; I2:71.6, p = 0.0001).
Table 2.
Subgroup analysis for the association between breakfast skipping and overweight/obesity in children and adolescents
| Outcome | No. effect size | Pooled effect size (95% CI) | I2 (%) | P heterogeneity |
|---|---|---|---|---|
| Gender | ||||
| Boy | 4 | 1.64 (1.38, 1.95) | 38.3 | 0.18 |
| Girl | 4 | 1.56 (1.38, 1.77) | 0 | 0.49 |
| Both | 15 | 1.47 (1.33, 1.63) | 75.2 | 0.0001 |
| Overweight | 8 | 1.44 (1.26, 1.65) | 71.9 | 0.001 |
| Obese | 5 | 1.68(1.52, 1.86) | 11.1 | 0.34 |
| Both in combination | 10 | 1.45 (1.28, 1.65) | 64.7 | 0.002 |
| Age (years) | ||||
| < 12 | 8 | 1.53 (1.33, 1.77) | 51.6 | 0.04 |
| ≥12 | 15 | 1.49 (1.35, 1.65) | 76.1 | 0.0001 |
For cross-sectional studies, sensitivity analysis showed the robustness of findings and based on Funnel plot, there was publication bias that was confirmed by the Egger test (p = 0.001). After using fill and trim test to correct the pooled RR, 5 studies were added and the effect estimate declined to 1.43 (95%CI: 1.32, 1.54), while remained significant.
Discussion
Findings of the current meta-analysis, proved the hypothesis that breakfast skipping increased the risk of overweight/obesity in cross-sectional studies. It was revealed that the risk of overweight /obesity in children and adolescent who skipped breakfast was 43% greater than those who ate breakfast regularly, while no significant link was found in cohort studies. As most studies had cross-sectional design and only two were cohort studies, we cannot make a decision regarding the cause-effect relationship between breakfast skipping and overweigh/obesity. Therefore, more studies are needed to clarify this link. Overall, findings should be interpreted by great caution.
To the best of our knowledge, it is the first meta-analysis on the association between breakfast skipping and the risk of overweight/obesity among children and adolescent covering all countries. In the meta-analysis by Horikawa et al., all studies without any age range limitation were included. Most included studies were on adult populations and no subgroup analysis was conducted to provide findings in adult and children, separately. Horikawa et al., found that breakfast skipping increased the risk of overweight/ obesity by 75% in individuals living in Asian and Pacific regions [7]. Differences in the amount of RRs, can be explained by the difference in age range of the study populations and locations. In the study by Horikawa et al., [7] all age groups in only Asia and Pacific countries were included, while we did not put any limitations for the study location.
It should be kept in mind that cut-off points for the definition of breakfast skipping were different among studies that might affect the result. However, due to limited studies with similar cut-off points, we could not compare the results among them. Furthermore, time of eating breakfast, breakfast composition, eating or skipping other meals and dietary patterns can play pivotal roles on the risk of obesity. However, in the most included studies they were not evaluated. Breakfast is defined as the first meal of the day that it is eaten within 2 h after waking up and typically it should be no later than 10:00 a.m. and including 20 to 35% of total energy need [23]. Therefore, consuming breakfast after this time might not be as useful as eating late. It is notable to consider this point when studying on the effects of breakfast on people’s health. Based on the study by Dubios et al., the snacks of breakfast skippers had greater energy and their diet consisted of larger servings of dairy products, grains, carbohydrate, total fat and protein [12]. Children who skipped breakfast consumed less protein than those who ate breakfast regularly. All in all, interactions between time of eating meals, meal patterns and quantity of each macronutrient can also affect the association [12].
Potential factors that can affect skipping breakfast are educational level, family composition (two- parents, single- parent families), ethnicity, physical activity level, age and gender. In the present meta-analysis, all the included studies were adjusted for such confounding factors. However, only two studies adjusted results for energy intake. Total energy intake plays a key role on BMI and ignoring this can affect the results. Furthermore, all the included studies had high quality. Therefore, the quality cannot affect the pooled RR and we can rely on findings.
In the current meta-analysis, subgroup analysis was conducted to reduce the heterogeneity. Stratification by gender, relatively could justify the between-study heterogeneity. Although heterogeneity was reduced in boy and girl categories, heterogeneity remained high in studies in which findings were reported for a combination of both genders.
Girls, particularly at younger age pay more attention to their body shape and weight compare to boys. When someone skipped breakfast, usually they have poorer dietary quality and lower physical activity levels [25]. Some previous studies have indicated that skipping breakfast is linked with less healthy dietary patterns characterized by high intake of fast foods, soft drinks and high fat and salt meals. It is likely that this factor affect the results [25]. However, in our studies, overlap points were observed in CIs in boys and girls categories and no considerable differences were observed between two genders.
It is notable that in the present meta-analysis, all studies except two [17, 18] had cross-sectional design. Accordingly, we cannot make a decision whether it is a cause and effect relationship or not.
According to the MSNS study, a lack of appetite and time was the main reason to skip breakfast. Feeling stomachache after breakfast and waking up late in the morning were also reported as the most common reasons to eliminate breakfast [25]. However, in the included studies, they did not examine the reason of skipping and only focused on the association with obesity.
Based on previous studies, individuals who consumed breakfast regularly had greater thermogenesis than those who skipped breakfast [7]. Through this possible mechanism, having daily breakfast can control weight. Another proposed mechanism that can justify the association is related to the effects of breakfast on appetite and total energy intake. Indeed, meal frequency impact upon energy balance and eating breakfast can modulate energy intake in the next meals and it prevents overeating throughout the day. Hence, the component of breakfast can play a key role on the link between breakfast and weight management. Fiber-rich breakfasts, for instance, are likely to improve postprandial glycemic responses, satiety and insulin sensitivity compared to other types. In addition, consuming more energy at dinner may reduce appetite in the morning. Therefore, nutrition recommendation regarding energy disturbance and attention to the interval between dinner and sleep may solve this problem.
Nutrition education at schools can be an effective strategy to encourage children and their parents to consume regular meals. Although nutrition education is not a formal course in school curriculum, dedicating even a short time to introduce healthy diets can be helpful to prevent some chronic diseases throughout life.
The present meta-analysis have several limitations as follows: (i) most studies had cross-sectional design and thus casual relationship remained unclear, (ii) the between-study heterogeneity was not attenuated considerably even after subgroup analysis, and (iii) search was not conducted systematically, (iv) time and composition of breakfast was not evaluated. However, the present study was the first meta-analysis in children and adolescent population in this regard. Other strength points of the present meta-analysis were due to evaluating study quality and doing sensitivity analysis.
In conclusion, the risk of obesity in children and adolescents who skipped breakfast was 43% greater than those who ate breakfast regularly in cross-sectional studies, no significant link was found in cohort studies. However, due to high heterogeneity findings should be interpreted by great caution. In addition, more cohort studies are needed to clarify the cause and effect association between breakfast skipping and the risk of overweight/obesity in children and adolescent.
Availability of data and materials
Not applicable
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict interests.
Ethics approval and consent to participate
Not applicable
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nazli Namazi, Email: nazli.namazi@yahoo.com.
Bagher Larijani, Email: larijanib@tums.ac.ir.
Leila Azadbakht, Email: azadbakhtleila@gmail.com.
References
- 1.World health organization. Global Strategy on Diet, Physical Activity and Health.
- 2.World health organization. Tenfold increase in childhood and adolescent obesity in four decades: new study by Imperial College London and WHO. 2018.
- 3.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011;35(7):891. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 4.Azadbakht L, Haghighatdoost F, Feizi A, Esmaillzadeh A. Breakfast eating pattern and its association with dietary quality indices and anthropometric measurements in young women in Isfahan. Nutrition. 2013;29(2):420–425. doi: 10.1016/j.nut.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Esmaillzadeh A, Azadbakht L. Major dietary patterns in relation to general obesity and central adiposity among Iranian women. J Nutr. 2008;138(2):358–363. doi: 10.1093/jn/138.2.358. [DOI] [PubMed] [Google Scholar]
- 6.Schröder H, Marrugat J, Vila J, Covas MI, Elosua R. Adherence to the traditional Mediterranean diet is inversely associated with body mass index and obesity in a Spanish population. J Nutr. 2004;134(12):3355–3361. doi: 10.1093/jn/134.12.3355. [DOI] [PubMed] [Google Scholar]
- 7.Horikawa C, Kodama S, Yachi Y, Heianza Y, Hirasawa R, Ibe Y, et al. Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med. 2011;53(4-5):260–267. doi: 10.1016/j.ypmed.2011.08.030. [DOI] [PubMed] [Google Scholar]
- 8.Potter C, Griggs RL, Brunstrom JM, Rogers PJ. Breaking the fast: meal patterns and beliefs about healthy eating style are associated with adherence to intermittent fasting diets. Appetite. 2019;133:32–39. doi: 10.1016/j.appet.2018.10.020. [DOI] [PubMed] [Google Scholar]
- 9.Rampersaud GC, Pereira MA, Girard BL, Adams J, Metzl JD. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc. 2005;105(5):743–760. doi: 10.1016/j.jada.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Croezen S, Visscher T, Ter Bogt N, Veling M, Haveman-Nies A. Skipping breakfast, alcohol consumption and physical inactivity as risk factors for overweight and obesity in adolescents: results of the E-MOVO project. Eur J Clin Nutr. 2009;63(3):405. doi: 10.1038/sj.ejcn.1602950. [DOI] [PubMed] [Google Scholar]
- 11.Dialektakou KD, Vranas PB. Breakfast skipping and body mass index among adolescents in Greece: whether an association exists depends on how breakfast skipping is defined. J Am Diet Assoc. 2008;108(9):1517–1525. doi: 10.1016/j.jada.2008.06.435. [DOI] [PubMed] [Google Scholar]
- 12.Dubois L, Girard M, Kent MP, Farmer A, Tatone-Tokuda F. Breakfast skipping is associated with differences in meal patterns, macronutrient intakes and overweight among pre-school children. Public Health Nutr. 2008;12(1):19–28. doi: 10.1017/S1368980008001894. [DOI] [PubMed] [Google Scholar]
- 13.Harding S, Teyhan A, Maynard MJ, Cruickshank JK. Ethnic differences in overweight and obesity in early adolescence in the MRC DASH study: the role of adolescent and parental lifestyle. Int J Epidemiol. 2008;37(1):162–172. doi: 10.1093/ije/dym252. [DOI] [PubMed] [Google Scholar]
- 14.Maddah M, Nikooyeh B. Factors associated with overweight in children in Rasht, Iran: gender, maternal education, skipping breakfast and parental obesity. Public Health Nutr. 2009;13(2):196–200. doi: 10.1017/S1368980009990589. [DOI] [PubMed] [Google Scholar]
- 15.Thompson-McCormick JJ, Thomas JJ, Bainivualiku A, Khan AN, Becker AE. Breakfast skipping as a risk correlate of overweight and obesity in school-going ethnic Fijian adolescent girls. Asia Pac J Clin Nutr. 2010;19(3):372. [PMC free article] [PubMed] [Google Scholar]
- 16.Andersen LF, Lillegaard ITL, Øverby N, Lytle L, Klepp K-I, Johansson L. Overweight and obesity among Norwegian schoolchildren: changes from 1993 to 2000. Scandinavian journal of public health. 2005;33(2):99–106. doi: 10.1080/140349404100410019172. [DOI] [PubMed] [Google Scholar]
- 17.Kim J-H, So W-Y. Association between frequency of breakfast eating and obesity in Korean adolescents. Iran J Public Health. 2012;41(6):50. [PMC free article] [PubMed] [Google Scholar]
- 18.Küpers L, De Pijper J, Sauer P, Stolk R, Corpeleijn E. Skipping breakfast and overweight in 2-and 5-year-old Dutch children—the GECKO Drenthe cohort. Int J Obes. 2014;38(4):569. doi: 10.1038/ijo.2013.194. [DOI] [PubMed] [Google Scholar]
- 19.Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2011. [Google Scholar]
- 20.Ahadi Z, Qorbani M, Kelishadi R, Ardalan G, Motlagh M, Asayesh H, et al. Association between breakfast intake with anthropometric measurements, blood pressure and food consumption behaviors among Iranian children and adolescents: the CASPIAN-IV study. Public Health. 2015;129(6):740–747. doi: 10.1016/j.puhe.2015.03.019. [DOI] [PubMed] [Google Scholar]
- 21.Duncan S, Duncan EK, Fernandes RA, Buonani C, Bastos KD, Segatto AF, et al. Modifiable risk factors for overweight and obesity in children and adolescents from São Paulo, Brazil. BMC Public Health. 2011;11(1):585. doi: 10.1186/1471-2458-11-585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dupuy M, Godeau E, Vignes C, Ahluwalia N. Socio-demographic and lifestyle factors associated with overweight in a representative sample of 11-15 year olds in France: results from the WHO-collaborative health behaviour in school-aged children (HBSC) cross-sectional study. BMC Public Health. 2011;11(1):442. doi: 10.1186/1471-2458-11-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nilsen BB, Yngve A, Monteagudo C, Tellström R, Scander H, Werner B. Reported habitual intake of breakfast and selected foods in relation to overweight status among seven-to nine-year-old Swedish children. Scand J Public Health. 2017;45(8):886–894. doi: 10.1177/1403494817724951. [DOI] [PubMed] [Google Scholar]
- 24.Shafiee G, Kelishadi R, Qorbani M, Motlagh ME, Taheri M, Ardalan G, et al. Association of breakfast intake with cardiometabolic risk factors. J Pediatr. 2013;89(6):575–582. doi: 10.1016/j.jped.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 25.Tee ES, Nurliyana AR, Karim NA, Jan Mohamed HJB, Tan SY, Appukutty M, et al. Breakfast consumption among Malaysian primary and secondary school children and relationship with body weight status-findings from the MyBreakfast study. Asia Pac J Clin Nutr. 2018;27(2):421. doi: 10.6133/apjcn.062017.12. [DOI] [PubMed] [Google Scholar]
- 26.Bjørnarå HB, Vik FN, Brug J, Manios Y, De Bourdeaudhuij I, Jan N, et al. The association of breakfast skipping and television viewing at breakfast with weight status among parents of 10–12-year-olds in eight European countries; the ENERGY (EuropeaN Energy balance research to prevent excessive weight gain among youth) cross-sectional study. Public Health Nutr. 2014;17(4):906–914. doi: 10.1017/S136898001300061X. [DOI] [PMC free article] [PubMed] [Google Scholar]